Developmental Anatomy of the Retinal and Choroidal Vasculature

Developmental Anatomy of the Retinal and Choroidal Vasculature
B Anand-Apte and J G Hollyfield, Cleveland Clinic, Cleveland, OH, USA
ã
2010 Elsevier Ltd. All rights reserved.
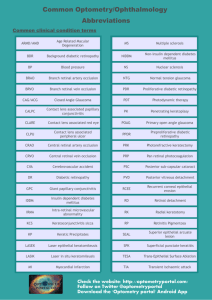
Glossary
Angiogenesis
– The formation of new blood vessels from preexisting ones, generally by sprouting.
Central retinal artery
– A branch of the ophthalmic artery that enters the eye via the optic nerve.
Choriocapillaris
– An exceptionally dense capillary bed that nourishes the posterior choroid up to the level of the equator of the eye.
Circle of Zinn
– An annular artery surrounding the optic nerve. Its branches contribute to the pial circulation, the optic nerve at the level of the lamina cribrosa and to the nerve fiber layer of the optic disk.
Fenestrae – The circular openings in the choriocapillaris facing Bruch’s membrane that choriocapillaries have a diaphragm covering.
Posterior ciliary arteries
– The branches of the ophthalmic artery that form the blood supply to the choroid.
Vasculogenesis
– The formation of new blood vessels through de novo formation of new endothelial cells.
Vortex veins
– The venous collecting vessels draining the choroid, ciliary body, and iris.
By the sixth week (12–17-mm stage), the choriocapillary network begins to develop a basal lamina. This, together with the basement membrane of the RPE, forms the initial boundaries of Bruch’s membrane separating the neural retina from the choroid. Concomitantly, rudimentary vortex veins develop in all four quadrants of the eye. Except for the two basal lamina (of the RPE and choriocapillaris), the only other component of Bruch’s membrane at this stage is a collagenous central core. The choroidal capillary network becomes almost completely organized by the eighth week (25–30-mm stage) with connections to the short posterior ciliary arteries. By the eleventh week (50–60-mm stage), the posterior ciliary arteries show extensive branching throughout the choroid. It is only following the third and fourth months of gestation that most of the choroidal vasculature matures.
While the molecular mechanisms regulating choroidal development have not been fully defined, it is largely accepted that the presence of differentiated RPE and its secretion of growth factors, such as vascular endothelial growth factor (VEGF) and fibroblast growth factor 9
(FGF-9), are critical for the physiological development and differentiation of the choroidal vascular network.
Choroidal Vascular Network
Embryology
At the fourth week of gestation in humans (5-mm stage), the undifferentiated mesoderm surrounding the optic cup begins to differentiate and form endothelial cells adjacent to the retinal pigment epithelium (RPE). These early vessels are the precursors of the choriocapillaris, which ultimately envelop the exterior surface of the optic cup. Concurrently, the hyaloid artery branches from the primitive dorsal ophthalmic artery and passes along the embryonic (choroidal) fissure to enter the optic cup. Shortly thereafter, the condensation of the mesoderm occurs at the site of future choroidal and scleral stroma with the gradual onset of pigmentation in the outer neuroepeithelial layer of the optic cup, the RPE. By the fifth week of development
(8–10-mm stage), the RPE becomes more melanized and the vascular plexus extends along the entire exterior surface of the cup from the posterior pole to the optic cup rim.
Gross Anatomy
Almost the entire blood supply of the eye comes from the choroidal vessels, which originate from the ophthalmic arteries. The left and right ophthalmic arteries arise as the first major branch of the internal carotid, usually where the latter break through the dura to exit the cavernous sinus. In some individuals (around 10%), the ophthalmic artery arises within the cavernous sinus, while in others
(around 4%), it arises from the middle meningeal artery, a branch of the external carotid.
The ophthalmic artery shows a wide variation in the branching pattern as it approaches the eye. The posterior ciliary arteries, which form the blood supply to the choroid, and the central retinal artery, which enters the eye via the optic nerve, are branches of the ophthalmic artery
(
Figure 1
). Other branches of the ophthalmic artery supply the lacrimal gland, extraocular muscles, and lids.
The choroid (also referred to as the posterior uveal tract) is vascularized by two separate arterial systems:
(1) the short posterior ciliary arteries, which supply the posterior choroid and (2) the long posterior ciliary arteries, which supply the anterior portion of the choroid
(as well as the iris and ciliary body).
9
10 Developmental Anatomy of the Retinal and Choroidal Vasculature
Approximately 16–20 short posterior ciliary arteries penetrate the sclera in a circular pattern surrounding the optic nerve, with the distance between these vessels and the nasal side of the nerve being closer than that on the temporal side. These arteries anastomose within the sclera to form the circle of Zinn, an annular artery surrounding the optic nerve (
Figures 1 and
2
). The branches from the circle of Zinn contribute to the pial circulation, the optic nerve at the level of the lamina cribrosa, and the nerve fiber layer of the optic disk. Other branches from the circle of Zinn along with direct branches from the short posterior ciliary arteries enter the choroid to provide the arterial blood supply to the posterior uveal track.
These arteries divide rapidly to terminate in the choriocapillaris, an exceptionally dense capillary bed that nourishes the posterior choroid up to the level of the equator of the eye.
The two long posterior ciliary arteries penetrate the sclera on either side of the optic nerve near the level of the horizontal meridian of the eye. The temporal long posterior ciliary artery enters the sclera approximately 3.9 mm from the temporal border of the optic nerve while the nasal long posterior ciliary artery enters approximately 3.4 mm from the nasal border of the optic nerve. Additional long posterior ciliary arteries are present that course farther toward the anterior segment before penetrating the sclera, usually more anterior than the entry of the temporal and nasal long posterior ciliary arteries. The long posterior ciliary arteries course through the suprachoroid, begin to branch just anterior to the equator, and contribute to the circulation of the iris and ciliary body. Just anterior to the equator, some branches of these vessels course down into the choroid and branch to terminate in the choriocapillaris from the ora serrata back to the equator of the eye.
In general, the larger diameter arteries of the choroid are found most proximal to the sclera, in an area referred to as the lamina fusca. These arteries continue to branch and ultimately form the extensive choriocapillaris adjacent to the acellular Bruch’s membrane located on the basal side of the RPE (
Figure 3
). The capillary network of the choriocapillaris is approximately 3–18 m m in diameter and oval shaped in the posterior eye, becoming gradually wider and longer as it moves toward the equatorial region (approximately 6–36 m m wide by 36–400 m m long). The network becomes irregular in the peripheral third of the choroid owing to the entrance and exit of arterioles and venules.
Compared to capillaries in other organs, the choriocapillary lumen are significantly larger, with a diameter of nearly
20 m m in the macular region and 18–50 m m in the periphery.
A network of collagen fibrils surrounds the choriocapillaris and provides a structural supportive framework.
From the choriocapillaris, venous collecting vessels emerge that ultimately exit the eye through the vortex veins (
Figure 1
). In addition to the choroid, the vortex veins also drain the ciliary body and iris circulation. The number of vortex veins is variable, with at least one per
Temporal
Vortex veins
Ciliary body
Iris
Long anterior ciliary artery
Fovea
Short posterior ciliary artery
Central retinal v.
Central retinal a.
Circle of Zinn
Schlemm’s canal
Short posterior ciliary artery
Long anterior ciliary artery
Vortex veins
Nasal
Figure 1 A cutaway drawing of the human eye showing the major blood vessels supplying the retina choroid and anterior segment.
The view is from a superior position over the left eye and the horizontal section passes through both the optic nerve and the fovea.
Drawing by Dave Schumick.
Developmental Anatomy of the Retinal and Choroidal Vasculature 11 eye quadrant; however, the total number per eye is usually seven, with more found on the nasal side than are found temporally. The vortex veins usually exit the sclera at the equator or up to 6 mm posterior to this location after forming an ampulla near the internal sclera. The venous branches that open into the anterior and posterior regions of the vortex venular network are oriented along the meridian and are mostly straight, while those joining on the lateral and medial sides have a circular orientation.
The vortex veins, in turn, empty into the superior and
Figure 2 A cutaway drawing along the superior–inferior axis of a left human eye through the optic nerve, showing details of the vascular supply in this location. The fovea is present on the right side of the drawing at the center of the termination of the central retinal vessels. Drawing by Dave Schumick.
Superficial capillary plexus
Deep capillary plexus
Choriocapillaris
Choroid
Fovea
Henle’s fiber layer
Photoreceptor layer
Pigmented epithelium
Bruch’s membrane
Scler a
Figure 3 A diagram showing details of the retinal and choroidal vasculature and changes that occur at the level of the human fovea. The branches from the central retinal circulation form two distinct capillary plexi within the ganglion cell layer (the superficial capillary plexus) and in the inner nuclear layer (the deep capillary plexus). These two vascular plexi end as the ganglion cell and inner nuclear layer disappear in the foveal slope. The choroid contains a dense vascular network terminating with the fenestrated choriocapillaris adjacent to Bruch’s membrane. Drawing by Dave Schumick.
12 Developmental Anatomy of the Retinal and Choroidal Vasculature inferior ophthalmic veins, which leave the orbit and enter the cavernous sinus.
Physiology
The primary function of the choroid vasculature is to provide nutrients and oxygen to the outer retina. The loss of the choriocapillaris, as occurs in central areolar choroidal sclerosis, results in atrophy of the overlying retina. The choriocapillary network is unique in that it lies in a single plane below Bruch’s membrane. Normal choroidal circulation occurs when both choroidal arterial and venous pressures are above 15–20 mm of Hg, which is the normal physiological intraocular pressure.
In addition, since the blood flow rate through the choroid is relatively high compared to other tissues and is regulated by the arterial vessel diameter, it causes relatively lower amounts of oxygen to be extracted from each milliliter of blood.
The wall of the choriocapillaris facing Bruch’s membrane is fenestrated with circular openings (fenestrae) measuring approximately 800 A choriocapillaries are unique in that they have a diaphragm covering them, unlike those seen in the renal glomerulus.
These fenestrae allow easy movement of large macromolecules into the extracapillary compartment. Fluid and macromolecules escaping from these leaky vessels percolate through Bruch’s membrane and have access to the basal side of the RPE. The passive movement of fluid and macromolecules from this leaky circulation is blocked from reaching the subretinal space (interphotoreceptor matrix) by zonula occludens junctions that form a continuous belt-like barrier near the apical border of the RPE.
Thus, the RPE is able to block the passive movement of the large molecules and fluid from the choroid, allowing the RPE to function as the outer portion of the blood retinal barrier.
Pathology
The exudative (wet form) of age-related macular degeneration (AMD) is characterized by an abnormal proliferation of the choriocapillaris with occasional invasion through
Bruch’s membrane into the subretinal space. Leakage of the fluid and/or blood often leads to retinal or RPE detachment and loss of central vision. VEGF, basic fibroblast growth factor (bFGF), and pigment epithelial-derived growth factor
(PEDF) have been postulated to play a role in the development of choroidal neovascularization (CNV). Some studies have suggested that the thickening of Bruch’s membrane that occurs with age and in AMD could result in decreased permeability. The survival factors for the choriocapillaris, such as VEGF, which are secreted basally from the RPE, could remain sequestered in Bruch’s membrane and be unable to reach the endothelial cells of the choriocapillaris.
This could potentially lead to atrophy of the choriocapillaris that is seen in dry AMD and may be the initiating event for local hypoxia, and upregulation of VEGF and CNV. Myopia is the second most common cause of CNV. Presumed ocular histoplasmosis syndrome, multiple white dot syndrome, multifocal choroiditis, punctate inner choroidopathy, birdshot chorioretinopathy, and the healing phase of choroidal ruptures are the other causes of CNV.
Hyaloid Vascular Network
Embryology
During the first gestational month, the posterior compartment of the globe contains the primary vitreous comprised of a fibrillary meshwork of ectodermal origin and vascular structures of mesodermal origin. At the 5-mm stage, the primitive dorsal ophthalmic artery sprouts off the hyaloid artery, which passes through the embryonic choroidal fissure and branches within the cavity of the primary optic vesicle. Behind the lens vesicle, some of the branches make contact with the posterior side of the developing lens
(capsula perilenticularis fibrosa), while others follow the margin of the cup and form anastomoses with confluent sinuses to form an annular vessel. The arborization of the hyaloid artery forms a dense capillary network around the posterior lens capsule (tunica vasculosa lentis, TVL) and surrounding the lens equator. In addition, capillary branches are given off that course throughout the vitreous
(vasa hyaloidea propria). The capsulopupillary vessels anastomose with the annular vessel around the rim of the optic cup and connect to the choroidal vasculature through which venous drainage occurs. By the sixth week (17–18-mm embryo), the annular vessel sends loops forward and centrally over the anterior lens surface. By the end of the third month, the anterior portion of the TVL is replaced by the pupillary membrane, which is supplied via loops from the branches of the long posterior ciliary arteries and the major arterial circle. The development of the hyaloid vasculature is almost complete at the ninth week (40 mm) stage. The venous drainage from the vessels of the anterior lens capsule and, subsequently, from the pupillary membrane and from the capsulopupillary vessels occurs through vessels that assemble into a network in the region where the ciliary body will eventually form and will anastomose and feed into the venules of the choroid.
Normally, the hyaloid vascular system begins to regress during the second month of gestation. This process begins with atrophy of the vasa hyaloidea propria, followed by the capillaries of the TVL, and, finally, the hyaloid artery (by the end of the third month). The occlusion of the regressing capillaries by macrophages appears to be a critical step for atrophy to occur. As the vascular structures regress, the primary vitreous retracts, and collagen fibers and a ground substance of hyaluronic acid are produced, forming a
Developmental Anatomy of the Retinal and Choroidal Vasculature 13 secondary vitreous. By the fifth to the sixth month of gestation, the posterior compartment is primarily composed of the secondary vitreous, and the primary vitreous is reduced to a small, central structure, the Cloquet canal, which is a thin, S -shaped structure that extends from the disk to the posterior surface of the lens.
Physiology
The hyaloid vascular system apparently supplies the nutritive requirements of both the lens and the developing retina before the acquisition of the retinal vasculature. The localization of VEGF in the TVL and papillary membrane may be responsible for fenestrae being present only in the hyaloid capillaries facing the lens. The hypoxia-inducible factor and VEGF have been postulated to play a role in the development and regression of the hyaloid. Other factors that have a part to play in regression are Wnt receptor
(Lrp5), Frizzled-4, collagen-18, Arf, Ang2, and BMP-4.
Pathology
Persistent hyperplastic primary vitreous occurs owing to the failure of the hyaloid vasculature to completely regress. The TVL, the anterior extension of the primary vitreous, is comprised of a layer of vascular channels originating from the hyaloid artery, the vasa hyaloidea propria, and the anterior ciliary vessels. The anterior part of this system is supplied by the ciliary system and the posterior part by the hyaloid artery and its branches.
The posterior system usually regresses completely by the seventh month of gestation, while the anterior part follows by the eighth month. Two clinical forms of persistent hyperplastic primary vitreous have been identified based on the vascular system that fails to regress: (1) persistent
TVL that mainly affects the anterior segment and is now termed anterior hyperplastic primary vitreous and
(2) posterior hyperplastic primary vitreous. The hallmark of posterior hyperplastic primary vitreous is the presence of a retinal fold. The lens is usually clear, but may form a cataract over time if the membranous vessels grow forward to enter the lens through the posterior capsule. Other complications include secondary angle-closure glaucoma, microophthalmia, vitreous membranes, tractional retinal detachment at the posterior pole, and a hypoplastic (underdeveloped) or dysplastic (disorganized) optic nerve head.
Patients with the anterior hyperplastic primary vitreous often have the best prognosis for visual recovery. The posterior pole is usually normal, with no evidence of a retinal fold or abnormalities in the optic nerve or macula. Patients characteristically present with the appearance of a whitish mass behind the lens (leukokoria) early in life. Occasionally, elongated ciliary processes are present and the eye is microphthalmic. Intralenticular hemorrhage can occur if the fibrovascular membrane invades the lens. Other complications include secondary angle-closure glaucoma, strabismus, and coloboma iridis.
Retinal Vascular Network
Embryology
Until the fourth month of gestation, the retina remains avascular as the hyaloid vasculature provides the nutrients to the developing retina. At the fourth month (100-mm stage), the primitive vascular mesenchyme cells near the hyaloid artery invade the nerve fiber layer. At later stages in development, the hyaloid artery regresses back to this point, which marks the posterior origin of the retinal circulation.
In the fourth month of gestation, the first retinal vessels appear when solid endothelial cords sprout from the optic nerve head to form a primitive central retinal arterial system. By the sixth month, these vessels start developing a faint lumen that occasionally contains a red blood cell. At this time, the vessels extend 1–2 mm from the optic disk and continue to migrate outward extending to the ora serrata nasally and to the equator temporally by the seventh to eighth month. Pericytes or mural cells are conspicuously absent from the vessels at this time and do not appear until
2 months after birth. The retinal vasculature achieves the adult pattern by the fifth month after birth. The relative roles of angiogenesis versus vasculogenesis in the development of the retinal vascular network are still controversial.
However, it is generally accepted that VEGF secreted in a temporal and spatial pattern by microglia and astrocytes plays a critical role in the development of the superficial and deep layers of the retinal vasculature. Platelet-derived growth factor (PDGF) produced by the neuronal cells induces the proliferation and differentiation of astrocytes, which respond to the hypoxic environment by secreting
VEGF. These cells establish a gradient of VEGF and a track for endothelial cells to follow. The hypoxia-inducible factor has been shown to be critical in the hypoxia-induced regulation of retinal vascular development. VEGF isoforms have been shown to perform highly specific functions during developmental retinal neovascularization.
Gross Anatomy
Usually, the only arterial blood supply to the inner retina is from the central retinal artery that runs along the inferior margin of the optic nerve sheath and enters the eye at the level of the optic nerve head (
Figure 2
). Within the optic nerve, the artery divides to form two major trunks and each of these divides again to form the superior nasal and temporal and the inferior nasal and temporal arteries that supply the four quadrants of the retina. The retinal venous branches are distributed in a relatively similar pattern. The major arterial and venous branches and the successive divisions of the retinal vasculature are present in the
14 Developmental Anatomy of the Retinal and Choroidal Vasculature nerve fiber layer close to the internal limiting membrane.
The retinal arterial circulation in the human eye is a terminal system with no arteriovenous anastomoses or communication with other arterial systems. Thus, the blood supply to a specific retinal quadrant comes exclusively from the specific retinal artery and vein that supply that quadrant. Any blockage in blood supply therefore results in infarction. As the large arteries extend within the retina toward the periphery, they divide to form arteries with progressively smaller diameters until they reach the ora serrata where they return and are continuous as a venous drainage system. The retinal arteries branch either dichotomously or at right angles to the original vessel. The arteries and venules generated from the retinal arteries and veins form an extensive capillary network in the inner retina as far as the external border of the inner nuclear layer. Arteriovenous crossings occur more often in the upper temporal quadrants with the vein usually lying deeper than the artery at these crossings.
Branches from the central retinal vessels dive deep into the retina forming two distinct capillary beds, one in the ganglion cell layer (superficial capillary plexus) and the other in the inner nuclear layer (deep capillary plexus).
Normally, no blood vessels from the central retinal arteries extend into the outer plexiform layer (
Figure 3
).
Thus, the photoreceptor layer of the retina is free of the blood vessels supplied by the central retinal artery. The choriocapillaris provides the blood supply to photoreceptors. Since the fovea contains only photoreceptors, this cone-rich area is free of any branches from the central retinal vessels (
Figure 3
).
In some individuals (18%), a cilioretinal artery derived from the short posterior ciliary artery (from the choroid vasculature) enters the retina around the termination of
Bruch’s membrane, usually on the temporal side of the optic nerve, and courses toward the fovea, where it ends in a capillary bed and contributes to the retinal vasculature.
In approximately 15% of eyes with a cilioretinal artery, the branches supply the macula exclusively, whereas in other individuals, they can nourish the macular region and regions of the upper or lower temporal retina.
Physiology
The rate of blood flow through the retinal circulation is approximately 1.6–1.7 ml g
–1 of retina with a mean circulation time of approximately 4.7 s. The flow rate through the retinal vessels is significantly slower than that through the choroidal vasculature.
The arteries around the optic nerve are approximately
100 m m in diameter with 18m m-thick walls. These decrease in diameter in the branched arteries located in the deeper retina to around 15 m m. The walls of the retinal arteries have the characteristics of other small muscular arteries and are composed of a single layer of endothelial cells: a subendothelial elastica, a media of smooth muscle cells, a poorly demarcated external elastic lamina, and an adventitia comprised of collagen fibrils. Near the optic disk, the arterial wall has five to seven layers of smooth muscle cells, which gradually decrease to two or three layers at the equator and to one or two layers at the periphery. These vessels continue to have the characteristics of arteries, and not arterioles, up to the periphery. The retinal arteries lose their internal elastic lamina soon after they bifurcate at the optic disk. This renders them immune from developing temporal arteritis and distinguishes them from muscular arteries of the same size in other tissues. As a compensatory mechanism, the retinal arteries have a thicker muscularis, which allows increased constriction in response to pressure and or chemical stimuli.
The major branches of the central vein close to the optic disk have a lumen of nearly 200 m m with a thin wall made up of a single layer of endothelial cells having a thin basement membrane (0.1
m m), which is continuous with the adjacent media comprised predominantly of elastic fibers, a few muscle cells, and a thin adventitia. The larger veins in the posterior wall have three to four layers of muscle cells in the media. As the retinal veins move peripherally from the optic disk, they lose the muscle cells, which are replaced by pericytes. The lack of smooth muscle cells in the venular vessel wall results in a loss of a rigid structural framework for the vessels, resulting in shape changes under conditions of sluggish blood flow
(e.g., diabetes mellitus) or increased blood viscosity (polycythemia), or with increased venous pressure (papilledema or orbital compressive syndromes).
The retinal capillary network is spread throughout the retina, diffusely distributed between the arterial and venous systems. There are three specific areas of the retina that are devoid of capillaries. The capillary network extends as far peripherally as the retinal arteries and veins up to 1.5 mm from the posterior edge of the troughs of the ora serrata (ora bays), leaving the ora serrata ridges
(ora teeth) without any retinal circulation. The 400m mwide capillary-free region centered around the fovea is another area lacking retinal capillaries. Finally, the retina adjacent to the major arteries and some veins lacks a capillary bed.
The retinal capillary wall is comprised of the endothelial cells, basement membrane, and intramural pericytes.
The retinal capillary lumen is extremely small (3.5–6 m m in diameter), requiring the circulating red blood cells to undergo contortions to pass through. Unlike the choriocapillaris, the endothelial cells of retinal capillaries are not fenestrated. The edges of endothelial cells show interdigitation and are joined by the zona occludens at their lumenal surface. The endothelial cells of the retinal arteries are linked by tight junctions, which prevent the movement of large molecules in or out of the retinal vessels. These tight junctions, in concert with the Muller
Developmental Anatomy of the Retinal and Choroidal Vasculature 15 cells and astrocytes, establish the blood–retinal barrier that prevents the passage of plasma proteins and other macromolecules in or out of the capillary system. The pericytes (also called mural cells) are embedded within the basal lamina of the retinal capillary endothelium. The pericytes are believed to play an important role in the stabilization of the retinal capillary vasculature.
Pathology
Diabetic retinopathy (maculopathy) is the leading cause of vision loss in patients with type 2 diabetes and is characterized by the hyperpermeability of retinal blood vessels, with subsequent formation of macular edema and hard exudates. Early changes in the retinal vasculature include thickening of the basement membrane, loss of pericytes, formation of microaneurysms, and increased permeability. It is generally hypothesized that these changes lead to the dysfunction of the retinal vessels, loss of vessel perfusion, hypoxia, induction of retinal
VEGF expression, and pathological neovascularization as seen in proliferative diabetic retinopathy. In severe cases, retinal detachment can occur as a result of traction caused by fibrous membrane formation. Laser photocoagulation and VEGF-blocking agents are currently being used as therapeutic approaches for this disease.
Retinopathy of prematurity is a potentially blinding disorder affecting premature infants weighing 1250 g or less and with a gestational age of less than 31 weeks. This disease is characterized by abnormal retinal vascularization and can be classified into several stages ranging from mild
(stage I), with mildly abnormal vessel growth, to severe
(stage V), with severely abnormal vessel growth and a completely detached retina. The pathophysiology of this disease has been extensively studied and several factors have been implicated. The premature birth of an infant before the retinal vasculature has extended to the periphery results in stoppage of the normal blood vessel growth that is driven by the hypoxia-mediated expression of
VEGF. This is compounded by the oxygen therapy given to alleviate the respiratory distress, which reduces VEGF expression leading to vaso-obliteration. Once the infant is taken off oxygen, there is a relative hypoxia, upregulation of VEGF, and florid abnormal neovascularization.
See also:
Angiogenesis in Inflammation; Angiogenesis in
Response to Hypoxia; Angiogenesis in the Eye; Angiogenesis in Wound Healing; Blood–Retinal Barrier; Development of the Retinal Vasculature; Vessel Regression.
Further Reading
Hogan, M. J., Alvarado, J. A., and Weddell, J. (1971).
Histology of the human eye.
Philadelphia, PA: W.B. Saunders.
Jakobiec, F. A. (1982).
Ocular anatomy, embryology and teratology.
Philadelphia, PA: Harper and Row.
Saint-Geniez, M. and D’Amore, P. A. (2004). Development and pathology of the hyaloid, choroidal and retinal vasculature.
International Journal of Developmental Biology 48: 1045–1058.
Wolff, E. (1933).
The anatomy of the eye and orbit.
Philadelphia, PA:
P. Blakiston’s and Co.