Trauma and TCD, Times are Changing - Barnes
advertisement

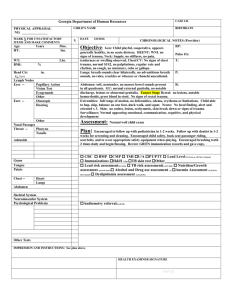
Douglas J.E. Schuerer, M.D. Associate Professor of Surgery Washington University School of Medicine May 7, 2014 In 2008, legislation passed in Missouri creating the “Time Critical Diagnosis” system. Created a statewide system for emergency medical care for trauma, stroke, or STEMI. Idea was to build on the trauma framework for the other two diagnoses. Goal: Quick assessment, diagnosis and treatment by a facility that can provide timely, definitive care to minimize risk for preventable complications and death. Trauma Task Force Review entire trauma system including ◦ ◦ ◦ ◦ Need for level IV trauma centers Develop statewide trauma classification system Develop triage/ transfer protocols Develop disease specific protocols (burns, amputations, etc.) Written regulations for Level IV centers Final Trauma classification and Triage Protocols Recognized the importance and need for regional EMS committees. Based planning on rapid disposition to appropriate centers. What is the Golden Hour? Developed as a theoretical concept initially in the care of the traumatically injured patient by Dr. Crowley in Baltimore. Important as we realized when trauma deaths occur and from what causes. Some studies have suggested that the concept is faulty and there is no specific benefit to getting to a trauma center quickly However many have shown that rapid transport to a trauma center improves survival Trauma mortality is higher in rural areas, often due to delayed transport. Air ambulances improve survival in rural areas as well. No definitive studies exist in trauma, but stroke and STEMI have well developed time targets Trauma likely different because of variability of the disease. Why would the Golden Hour make a difference? Treatment Problem Loss of airway Tension pneumothorax Pericardial tamponade Acute blood loss Epidural hematoma Aortic rupture Intubation Chest tube Pericardiocentesis Transfusion / Operating Room (OR) OR OR / Blood Pressure control Have facilities always ready to care for the acute injuries Surgeon available for immediate Operating Room (except Level IVs) Multidisciplinary team ready Trauma centers improve survival over nontrauma centers. Patients transferred to higher level trauma centers do better than if not transferred from lower level trauma centers. State verification as highest level of preparedness. American College of Surgeons verification an even more stringent review process. Fewer hospitals in the region have achieved this higher benchmark. None have held in continuously as BarnesJewish as for 17 years. Able to treat all types of trauma at a moments notice. Regional resource for the care of the injured patient. Research and education an important part of the mission. Injury prevention initiatives a required element. Developed Triage and Transfer Protocols to guide initial placement of patients with injuries. In general, the plan calls for more injured patients to be taken to higher level centers. Add Level 4 centers for the lowest level patients. March 16, 2009, Richardson sustained a head injury when she fell skiing. No helmet, not required in Quebec Skiing lesson at the Mont Tremblant Resort in Quebec, Canada about 80 miles (130 km) from Montreal. Was initially lucid Ski Patrol called ambulance, who were waiting at bottom of the mountain They skied by and told them they were not needed. She refused treatment at least twice, but was eventually taken by ambulance from the hotel 3 hours after the injury to a local hospital. She was transferred to a trauma center in Montreal by ground, and arrived 7 hours after her injury. There were no air ambulance services in Quebec at the time She died the next day, and was an organ donor, from a epidural hematoma. What about TCD? Debate over who can refuse care Early launch of helicopters can improve survival Patients like this will need to go directly to a higher level of care, reducing double transfers and time to definitive care With early transfer, this was survivable And then there was the helmet issue… Had watched the Mike Tyson fight the night of September 7, 1996 He decided not to wear his normal bullet proof vest. At about 11:15 pm, he was a passenger in a car riding on the Las Vegas strip. A car pulled next to them and emptied multiple rounds into the car. The driver, Suge Night was also superficially hit in the head Tupac could talk and breathe at the time. He floored it, did a spin out and drove about 1 mile away in a few minutes This was impressive as the strip was crowded and three wheels were shot out. Ambulance met them at 1130pm He was at UMC at 12 MN He reportedly said, “ I can’t breathe.” A chest tube was placed with 1500 mL out He underwent an immediate operation Unclear what happened when, but at next operation the next day he likely had a pmeumonectomy. Originally he improved, but he died 6 days after the shooting after several rounds of bleeding and CPR. He unfortunately was on such a crowded road, it was almost like a rural location EMS did meet him at a location, but it was still 30 minute transport time Unclear if a balanced resuscitation was used, but he did develop coagulopathy Even more rapid transport unlikely to help given need for pulmonectomy. The events of Sunday, August 31, 1997: ◦ 12:20 am: Princess Di and Dodi Fayed leave in car with bodyguard Trevor Rees-Jones and driver Henri Paul. ◦ There is still much debate over whether Paul was intoxicated – he probably was. ◦ 12:23: The car reaches the Place de l’Alma tunnel. Estimates are the car was going 90 – 120 mph – it is zoned 30 mph. For unknown reasons, the car veered, braked and lost control. It then struck the 13th concrete pillar, rolled over and rebounded off the right wall. Paul and Fayed were killed instantly. 12:27 : Firefighters get the first call for help. Dr. Frederic Mailez, a bystander ER physician, said Diana “was unconscious, moaning, and gesturing.” 12:40 : Police and firefighters arrive. Trevor-Jones and Diana are still alive. First reports were they had to cut Diana out, but later this was not the case. 52 minutes later, Diana was placed in the ambulance. The ambulance started on the journey to the hospital – 3.7 miles away. 2:05 : 43 minutes later she arrives at the hospital. There was one stop in route to administer adrenaline. Travel rate was 25 mph. Total ambulance arrival to hospital time was 1 hour 35 minutes (3.7 miles) Resuscitation including thoracotomy is tried for 2 hours. 4:05 : Princess Diana declared dead. Ambulance ◦ The French developed the first ambulances in 1797. ◦ Developed to rapidly evacuate casualties from the battlefield during the Italian campaign (The French always seem to have a lot of casualties when they don’t surrender first.) ◦ Horse- drawn wagons. SAMU (Service d’Aide Medicale Urgente) ◦ French ambulance system ◦ Physician on board at all times, traveling MICU ◦ They believe in treating the patient at the scene “Stay and Play” In US “ Scoop and Run” ◦ Driving slower is better, “So the patient is not rocked around.” Diana was found to have a torn left pulmonary vein. Normally, this would present as a left hemothorax and require a left thoracotomy. Hemothorax Wide Mediastinum CT By report, she actually had a right hemothorax secondary to a torn pericardium. The initial incision was on the wrong side, thus delaying time until the repair of the pulmonary vein. My thoughts: ◦ The delayed time until the patient got to the O.R. probably changed her outcome. Apparently “The Golden Hour” is not important in France. ◦ TCD principles would likely have saved her, including balanced resuscitation. ◦ Pulmonary vein bleeding can still be fatal, even with rapid hospital transport. ◦ The unfortunate wrong initial side of surgery compounded the time until repair was effected. I think in the United States she would have lived if not in a rural area. March 30, 1981: Only 70 days after taking office, at 1425, Reagan exited the Hilton Hotel and approached his limo. As he waved to the crowd, he and three others were shot by John Hinkley, who was apparently trying to impress Jodi Foster. Watched “Taxi Driver” with DeNiro playing a man who protected Foster’s character in the movie by killing her pimps. Wanted to do a grand gesture to impress Foster. Bought a $25 gun and waited outside the Washington Hilton. Hinkley fired six times in three seconds. He used Devastator bullets, designed to expand on impact. Four of the six hit someone, the last hit Reagan. SS Agent McCarthy also was hit. McCarthy dove in front of the President to stop a bullet. He was hit in the chest, but survived. He received the NCAA Award of Valor. Reagan was hit by a bullet that ricocheted off his armor plated limo. (He did not know it at the time.) Also shot were Press Secretary James Brady, Secret Service Agent Timothy McCarthy, and a D.C. police officer, Thomas Delahanty. He was pushed into the limo by the secret service and he felt pain in his rib. He said, “Get the … off, I think you’ve broken a rib.” Then he coughed up blood. The agent ordered the limo driver to go to George Washington Medical Center – 9 blocks away. He reported difficulty breathing. 1435: Arrival to ED – “I can’t catch my breath.” ◦ He fell to his knees and was carried to a trauma room. ◦ Extreme pain. ◦ Initial BP – 80/palp Blood noted at face and mouth. O2 by mask, Fluid, 2 Units PRBCs started. President able to make jokes. Wound at 4th intercostal space, posterior axillary line. No breath sounds over left chest. Hct from 40 to 30 in 30 minutes. Chest tube yielded 1200 ml of blood and continued at 200 – 300/ 15 minutes. – Total of 2275 in the E.D. There is some discrepancy here, with other reports of only 1200 to 1300 total. Most trauma texts now advise thoracotomy if more than 1500 ml at first and more than 200 an hour of bleeding. BP – 160/100 in 15 minutes. There are some who say a left subclavian line was attempted which led to the increased bleeding from the chest tube – so a trip to the O.R. In fact, most low velocity GSW’s to the chest do not require thoracotomy (90%) Did he really need the O.R? Likely yes, but not from the lung injury but potentially from a subclavian vein injury – we will never know. It turns out it was a devastator bullet with lead azide-filled centers that wold have required an operation to remove anyway. 1458 CXR: President to the surgeon Dr. Benjamin Aaron, “Please tell me you’re a Republican.” Dr. Aaron, a liberal Democrat, “Today, Mr. President, we’re all Republicans.” Bullet finally found and bleeding controlled. Operation ◦ ◦ ◦ ◦ 2 hours and 40 minutes EBL 3000 to 3500 Transfused 8 units PRBC, 3 units FFP, 1 pack plts HCT 33 in the recovery room Recovery delayed by atelectasis, mucous plugging, and possible pneumonia He was never reintubated, but was bronched twice. He was discharged on 4/11/81, POD #12 What would be different with TCD? ◦ Ambulance vs. limo. ◦ Chest CT with angio would rule-out concern for cardiac wound. ◦ Abdominal CT would replace DPL. ◦ Likely would have avoided emergent O.R. ◦ Would not have looked so long for the bullet during the case (avoid coagulopathy). Questions?