Chapter 105 - Brain and Cranial Nerve Disorders
advertisement

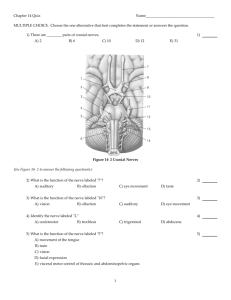
CHAPTER 105 Brain and Cranial Nerve Disorders Brian A. Stettler This chapter discusses cranial nerve problems, cerebral venous thrombosis, and multiple sclerosis—neurologic disorders that often provide significant diagnostic and therapeutic challenges in the emergency department (ED) setting (Table 105-1). TRIGEMINAL NEURALGIA Perspective Trigeminal neuralgia, or tic douloureux, is a syndrome featuring painful paroxysms in one or more distributions of the trigeminal nerve. Trigeminal neuralgia is relatively uncommon, with an annual incidence of 4 to 13 cases per 100,000 population.1,2 It is more common in women than in men, with a female-to-male ratio of 1.7 : 1. Affected persons typically are between 50 and 69 years of age, and symptoms occur more frequently on the right side of the face.3 Pathophysiology Trigeminal neuralgia is an idiopathic disorder, although significant evidence points to vascular compression of the trigeminal nerve root in many cases. This compression commonly is caused by a tortuous arterial or venous loop in the posterior fossa, an arteriovenous malformation, or rarely a tumor. In surgical case series, vascular compression of the trigeminal nerve root is found in 80 to 90% of cases.4,5 Of note, however, structural lesions are not found in all patients with trigeminal neuralgia.6 Clinical Features Trigeminal neuralgia is manifested with unilateral facial pain, typically characterized as lancinating paroxysms of pain in the lips, teeth, gums, or chin. The pain of trigeminal neuralgia is commonly associated with physical triggers such as chewing, brushing the teeth, shaving, washing or touching the affected area of the face, swallowing, or exposure to hot or cold temperature in the affected area. The maxillary and mandibular divisions of the trigeminal nerve are most commonly involved; rarely, the ophthalmic division alone is involved. Patients tend to experience the pain in clustered episodes that last a few seconds to several minutes. The attacks can occur during the day or night but rarely arise during sleep.6,7 Diagnostic Strategies A careful history and physical examination should be performed to rule out other painful facial conditions, including odontogenic infections, sinus disease, otitis media, acute glaucoma, temporomandibular joint disease, and herpes zoster. Patients who lack local pathologic findings to explain the painful syndrome require a careful neurologic examination. The presence of a neurologic deficit should prompt suspicion of a structural lesion, such as aneurysm, tumor, or other intracranial lesion (e.g., from multiple sclerosis). Of note, 2 to 4% of patients with trigeminal neuralgia also have multiple sclerosis.8 Patients with normal findings on the head and neck examination and no neurologic deficits who have episodic, unilateral facial pain associated with nonpainful triggers are likely to have trigeminal neuralgia. Management Since the 1960s the treatment of choice for trigeminal neuralgia has been the anticonvulsant medication carbamazepine. The purported effectiveness of this treatment, however, is based on uncontrolled studies, and the mechanism of action of anticonvulsant therapy for trigeminal neuralgia is unclear. The true efficacy of medical therapy is difficult to assess owing to a high rate of spontaneous remission. Nonetheless, carbamazepine appears to be an effective and well-tolerated agent for treatment of trigeminal neuralgia. The initial dosage of carbamazepine is 100 mg twice daily; this dose is then increased to three times daily after 1 week. The dose may be increased by 100 mg/day, up to a maximum of 1200 mg/day. A complete blood count and liver function studies are performed periodically in patients who are taking carbamazepine to monitor for hematologic and hepatic side effects. Additional agents that have been used for treatment of trigeminal neuralgia include phenytoin, baclofen, valproate sodium, lamotrigine, gabapentin, and levetiracetam. None of these drugs has been shown to be more effective than carbamazepine.7 Surgical management has been a therapeutic option since the 1950s. Surgical procedures include both peripheral and central procedures. Peripheral strategies include medication injection and cryotherapy techniques designed to temporarily block or permanently ablate branches of the peripheral trigeminal nerve. Although these procedures are relatively effective initially, recurrence is common. Repeated nerve blocks are not recommended because of a high risk of permanent facial anesthesia. Central procedures can be divided into percutaneous approaches and open approaches. Percutaneous destruction of the trigeminal ganglion can be done by means of radiofrequency ablation, thermal ablation, glycerol injection, or balloon microcompression. These procedures carry the risk of corneal anesthesia, oculomotor paresis, or masticatory weakness.9 Open surgical management is the surgical option of choice in many treatment centers. Open surgical procedures include 1409 1410 PART III ◆ Medicine and Surgery / Section Seven • Neurology Table 105-1 The Cranial Nerves: Normal Function and Pathologic Considerations CLINICAL FUNCTION RELEVANT TO EMERGENCY MEDICINE PATHOLOGIC FEATURES POSSIBLE CAUSES Cranial nerve I: Olfactory nerve Sense of smell Unilateral anosmia Trauma: Skull fracture or shear injury interrupting olfactory fibers traversing the cribriform plate Tumor: Frontal lobe masses compressing the nerve Cranial nerve II: Optic nerve Vision Unilateral vision loss Trauma: Traumatic optic neuropathy Tumor: Orbital compressive lesion Inflammatory: Optic neuritis (MS) Ischemic: Ischemic optic neuropathy Cranial nerve III: Oculomotor nerve Extraoculomotor function via motor fibers to levator palpebrae, superior rectus, medial rectus, inferior rectus, inferior oblique muscles Pupillary constriction via parasympathetic fibers to constrictor pupillae and ciliary muscles Ptosis caused by loss of levator palpebrae function Eye deviated laterally and down Diplopia Dilated, nonreactive pupil Loss of accommodation Trauma: Herniation of the temporal lobe through the tentorial opening, causing compression and stretch injury to the nerve Ischemic: Especially in diabetes Microvascular ischemic injury to nerve causes extraocular muscle paralysis but usually is papillary sparing (often painful) Vascular: Intracranial aneurysms may press on the nerve, leading to dysfunction Myasthenia gravis can lead to atraumatic ocular muscle palsy Cranial nerve IV: Trochlear nerve Motor supply to the superior oblique muscle Inability to move eye downward and laterally Diplopia Patients tilt head toward unaffected eye to overcome inward rotation of affected eye Trauma is the most common cause of nerve dysfunction Cranial nerve V: Trigeminal nerve Motor supply to muscles of mastication and to tensor tympani Sensory to face, scalp, oral cavity (including tongue and teeth) Partial facial anesthesia Episodic, lancinating facial pain associated with benign triggers such as chewing, brushing teeth, light touch Trauma: Facial bone fracture may injure one section, leading to area of facial anesthesia Tic douloureux Cranial nerve VI: Abducens nerve Motor supply to the lateral rectus muscle Inability to move affected eye laterally Diplopia on attempting lateral gaze Tumor: Lesions in the cerebellopontine angle Any lesion, vascular or otherwise, in the cavernous sinus may compress nerve Elevated intracranial pressure (ICP): Because of its position and long intracranial length, increased ICP from any cause may lead to injury and dysfunction of the nerve Cranial nerve VII: Facial nerve Motor supply to muscles of facial expression Parasympathetic stimulation of the lacrimal, submandibular, and sublingual glands Sensation to the ear canal and tympanic membrane Hemifacial paresis: Lower motor neuron lesion leaves entire side of face paralyzed Upper motor neuron lesion leaves forehead musculature functioning Abnormal taste Sensory deficit around ear Intolerance to sudden loud noises Lower motor neuron: Infection (viral): The likely cause of Bell’s palsy Lyme disease: The most common cause of bilateral cranial nerve VII palsy in areas where Lyme disease is endemic Bacterial infection extending from otitis media Upper motor neuron: Stroke, tumor Cranial nerve VIII: Vestibulocochlear nerve Hearing and balance Unilateral hearing loss Tinnitus Vertigo, unsteadiness Tumor: Acoustic neuroma Mimics Ménière’s disease, perilymphatic fistula Cranial nerve IX: Glossopharyngeal nerve General sensation to posterior third of tongue Taste for posterior third of tongue Motor supply to the stylopharyngeus Clinical pathology referable to the nerve in isolation is very rare Occasionally painful paroxysms beginning in the throat and radiating down the side of the neck in front of the ear but behind the mandible Brainstem lesion Glossopharyngeal neuralgia CRANIAL NERVE Chapter 105 / Brain and Cranial Nerve Disorders 1411 Table 105-1 The Cranial Nerves: Normal Function and Pathologic Considerations—cont’d CRANIAL NERVE CLINICAL FUNCTION RELEVANT TO EMERGENCY MEDICINE PATHOLOGIC FEATURES POSSIBLE CAUSES Cranial nerve X: Vagus nerve Motor to striated muscles and muscles of the pharynx, larynx, and tensor (veli) palatini Motor to smooth muscles and glands of the pharynx, larynx, thoracic and abdominal viscera Sensory from larynx, trachea, esophagus, thoracic and abdominal viscera Unilateral loss of palatal elevation: Patients complain that on drinking liquids, the fluid refluxes through the nose Unilateral vocal cord paralysis: Hoarse voice Brainstem lesion Injury to the recurrent laryngeal nerve during surgery Cranial nerve XI: Spinal accessory nerve Motor supply to the sternocleidomastoid and trapezius muscles Downward and lateral rotation of the scapula and shoulder drop Trauma to the nerve Cranial nerve XII: Hypoglossal nerve Motor supply to the intrinsic and extrinsic muscles of the tongue Tongue deviations: Upper motor neuron lesion causes the tongue to deviate toward the opposite side Lower motor neuron lesion causes the tongue to deviate toward the side of the lesion, and the affected side atrophies over time Stroke or tumor can cause upper motor neuron lesion Amyotrophic lateral sclerosis can cause bilateral lower motor neuron lesion with atrophy Metastatic disease to the skull base may involve the nerve microvascular decompression of the nerve with or without partial ablation. Although the open microvascular decompression procedure has proved to be effective, with pain relief achieved in 80 to 95% of patients, the surgery is associated with the risk of significant complications, including hearing loss, facial anesthesia, cerebrospinal fluid (CSF) leak, brainstem or cerebellar injury, headaches, meningitis, and death.10,11 Gamma Knife radiosurgery, a minimally invasive, precision-directed stereotactic radiosurgery, also has been associated with good outcomes. This highly specialized technique requires extremely sophisticated stereotactic radiofrequency equipment and is available only in specialized centers, but in many cases it has similar results for pain relief without the morbidity associated with open procedures in patients who might otherwise be a surgical risk.12-14 Disposition Patients with suspected trigeminal neuralgia should be referred for specialty evaluation. Patients with a neurologic deficit require urgent imaging studies, typically magnetic resonance imaging (MRI), to rule out a mass or vascular abnormality. FACIAL NERVE PARALYSIS Perspective The acute onset of facial nerve paralysis often will prompt an ED visit. Fortunately, early diagnosis and therapy may improve the patient’s chance for recovery of function of the facial nerve. Facial nerve paralysis of acute onset affects approximately 20 to 25 persons per 100,000 population per year, without geographic, gender, or race predilection.15,16 Principles of Disease The facial nerve innervates the muscles of facial expression and the muscles of the scalp and external ear in addition to the buccinator, platysma, stapedius, stylohyoid, and posterior belly of the digastric muscles. The sensory portion of the nerve supplies the anterior two thirds of the tongue with taste and sensation to portions of the external auditory meatus, soft palate, and adjacent pharynx. The parasympathetic portion supplies secretomotor fibers for the submandibular, sublingual, lacrimal, nasal, and palatine glands.17 The nerve originates from the pontomedullary junction of the brainstem and enters the internal auditory meatus with cranial nerve VIII. Within the temporal bone, the facial nerve has four major branches: the greater and lesser superficial petrosal nerves, the nerve to the stapedius muscle, and the chorda tympani. The facial nerve exits the temporal bone at the stylomastoid foramen and then enters the parotid gland, where it divides to supply the muscles of facial expression.17,18 Pathophysiology The three main causes of facial nerve paralysis that are relevant to emergency medicine are grouped into infectious, traumatic, and neoplastic. Infection Bell’s Palsy. Bell’s palsy, also commonly called idiopathic facial paralysis, has long been postulated to have a viral cause. This disease entity is characterized by an abrupt onset of a lower motor neuron paresis that can progress during 1 to 7 days to complete paralysis. A prodromal illness is described by 60% of patients. Symptoms and signs frequently associated with the facial paresis include ear pain, perception of sensory change on the involved side of the face, decreased tearing, overflow of tears on the cheek (epiphora), abnormally acute hearing (hyperacusis), and impairment or perversion of taste (dysgeusia).19 Treatment approaches can be medical or surgical. The primary medical therapies for Bell’s palsy center on reducing inflammatory changes to the nerve with corticosteroids and treating the presumed viral cause. If these therapies are unsuccessful, surgical decompression may be considered. Available evidence now strongly favors the use of corticosteroids for the treatment of Bell’s palsy, and earlier treatment is associated with better efficacy and outcomes.20-24 The rationale for this application of steroid therapy is that edema of the nerve, confined within the facial canal, is thought to cause or contribute to the nerve injury. On the basis of this theory, most experts currently recommend a course of prednisone with an initial dose of 1 mg/kg per day for 7 to 10 days, with or without a short 1412 PART III ◆ Medicine and Surgery / Section Seven • Neurology taper.15,18,25,26 The most definitive randomized, double-blind, placebo-controlled trial involving 496 patients showed an improvement in complete recovery of facial nerve function at 3 months from 64% with placebo to 83% with the use of prednisolone in a dose of 25 mg by mouth twice daily.27 Therapy should be started as soon as possible, ideally within the first 24 hours, but it is still recommended for patients without contraindications who seek treatment within 1 week of symptom onset.25 A number of studies have supported the contention that Bell’s palsy may be caused by herpes virus infection. One study demonstrated herpes simplex virus type 1 DNA in the endoneurial tissue of 11 of 14 patients with Bell’s palsy but not in control subjects.28 In a trial of prednisone and acyclovir in 99 patients, patients treated with prednisone and acyclovir had a more favorable recovery than that observed in patients receiving prednisone alone.29 A study of 296 patients with Bell’s palsy treated with valacyclovir or placebo in addition to a fixed dose of prednisolone found significant benefit to the addition of valacyclovir, particularly in the setting of severe palsy or in those treated within 24 hours of symptom onset.30 Other studies have found conflicting results. Despite a lack of overwhelming evidence, the addition of an antiviral agent should be considered in the treatment of Bell’s palsy, especially with severe loss of function. The most commonly recommended antiviral regimen is valacyclovir, 1000 mg orally two times daily for 10 days. Valacyclovir and famciclovir have better oral absorption, are better tolerated, and are dosed less frequently, resulting in higher compliance than with acyclovir treatment.18,25,26,28,31 As with steroid therapy, although earlier treatment is preferred, treatment should be considered for patients presenting within 1 week of symptom onset. Ramsay Hunt Syndrome. Ramsay Hunt syndrome (herpes zoster oticus) is characterized by unilateral facial paralysis, a herpetiform vesicular eruption, and vestibulocochlear dysfunction. The vesicular eruption may occur on the pinna, external auditory canal, tympanic membrane, soft palate, oral cavity, face, and neck as far down as the shoulder. The pain is considerably more severe than that associated with Bell’s palsy, and it frequently is out of proportion to physical findings. In addition, outcomes are worse than with Bell’s palsy, with a lower incidence of complete facial recovery and the possibility of sensorineural hearing loss. Therapy is similar to that for Bell’s palsy. Both prednisone and antiviral therapy for 7 to 10 days are advocated.18,32,33 Lyme Disease. Lyme disease is the most frequent vector-borne infection in the United States. It is caused by the spirochete Borrelia burgdorferi and is spread by the bite of Ixodes genus ticks. Neurologic manifestations can arise in any phase of the disease, and the incidence of facial palsy in patients with neurologic involvement is 35 to 51%. In regions in which Lyme disease is endemic, it has been shown to be the leading cause of facial paralysis in children, responsible for half of all pediatric cases of facial nerve paralysis.34,35 Bilateral facial nerve paralysis is rare but can occur with systemic infections. The two diseases most commonly associated with bilateral simultaneous onset of facial paralysis are Lyme disease and infectious mononucleosis. Bilateral facial paralysis should be considered to be a manifestation of Lyme disease until further testing excludes this diagnosis.26,34-36 The evaluation and treatment of Lyme disease are discussed in Chapter 134. Bacterial Infections. Facial paralysis can be caused by acute bacterial infections of the middle ear, mastoid, or external auditory canal. In the pre-antibiotic era, facial paralysis was associated with acute otitis media in approximately 2% of cases; today, however, it occurs in only 0.2% of cases. Treatment consists of intravenous antibiotics and myringotomy for decompression. Malignant otitis externa can be associated with facial paralysis. This disease entity is most commonly seen in immunocompromised patients and usually is caused by Pseudomonas infection. Treatment involves prolonged intravenous antipseudomonal antibiotic therapy and may require surgical débridement.26,37 Trauma In patients with head trauma, the facial nerve is the most commonly injured cranial nerve. The cause generally is a temporal bone fracture with nerve transection. Surgical exploration is warranted if there is firm evidence that the nerve has been transected, indicated by a sudden onset of complete unilateral facial paralysis, loss of electrical activity, and evidence of a displaced fracture involving the facial canal. Neoplasm Tumors of the facial nerve itself or tumors anywhere along the course of the facial nerve that invade or compress the nerve may lead to facial paralysis. The course is typically progressive for at least 3 weeks. A sudden onset of paralysis, however, does not rule out an underlying tumor because facial paralysis secondary to a neoplasm is of sudden onset in approximately 25% of cases.38 A neoplastic cause should be suspected in patients who suffer from recurrent ipsilateral facial paralysis, significant pain, prolonged symptoms, or any other concomitant cranial nerve abnormality. Clinical Features and Differential Considerations The medical history in patients with facial paralysis focuses on onset of the paralysis, concentrating on timing and rapidity of onset and associated signs and symptoms. A rapid onset of facial paralysis with dysgeusia and hyperacusis preceded by a viral prodrome is suggestive of Bell’s palsy. A history of recurrent ipsilateral paralysis or slow progression of symptoms is more characteristic of a tumor. Associated cranial nerve abnormalities, although occasionally seen with Bell’s palsy, also point to the possibility of a tumor or ischemic insult. The Ramsay Hunt syndrome causes significant pain and a vesicular rash, although the rash may follow the facial paresis by a few days. Significant anatomic abnormalities on visual or otoscopic inspection of the ipsilateral ear will be found with bacterial otitis media and otitis externa. Finally, systemic symptoms or bilateral facial paresis, especially in endemic areas, should raise the possibility of Lyme disease. Diagnostic Strategies The diagnostic workup of acute facial nerve paresis is based on whether the clinical picture is suggestive of a disease process other than Bell’s palsy. If the clinical history is classic for Bell’s palsy, no imaging or laboratory studies are required. Of note, any history of possible exposure warrants serologic evaluation for Lyme disease. Although outpatient testing including electroneurography may ultimately be performed, this usually is not part of the initial evaluation. The presence of a “central” seventh nerve paralysis (upper face sparing) should prompt imaging with computed tomography (CT) or MRI, and consideration should be given to the possibility of an acute stroke or other hemispheric lesion. History or physical examination findings suggestive of a possible tumor require imaging to rule out a neoplasm. The study of choice will depend on the institution and preferences of the consultant. Disposition Most patients who have a seventh nerve paralysis will have a clinical diagnosis of Bell’s palsy and may be discharged with referral Chapter 105 / Brain and Cranial Nerve Disorders 1413 for short-term follow-up. Patients with a possible hemispheric process, such as stroke or tumor, require further evaluation and usually hospitalization. Patients thought to have Lyme disease require immediate initiation of appropriate antibiotic therapy. In patients with a peripheral facial nerve paralysis, the ipsilateral eye should be patched, and consideration should be given to ophthalmologic follow-up because there is a high rate of corneal abrasions and corneal dryness associated with the inability to blink properly or to close the eye completely. VESTIBULAR SCHWANNOMA Perspective Vestibular schwannoma, formally referred to as acoustic neuroma, is a rare but important cause of sensorineural hearing loss. The annual incidence of vestibular schwannoma is 1 case per 100,000 population, with a mean age at the time of detection of 46 to 58 years.39 The female-to-male ratio is 1.5 : 1. Vestibular schwannoma is rarely bilateral, occurring in this form in appro­ ximately 5% of cases and generally associated with type 2 neurofibromatosis. Although histologically benign, vestibular schwannoma can cause neurologic damage by direct compression on the eighth cranial nerve and the other structures in the cerebellopontine angle.40 Principles of Disease Vestibular schwannoma arises from the Schwann cells covering the vestibular branch of the eighth cranial nerve as it passes through the internal auditory canal. The tumor may compress the cochlear (acoustic) branch of the eighth cranial nerve, causing hearing loss, tinnitus, and dysequilibrium. Continued growth of the tumor may result in compression of structures in the cerebellopontine angle, where the facial and trigeminal nerves may be compressed and damaged. Larger tumors may further encroach on the brainstem and if large enough may compress the fourth ventricle, ultimately resulting in signs of increased intracranial pressure (ICP).41 Clinical Features Asymmetrical sensorineural hearing loss is the hallmark of vestibular schwannoma. Up to 15% of patients with this tumor, however, will have normal results on audiometry. These patients typically have symptoms such as unilateral tinnitus, imbalance, headache, fullness in the ear, otalgia, and facial nerve weakness. Thus, patients with asymmetrical symptoms should be further evaluated for vestibular schwannoma even with normal findings on audiometry.42 Vestibular schwannomas are extremely slow-growing tumors, averaging an approximately 1-mm increase per year, although many do not grow at all on serial examinations.43 Symptom onset is therefore generally gradual. In one series of 126 cases, the average time from symptom onset to discovery of a vestibular schwannoma was approximately 4 years.44 Diagnostic Strategies When vestibular schwannoma is suspected, the patient is evaluated by audiometry or gadolinium-enhanced MRI. This imaging technique is extremely sensitive and has led to earlier diagnosis and a decrease in mean size at detection of vestibular schwannoma. CT lacks the necessary sensitivity in the posterior cranial fossa to reliably rule out the presence of vestibular schwannoma. The smaller the tumor at the time of diagnosis, the more options there are for therapy and the better the potential prognosis.40 Differential Considerations A majority of disease entities included in the differential diagnosis for vestibular schwannoma cause symmetrical sensorineural hearing loss. Asymmetrical sensorineural hearing loss has few causes other than vestibular schwannoma. Ménière’s disease may present a diagnostic dilemma because it can be asymmetrical. Ménière’s disease may be differentiated from vestibular schwannoma in that the tinnitus of Ménière’s disease usually is intermittent, whereas the tinnitus of vestibular schwannoma typically is continuous. In addition, patients with Ménière’s disease typically describe true vertigo, whereas patients with a vestibular schwannoma are more likely to describe imbalance or dysequilibrium. Vestibular schwannomas account for 80% of all cerebellopontine angle tumors. Among all other lesions, meningioma is the most common. Meningiomas more frequently cause symptoms of facial palsy or trigeminal nerve abnormality. Of note, however, considerable similarity between the clinical picture of a meningioma and that of vestibular schwannoma in the cerebellopontine angle has been described.45 Management Vestibular schwannoma may be removed surgically or ablated with stereotactic radiation therapy. In general, tumors larger than 3 cm are recommended for microsurgery because radiation treatments, such as with the Gamma Knife or linear accelerator, are less effective for local control and growth arrest in larger masses. Smaller tumors are amenable to use of stereotactic radiation therapy, which has greater salvage rates of facial nerve function and hearing.46,47 Stereotactic radiation therapy generally has good long-term outcomes of local growth arrest, with nerve salvage approaching 90% or greater. Injuries to the trigeminal, facial, and acoustic nerves and to the cerebellum are possible complications of both procedures. In patients who are minimally symptomatic with small tumors, serial monitoring with MRI is a viable nonsurgical option. All patients should be evaluated by a specialist in the evaluation and treatment of vestibular schwannoma because smaller tumor size at detection is associated with a better longterm outcome.39,43 Disposition Patients with suspected acoustic neuroma should be referred for audiometry or MRI and evaluation by a specialist in either otolaryngology or neurosurgery. DIABETIC CRANIAL MONONEUROPATHY Perspective Cranial mononeuropathies occur uncommonly, usually are a complication of diabetes, and most often affect the extraocular muscles. The oculomotor nerve is most commonly affected, followed in order by the trochlear and abducens nerves. In one large series in Japan, the incidence of cranial nerve palsies was 1.0% among diabetics and 0.1% among nondiabetics.48,49 Whereas ophthalmoplegia appears to be closely related to diabetes, facial palsy is less strongly correlated with this disease.48,50 Principles of Disease The pathologic basis of diabetic mononeuropathy appears to be ischemia of the affected cranial nerve caused by occlusion of an intraneural nutrient artery serving the nerve. This occlusion leads 1414 PART III ◆ Medicine and Surgery / Section Seven • Neurology to injury located primarily in the center of the nerve because the core fibers are more dependent on the supply from such nutrient arteries. The peripheral fibers are less affected because they also are supplied by collateral vessels. In the oculomotor nerve, the preservation of the circumferentially located parasympathetic fibers explains the pupillary sparing that usually is found in this syndrome. In two studies, the microvascular changes in the intraneural arteries that lead to occlusion were noted in diabetic patients but absent in nondiabetics.51,52 Clinical Features Patients typically describe acute onset of unilateral retro-ocular and supraorbital pain, diplopia, and ptosis.49 The physical manifestations of a third cranial nerve palsy include the inability to move the eye superiorly and medially, accompanied by ptosis. The pupillary light reflex usually is present. Although it is a less common finding, the fourth and sixth cranial nerves may be affected. Patients with a fourth cranial nerve palsy are unable to move the eye inferolaterally, and those with a sixth cranial nerve palsy are unable to move the eye laterally. Because of the long intracranial course of the sixth nerve, a patient with an isolated sixth nerve palsy should be evaluated for an intracranial lesion or increased ICP.53 Differential Considerations Evaluation of cranial nerve dysfunction requires a thorough history and physical examination and cranial imaging, usually with MRI. Diabetic mononeuropathy should be considered a diagnosis of exclusion. Considerations in the differential diagnosis include trauma, tumor, vertebrobasilar ischemia, aneurysm, and hemorrhage into the brainstem.54 Management Treatment consists of patching of the affected eye and administration of analgesics and antiplatelet therapy. The prognosis is good. If the neuropathy does not begin to resolve within 3 to 6 months or if more than one nerve is affected, another cause should be sought. Complete resolution is expected within the first year. Antioxidant preparations, including α-lipoic acid, have been used therapeutically and have not shown harm, but such agents have yet to be shown to have convincing clinical effect.55 CEREBRAL VENOUS THROMBOSIS Perspective No exhaustive studies of the epidemiology of cerebral venous thrombosis (CVT) have been performed. In case series, the median patient age is 38 years; women represent 60 to 75% of those diagnosed.56,57 Principles of Disease Cerebral blood is drained by several major veins that lead into the dural sinuses. The major dural sinuses are the superior sagittal sinus, the inferior sagittal sinus, the straight sinus, the lateral sinuses, and the sigmoid sinuses. The variability in symptoms and signs in patients who present with CVT stems from differences in thrombus location and acuity of thrombus formation. Symptoms of intracranial hypertension, especially headache, are present in most patients with sinus thrombosis, whereas those with thrombosis of the cerebral veins are thought to be more prone to hemorrhagic infarction and localizing neurologic deficits.58 As with venous thrombosis in other locations, multiple causes and predisposing factors for CVT are recognized. Underlying causes are often divided into infectious and noninfectious categories. Infectious causes include local infections, such as sinusitis, otitis media, facial cellulitis, and systemic infections. Noninfectious causes include direct injury to the cerebral venous system from trauma, surgery, dehydration, or any other condition that may predispose the patient to development of a hypercoagulable state, including the presence of a malignant neoplasm or the use of oral contraceptive agents.59 Clinical Features The symptoms and signs associated with CVT are varied. Headache is the primary feature of CVT in 74 to 92% of affected patients.59,60 Papilledema is noted in 28 to 45% of cases.57,60,61 Lethargy, decreased level of consciousness, or mental status changes may be noted. Seizures occur in 35 to 50% of patients in the acute phase.57,59,61,62 In addition to the location and acuity of thrombosis formation, a patient’s symptom onset will vary in accordance with the extent of collateral vessel growth in the venous territory. Early thrombotic changes may be well compensated for by the collateral venous drainage. Symptoms will appear only when the compensation for venous thrombosis is no longer sufficient or when hemorrhagic infarction occurs. Variability in collateralization between patients also adds to the variability and time course of symptoms. Two national and international observational studies documented an average time from symptom onset to diagnosis of 7 days, reflecting the difficulty in diagnosis of this rare disease entity.57,61,63 The reported incidence of focal neurologic signs, including seizures, on clinical examination varies widely between series, ranging from 25 to 71%.59,60 Because of the broad spectrum of possible clinical features, the diagnosis of CVT may be difficult but should be a consideration in any patient with unexplained headache, especially in combination with focal neurologic deficit, papilledema, or seizures. Diagnostic Strategies Cerebral angiography no longer plays a significant role in the diagnosis of CVT. Both MRI and CT scan with venous-phase imaging have been evaluated as both primary and definitive imaging modalities for the diagnosis of CVT. CT scanning is useful in the initial workup of the patient with possible CVT, but non– contrast-enhanced CT is neither sensitive nor specific enough to reliably confirm or exclude the diagnosis. Findings on CT that are consistent with CVT include hyperdensity of a thrombosed sinus or deep vein (referred to as the cord sign or attenuated vein sign, respectively), brain edema, and hemorrhage secondary to venous congestion. Whereas non–contrast-enhanced CT in the diagnosis of CVT has been evaluated only in case series, the published sensitivity and specificity typically range from 65 to 100% when it is evaluated against MRI as the “gold standard.”64 Similar to CT scanning, MRI also can demonstrate local changes secondary to venous congestion, such as brain edema and hemorrhage. In addition, MRI can demonstrate the possibility of CVT by the lack of a “flow void.” On conventional MRI, a flow void indicates the presence of moving blood within the sinus, whereas the absence of a flow void indicates a possible thrombus. Diagnostic accuracy, however, is greatly improved through use of magnetic resonance venography (MRV). This technique takes advantage of the MRI signal characteristics of flowing blood to create images of venous structures. Combination of these imaging techniques further enhances diagnostic accuracy. For imaging of a particular dural sinus, presence of the sinus on conventional MRI and lack of flow on MRV are diagnostic of a sinus thrombosis. This Chapter 105 / Brain and Cranial Nerve Disorders 1415 combined approach has diagnostic sensitivity similar to that of conventional angiography.59,65 Several studies show similar sensitivity between MRV and CT venography for the diagnosis of CVT when the CT study is performed on a multidetector row CT scanner. These studies, involving several hundred patients, showed sensitivity of CT venography for CVT that approached 100% and was comparable to that of MRV both in sensitivity and in inter-rater reliablity.66-69 The sensitivity of CT venography performed by scanners that do not use multidetector row technology is unknown. Several small studies have attempted to evaluate the usefulness of the D-dimer assay as a screening tool to exclude CVT, particularly when MRI or CT venography is not available. Although the reported sensitivity rates are fair at 83 to 100%, larger prospective studies need to be done to further define the role of D-dimer in the evaluation of CVT because several case reports have noted normal D-dimer levels in the setting of documented CVT.70-74 In general, although a normal D-dimer level does not exclude the diagnosis of CVT, it does appear to make this diagnosis much less likely, particularly in a patient with symptoms of less than 2 weeks in duration. Differential Considerations Considerations in the differential diagnosis of CVT include the conditions that cause patients to present with the new onset of neurologic deficits, alteration in consciousness, or severe headache. A diagnosis of CVT should be considered in a patient with such symptoms when the etiology is unclear, particularly when there is the possibility of a hypercoagulable state and when the head CT scan is normal in appearance or shows subtle signs of CVT. Management CVT is a relatively rare disease, and controlled studies evaluating its treatment are lacking. Current therapeutic consensus strongly recommends systemic anticoagulation with low-molecular-weight heparin (LMWH) or unfractionated heparin to prevent further clot formation and to promote recanalization, even in patients with intracranial hemorrhage on initial imaging.59,60,74,75 In one placebo-controlled randomized trial comprising only 20 patients, anticoagulation with unfractionated heparin demonstrated benefit, even in patients with evidence of intracranial hemorrhage on the pretreatment CT scan.76 A registry comparing outcomes of patients treated with unfractionated heparin compared with LMWH found more benefit in the LMWH group, although the effect was modest.77 Two large observational trials also showed improvement in modified Rankin scale at follow-up in the anticoagulated groups, although the trials were not randomized.57,61 Despite a paucity of randomized controlled trials, expert opinion favors anticoagulation in all groups unless another contraindication is present.78 Catheter-based intervention with thrombolysis has been attempted in multiple case series with use of either urokinase or tissue plasminogen activator. Thrombolysis was shown to be relatively safe and relatively successful in very small case series.75 In one nonrandomized study of 40 patients, 20 received systemic heparin and 20 received catheter-based infusion of urokinase followed by systemic heparin. Despite initially worse neurologic function in the thrombolysis group, a significant difference in neurologic function favoring thrombolysis was observed at discharge.79 This promising therapy is typically considered only for patients with symptoms of decreased level of consciousness, elevated ICP, or rapid deterioration on neurologic examination. Disposition All patients with suspected CVT should be admitted to a unit capable of providing a high level of care with neurologic consultation. Patients should be anticoagulated if no contraindication exists, and catheter-based thrombolysis should be considered in patients with depressed mental status or focal findings on neurologic examination. MULTIPLE SCLEROSIS Perspective Multiple sclerosis (MS) is an inflammatory disease that affects the central nervous system (CNS). Although the exact etiology remains uncertain, the pathologic manifestation of this inflam­ matory disease is a demyelination of discrete regions (plaques) within the CNS with a relative sparing of axons. The clinical picture is highly variable but is classically characterized by episodes of neurologic dysfunction that evolve in days and resolve during weeks. MS has an overall prevalence in the United States of 0.1%. The peak age at onset is 25 to 30 years; women are slightly younger than men at onset. The incidence in women exceeds that of men by a ratio of 1.8 : 1. The worldwide prevalence is greatest in the United Kingdom, Scandinavia, and North America. Epidemiologic studies indicate that both genetic and environmental factors are associated with an increased incidence of this disease. MS has a 30% concordance rate between monozygotic twins, and 20% of patients with MS have at least one affected relative. MS is more common in temperate climates. It is rare between 23 degrees north and south latitudes but has a rising incidence above and below 50 degrees north and south latitudes, respectively. Although no exact environmental factor has been identified, if a person emigrates from an area of high prevalence to an area of low prevalence before the age of 20 years, the risk is diminished. MS is rare in Africans and Asians, but African Americans have a higher incidence than their relatives who remain in Africa.80 In addition, reports of clusters or mini-epidemics support environmental factors. Thus, an environmental cause superimposed on genetic susceptibility appears to be a likely etiologic scenario.81,82 Principles of Disease MS is considered to be an organ-specific autoimmune disease. One theory proposes that genetic factors interact with an environmental trigger or infection to establish pathologically autoreactive T cells in the CNS. After a long and variable latency period (typically 10 to 20 years), a systemic trigger, such as a viral infection or superantigen, activates these T cells. The activated T cells, on reexposure to the autoantigen, initiate the inflammatory response. This sets off a complex immunologic cascade that leads to the demyelination characteristic of MS. This demyelination process releases CNS antigens that are hypothesized to initiate further episodes of autoimmune-induced inflammation. The mechanisms underlying this autoimmunity in MS are unknown.83 Clinical Features The clinical picture in MS is one of marked heterogeneity. The classic clinical syndrome consists of recurring episodes of neurologic symptoms that rapidly evolve during days and slowly resolve. Variability occurs in age at onset, location of CNS lesions, frequency and severity of relapses, and degree and time course of progression. The clinical features of MS can be divided into areas of specific CNS impairment: cognition; cranial nerves; motor pathways; 1416 PART III ◆ Medicine and Surgery / Section Seven • Neurology sensory pathways; cerebellar pathways; and bowel, bladder, and sexual dysfunction.80 Patients with MS have frequent complaints of poor memory, distractibility, and decreased capacity for sustained mental effort. Formal neuropsychological testing suggests that cognitive involvement is common and underreported. Specifically, neuropsychological testing has shown that 43 to 65% of patients with MS have some degree of cognitive impairment.84,85 Of note, a correlation has been found between the MRI-based total lesion load and presence of cognitive impairment.86 Cranial nerve dysfunction is common in MS. The most common associated cranial nerve abnormality is optic neuritis, a unilateral syndrome characterized by pain in the eye and a variable degree of visual loss affecting primarily central vision. Within 2 years of an attack of optic neuritis, the risk of MS is approximately 20%, and within 15 years, it is approximately 45 to 80%.87,88 Optic neuritis often is the first symptom of MS.89,90 As a result of lesions in the vestibulo-ocular connections, the oculomotor pathways also may be affected. The deficit may be manifested as diplopia or nystagmus. The nystagmus may be severe enough that the patient may complain of oscillopsia (a subjective oscillation of objects in the visual field). Cranial nerve impairment also may include impairment of facial sensation, which is relatively common. Unilateral facial paresis also may occur. In addition, the occurrence of trigeminal neuralgia in a young person may be an early sign of MS. Motor pathways also are commonly involved. Specifically, corticospinal tract dysfunction is common in patients with MS. Paraparesis or paraplegia occurs with greater frequency than upper extremity lesions owing to the common occurrence of lesions in the motor tracts of the spinal cord. In patients with significant motor weakness, spasms of the legs and trunk may occur on attempts to stand from a seated position. This dysfunction is manifested on physical examination as spasticity that typically is worse in the legs than in the arms. The deep tendon reflexes are markedly exaggerated, and sustained clonus may be demonstrated. Although these symptoms frequently are bilateral, they generally are asymmetrical.80 Sensory manifestations are a frequent initial feature of MS and will be present in nearly all patients at some point during the course of the disease. Sensory symptoms are commonly described as numbness, tingling, “pins and needles” paresthesias, coldness, or a sensation of swelling of the limbs or trunk.80 Impairment of the cerebellar pathway results in significant gait imbalance, difficulty with coordinated actions, and dysarthria. Physical examination reveals the typical features of cerebellar dysfunction, including dysmetria, dysdiadochokinesis (an impairment of rapid alternating movements), breakdown in the ability to perform complex movements, intention tremor in the limbs and head, truncal ataxia, and dysarthria.80 Impairment of bowel, bladder, and sexual function also is common. The extent of sphincter and sexual dysfunction usually parallels the motor impairment in the lower extremities. Urinary frequency may progress to urinary incontinence as the disease advances. An atonic bladder may develop, which empties by simple overflow and often is associated with the loss of perception of bladder fullness and with anal and genital hypoesthesia. Constipation becomes common in time, and almost all patients with paraplegia require special measures to maintain effective bowel habits. Sexual dysfunction, although frequently overlooked, is common in MS. Approximately 50% of patients become completely sexually inactive as a result of this disease.80 Diagnostic Strategies Although no laboratory tests are diagnostic for MS, one clinical feature remains unique to this disease: Uhthoff ’s phenomenon, temporary worsening of current or preexisting signs or symptoms of MS secondary to small increases in the patient’s body temperature. Accordingly, exercise, a hot bath, exposure to a warm environment, or fever can bring about Uhthoff ’s phenomenon. This phenomenon reflects subclinical demyelination or preexisting injury to nerves without obvious significant clinical involvement before heat exposure or temperature elevation.80 MS is described as a relapsing-remitting disorder with symptoms that fluctuate over time. Therefore, the clinical diagnosis rests on occurrence of at least two clinical episodes with different neurologic symptoms at different times. Findings on CSF analysis are abnormal in 90% of the cases. Fifty percent of patients will have pleocytosis, with more than five lymphocytes per high-power field in the CSF. Approximately 70% of patients will have an elevated gamma globulin level, with immunoglobulin G (IgG) ranging from 10 to 30% of the CSF total protein. Electrophoresis of the CSF demonstrates oligoclonal bands of IgG in 85 to 95% of patients who carry a diagnosis of MS; however, oligoclonal bands of IgG also are seen with neurosyphilis, fungal meningitis, and other CNS infections. Lumbar puncture is recommended for patients with suspected MS, but mass lesions and elevated ICP should be ruled out before lumbar puncture is attempted.91 The initial imaging test to aid in the diagnosis of MS is gadolinium-enhanced MRI. MRI is a sensitive test for the detection of lesions consistent with MS and also is useful to assess disease severity.92 The lesions of MS typically appear hyperintense, or bright white, on T2-weighted or fluid-attenuated inversion recovery (FLAIR) MRI studies. Lesions usually are multiple and commonly are found in the periventricular white matter.93 In patients with an initial neurologic event consistent with CNS demyelination and an MRI cranial study showing multiple white matter lesions, the 5-year risk for development of MS is 60%. Patients with similar clinical syndromes and a normal MRI appearance have less than a 5% 5-year risk.94 Differential Considerations Other diseases that affect the CNS white matter may be clinically and radiographically similar to MS. Considerable care must be taken to exclude these disease processes before a diagnosis is made. These include CNS tumors (especially lymphomas and gliomas), spinal cord compression, vasculitides, Behçet’s disease, neuro­ sarcoidosis, postinfectious and postvaccinal encephalomyelitis, human immunodeficiency virus (HIV) encephalopathy, Lyme disease, and vitamin B12 deficiency. Management Management of patients with MS has essentially three aspects: (1) therapies aimed at halting the progression of the disease, (2) treatment of acute exacerbations, and (3) therapies designed to modify complications. Therapies aimed at halting disease progress are based primarily on the use of either interferon-β or glatiramer acetate. The interferons are a group of natural compounds with antiviral and immunomodulatory actions used in therapy for MS. Side effects of the agents interferon-β1a and interferon-β1b include influenzalike symptoms, depression, anxiety, and confusion. In one study, 560 patients with MS were randomly assigned to receive subcutaneous interferon-β1a or placebo (n = 187) three times a week for 2 years.95 The relapse rate was significantly lower at 1 and 2 years with interferon-β1a than with placebo. The time to first relapse was prolonged significantly and the accumulation of brain lesions on MRI was lower in the treatment group than in the placebo group. The investigators concluded that subcutaneous interferon-β1a is a well-tolerated and effective treatment of Chapter 105 / Brain and Cranial Nerve Disorders 1417 relapsing-remitting MS in terms of relapse rate, defined disability, and all MRI outcome measures.81 Interferon-β also has been shown to retard progression to clinically definite MS and to decrease the total number of brain lesions seen on subsequent MRI studies in patients who have their first demyelinating episode with MRI abnormalities at initial presentation.96-99 This finding highlights the importance of early evaluation and treatment. Glatiramer acetate also has successfully been used in the treatment of MS. This agent is a mixture of synthetic polypeptides designed to mimic myelin basic protein. The mechanism of action by which glatiramer acetate exerts its effect is unknown, but it is thought to modify the immune processes responsible for the pathogenesis of MS. In one study, 251 patients with relapsingremitting MS were randomized to receive daily subcutaneous injections of glatiramer acetate (previously called copolymer 1) or placebo for 24 months. Patients receiving glatiramer acetate experienced significantly fewer relapses and were more likely to demonstrate neurologic improvement, whereas those receiving placebo were more likely to worsen. This drug generally is well tolerated.100 Glatiramer acetate has also been shown to slow the progression to clinically definite MS after a first clinical demyelinating episode.101 Current recommendations for management of relapsingremitting MS are to initiate treatment with interferon-β or glatiramer acetate. Such regimens have been demonstrated to decrease the volume of plaques seen on MRI and to diminish relapses.83 The use of newer disease-modifying agents, such as fingolimod, cladribine, and natalizumab, has shown promise in clinical trials, but each has significant side effect profiles, and appropriate patient selection is still underway.102-107 At this point, each of these agents is considered second line for severe or refractory patients. Acute exacerbations of MS also should be targets for therapy. Although most such episodes will resolve without therapy, steroids have been demonstrated to diminish the duration of acute exacerbations. More than 85% of patients with relapsing-remitting MS show improvement with intravenous methylprednisolone. Intravenous steroids have been shown in controlled trials to speed the recovery from the visual loss of optic neuritis compared with placebo. In addition, when patients with acute optic neuritis are treated with high-dose intravenous steroids, the 2-year rate of development of MS is reduced, although this effect diminishes over time.88,108 Of interest, oral prednisone was not found to be helpful in the optic neuritis trials and was associated with a potential increase in the number of optic neuritis episodes. The current standard therapy for an acute exacerbation in MS is intravenous methylprednisolone. A typical intravenous dose is 250 to 500 mg every 12 hours for 3 to 7 days. Whether this should be followed by an oral prednisolone taper remains controversial. Potential adverse effects of methylprednisolone therapy include fluid retention, gastrointestinal hemorrhage, anxiety, psychosis, infection, and osteoporosis. Several therapies directed toward the complications of MS may be helpful. The associated spasticity generally is treated with baclofen. This is a highly effective therapy aimed at reducing the painful flexor and extensor spasms. A major side effect is drowsiness, which generally diminishes with continued use. Higher-dose therapy can cause confusion, especially in the setting of baseline cognitive impairment. For patients with intractable spasticity, baclofen is available for intrathecal administration by either bolus therapy or continuous implanted pump therapy. Additional therapeutic agents for control of spasticity include tizanidine, diazepam, and dantrolene. The tremor and ataxia associated with MS occasionally are treated with propranolol, diazepam, or clonazepam. The results of these therapies, however, generally are unsatisfactory. Pain often is associated with MS and affects the shoulders, pelvic girdle, and face. The facial pain may be indistinguishable from that of trigeminal neuralgia. Treatment options include carbamazepine, baclofen, and tricyclic antidepressants. Fatigue, which is common, may be ameliorated with amantadine. This agent produces partial relief for a minority of patients. In controlled studies, the effect is only slightly better than placebo.83 Disposition Patients with a history of MS who seek treatment for significant symptoms must first be evaluated to rule out other, non– MS-related pathologic processes. Also, other systemic illnesses, especially infections, which can worsen the symptoms of MS, should be excluded. If the problem is thought to be an exacerbation of MS, most patients will require hospital admission for intravenous steroid therapy. An alternative to hospitalization may be to initiate intravenous steroids in the ED and to arrange for a next-day follow-up visit with the primary care physician or neurologist if outpatient intravenous steroid administration is an option. Patients with the new onset of symptoms suggestive of MS should be admitted or referred to a neurologist because early treatment has been shown to significantly decrease progression of the disease. KEY CONCEPTS Trigeminal Neuralgia ■ Patients with unilateral, intermittent, lancinating facial pain without abnormalities on physical examination are likely to have trigeminal neuralgia. ■ Carbamazepine is the first-line agent for medical treatment. ■ Patients who do not tolerate or whose pain is refractory to medical management may be candidates for microvascular decompression or ablation. Facial Nerve Paralysis ■ Patients with Bell’s palsy should be treated early in the course with corticosteroids, and antiviral medication is warranted in patients with severe loss of function. ■ Slowly progressive or recurrent facial paralysis is suggestive of a neoplasm. Recurrent unilateral paralysis may occur with Bell’s palsy but frequently (30%) is seen in patients with tumor. ■ Simultaneous bilateral facial paralysis is suggestive of Lyme disease, especially in endemic regions. ■ Patients who have facial muscle paresis with intact forehead movement should be considered to have a central (upper motor neuron) lesion until the diagnostic investigation proves otherwise. Vestibular Schwannoma ■ The onset of unilateral auditory symptoms, especially sensorineural hearing loss, requires evaluation and referral to an ear, nose, and throat specialist. ■ Neurologic symptoms of lower cranial nerve dysfunction, ataxia, or raised ICP may be caused by a benign tumor of the cerebellopontine angle. Diabetic Cranial Mononeuropathy ■ Diabetic neuropathy is a diagnosis of exclusion because no definitive diagnostic testing is available. ■ Both ischemic and hemorrhagic brainstem lesions must be ruled out in the case of an acute ophthalmoplegia. ■ Extraocular mononeuropathy is sufficiently common in patients with diabetes mellitus that its occurrence in isolation warrants evaluation of the patient for previously undiagnosed diabetes. Cerebral Venous Thrombosis ■ The differential diagnosis for CVT includes other conditions that present with new-onset neurologic deficits, alteration in 1418 PART III ◆ Medicine and Surgery / Section Seven • Neurology consciousness, or severe headache. CVT is more likely to be present in such patients when the etiology is unclear, the patient is thought to have a hypercoagulable state, and the head CT is normal in appearance or shows subtle signs of CVT. ■ Non–contrast-enhanced CT scanning is not adequate to rule out CVT. MRI with MRV is recommended, although multidetector row CT venography is an acceptable alternative. ■ Treatment of most patients with CVT includes systemic anticoagulation, even in the setting of hemorrhagic cerebral infarcts, unless another contraindication exists. Multiple Sclerosis ■ Any patient with a long-term illness, such as MS, must be evaluated to rule out pathologic processes not related to that illness before an exacerbation of the illness can be assumed to be the cause of any problems experienced by the patient. ■ Therapy for patients with MS will require consultation with the patient’s primary care provider or neurologist to provide consistent disease management. ■ Intravenous methylprednisolone effectively promotes earlier resolution of recurrences. ■ Intravenous methylprednisolone has been shown to speed the recovery from vision loss from optic neuritis. The references for this chapter can be found online by accessing the accompanying Expert Consult website. Chapter 105 / Brain and Cranial Nerve Disorders 1418.e1 References 1. Bennetto L, Patel NK, Fuller G: Trigeminal neuralgia and its management. BMJ 2007; 334:201. 2. MacDonald BK, Cockerell OC, Sander JWAS, Shorvon SD: The incidence and lifetime prevalence of neurological disorders in a prospective community-based study in the UK. Brain 2000; 123:665. 3. Katusic CS, Beard M, Bergstralth E, Kurland LT: Incidence and clinical features of trigeminal neuralgia, Rochester, Minnesota, 1945-1984. Ann Neurol 1990; 27:89. 4. Patel NK, et al: How accurate is magnetic resonance angiography in predicting neurovascular compression in patients with trigeminal neuralgia? A prospective, single-blinded comparative study. Br J Neurosurg 2003; 17:60. 5. Fukuda H, Ishikawa M, Okumura R: Demonstration of neurovascular compression in trigeminal neuralgia and hemifacial spasm with magnetic resonance imaging: Comparison with surgical findings in 60 consecutive cases. Surg Neurol 2003; 59:93. 6. Tenser RB: Trigeminal neuralgia: Mechanisms of treatment. Neurology 1998; 51:17. 7. Delzell JE Jr, Grelle AR: Trigeminal neuralgia: New treatment options for a well-known cause of facial pain. Arch Fam Med 1999; 8:264. 8. Jensen T, et al: Association of trigeminal neuralgia with multiple sclerosis: Clinical and pathological features. Acta Neurol Scand 1982; 65:182. 9. Taha JM, Tew JM: Comparison of surgical treatments for trigeminal neuralgia: Reevaluation of radiofrequency rhizotomy. Neurosurgery 1996; 38:865. 10. Chen JF, Lee ST: Comparison of percutaneous trigeminal ganglion compression and microvascular decompression for the management of trigeminal neuralgia. Clin Neurol Neurosurg 2003; 105:203. 11. McLaughlin MR, et al: Microvascular decompression of cranial nerves: Lessons learned after 4400 operations. J Neurosurg 1999; 90:1. 12. Dhople AA, et al: Long-term outcomes of Gamma Knife radiosurgery for classic trigeminal neuralgia: Implications of treatment and critical review of the literature. J Neurosurg 2009; 111:351-358. 13. Kondziolka D, et al: Gamma Knife radiosurgery for trigeminal neuralgia: Results and expectations. Arch Neurol 1998; 55:1524. 14. Shetter AG, et al: Gamma Knife radiosurgery for recurrent trigeminal neuralgia. J Neurosurg 2002; 97:536. 15. Adour K, et al: The true nature of Bell’s palsy: Analysis of 1000 consecutive patients. Laryngoscope 1978; 88:787. 16. Hauser W, et al: Incidence and prognosis of Bell’s palsy in the population of Rochester, Minnesota. Mayo Clin Proc 1971; 46:258. 17. Logan BM, Reynolds PA, Hutchings RT, eds: McMinn’s Color Atlas of Head and Neck Anatomy, 3rd ed. London: Mosby; 2004. 18. Jackson CG, Doersten PGV: The facial nerve: Current trends in diagnosis, treatment, and rehabilitation. Med Clin North Am 1999; 83:179. 19. Marenda S, Olsson J: The evaluation of facial paralysis. Otolaryngol Clin North Am 1997; 30:669. 20. Sullivan FM, et al: A randomised controlled trial of the use of aciclovir and/or prednisolone for the early treatment of Bell’s palsy: The BELLS study. Health Technol Assess 2009;13:iii-iv, ix-xi, 1-130. 21. de Almeida JR, et al: Combined corticosteroid and antiviral treatment for Bell Palsy. JAMA 2009; 302:985-993. 22. Salinas RA, Alvarez G, Daly F, Ferreira J: Corticosteroids for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 2010; 3:CD001942. 23. Yeo SG, Lee YC, Park DC, Cha CI: Acyclovir plus steroid vs steroid alone in the treatment of Bell’s palsy. Am J Otolaryngol 2008; 29:163-166. 24. Engström M, et al: Prednisolone and valaciclovir in Bell’s palsy: A randomised, double-blind, placebo-controlled, multicentre trial. Lancet Neurol 2008; 7:993-1000. 25. Knox GW: Treatment controversies in Bell’s palsy. Arch Otolaryngol Head Neck Surg 1998; 124:821. 26. Ruckenstein MJ: Evaluating facial paralysis: Expensive diagnostic tests are often unnecessary. Postgrad Med 1998; 103:187. 27. Sullivan FM, et al: Early treatment with prednisolone or acyclovir in Bell’s palsy. N Engl J Med 2007; 357:1598. 28. Murakami S, et al: Bell’s palsy and herpes simplex virus: Identification of viral DNA in endoneurial fluid and muscle. Ann Intern Med 1996; 124:27. 29. Adour KK, Ruboyianes JM, Doersten PGV, Byl FM: Bell’s palsy treatment with acyclovir and prednisone compared with prednisone alone: A double-blind, randomized, controlled trial. Ann Otol Rhinol Laryngol 1996; 105:371. 30. Hato N, et al: Valacyclovir and prednisolone treatment for Bell’s palsy: A multicenter, randomized, placebo-controlled study. Otol Neurotol 2007; 28:408. 31. Axelsson S, Lindberg S, Stjernquist-Desatnik A: Outcome of treatment with valacyclovir and prednisone in patients with Bell’s palsy. Ann Otol Rhinol Laryngol 2003; 112:197. 32. Dickins JRE, Smith JT, Graham S: Herpes zoster oticus: Treatment with intravenous acyclovir. Laryngoscope 1988; 98:776. 33. Uri N, Greenberg E, Kitzes-Cohen R, Doweck I: Acyclovir in the treatment of Ramsay Hunt syndrome. Otolaryngol Head Neck Surg 2003; 129:379. 34. Dotevall L, Hagberg L: Successful oral doxycycline treatment of Lyme disease–associated facial palsy and meningitis. Clin Infect Dis 1994; 28:569. 35. Cook SP, et al: Lyme disease and seventh nerve paralysis in children. Am J Otolaryngol 1997; 18:320. 36. Smith V, Traquina DN: Pediatric bilateral facial paralysis. Laryngoscope 1998; 108:519. 37. Joseph EM, Sperling NM: Facial nerve paralysis in acute otitis media: Cause and management revisited. Otolaryngol Head Neck Surg 1998; 118:694. 38. Jackson CG, Glasscock ME, Hughes G, Sismanis A: Facial paralysis of neoplastic origin: Diagnosis and management. Laryngoscope 1980; 90:1581. 39. Myrseth E, Pedersen PH, Moller P, Lund-Johansen M: Treatment of vestibular schwannomas: Why, when and how? Acta Neurochir (Wien) 2007; 149:647. 40. The Consensus Development Panel: National Institutes of Health Consensus Development Conference Statement on Acoustic Neuroma, December 11-13, 1991. Arch Neurol 1994; 51:201. 41. Selesnick S, Jackler R: Clinical manifestations and audiologic diagnosis of acoustic neuromas. Otolaryngol Clin North Am 1992; 25:521. 42. Wright A, Bradford R: Management of acoustic neuroma. BMJ 1995; 311:1141. 43. Backous DD, Pham HT: Guiding patients through the choices for treating vestibular schwannomas: Balancing options and ensuring informed consent. Otolaryngol Clin North Am 2007; 40:521. 44. Selesnick S, Jackler R, Pitts L: The changing clinical presentation of acoustic tumors in the MRI era. Laryngoscope 1993; 103:431. 45. Harvey S, Haberkamp T: Pitfalls in the diagnosis of CPA tumors. Ear Nose Throat J 1991; 70:290. 46. Myrseth E, Moller P, Pedersen PH, Lund-Johansen M: Vestibular schwannoma: Surgery or gamma knife radiosurgery? A prospective, nonrandomized study. Neurosurgery 2009; 64:654-661. 47. Murphy ES, et al: Long-term outcomes of Gamma Knife radiosurgery in patients with vestibular schwannomas. J Neurosurg 2011; 114:432-440. 48. Watanabe K, et al: Characteristics of cranial nerve palsies in diabetic patients. Diabetes Res Clin Pract 1990; 10:19. 49. Thomas PK: Clinical features and investigation of diabetic somatic peripheral neuropathy. Clin Neurosci 1997; 4:341. 50. Greco D, Gambina F, Pisciotta M, Abrignani M, Maggio F: Clinical characteristics and associated comorbidities in diabetic patients with cranial nerve palsies. J Endocrinol Invest 2012; 35:146-149. 51. Asbury AK, Aldredge H, Hershberg R, Fisher CM: Oculomotor palsy in diabetes mellitus: A clinico-pathological study. Brain 1970; 93:555. 52. Brown MJ, Asbury AK: Diabetic neuropathy. Ann Neurol 1984; 15:2. 53. Clements RS, Bell DS: Diabetic neuropathy: Peripheral and autonomic syndromes. Postgrad Med 1982; 71:50. 54. Fujioka T, et al: Ischemic and hemorrhagic brain stem lesions mimicking diabetic ophthalmoplegia. Clin Neurol Neurosurg 1995; 97:167. 55. Tankova T, Cherninkova S, Koev D: Treatment for diabetic mononeuropathy with alpha-lipoic acid. Int J Clin Pract 2005; 59:645. 56. Wasay M, et al: Cerebral venous thrombosis: Analysis of a multicenter cohort from the United States. J Stroke Cerebrovasc Dis 2008; 17:49-54. 57. Ferro JM, Canhão P, Bousser MG, Stam J, Barinagarrementeria F, ISCVT Investigators: Prognosis of cerebral vein and dural sinus thrombosis: Results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004; 35:664. 58. Stam J: Thrombosis of the cerebral veins and sinuses. N Engl J Med 2005; 352:1791. 59. Villringer A, Einhäupl KM: Dural sinus and cerebral venous thrombosis. New Horiz 1997; 5:332. 60. Wasson J, Redenbaugh J: Transverse sinus thrombosis: An unusual cause of headache. Headache 1997; 37:457. 61. Ferro JM, et al: Cerebral vein and dural sinus thrombosis in Portugal: 1908-1998. Cerebrovasc Dis 2001; 11:177. 1418.e2 PART III ◆ Medicine and Surgery / Section Seven • Neurology 62. Ferro JM, Canhão P, Bousser MG, Stam J, Barinagarrementeria F, ISCVT Investigators: Early seizures in cerebral vein and dural sinus thrombosis: Risk factors and role of antiepileptics. Stroke 2008; 39:1152-1158. 63. Villringer A, Mehraein S, Einhäupl KM: Pathophysiological aspects of cerebral sinus venous thrombosis (SVT). J Neuroradiol 1994; 21:72. 64. Linn J, et al: Noncontrast CT in deep cerebral venous thrombosis and sinus thrombosis: Comparison of its diagnostic value for both entities. AJNR Am J Neuroradiol 2009; 30:728-735. 65. Provenzale JM, Joseph GJ, Barboriak DP: Dural sinus thrombosis: Findings on CT and MR imaging and diagnostic pitfalls. AJR Am J Roentgenol 1998; 170:777. 66. Gratama van Andel HA, et al: Interobserver variability in the detection of cerebral venous thrombosis using CT venography with matched mask bone elimination. Clin Neurol Neurosurg 2009; 111:717-723. 67. Gaikwad A, Mudalgi B, Patankar K, Patil J, Ghongade D: Diagnostic role of 64-slice multidetector row CT scan and CT venogram in cases of cerebral venous thrombosis. Emerg Radiol 2008; 15:325-333. 68. Linn J, et al: Diagnostic value of multidetector-row CT angiography in the evaluation of thrombosis of the cerebral venous sinuses. Am J Neuroradiol 2007; 28:946. 69. Khandelwal N, et al: Comparison of CT venography with MR venography in cerebral sinovenous thrombosis. AJR Am J Roentgenol 2006; 187:1637. 70. Kosinski CM, et al: Do normal D-dimer levels reliably exclude cerebral sinus thrombosis? Stroke 2004; 35:2820. 71. Talbot K, Wright M, Keeling D: Normal D-dimer levels do not exclude the diagnosis of cerebral venous sinus thrombosis. J Neurol 2002; 249:1603. 72. Lalive PH, et al: Is measurement of D-dimer useful in the diagnosis of cerebral venous thrombosis? Neurology 2003; 61:1057. 73. Tardy B, et al: D-dimer levels in patients with suspected acute cerebral venous thrombosis. Am J Med 2002; 113:238. 74. Preter M, Tzourio C, Ameri A, Bousser MG: Long-term prognosis in cerebral venous thrombosis: Follow-up of 77 patients. Stroke 1996; 27:243. 75. Frey JL, et al: Cerebral venous thrombosis: Combined intrathrombus rtPA and intravenous heparin. Stroke 1999; 30:489. 76. Einhäupl KM, Villringer A: Heparin treatment in sinus venous thrombosis. Lancet 1991; 338:597. 77. Coutinho JM, et al: Unfractionated or low-molecular weight heparin for the treatment of cerebral venous thrombosis. Stroke 2010; 41:2575-2580. 78. Stam J, De Bruijn SF, DeVeber G: Anticoagulation for cerebral sinus thrombosis. Cochrane Database Syst Rev 2002; 4:CD002005. 79. Wasay M, et al: Nonrandomized comparison of local urokinase thrombolysis versus systemic heparin anticoagulation for superior sagittal sinus thrombosis [editorial comment]. Stroke 2001; 32:2310. 80. Francis G, et al: Inflammatory demyelinating diseases of the central nervous system. In: Bradley WG, ed: Neurology in Clinical Practice. Boston: Butterworth-Heinemann; 1996. 81. Kurtzke JF, Hyllested K, Heltberg A: Multiple sclerosis in the Faroe Islands: Transmission across four epidemics. Acta Neurol Scand 1995; 91:321. 82. Hogancamp WE, Rodriguez M, Weinshenker BG: Symposium on multiple sclerosis—part III: The epidemiology of multiple sclerosis. Mayo Clin Proc 1997; 72:871. 83. Giovannoni G, Miller DH: Multiple sclerosis and its treatment. J R Coll Physicians Lond 1999; 33:315. 84. Winkelmann A, Engel C, Apel A, Zettl UK: Cognitive impairment in multiple sclerosis. J Neurol 2007; 254:II35. 85. Rao SM, Leo GJ, Bernardin L, Unverzagt F: Cognitive dysfunction in multiple sclerosis. I. Frequency, patterns, and prediction. Neurology 1991; 41:685. 86. Swirsky-Sacchetti T, et al: Neuropsychological and structural brain lesions in multiple sclerosis: A regional analysis. Neurology 1992; 42:1291. 87. Wray SH: Optic neuritis: Guidelines. Curr Opin Neurol 1995; 8:72. 88. Beck RW, et al: The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. N Engl J Med 1993; 329:1764. 89. Ebers GC: Optic neuritis and multiple sclerosis. Arch Neurol 1985; 42:702. 90. Kidd D: Presentations of multiple sclerosis. Practitioner 1999; 1:24. 91. Mehta PD: Diagnostic usefulness of cerebrospinal fluid in multiple sclerosis. Crit Rev Clin Lab Sci 1991; 28:233. 92. Lee KH, et al: Magnetic resonance imaging of the head in the diagnosis of multiple sclerosis: A prospective 2-year follow-up with comparison of clinical evaluation, evoked potentials, oligoclonal banding, and CT. Neurology 1991; 41:657. 93. Neema M, et al: MRI in multiple sclerosis: What’s inside the toolbox? Neurotherapeutics 2007; 4:602. 94. Morrissey SP, et al: The significance of brain magnetic resonance imaging abnormalities at presentation with clinically isolated syndromes suggestive of multiple sclerosis: A 5-year follow-up study. Brain 1993; 116:135. 95. European Study Group on Interferon β-1b in Secondary Progressive MS: Randomised double-blind placebo-controlled study of interferon β-1a in relapsing/remitting multiple sclerosis. Lancet 1998; 352:1498. 96. Kappos L, et al: Treatment with interferon β-1b delays conversion to clinically definite and McDonald MS in patients with clinically isolated syndromes. Neurology 2006; 67:1242. 97. Comi G, et al: Effect of early interferon treatment on conversion to definite multiple sclerosis: A randomised study. Lancet 2001; 357:1576. 98. Jacobs LD, et al: Intramuscular interferon β-1a therapy initiated during a first demyelinating event in multiple sclerosis. N Engl J Med 2000; 343:898. 99. Stuve O, et al: Pharmacological treatment of early multiple sclerosis. Drugs 2008; 68:73. 100. Johnson KP, et al: Extended use of glatiramer acetate (Copaxone) is well tolerated and maintains its clinical effect on multiple sclerosis relapse rate and degree of disability. Neurology 1998; 50:701. 101. Comi G, et al: Effect of glatiramer acetate on conversion to clinically definite multiple sclerosis in patients with clinically isolated syndrome (PreCISe study): A randomised, double-blind, placebo-controlled trial. Lancet 2009; 374:1503-1511. 102. Kappos L, et al: Natalizumab treatment for multiple sclerosis: Recommendations for patient selection and monitoring. Lancet Neurol 2007; 6:431-441. 103. Kappos L, et al: A placebo-controlled trial of oral fingolimod in relapsing multiple sclerosis. N Engl J Med 2010; 362:387-401. 104. Cohen JA, et al: Oral fingolimod or intramuscular interferon for relapsing multiple sclerosis. N Engl J Med 2010; 362:402-415. 105. Giovannoni G, et al: A placebo-controlled trial of oral cladribine for relapsing multiple sclerosis. N Engl J Med 2010; 362:416-426. 106. Polman CH, et al: A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med 2006; 354:899-910. 107. Rudick RA, et al: Natalizumab plus interferon β-1a for relapsing multiple sclerosis. N Engl J Med 2006; 354:911-923. 108. Beck RW, et al: A randomized, controlled trial of corticosteroids in the treatment of acute optic neuritis. The Optic Neuritis Study Group. N Engl J Med 1992; 326:581.