Clinical Medicine: Therapeutics
Review
Open Access
Full open access to this and
thousands of other papers at
http://www.la-press.com.
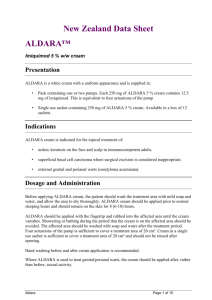
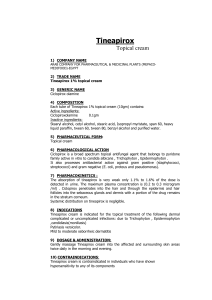
A Review of Topical Imiquimod in the Management of Basal
Cell Carcinoma, Actinic Keratoses, and Other Skin Lesions
Jubin Ryu1 and F. Clarissa Yang2
Harvard Medical School, Boston, MA 02115. 2Brigham and Women’s Hospital, Department of Dermatology,
221 Longwood Avenue, Boston, MA 02115.
1
Abstract: Imiquimod (trade name Aldara™) is a small molecule of the imidazoquinoline family, a group of nucleoside analogs that
were first synthesized as potential antiviral agents. It has since been discovered to activate both innate and adaptive immunity, as well
as apoptosis. Clinically, it has been approved for three indications thus far: external genital warts, actinic keratosis, and superficial
basal cell carcinoma. In addition to these applications, a number of off-label uses have been reported in the literature. In this review,
we summarize and discuss the literature describing imiquimod’s mechanism of action, its approved and off-label clinical uses, and its
safety and tolerability.
Keywords: imiquimod, aldara, immunomodulator, external genital warts, actinic keratosis, basal cell carcinoma
Clinical Medicine: Therapeutics 2009:1 1557–1575
This article is available from http://www.la-press.com.
© Libertas Academica Ltd.
This is an open access article distributed under the terms of the Creative Commons Attribution License
(http://www.creativecommons.org/licenses/by/2.0) which permits unrestricted use, distribution and reproduction
provided the original work is properly cited.
The authors grant exclusive rights to all commercial reproduction and distribution to Libertas Academica. Commercial
reproduction and distribution rights are reserved by Libertas Academica. No unauthorised commercial use permitted
without express consent of Libertas Academica. Contact tom.hill@la-press.com for further information.
Clinical Medicine: Therapeutics 2009:1
1557
Ryu and Yang
Introduction
Imiquimod (1-(2-methylpropyl)-1H-imidazo[4,5-c]
quinolin-4-amine) (trade name Aldara™) is a small
molecule of the imidazoquinoline family, a group
of nucleoside analogs that were first synthesized
as potential antiviral agents.1–4 Although no direct
antiviral activity was initially found in vitro,
imiquimod has since been shown to stimulate both
innate and adaptive immunity, as well as induce
apoptosis.
This novel biological activity has piqued clinical
interest and led to multiple trials testing imiquimod’s efficacy and safety across a range of skin
pathologies.5–8 Currently, it is approved for external
anogenital warts, actinic keratosis (AK), and superficial basal cell carcinoma (sBCC). In addition, its use
has been investigated in non-genital cutaneous warts,
genital herpes, molluscum contagiosum, squamous
cell carcinoma in situ (SCCIS), squamous cell carcinoma (SCC), nodular BCC (nBCC), lentigo maligna,
metastatic melanoma, vulvar and vaginal intraepithelial neoplasia (VIN/VAIN), mycosis fungoides, Kaposi’s
sarcoma, infantile hemangioma, pyogenic granuloma, leishmaniasis, scars/keloids, and in immunosuppressed patients.
In this review, we will describe imiquimod’s
molecular and cellular mechanism of action, as well
as its pharmacokinetic profile. Next, we will report
salient clinical trials that have characterized its efficacy and safety for specific skin diseases. We conclude this review with an overview of imiquimod’s
role in therapy, a survey of the gaps in the current
research literature, and a look towards possible applications in the future.
Mechanism of Action
Shortly after imiquimod was found to have no
direct in vitro effect against viruses, several lines of
in vivo data demonstrated that it did still harbor indirect
antiviral activity. In guinea pigs, the drug acted both
prophylactically and therapeutically against primary
herpes simplex virus (HSV) infection when administered orally, parenterally, intravaginally, or topically.2,9 In addition to activity against HSV, imiquimod
reduced cytomegalovirus (CMV) viremia when given
to guinea pigs 24 hours before virus inoculation.10 In
1992, Sidky et al demonstrated for the first time that
imiquimod possessed anti-tumor activity as well.11
1558
This effect was inhibited by concurrent administration
of anti-interferon-α (IFN-α) serum.
Imiquimod was thus shown to have an antiviral effect, although it was not through a direct
mechanism as originally predicted. In addition, it was
shown to have unanticipated anti-tumor activity. Subsequent studies delineated cellular and molecular
mechanisms that might account for these biological
effects. In the most established of these models,
imiquimod induces the release of inflammatory cytokines, thereby triggering the innate immune system.
Imiquimod stimulates adaptive immunity as well,
most likely indirectly by acting on antigen-presenting
cells (APCs). In addition to its effects on innate and
adaptive immunity, more recent data has shown
that imiquimod induces apoptosis as well.
Imiquimod in innate immunity
Vertebrates possess immune systems that can be
divided into two components: innate and adaptive
immunity.12 Cells of the innate response consist of
macrophages, neutrophils, basophils, mast cells,
eosinophils, and natural killer (NK) cells; these cells
coordinate the initial, rapid response to pathogens.
This response is marked by its relative nonspecificity.
Rather than target highly unique antigens, the cells
of this system scan for broadly conserved pathogen
associated molecular patterns (PAMPs). Cytokines
released during innate immune responses include
tumor necrosis factor (TNF)-α, interleukin (IL)-1,
IL-6, IL-10, IL-12, IL-15, IL-18, type I interferons
such as IFN-α, and chemokines.
A number of studies have demonstrated imiquimod’s ability to induce cytokines of the innate
immune system, both in vitro and in vivo. In cultured
mouse spleen cells, imiquimod induced IFN-α, IL-6,
and TNF-α.13 In mouse macrophage cells, imiquimod
stimulated TNF-α, as well as 2’5’-oligoadenylate
synthase (2-5-OAS), an enzyme regulated by
IFN-α/β.14 In cultured monkey peripheral blood
monocytes (PBMCs), imiquimod induced IFN-α,
IL-1β, IL-6 and IL-8.15 In addition, messenger RNA
(mRNA) levels of IFN-α, IL-1α, IL-1, and the IFNinducible gene MxA were increased with imiquimod.
In human PBMCs, increases were reported in
serum protein concentrations of IFN-α, TNF-α, IL-1,
IL-1RA, IL-6, IL-8, IL-10, IL-12 p40, granulocyte
colony stimulating factor (G-CSF), macrophage
Clinical Medicine: Therapeutics 2009:1
Topical imiquimod: mechanism of action and clinical uses
inflammatory proteins 1-α and 1-β, and macrophage
chemotactic protein.16,17 In addition to protein induction,
imiquimod caused increases in mRNA levels of IFN-α,
IFN-β, IL-6, IL-8, and TNF-α in human PBMCs.18
In human keratinocytes and epidermal cancer cells,
Kono et al observed mRNA induction for IL-6 and
IL-8, but not for IL-1α.19
These in vitro data have been corroborated by
in vivo studies. In guinea pigs, imiquimod increased
serum levels of IFN-α when given orally, intravaginally, topically, or parenterally.20 When given orally or
parenterally to mice, the drug induced IFN-α, TNF-α,
and IL-6.13 Imbertson et al applied imiquimod to the
flanks of hairless mice and rats and found increased
IFN-α mRNA and protein and TNF-α protein.21
In cynomolgus monkeys, oral imiquimod increased
serum levels of IFN-α and IL-1RA.15 Tyring et al
treated genital warts with topical 5% imiquimod and
analyzed the skin biopsy for human papilloma virus
(HPV) DNA and cytokine mRNA. Polymerase chain
reaction (PCR) revealed that imiquimod-treated
lesions were significantly reduced in viral DNA, and
reverse transcriptase (RT)-PCR revealed increased
mRNA expression of IFN-α and TNF-α.22
How does imiquimod initiate this cytokine response
on a molecular level? One possibility is through the
Toll-like receptor (TLR), a cell surface transmembrane receptor homologous to the Toll protein found in
Drosophila melanogaster.23–25 Like D. melanogaster
Toll, human TLRs can activate nuclear factor-κB
(NF-κB) signaling, as well as induce downstream
expression of IL-1, IL-6, and IL-8.26 Interestingly,
overexpressed TLR also induced the costimulatory B7 protein, indicating that TLRs can activate
adaptive immunity. A total of 10 human TLRs have
been discovered, and they are now established as a
critical type of pattern recognition protein (PRP) on
the surface of innate immune cells that can recognize
PAMPs on invading pathogens.27,28
The link between imidazoquinolines and TLRs
was made when Hemmi et al reported that mice
deficient in TLR7 showed a muted immune response
to resiquimod (R-848), a derivative of imiquimod.29
Furthermore, mice deficient in MyD88, an adaptor
protein in TLR signaling, showed a similarly
inhibited immune response. Jurk et al provided
in vitro evidence that R-848 can activate both TLR7
and TLR8 to stimulate NF-κB in a dose dependent
Clinical Medicine: Therapeutics 2009:1
manner.30 These data suggested that imiquimod’s
immunologic activity is mediated, at least in part, by
activation of TLR7 and/or TLR8, leading to activation of NF-κB and subsequent gene expression of its
proinflammatory cytokine targets.
In support of these data, Megyeri et al identified
increased levels of NF-κB-DNA complexes after
imiquimod application to human PBMCs.18 In addition, they found increased complexes of a second
transcription factor, α4F1. A third transcription
factor, signal transducer and activator of transcription 1 (STAT-1), also seems to be a critical downstream transcription factor, as mice deficient in this
protein show a blunted response to imiquimod.31
Together, these studies identify STAT-1, NF-κB, and
α4F1 as important downstream signaling components
of the imiquimod response.
Imiquimod in adaptive immunity
The ability of TLRs to stimulate both innate and
adaptive immunity raised the possibility that imiquimod might also regulate both arms of the immune
system. Unlike innate immunity, adaptive immunity is
hallmarked by the specificity of its response to unique
antigens.12 The adaptive immune system consists of
B and T-lymphocytes, as well as the APCs that are
necessary to activate them within lymphoid tissue.
T-helper (Th) cells are among the major releasers
of cytokines within the adaptive immune system,
and they are divided into two classes based on the
cytokines they release. Th1 cells generally activate
cellular responses to pathogens, including macrophages and cytotoxic T cells (Tc cells); this cytokine
profile consists of IFN-γ, lymphotoxin, and TNF-β.
Th2 cells activate a humoral response by stimulating
B cells; cytokines of this subtype include IL-4, IL-5,
and IL-13.
Although imiquimod has not been shown to directly
stimulate lymphocyte proliferation or cytokine release,
it has been reported to induce adaptive immunity in the
presence of APCs. In 1999, Wagner et al reported that
imiquimod could induce release of the Th1 cytokine
IFN-γ in both murine and human cell cultures.15 The
cytokines IL-12 and IFN-α were necessary for IFN-γ
induction. In addition to inducing IFN-γ, imiquimod
has been shown to have a broader stimulatory effect
on antigen presentation. In mice, topical imiquimod
led to a reduced number of Langerhans cells (LCs) in
1559
Ryu and Yang
the epidermis, and the remaining epidermal LCs were
morphologically activated.32 In addition, imiquimod
enhanced LC migration from skin to draining lymph
nodes following antigen challenge. Consistent with
these murine data, studies in cultured human LCs
showed that imiquimod-treated LCs could induce
30–300-fold greater T-cell proliferation relative to
untreated control LCs.33,34 Furthermore, imiquimodtreated LCs showed expression of several cell-surface
co-stimulatory proteins, including CD1a, HLA-DR,
HLA-DP, HLA-DQ, CD40, CD86, and CD80.
Several studies have also reported imiquimodmediated activation of B-cells. In purified B-cells from
mice and humans, imiquimod stimulated proliferation
and secretion of immunoglobulins in the absence of
other immunocytes.35 These data suggest that unlike
T-cells, B-cells may be directly activated by imiquimod. Bishop et al suggested that this effect may be
through binding and activation of CD40, a B-cell
surface receptor. This group reported that R-848 can
induce signaling mechanisms and cellular changes
similar to those activated by CD40 binding.36,37
Imiquimod in apoptosis
In addition to its wide-ranging activation of the
immune system, imiquimod has also been shown by
more recent data to possess pro-apoptotic activity.
In human basal cell carcinoma (BCC), topical application induces increased expression of the pro-apoptosis
death receptor CD95 (Fas).38 In addition, several
groups have reported decreases in the pro-survival
protein Bcl-2, and transfection of Bcl-2 into tumor
cells blunts imiquimod’s pro-apoptotic effect.39,40
Finally, downstream of these signaling events, inhibition of caspases reduces imiquimod-induced apoptosis, indicating that this proteolytic cascade is a
necessary part of the mechanism.40
Pharmacokinetics
Several studies have investigated the pharmacokinetics
of imiquimod in the context of specific skin diseases.
Harrison et al reported a study of 58 adult patients
with 5–20 AK lesions divided into three groups.41
The first group (12 males/11 females) applied 12.5
mg of imiquimod to facial lesions. The second group
(11 males) applied 25 mg to bald areas of the scalp.
The third group (12 males/12 females) applied 75 mg
to their hands and forearms bilaterally. All groups
1560
applied their specified dosages three times a week
for up to 16 weeks. Pharmacokinetic data were taken
biweekly, and after the first and last dose.
Serum concentrations of imiquimod after first
and last doses were low, reflecting minimal dermal
absorption.41 After the first dose of imiquimod, peak
serum concentration (Cmax) was 0.09, 0.14, and
0.78 ng/mL for the face, scalp, and hand/arm groups,
respectively. After the final dose, Cmax values were
0.12, 0.21, and 1.35 ng/mL for the three groups. Area
under the serum concentration-time curve (AUC)
also increased with multiple dosing. After the first
dose, AUC was 1.99, 3.32, and 23.6 ng/h/mL for the
face, scalp, and hand/arm groups, respectively. After
the last dose, AUC was 2.06, 4.89, and 29.1 ng/h/mL.
Metabolite levels were undetectable in any of the
three groups after the first dose and were transiently
detected only in the face and hand/arm groups after
the last dose. The calculated half-life (t1/2) after the
last dose of imiquimod was 23, 21, and 27 hours for
the face, scalp, and hand/arm groups, respectively.
Urinary excretion of imiquimod or any of its five
metabolites was minimal, ranging from 0.05% to
0.24% of the total dose among the three groups.
Another study by Myhre et al studied imiquimod
pharmacokinetics in 22 children (ages 2–12 years) with
molluscum contagiosum.42 All children had 10% of
their total body surface area affected by molluscum con­
tag­iosum and were assigned to between 12.5–37.5 mg
of imiquimod per dose. Each patient applied their
assigned dose three times per week for a total of
4 weeks. As in the Harrison et al study, serum concentrations of imiquimod were low after both first and
last dose, regardless of the size of individual dose.
Cmax values ranged from 0.1 to 0.6 ng/mL after the first
dose, and from 0.2–2.2 ng/mL after the last dose. AUC
ranged from 0.1–3.0 ng/h/ml after the first dose and
from 1.4–10.8 ng/h/mL after the last dose. Both Cmax
and AUC values rose proportionally with dose normalized for body weight (p 0.05 for both Cmax and AUC).
After the first dose, 5 out of 22 children had detectable
metabolites, all at a serum concentration 0.1 ng/mL.
After the last dose, 8 out of 22 children had measurable
metabolites, with a maximum value of 0.23 ng/mL.
Clinical Applications
In addition to its three approved indications for external
anogenital warts, actinic keratosis, and superficial
Clinical Medicine: Therapeutics 2009:1
Clinical Medicine: Therapeutics 2009:1
*p 0.01 relative to vehicle. **p 0.001 relative to vehicle. ***p 0.0001 relative to vehicle. +defined as 100% disappearance of lesions assessed clinically. ^percentages calculated from
patients with complete clearance only.
Abbreviations: P, prospective; R, randomized; DB, double-blinded; VC, vehicle-controlled; TIW, 3x/week; V, vehicle; ET, end of treatment; PT, post-treatment.
5%: 100% (6/6) (6 mos PT)
V: NR
5%: 70% (23/34) (ET)*
V: 9% (1/11) (ET)
5% TIW (12 wks)
P, R, DB, VC
Arican et al45
45
1%: 17% (2/12) (12 wks PT)
5%: 19% (9/48) (12 wks PT)
V: 0% (0/3) (12 wks PT)
1%: 14% (13/90) (ET)**
5%: 52% (49/94) (ET)***
V: 4% (3/95) (ET)
1% or 5% daily (16 wks)
P, R, DB, VC
Beutner et al44
279
5%: 19% (3/16) (10 wks PT)
V: N/A
5%: 37% (19/51) (ET)**
V: 0% (0/57) (ET)
5% TIW (8 wks)
108
P, R, DB, VC
311
P, R, DB, VC
Edwards et al
46
Beutner et al43
1%: 21% (21/102) (ET)
5%: 50% (54/109) (ET)**
V: 11% (11/100) (ET)
Clearance+
Regimen (total duration)
# patients
Design
Author
Table 1. Efficacy of imiquimod on external genital warts.
External anogenital warts were the first approved
indication for imiquimod (1997). There have been
a number of randomized, double-blinded, vehiclecontrolled trials testing topical imiquimod for this
indication (Table 1).43–46 Summing these four trials,
a total of 743 patients were studied. Three of the
4 studies tested 1% or 5% imiquimod given 3 times per
week.43,45,46 The fourth study by Beutner et al tested
1% or 5% imiquimod given daily.44 Total treatment
duration was 8–16 weeks. Complete clearance rates
ranged from 37%–70% for 5% imiquimod, 14%–21%
for 1% imiquimod, and 0%–11% for vehicle (p-values
for individual trials listed in Table 1). Recurrence
rates at 10–12 week post-treatment follow-up ranged
from 13%–19% for 5% imiquimod, 0%–17% for 1%
imiquimod, and 0%–10% for vehicle. Arican et al
conducted a longer, 6-month post-treatment followup and found that 6 of 6 patients, treated with 5%
imiquimod three times per week for 12 weeks, experienced recurrence.45
There are relatively few clinical trials comparing
imiquimod against other therapies used for external
anogenital warts. In a 2001 abstract, Romero-Sanchez
et al reported results of a prospective, randomized,
double-blinded trial with a total of 110 men.47 Half
the men were assigned to 5% imiquimod applied three
times per week for 16 weeks, and the other half were
assigned to 1% 5-fluorouracil (5-FU) applied three
times per week for 16 weeks. Fifty-eight percent of
the imiquimod group experienced complete clearance after a mean of 12 weeks, compared to 36% of
the 5-FU group after a mean of 13 weeks (p 0.05).
At 12 weeks post-treatment follow-up, sustained clearance rates were 56% in the imiquimod group and
36% in the 5-FU group.
In 2006, Schofer et al reported a prospective, randomized, open-label trial comparing imiquimod versus
ablative therapy for external anogenital warts.48 Three
hundred and fifty-eight patients were randomized to
one of three arms: ablation alone, 5% imiquimod
cream three times a week for up to 16 weeks, or combined therapy with ablation and 5% imiquimod cream
Recurrence^
External anogenital warts
1% or 5% TIW (16 wks)
basal cell carcinoma, imiquimod’s efficacy has been
tested in a number of other dermatologic diseases.
We present the data behind the approved indications
first, with the other studies to follow.
1%: 0% (0/18) (12 wks PT)
5%: 13% (6/45) (12 wks PT)
V: 10% (1/10) (12 wks PT)
Topical imiquimod: mechanism of action and clinical uses
1561
1562
*p 0.01 relative to vehicle. **p 0.001 relative to vehicle. ***p 0.0001 relative to vehicle. ºComplete clearance defined as negative biopsy and no clinical lesions in treatment area.
×
Complete clearance defined as no clinical lesions in treatment area. &2nd 4-week course entered only if no clearance after 4 week rest period. ^Percentages calculated from patients with
complete clearance only.
Abbreviations: P, prospective; R, randomized; DB, double-blinded; VC, vehicle-controlled; BIW, 2x/week; TIW, 3x/week; V, vehicle; PT, post-treatment; C1, 1st 4-week course of 5%
imiquimod; C2, 2nd 4-week course of 5% imiquimod; NR, not recorded.
5%: 39% (23/59)
(1 yr)
V: 57% (8/14)
(1 yr)
5%: 27% (33/123) (4 wks post-C1)
V: 4% (5/123) (4 wks post-C1)
5%: 54% (66/123) (8 wks post-C2)***
V: 15% (18/123) (8 wks post-C2)
Jorizzo et al50,×
P, R, DB, VC
246
5% TIW (4 wks)
Rest (4 wks)
5% TIW (4 wks)&
NR
5%: 37% (48/129) (8 wks post-C1)***
V: 1% (1/130) (8 wks post-C1)
5%: 55% (71/129) (8 wks post-C2)***
V: 2% (3/130) (8 wks post-C2)
259
P, R, DB, VC
Alomar et al49,º
5% TIW (4 wks)
Rest (4 wks)
5% TIW (4 wks)&
NR
5%: 48% (117/242) (8 wks PT)**
V: 7% (18/250) (8 wks PT)
492
P, R, DB, VC
Korman et al51,×
5% TIW (16 wks)
NR
5%: 45% (97/215) (8 wks PT)**
V: 3% (7/221) (8 wks PT)
436
Lebwohl et al
P, R, DB, VC
5% BIW (16 wks)
Complete clearance
Regimen (total duration)
# patients
Design
52,×
Imiquimod 5% was approved for treatment of
actinic keratosis (AK) in 2004. Four randomized,
double-blinded, vehicle-controlled trials addressing
this indication are summarized in Table 2.49–52 A total
of 1433 patients with AK of the face and balding
scalp were included in these trials. Two of the trials
designed treatment regimens divided into two 4-week
courses of 5% imiquimod three times a week,
separated by a 4-week rest period.49,50 Total treatment
duration ranged from 4 to 16 weeks. Complete clearance rates ranged from 45%–55% for 5% imiquimod
and 2%–15% for vehicle (p-values for individual
trials listed in Table 2). Jorizzo et al conducted a
1-year post-treatment follow-up and found recurrence rates of 39% in the 5% imiquimod group and
57% in the vehicle group.50
A study by Tanghetti and Werschler compared 5%
imiquimod with 5% 5-FU in a prospective, randomized trial of 36 patients with AK lesions on face or
balding scalp.53 Patients received either 5% 5-FU
Author
Actinic keratosis
Table 2. Efficacy of imiquimod on facial and balding scalp actinic keratoses.
(applied for 12 weeks after wound healing). Ablative
techniques included electrocautery, laser therapy,
liquid nitrogen, and surgical excision. At the end of
the treatment phase, patients undergoing ablation
alone had a 92% complete clearance rate, compared
to 65% in the imiquimod only group and 73% in the
combination therapy group (statistical significance
not reported). Patients with complete clearance were
followed up for a total of 6 months. At the 3 month
follow-up, 14 of 87 patients (16%) in the ablation
only group reported recurrence, compared to 6 of
96 patients (6%) in the imiquimod monotherapy
group and 6 of 72 patients (8%) in the combination
group (p 0.03 for ablation only vs. imiquimod
only; p = 0.142 for ablation only vs.combination).
By the 6 month follow-up, a total of 23 of 87 patients
(26%) in the ablation only group had reported
recurrence. This was compared with 6 of 95 patients
(6%) in the imiquimod monotherapy group and 6 of
71 patients (8%) in the combination group (p 0.004
comparing ablation only group to either imiquimod
group). Thus, imiquimod, either alone or in combination with ablative therapy, appears to have lower
initial clearance rates than ablation alone, but leads
to a statistically significant lower recurrence rate
at 6 months.
Recurrence^
Ryu and Yang
Clinical Medicine: Therapeutics 2009:1
Clinical Medicine: Therapeutics 2009:1
*p 0.05 relative to vehicle. **p 0.001 relative to vehicle. ***p 0.0001 relative to vehicle. +Complete clearance defined histologically. ºComplete clearance defined as no lesions clinically.
^Percentages calculated from patients with complete clearance only.
Abbreviations: P, prospective; R, randomized; DB, double-blinded; VC, vehicle-controlled; OL, open-label; NC, non-comparative; BID, twice a day; V, vehicle; PT, post-treatment; NR, not
recorded.
5%: 11% (18/163)
(5 yrs PT)
5%: 90% (163/182) (12 wks PT)
5% 5x/week (6 wks)
P, OL, NC
Gollnick et al56,º
182
NR
5%: 80% (67/84) (12 wks PT)**
V: 6% (5/82) (12 wks PT)
5% 7x/week (6 wks)
P, R, DB, VC
Schulze et al57,+
166
NR
7x/week: 79% (142/179) (12 wks PT)**
5x/week: 82% (152/185) (12 wks PT)**
V: 3% (11/360) (12 wks PT)
5% 7x/week (6 wks) or
5% 5x/week (6 wks)
P, R, DB, VC
Geisse et al54,+
724
BID: 100% (10/10) (6 wks PT)NR
Daily: 87% (27/31) (6 wks PT)***
5x/wk: 81% (21/26) (6 wks PT)***
3x/wk: 52% (15/29) (6 wks PT)**
V: 19% (6/32) (6 wks PT)
5% BID (12 wks) or
5% daily (12 wks) or
5% 5x/week (12 wks) or
5% 3x/week (12 wks)
128
P, R, DB, VC
Geisse et al55,+
# patients
Design
Author
Superficial basal cell carcinoma (sBCC) is the third
and most recently approved indication for imiquimod
(2005). A number of prospective, randomized, doubleblinded, placebo-controlled trials have shown 5%
imiquimod to be superior to the natural course of the
disease (Table 3).55–58 Twelve hundred total patients
were included in these trials. Treatment regimens
included 3 times per week, 5 times per week, once
daily, and twice daily. Treatment duration ranged
from 6–12 weeks. Complete clearance rates, defined
histologically or clinically, ranged from 52%–100%
for 5% imiquimod-treated patients and 3%–19%
for the vehicle group (p-values for individual trials
listed in Table 3). The 100% clearance rate occurred
in 10 patients receiving 5% imiquimod twice daily.56
Gollnick et al performed a 5-year post-treatment
follow-up and found a recurrence rate of 11%.57
In 2002, Shumack et al evaluated imiquimod’s
efficacy in the treatment of nodular BCC (nBCC).59
They performed two trials, the first of which was a
prospective, open-label, non-controlled study of
99 patients. This trial assigned patients to one of four
Table 3. Efficacy of imiquimod on superficial basal cell carcinoma.
Basal cell carcinoma
Regimen
(total duration)
Complete clearance
Recurrence^
cream twice daily for 2–4 weeks or 5% imiquimod
cream twice weekly for 16 weeks. At week 24, 84%
of patients in the 5-FU group experienced complete
clearance, compared with 24% of imiquimod-treated
patients (p 0.01).
In another comparative study, Krawtchenko et al
also found that 5-FU was more efficacious initially
than imiquimod, but in addition, they showed higher
sustained clearance rates with imiquimod than 5-FU.54
In this study, patients were randomized to one or two
courses of cryosurgery (20–40 seconds per lesion),
5% 5-FU (twice daily for 4 weeks), or one or two
courses of 5% imiquimod (three times per week for
four weeks each). 17 of 25 patients (68%) in the cryosurgery group, 23 of 24 patients (96%) in the 5-FU
group, and 22 of 26 patients (85%) in the imiquimod group experienced initial clearance (p < 0.05).
At 12-month follow-up, 1 of 25 patients (4%) in the
cryosurgery group, 8 of 24 patients (33%) in the 5-FU
group, and 19 of 26 patients (73%) in the imiquimod
group had sustained clearance of the total treatment
field (p < 0.01). These data suggest that imiquimod
has more long-term efficacy against AK lesions than
either cryosurgery or topical 5% 5-FU.
NR
Topical imiquimod: mechanism of action and clinical uses
1563
Ryu and Yang
dosing regimens: once daily for 3 or 7 days per week,
or twice daily for 3 or 7 days per week. The total
duration of treatment was 6 weeks. The second trial
was a prospective, randomized, double-blinded,
vehicle-controlled trial of 92 patients. Patients in this
trial applied either 5% imiquimod or vehicle once daily
for 3, 5, or 7 days per week, or twice daily for 7 days
per week. Unlike the first trial, total treatment duration
during this trial was 12 weeks. In both of these trials,
5% imiquimod once daily for 7 days per week was
the most efficacious regimen, with 25 of 35 patients
(71%) in the 6-week trial and 16 of 21 patients (76%)
in the 12-week trial showing complete clearance of
tumor on this regimen (p 0.001 for 5% imiquimod
once daily vs. vehicle in 12-week trial). Enrollment
into the twice daily, 7 days per week regimen was
halted shortly after study initiation because of severe
local skin reactions. Therefore, only a small number
of patients were randomized to this group (1 patient in
the 6-week trial, and 4 patients in the 12-week trial).
The single patient in the 6-week trial failed to respond
completely to imiquimod, and 3 of 4 patients in the
12-week trial were complete responders.
Several studies in the literature address the role
of imiquimod as adjunct therapy in the treatment of
BCC. In 2006, Spencer et al reported a randomized,
prospective, double-blind, vehicle-controlled study of
20 patients with nBCC.60 These patients were randomized to three cycles of curettage and electrodessication (C&D), followed by either 5% imiquimod
or vehicle cream once daily for 1 month. At 8 weeks
post-treatment follow-up, 10% of the adjunct imiquimod group experienced recurrent tumor, compared to
40% of the placebo group (statistical significance not
reported). Rigel et al performed a prospective, noncontrolled study of 57 patients with nBCC or sBCC.61
These patients were treated initially with curettage
alone, followed by 5% imiquimod 5 times per week
for 6 weeks. At 1 year follow-up, none of the patients
demonstrated residual BCC.
Non-genital, cutaneous warts
Several trials have explored imiquimod’s efficacy
in non-genital warts. In 2000, Hengge et al reported
a prospective, open-label, non-comparative trial of
50 patients with cutaneous warts resistant to previous
therapies, including salicylic acid, local surgery, cryotherapy, laser vaporization, electrodessication, trichlo1564
roacetic acid (TCA), intralesional interferon, and X-ray
treatment.62 Of the 50 patients, 20 had warts on their
hands, 16 on their feet, 10 on their face, and 4 were
disseminated. Imiquimod 5% was applied five days per
week for up to 16 weeks or complete clearance. Fifteen
of 50 patients (30%) experienced complete clearance, while 13 patients (26%) experienced a 50%
reduction in wart area after a mean treatment period
of 9.2 weeks. Stratification by lesion site revealed that
response rates (partial and complete combined) were
higher on the trunk, face, and hands (75%, 70%, and
60%, respectively) than on the feet (37.5%).
In 2002, Grussendorf-Conen et al reported
a prospective, open-label, non-comparative trial of
37 patients with resistant cutaneous warts (mean duration 6.3 years).63 Warts were located on the hands and/
or feet of 36 of 37 patients; the last patient had warts
on the knee. Imiquimod 5% was self-applied twice
daily for 24 weeks or complete clearance. 10 of 37
patients (27%) cleared completely, 18 patients (49%)
showed a 50% reduction in wart area, and 5 patients
(14%) showed a 50% reduction.
Herpes simplex virus
In a prospective, randomized, double-blinded, placebocontrolled trial, Schacker et al investigated whether
imiquimod could alter the natural history of HSV-1
and/or 2 infections.64 This study included 124 patients
with genital herpes (both HSV-1 and HSV-2 subtypes
included) who had at least 6 recurrences per year.
Patients in the midst of a recurrence applied either
5% imiquimod or vehicle once, twice, or three times
weekly for a total of 3 weeks. A 16-week observation
period followed the treatment period. The primary
endpoint was median time to next recurrence after
treatment. Median time to recurrence was 53, 54,
60, and 64 days for placebo, imiquimod once, twice,
and three times per week, respectively (no statistical
significance between groups). Despite a slight trend
towards increased time to recurrence, 5% imiquimod
appears to have no clear effect on HSV recurrence
when dosed and applied in this manner.
Molluscum contagiosum
Several randomized, prospective, double-blinded,
placebo-controlled trials have tested topical imiquimod in children (ages 1–12) with molluscum contagiosum.8,65,66 Imiquimod 5% was applied three times
Clinical Medicine: Therapeutics 2009:1
Topical imiquimod: mechanism of action and clinical uses
per week for up to 12 weeks in the Theos et al trial
or 16 weeks in the other two trials, conducted by 3M.
Theos et al found that 4 of 12 imiquimod-treated
patients (33%) completely cleared versus 1 of 11 (9%)
in the placebo group at the end of the 12-week treatment period (statistical significance not reported).
The two 3M-conducted trials, though larger in scope
(n = 323 and 379, respectively), found no statistically
significant difference between imiquimod and placebo
(clearance in 24% of imiquimod group and 26%–28%
of placebo group).
Squamous cell carcinoma in situ
Squamous cell carcinoma in situ (SCCIS) has
been identified as a possible therapeutic target for
imiquimod. In 2006, Patel et al conducted a randomized,
prospective, double-blinded, placebo-controlled study
of 31 patients with biopsy-proven SCCIS.67 Patients
applied either 5% imiquimod or vehicle cream daily
for up to 16 weeks and were assessed at 28 weeks.
Eleven of 15 patients (73%) in the imiquimod
group achieved complete clearance, compared with
0% of the placebo group (p 0.001). In addition,
at 9 month follow-up, none of the eligible patients
showed recurrence of their disease.
Squamous cell carcinoma
In a 2005 abstract, Li et al reported a prospective,
non-controlled trial of 20 patients with invasive SCCs
receiving a combination of 5% imiquimod, tretinoin,
calcipotriene, diclofenac, and hydrocortisone valerate
as part of a protocol called OLCAT-005. This protocol
was initiated at two times per week and increased
to at least three times per week for 12 weeks. Dose
schedule per lesion was optimized by an Individualized Maximally Tolerated Dose (IMTD) regimen.68
At 12-week post-treatment follow-up, 33 of 35 lesions
(94%) showed complete histologic clearance, and
none of the cleared lesions showed recurrence at
5 years.
Melanoma
A few prospective, non-controlled trials have investigated a role for imiquimod in lentigo maligna.
Naylor et al assigned 30 patients with lentigo maligna
to 5% imiquimod once daily for 3 months.69 At the
1 month post-treatment follow-up, 26 of 28 evaluable
patients (93%) had complete histological clearance.
Clinical Medicine: Therapeutics 2009:1
Over 80% of the complete responders showed no
recurrence after 1 year. In smaller studies, Powell
et al used 5% imiquimod three times per week for
6 weeks, Fleming et al used 5% imiquimod daily for
6 weeks, and Wolf et al used 5% imiquimod daily
for up to 13 weeks. Powell et al reported complete
clearance in 10 of 12 patients (83%), Fleming et al in
4 of 6 patients (67%), and Wolf et al in 5 of 5 patients
(100%).70–72
In 2007, Green et al reported a prospective, noncontrolled trial of 10 patients with subcutaneous and
cutaneous melanoma metastases.73 Imiquimod 5% was
applied daily to the lesions for 4 weeks, followed by
5% imiquimod daily plus intralesional IL-2 injections
(0.36 million international units) three times per week
every two weeks for 4 weeks. This was followed by
imiquimod every other day for 4 weeks after lesion
disappearance, plus IL-2 three times per week every
4 weeks. A total of 182 lesions were treated, and
complete response to this regimen was observed in
74 lesions (40.7%). Ninety-one percent of the completely responding lesions were cutaneous.
Contrary to the moderate success reported by
Green et al Kowalzick and Eickenscheidt reported
the case of a 68-year old man with primary malignant
melanoma of the temple in whom topical imiquimod
was ineffective. Following excision of his primary
tumor, multiple cutaneous and subcutaneous metastases arose, and his disease progressed fatally despite
irradiation, chemotherapy, and topical imiquimod
three times a week. No intralesional therapy, however,
was given in this case.74
Vulvar and vaginal intraepithelial
neoplasia
Several prospective, non-controlled studies have
been performed to investigate the efficacy of imiquimod in vulvar intraepithelial neoplasia (VIN) (grade
2/3) and vaginal intraepithelial neoplasia (VAIN).
Marchitelli et al assigned patients to 5% imiquimod
three times a week for up to 16 weeks and reported
the highest efficacy rates among these studies: 6 of
8 patients (75%) had complete clearance assessed
by colposcopy, and 2 of 8 patients (25%) had partial clearance (defined as 50% decrease in lesion
area).75 In addition, post-treatment histopathology
showed no evidence of VIN in 7 of 8 patients (88%).
Le et al reported that a 16 week course of therapy led
1565
Ryu and Yang
to complete histological response in 9 of 17 patients
(53%) and partial response in 5 of 17 (29%).76 Todd
et al reported a lower rate of response, with 4 of
15 patients (27%) showing clinical improvement after
16 weeks of therapy.77 Wendling et al reported a trial
of 12 patients, in which 3 of 12 (25%) achieved complete clearance and 4 of 12 (33%) partial response
(defined as 75% decrease in lesion size).78
In 2003, Buck and Guth reported a prospective,
non-controlled study in 56 women (42 available for
follow-up) with primarily low-grade VAIN.79 Of the
14 women lost to follow-up, one of them reported
vulvar excoriation as the reason for discontinuation; the other 13 discontinued for either unknown
or non-drug related reasons. These patients applied
0.25 g of cream into the vagina once a week for
3 weeks. Thirty-six of 42 patients (86%) showed
complete clearance by colposcopy at 1 week or later
after conclusion of treatment. Five patients cleared
after an additional cycle of therapy (total 2 cycles),
and the last patient cleared after 2 additional cycles
(total 3 cycles). Therefore, all women available for
follow-up eventually showed clearance of their VAIN
after 1–3 cycles of imiquimod topical therapy.
Infantile hemangioma
Mycosis fungoides
Pyogenic granuloma
A small prospective, randomized, double-blinded,
vehicle-controlled trial by Chong et al studied
imiquimod’s effects in mycosis fungoides.80 This trial
included only 4 patients with mycosis fungoides;
3 were assigned to imiquimod once daily for
16 weeks, and the remaining patient was assigned to
vehicle. In the imiquimod cohort, mean surface area
decreased by 9% on imiquimod-treated lesions and
increased by 40% on untreated control lesions (statistical
significance not reported). Within the placebo group,
mean lesion surface area increased by 40%.
Kaposi’s sarcoma
Celestin-Schartz et al conducted a prospective,
open-label, non-comparative trial of 17 human immunodeficiency virus (HIV)-negative patients (14 males,
3 females) with classic or endemic Kaposi’s sarcoma.81
Patients applied 5% imiquimod cream under occlusion
three times a week for 24 weeks. At 36 weeks, 2
of 17 patients (12%) had a complete response and
6 of 17 (35%) had a partial response. Six of 17 patients
(35%) experienced tumor progression.
1566
McCuaig et al conducted a prospective, open-label,
non-comparative trial of 16 infants (mean age
4.1 months) with previously untreated, non-ulcerated
superficial or mixed infantile hemangioma.82 Imiquimod
5% was applied 3 to 7 times per week for 16 weeks.
Lesions were assessed at the end of the 16 week
treatment as well as at 16 weeks post-treatment.
No changes in mean lesion area, volume, depth, or elevation were observed at either timepoint. Erythema was
significantly improved at the 16-week post-treatment
timepoint compared to baseline (p 0.01).
In a prospective, non-comparative trial, Welsh et al
treated 10 infants with infantile hemangiomas with
5% imiquimod 5 days per week for up to 16 weeks.83
Four of the 10 infants (40%) had complete resolution
of their lesions, another 4 infants (40%) experienced
partial resolution, 1 infant did not respond to therapy
(10%), and the remaining infant discontinued at
3 weeks in order to receive microembolizaton. A recent
case series of 5 infants by Barry et al reported similar
results.84 Two of the 5 infants (40%) had a complete
response, 2 (40%) had a partial response and 1 had
no response to treatment.
A number of case reports describe imiquimod’s efficacy
for pyogenic granuloma. The largest of these reports
describes 5 children (ages 6 months to 4 years) treated
with 5% imiquimod cream.85 Three of the children
were treated daily; one was treated daily for 1 week
and then every other day for 4 more applications;
the fifth child was treated three times a week. The
duration of treatment ranged from 2–4 weeks, and
all 5 children experienced full resolution of their
pyogenic granuloma during this period.
Adults with pyogenic granuloma appear to benefit
from imiquimod as well. A report by Georgiou
et al described an 82-year old man with recurrent
pyogenic granuloma on his hand that was treated with
5% imiquimod twice daily for 3 weeks. At 8 month
follow- up, he had no evidence of recurrence.86
Skin diseases in immunosuppressed
patients
Because imiquimod is thought to work primarily
by stimulating innate and adaptive immunity, its
efficacy in immunosuppressed patients has been
Clinical Medicine: Therapeutics 2009:1
Topical imiquimod: mechanism of action and clinical uses
an interesting point of study. In 1999, Gilson et al
reported a prospective, randomized, double-blinded,
vehicle-controlled study of 100 HIV-positive
patients (97 men and 3 women) with external anogenital warts across 13 institutions in the United
Kingdom and United States.87 These patients were
randomized to either 5% imiquimod or vehicle
cream, three times per week for up to 16 weeks.
Inclusion criteria were age 18 years, CD4 count
100 cells/µL, and Karnofsky score 70. Eleven
percent of imiquimod treated patients demonstrated
complete clearance of their warts, compared to 6%
of placebo patients (p = 0.488). Although complete
clearance was not significantly different for the
imiquimod group, imiquimod-treated patients did
demonstrate a higher rate of partial clearance (50%
reduction in wart area) than placebo patients (38% vs.
14% respectively; p 0.05). Overall, these results
support the model that imiquimod is less effective
in the context of HIV.
Transplant patients represent another cohort in
which immunosuppression could hinder imiquimod’s
effects. A randomized, prospective, double-blinded,
vehicle-controlled study by Ulrich et al investigated the safety of imiquimod in 43 transplant
patients (kidney, heart, or liver) with AK on the face
or balding scalp. Patients applied 5% imiquimod
or vehicle cream three times a week for 16 weeks,
regardless of lesion clearance. At 8 weeks post-treatment
follow-up, 18 of 29 patients (62%) treated with imiquimod experienced complete clearance, compared
to 0 of 14 patients treated with vehicle (statistical
significance not reported).88
In another prospective, randomized, doubleblinded, placebo-controlled trial, Brown et al studied
imiquimod in 20 renal transplant patients at high risk
of skin cancer, as predicted by skin type, previous sun
exposure, and time since transplantation.89 Patients
were required to have equivalent areas of viral warts,
actinic keratoses, or other premalignant skin lesions
(assessed clinically) on both dorsal forearms or
hands. The patients applied either 5% imiquimod or
vehicle cream to lesions on one dorsal forearm/hand
three times per week for up to 16 weeks. The other
forearm/hand served as an untreated internal control.
At week 16, 5 of 14 imiquimod-treated patients (36%)
showed reduced histologic dysplasia at the treatment site relative to the untreated contralateral side.
Clinical Medicine: Therapeutics 2009:1
One of 6 patients (17%) in the vehicle group showed
reduced histologic dysplasia (p = 0.32 for imiquimod
vs. vehicle groups). In addition, 7 of 14 imiquimodtreated patients (50%) had reduced non-genital warts,
compared with 0 of 6 placebo patients (p 0.05).
Imiquimod still seems to be effective in transplant
patients.
Leishmaniasis
Several studies have examined the efficacy of imiquimod for leishmaniasis infection. Firooz et al performed
a prospective, randomized, assessor-blind, vehiclecontrolled trial of 119 patients across 2 primary
health clinics.90 All patients were treated daily with
20 mg/kg of meglumine antimoniate, given intramuscularly for 14 days. In addition, patients were
randomized to receive either 5% imiquimod or
placebo cream 3 times per week for 4 weeks. At four
weeks after the end of treatment, 26 of 59 imiquimodtreated patients (44.1%) and 29 of 60 placebo patients
(48.3%) showed clinical cure, revealing no therapeutic benefit of imiquimod over meglumine antimoniate
alone (p = 0.64).
In contrast, another randomized, prospective,
double-blind, placebo-controlled trial did show a
benefit with imiquimod. Miranda-Verastegui et al
assigned 40 patients to meglumine antimoniate
(20 mg/kg) daily for 20 days plus either 5% imiquimod
or vehicle cream every other day for 20 days.91 At
1 month post-treatment follow-up, 50% of the
imiquimod group achieved cure, compared to 15%
of the vehicle group (p 0.02). At 3 months posttreatment, 72% of the imiquimod group and 35% of
the vehicle group had achieved cure (p 0.02).
Keloids/scars
Based on its ability to induce IFN-α, several
small studies have examined imiquimod use in
the prevention of keloid recurrence. Berman and
Kaufman performed a non-comparative pilot study
of 12 patients with 13 keloids (12 on the earlobe,
1 on the back).92 The patients’ keloids were excised,
and starting the night of excision, imiquimod 5%
cream was applied daily for 8 weeks. At 16 weeks
post-treatment, 11 of 11 assessed keloids had not
recurred. In contrast, Cação et al examined 9 patients
with keloids on the trunk who were treated with
surgical excision and application of imiquimod 5%
1567
Ryu and Yang
cream daily for 8 weeks.93 One patient was lost to
follow-up, and all 8 of the remaining patients experienced recurrence by 20 weeks post-excision. Larger
scale studies are required, and the varied success
rates may reflect differences in resection location.
Regarding imiquimod’s potential role in scar
reduction and cosmesis, Berman et al conducted a
prospective, randomized, double-blinded, vehiclecontrolled trial of 18 patients, each with two skin
lesions diagnosed as melanocytic nevi in a similar
anatomic area of skin.94 Each patient underwent
surgical excision of both lesions; one lesion was
treated with 5% imiquimod daily for 4 weeks,
and the other was treated with vehicle. At week 8,
investigators rated the wounds on overall cosmesis,
erythema, induration, and pigmentary alteration.
Vehicle-treated wounds received significantly better
cosmesis and erythema scores than imiquimodtreated lesions (p 0.01). Vehicle-treated lesions
also scored more favorably for induration and pigmentary alteration, but to a lesser degree (p = 0.065
and 0.021, respectively).
Safety and Tolerability
Several large studies of imiquimod’s local and
systemic tolerability exist for its approved indications
(external genital warts, actinic keratosis, superficial
basal cell carcinoma). The results of these safety
studies are summarized in Tables 4, 5, and 6.
Summary of safety trials
Across indications, the most common local skin reaction
(LSR) assessed by investigators was erythema. Sixty
seven to 82% of patients with external genital warts,
97%–98% of patients with AK, and 90%–100% of
patients with sBCC experienced this reaction.43,44,46,49–
52,55,56,58
Other commonly-experienced LSRs included
excoriation/flaking, erosion/ulceration, edema, scabbing, and induration. Vesicles were less common than
the other reactions, ranging from 5% of patients
with external genital warts in one study to 37% of
patients with AK in another study.46,49
Interestingly, there was a greater rate of certain
LSRs in patients with AK or sBCC relative to
those with external genital warts. Among AK
patients, the rates of erythema, excoriation/flaking,
and scabbing were 97%–98%, 93%–95%, and
79%–88%, respectively. Among sBCC patients, the
analogous rates were 90%–100%, 80%–91%, and
83%–85%. Among patients with external genital
warts, these rates were substantially lower: 67%–82%
for erythema, 25%–42% for excoriation/flaking, and
15%–34% for scabbing. It is difficult to attribute this
difference to application frequency, as part of the data
for external genital warts came from a study which
used 5% imiquimod daily for 16 weeks.44 Other possible causes of this difference include anatomic site,
nature of the skin lesion, and demographic differences
between the study populations.
Regarding patient-reported adverse events, the
most common local adverse event was application
site reaction. In particular, itching was most commonly reported, with 16%–62% of all imiquimodtreated patients reporting this symptom at some time.
In addition, pain, burning, and bleeding at the target
site were reported to a lesser degree.
Systemic adverse events (SAEs), including flu-like
symptoms, were minimal. In their trial, Beutner et al
Table 4A. Safety of imiquimod on external genital warts—Local site reactions assessed by investigator.
Edwards et al46
5% IMI (106)/vehicle (95)
Beutner et al44
5% IMI (92)/vehicle (92)
Erythema
67%/24%
82%/37%
Excoration/Flaking
25%/2%
42%/15%
Erosion
32%/8%
48%/5%
Edema
16%/1%
39%/3%
Scabbing
15%/2%
34%/5%
Induration
9%/3%
24%/3%
Ulceration
5%/5%
13%/0%
Vesicles
5%/5%
8%/0%
1568
Clinical Medicine: Therapeutics 2009:1
Topical imiquimod: mechanism of action and clinical uses
Table 4B. Safety of imiquimod on external genital warts—
Local site reactions reported by patient.
Beutner
et al43*
5% IMI (48)
Beutner et al44
5% IMI (92)/
vehicle (92)
Itching
54%
33%/19%
Pain
8%
35%/2%
Burning
31%
16%/1%
Tenderness
13%
12%/2%
*No values reported for vehicle.
reported the most common SAE to be headache (29%)
and upper respiratory tract infection (14%).44 Consis­
tent with this, Geisse et al also reported headache
as the most common SAE (8%), followed by back
pain (4%), upper respiratory tract infection (3%),
rhinitis (3%), and lymphadenopathy (3%).55 Lebwohl
et al reported upper respiratory tract infection in 15%,
sinusitis in 7%, and headache in 5%.52 This group
also described changes in hemoglobin and platelet
levels but did not specify how many patients this
affected or the degree of change. Jorizzo et al qualitatively reported one patient with a transient fall in
leukocytes and absolute neutrophil count (ANC).50
Safety in immunosuppressed patients
The previously cited study by Ulrich et al investigated
the safety of imiquimod in 43 transplant patients
(kidney, heart, or liver) with AK on the face or balding
scalp. Patients applied 5% imiquimod or vehicle
cream three times a week for 16 weeks, regardless
of lesion clearance. No graft rejections or laboratory
abnormalities were found in the imiquimod group
throughout the 16-week course of therapy. Though
skin reactions were evaluated at 8 weeks posttreatment, no mention was made of graft evaluation
at this timepoint.88
Table 4C. Safety of imiquimod on external genital warts—
Systemic reactions.
Beutner et al44
5% IMI (92)/vehicle (92)
Headache
29%/33%
Upper Respiratory Tract
Infection
14%/27%
Abbreviation: IMI—imiquimod.
Clinical Medicine: Therapeutics 2009:1
Another retrospective study of 24 transplant patients
(18 kidney, 4 kidney-pancreas, and 2 heart) tested
the safety of imiquimod in treating warts, AK, and
bowenoid papulosis.95 Imiquimod 5% was applied
three times a week over a median of 9 weeks. All measures of graft function were normal.
Reportable adverse reactions
Several case reports describe imiquimod-induced
exacerbations of previously controlled skin diseases.
In one report, Yang et al described a 67-year old
man who developed fever, myalgias, fatigue, and
exacerbation of pityriasis rubra pilaris (PRP)
after a 2-week application of imiquimod three
times per week to focal areas on the scalp and right
cheek.96
Similar exacerbations of psoriasis have been
reported in the literature. Gilliet et al reported a
58-year old man who received 5% imiquimod daily
for a single psoriatic plaque on his back.97 Over the
next 10 weeks, his lesion increased 4-fold in size
and was associated with new smaller plaques on
his back and legs. Rajan et al described a 64-year
old woman with long-standing, well-controlled
psoriasis who began treating sBCC lesions on
her trunk with 5% imiquimod daily.98 By the fifth
week, she had developed psoriatic plaques both at
the treatment site as well as distantly on her legs.
Interestingly, both Gilliet et al and Rajan et al
describe psoriatic eruptions at sites distant from
imiquimod application.
Three case reports describe the appearance of
pemphigus-like lesions with imiquimod use.99–101
The first patient treated two sBCCs on her back
and shoulder with 5% imiquimod 5 days per
week and within two weeks developed vesicles
and crusts at the treatment site as well as on her
neckline and lips; biopsy of the neckline showed
an intraepidermal acantholytic blister consistent
with pemphigus vulgaris.99 The second patient used
imiquimod for high grade VIN and experienced
blistering of her vulva; biopsy of her vulva revealed
an intraepidermal blister with suprabasal separation.100 The third patient applied 5% imiquimod daily
to a suspected sBCC on her face and discontinued
after 2 months because of redness and pain. 6
months after starting treatment, a biopsy revealed
pemphigus foliaceus.101
1569
Ryu and Yang
Table 5A. Safety of imiquimod on actinic keratoses—Local site reactions assessed by investigator.
Lebwohl et al52
5% IMI (215)/vehicle (220)
Korman et al51
5% IMI (242)/vehicle (250)
Alomar et al49
5% IMI (129)/vehicle (130)
Erythema
97%/93%
98%/88%
97%/71%
Excoration/Flaking
93%/91%
95%/84%
94%/74%
Scabbing
79%/42%
87%/44%
88%/50%
Erosion/Ulceration
48%/9%
NR
74%/17%
Edema
49%/10%
NR
70%/8%
Weeping/Exudate
22%/1%
NR
64%/5%
Induration
NR
NR
NR
Vesicles
9%/1%
NR
37%/1%
Conclusions: Current and Future
Roles of Imiquimod
To date, the FDA has approved three indications for
imiquimod: clinically typical, nonhyperkeratotic
actinic keratoses on the face or scalp of
immunocompetent adults; biopsy-confirmed, primary
superficial basal cell carcinoma in immunocompetent
adults with a maximum tumor diameter of 2.0 cm
on the trunk, neck, or extremities (excluding hands
and feet), only when surgical methods are less appropriate and follow-up can be assured; and external
genital and perianal warts in patients 12 years and
older.
The approved therapeutic regimen for each of these
indications is as follows: AK – 5% cream 2 times per
week for 16 weeks; sBCC – 5% cream 5 times per week
for 6 weeks; external genital warts – 5% cream 3 times
per week until total clearance or up to 16 weeks.
The superiority of imiquimod over placebo has
been well established for each of these indications.
Regard­ing AK, the trial using the approved regimen
(2 times per week for 16 weeks) reported complete
clearance rates of 45% in imiquimod-treated patients
compared to 3% in the placebo group at 8-week
post-treatment follow-up.52 A three times per week reg­
imen for 16 weeks resulted in similar clearance rates
(48% imiquimod vs. 7% placebo).51 Two studies using
three times per week dosing for two 4-week courses
separated by a 4-week rest period cited 54%–55%
overall clearance in imiquimod groups compared to
2%–15% in placebo groups.49,50 For sBCC, the app­r­
oved regimen (5 times per week/6 weeks) resulted in
Table 5B. Safety of imiquimod on actinic keratoses—Local site reactions reported by patients.
Itching at target site
Burning at target site
Bleeding at target site
Stinging at target site
Induration at target site
Pain at target site
Tenderness at target site
Infection at target site
Burning at remote site
Induration at remote site
Tenderness at remote site
1570
Lebwohl et al52
5% IMI (215)/vehicle (221)
21%/8%
6%/2%
3%/1%
3%/1%
2%/1%
2%/1%
2%/1%
NR
2%/0%
NR
NR
Korman et al51
5% IMI (242)/vehicle (250)
29%/4%
7%/1%
NR
1%/0%
NR
4%/0%
2%/1%
2%/0%
2%/0%
1%/0%
1%/0%
Clinical Medicine: Therapeutics 2009:1
Topical imiquimod: mechanism of action and clinical uses
Table 5C. Safety of imiquimod on actinic keratoses—
Systemic reactions.
Lebwohl et al52
5% IMI (215)/vehicle (221)
Upper Respiratory
Tract Infection
15%/12%
Sinusitis
7%/6%
Headache
5%/3%
Squamous Cell
Carcinoma
4%/2%
Diarrhea
3%/1%
Eczema
2%/1%
Back Pain
1%/1%
Fatigue
1%/1%
Atrial Fibrillation
1%/1%
Viral Infection
1%/1%
Dizziness
1%/1%
Vomiting
1%/1%
Urinary Tract Infection
1%/1%
Fever
1%/0%
Rigors
1%/0%
Abbreviation: IMI, imiquimod.
clearance rates of 82%–90% for the imiquimod groups
versus 3% for the placebo groups.55,57 A maximum
clearance rate of 100% was achieved with twice per
day dosing over 12 weeks.56 For external genital
warts, the approved regimen (3 times per week for
up to 16 weeks) achieved a clearance rate of 50%
in the imiquimod group compared to 11% in the
vehicle group.46 In a second study, treating at the
same frequency for only 8 weeks led to a lower
clearance rate (37%), while a third study reported a
70% clearance rate with three times per week dosing
for a total of 12 weeks.43,45 A fourth study suggested
that daily dosing did not add significant benefit, with
a complete clearance rate of 52%.44
For all these indications, the next vital piece of
information is how imiquimod directly compares
to other standard therapies with regard to long-term
clinical efficacy, financial cost, ease of use, and side
effect profile. Unfortunately, the literature addressing
this question is scarce. One study compared 5%
imiquimod with 5% 5-FU in 36 patients with AK
and found that complete clearance rates were much
higher in the 5-FU group (84% vs. 24%).53 However,
Krawtchenko et al showed that 5% imiquimod has
significantly higher sustained clearance rates at
12-month follow-up than 5% 5-FU (73% vs. 33%).54
Another study concerning external anogenital warts
compared 5% imiquimod with 1% 5-FU and found
no statistically significant difference, although there
was a trend towards increased clearance rates in
the imiquimod group (56% sustained clearance in
imiquimod group vs. 36% in 5-FU group at 12 week
follow-up).47
In short, the current literature firmly supports
imiquimod’s treatment success compared to the natural
evolution of AK, sBCC, and external anogenital
warts, but does not offer much help to clinicians
in deciding between imiquimod and concurrent
therapies. In theory, imiquimod seems an attractive
choice, with substantive clearance rates, ease of
patient use, avoidance of invasive techniques, and
Table 6A. Safety of imiquimod on superficial basal cell carcinoma—Local site reactions assessed by investigator.
Geisse et al55*
5x per wk (26)/vehicle (32)
Geisse et al54
5x per wk (184)/vehicle (178)
Erythema
90%/90%
100%/97%
Excoration/Flaking
80%/50%
91%/76%
Erosion
65%/15%
66%/14%
Edema
70%/15%
78%/36%
Scabbing
85%/40%
83%/34%
Induration
70%/45%
84%/53%
Ulceration
40%/10%
40%/3%
Vesicles
20%/0%
31%/2%
*estimates based on bar graph data.
Clinical Medicine: Therapeutics 2009:1
1571
Ryu and Yang
Table 6B. Safety of imiquimod on superficial basal cell carcinoma—Local site reactions reported by patients.
Geisse et al55
5x per wk (26)/vehicle (32)
Geisse et al54
5x per wk (185)/vehicle (179)
Schulze et al57
5% IMI (84)/vehicle (82)
Itching at target site
62%/13%
16%/1%
23%/0%
Burning at target site
NR
6%/1%
10%/0%
Pain at target site
8%/0%
3%/0%
NR
Tenderness at target site
8%/6%
1%/0%
NR
Bleeding at target site
NR
2%/0%
NR
Infection at target site
NR
1%/0%
NR
Table 6C. Safety of imiquimod on superficial basal cell carcinoma—Systemic reactions.
Headache
Back pain
Upper Respiratory Tract Infection
Gastrointestinal
Rhinitis
Lymphadenopathy
Fatigue
Sinusitis
Dyspepsia
Coughing
Fever
Dizziness
Anxiety
Pharyngitis
Chest Pain
Nausea
Geisse et al54
5x per wk (185)/vehicle (179)
8%/2%
4%/1%
3%/1%
NR
3%/1%
3%/1%
2%/1%
2%/1%
2%/1%
2%/1%
2%/0%
1%/1%
1%/1%
1%/1%
1%/0%
1%/0%
relatively benign toxicity profile. In order to make this
a more quantitative decision, however, head-to-head,
randomized, prospective, double-blinded trials are
necessary.
In addition to the three current indications for
imiquimod, it seems reasonable to assume that further
therapeutic targets could be approved in the future.
In several of the skin disorders mentioned previously,
off-label use of imiquimod for non-genital warts,
SCCIS, SCC, VIN/VAIN, melanoma, and pyogenic
granulomas may be useful. Other creative applications
for imiquimod have started to emerge in the literature
as well. For example, its potential use as a vaccine
adjuvant for infectious pathogens and tumors makes
1572
Schulze et al57
5% IMI (84)/vehicle (82)
6%/1%
NR
5%/6%
6%/1%
NR
NR
NR
NR
NR
NR
NR
NR
NR
NR
NR
NR
theoretical sense and has been supported by several
preclinical studies.102,103 As the first commercially
available TLR agonist, imiquimod has vividly
demonstrated the broad applicability of this novel
class of agents. It should continue to advance disease
therapy, both by its own efficacy as well as by serving
as a molecular blueprint upon which to create further
derivatives. Resiquimod, one such derivative that
is available orally as well as topically, has already
shown promise with its own distinct molecular and
therapeutic profile.
Disclosures
The authors report no conflicts of interest.
Clinical Medicine: Therapeutics 2009:1
Topical imiquimod: mechanism of action and clinical uses
References
1. Hurwitz DJ, Pincus L, Kupper TS. Imiquimod: a topically applied
link between innate and acquired immunity. Arch Dermatol. 2003
Oct;139(10):1347–50.
2. Miller RL, Gerster JF, Owens ML, Slade HB, Tomai MA. Imiquimod
applied topically: a novel immune response modifier and new class of drug.
Int J Immunopharmacol. 1999 Jan;21(1):1–14.
3. Sauder DN. Immunomodulatory and pharmacologic properties of imiquimod.
J Am Acad Dermatol. 2000 Jul;43(1 Pt 2):S6–11.
4. Schon M, Schon MP. The antitumoral mode of action of imiquimod and
other imidazoquinolines. Curr Med Chem. 2007;14(6):681–7.
5. Salasche S, Shumack S. A review of imiquimod 5% cream for the treatment of various dermatological conditions. Clin Exp Dermatol. 2003 Nov;
28 Suppl 1:1–3.
6. Tyring S, Conant M, Marini M, Van Der Meijden W, Washenik K.
Imiquimod; an international update on therapeutic uses in dermatology.
Int J Dermatol. 2002 Nov;41(11):810–6.
7. Edwards L. Imiquimod in clinical practice. J Am Acad Dermatol. 2000
Jul;43(1 Pt 2):S12–7.
8. Wagstaff AJ, Perry CM. Topical imiquimod: a review of its use in the
management of anogenital warts, actinic keratoses, basal cell carcinoma
and other skin lesions. Drugs. 2007;67(15):2187–210.
9. Bernstein DI, Harrison CJ. Effects of the immunomodulating agent R837 on
acute and latent herpes simplex virus type 2 infections. Antimicrob Agents
Chemother. 1989 Sep;33(9):1511–5.
10. Chen M, Griffith BP, Lucia HL, Hsiung GD. Efficacy of S26308 against
guinea pig cytomegalovirus infection. Antimicrob Agents Chemother. 1988
May;32(5):678–83.
11. Sidky YA, Borden EC, Weeks CE, Reiter MJ, Hatcher JF, Bryan GT. Inhibition
of murine tumor growth by an interferon-inducing imidazoquinolinamine.
Cancer Res. 1992 Jul 1;52(13):3528–33.
12. Abbas AK, Lichtman AH. Basic immunology: functions and disorders of
the immune system. 3rd ed. Philadelphia, PA: Saunders/Elsevier; 2009.
13. Reiter MJ, Testerman TL, Miller RL, Weeks CE, Tomai MA. Cytokine
induction in mice by the immunomodulator imiquimod. J Leukoc Biol. 1994
Feb;55(2):234–40.
14. Miller R, Birmachu W, Gerster JF, et al. Imiquimod: cytokine induction and
antiviral activity. International Antiviral News. 1995;3:111–3.
15. Wagner TL, Horton VL, Carlson GL, et al. Induction of cytokines in cynomolgus monkeys by the immune response modifiers, imiquimod, S-27609
and S-28463. Cytokine. 1997 Nov;9(11):837–45.
16. Weeks CE, Gibson SJ. Induction of interferon and other cytokines by
imiquimod and its hydroxylated metabolite R-842 in human blood cells
in vitro. J Interferon Res. 1994 Apr;14(2):81–5.
17. Testerman TL, Gerster JF, Imbertson LM, et al. Cytokine induction by the
immunomodulators imiquimod and S-27609. J Leukoc Biol. 1995 Sep;
58(3):365–72.
18. Megyeri K, Au WC, Rosztoczy I, et al. Stimulation of interferon and
cytokine gene expression by imiquimod and stimulation by Sendai virus
utilize similar signal transduction pathways. Mol Cell Biol. 1995 Apr;
15(4):2207–18.
19. Kono T, Kondo S, Pastore S, et al. Effects of a novel topical
immunomodulator, imiquimod, on keratinocyte cytokine gene expression.
Lymphokine Cytokine Res. 1994 Apr;13(2):71–6.
20. Miller R, Imbertson L, Reiter M, Pecore S, Gerster J. Interferon induction by
antiviral S-26308 in guinea pigs. Paper presented at: Twenty-Sixth Conference
on Antimicrobial Agents and Chemotherapy, 1986; New Orleans, LA.
21. Imbertson LM, Beaurline JM, Couture AM, et al. Cytokine induction
in hairless mouse and rat skin after topical application of the immune
response modifiers imiquimod and S-28463. J Invest Dermatol. 1998
May;110(5):734–9.
22. Tyring SK, Arany II, Stanley MA, et al. Mechanism of action of imiquimod
5% cream in the treatment of anogenital warts. Prim Care Update Ob Gyns.
1998 Jul 1;5(4):151–2.
23. Hashimoto C, Hudson KL, Anderson KV. The Toll gene of Drosophila,
required for dorsal-ventral embryonic polarity, appears to encode a transmembrane protein. Cell. 1988 Jan 29;52(2):269–79.
Clinical Medicine: Therapeutics 2009:1
24. Gay NJ, Keith FJ. Drosophila Toll and IL-1 receptor. Nature. 1991 May 30;
351(6325):355–6.
25. Lemaitre B, Nicolas E, Michaut L, Reichhart JM, Hoffmann JA. The
dorsoventral regulatory gene cassette spatzle/Toll/cactus controls the
potent antifungal response in Drosophila adults. Cell. 1996 Sep 20;86(6):
973–83.
26. Medzhitov R, Preston-Hurlburt P, Janeway CA Jr. A human homologue of
the Drosophila Toll protein signals activation of adaptive immunity. Nature.
1997 Jul 24;388(6640):394–7.
27. Diebold SS, Kaisho T, Hemmi H, Akira S, Reis e Sousa C. Innate antiviral
responses by means of TLR7-mediated recognition of single-stranded RNA.
Science. 2004 Mar 5;303(5663):1529–31.
28. Kaisho T, Akira S. Toll-like receptor function and signaling. J Allergy Clin
Immunol. 2006 May;117(5):979–87; quiz 988.
29. Hemmi H, Kaisho T, Takeuchi O, et al. Small anti-viral compounds
activate immune cells via the TLR7 MyD88-dependent signaling pathway.
Nat Immunol. 2002 Feb;3(2):196–200.
30. Jurk M, Heil F, Vollmer J, et al. Human TLR7 or TLR8 independently confer responsiveness to the antiviral compound R-848. Nat Immunol. 2002
Jun;3(6):499.
31. Bottrel RL, Yang YL, Levy DE, Tomai M, Reis LF. The immune response
modifier imiquimod requires STAT-1 for induction of interferon, interferonstimulated genes, and interleukin-6. Antimicrob Agents Chemother. 1999
Apr;43(4):856–61.
32. Suzuki H, Wang B, Shivji GM, et al. Imiquimod, a topical immune response
modifier, induces migration of Langerhans cells. J Invest Dermatol. 2000
Jan;114(1):135–41.
33. Ahonen CL, Gibson SJ, Smith RM, et al. Dendritic cell maturation and subsequent enhanced T-cell stimulation induced with the novel synthetic immune
response modifier R-848. Cell Immunol. 1999 Oct 10;197(1):62–72.
34. Burns RP Jr, Ferbel B, Tomai M, Miller R, Gaspari AA. The imidazoquinolines, imiquimod and R-848, induce functional, but not phenotypic, maturation of human epidermal Langerhans’ cells. Clin Immunol. 2000 Jan;94(1):
13–23.
35. Tomai MA, Imbertson LM, Stanczak TL, Tygrett LT, Waldschmidt TJ. The
immune response modifiers imiquimod and R-848 are potent activators of
B lymphocytes. Cell Immunol. 2000 Jul 10;203(1):55–65.
36. Bishop GA, Hsing Y, Hostager BS, Jalukar SV, Ramirez LM, Tomai MA.
Molecular mechanisms of B lymphocyte activation by the immune response
modifier R-848. J Immunol. 2000 Nov 15;165(10):5552–7.
37. Bishop GA, Ramirez LM, Baccam M, Busch LK, Pederson LK, Tomai MA.
The immune response modifier resiquimod mimics CD40-induced B cell
activation. Cell Immunol. 2001 Feb 25;208(1):9–17.
38. Berman B, Sullivan T, De Araujo T, Nadji M. Expression of Fas-receptor on
basal cell carcinomas after treatment with imiquimod 5% cream or vehicle.
Br J Dermatol. 2003 Nov;149 Suppl 66:59–61.
39. Vidal D, Matias-Guiu X, Alomar A. Efficacy of imiquimod for the expression of Bcl-2, Ki67, p53 and basal cell carcinoma apoptosis. Br J Dermatol.
2004 Sep;151(3):656–62.
40. Schon MP, Wienrich BG, Drewniok C, et al. Death receptor-independent
apoptosis in malignant melanoma induced by the small-molecule immune
response modifier imiquimod. J Invest Dermatol. 2004 May;122(5):
1266–76.
41. Harrison LI, Skinner SL, Marbury TC, et al. Pharmacokinetics and safety of
imiquimod 5% cream in the treatment of actinic keratoses of the face, scalp,
or hands and arms. Arch Dermatol Res. 2004 Jun;296(1):6–11.
42. Myhre PE, Levy ML, Eichenfield LF, Kolb VB, Fielder SL, Meng TC.
Pharmacokinetics and safety of imiquimod 5% cream in the treatment of
molluscum contagiosum in children. Pediatr Dermatol. 2008 Jan–Feb;
25(1):88–95.
43. Beutner KR, Spruance SL, Hougham AJ, Fox TL, Owens ML,
Douglas JM Jr. Treatment of genital warts with an immune-response
modifier (imiquimod). J Am Acad Dermatol. 1998a Feb;38(2 Pt 1):
230–9.
44. Beutner KR, Tyring SK, Trofatter KF Jr, et al. Imiquimod, a patientapplied immune-response modifier for treatment of external genital warts.
Antimicrob Agents Chemother. 1998b Apr;42(4):789–94.
1573
Ryu and Yang
45. Arican O, Guneri F, Bilgic K, Karaoglu A. Topical imiquimod 5% cream in
external anogenital warts: a randomized, double-blind, placebo-controlled
study. J Dermatol. 2004 Aug;31(8):627–31.
46. Edwards L, Ferenczy A, Eron L, et al. Self-administered topical 5% imiquimod cream for external anogenital warts. HPV Study Group. Human PapillomaVirus. Arch Dermatol. 1998 Jan;134(1):25–30.
47. Romero-Sanchez A, Castro-Castaneda B, Abad-Gastelum M. Comparative
study using 5% imiquimod cream vs. 1% 5-fluorouracil cream for the treatment of genital warts in male patients. Paper presented at: 41st Interscience
Conference on Antimicrobial Agents and Chemotherapy, 2001; Chicago, IL.
48. Schofer H, Van Ophoven A, Henke U, Lenz T, Eul A. Randomized,
comparative trial on the sustained efficacy of topical imiquimod 5% cream
versus conventional ablative methods in external anogenital warts. Eur J
Dermatol. 2006 Nov–Dec;16(6):642–8.
49. Alomar A, Bichel J, McRae S. Vehicle-controlled, randomized, double-blind
study to assess safety and efficacy of imiquimod 5% cream applied once
daily 3 days per week in one or two courses of treatment of actinic keratoses
on the head. Br J Dermatol. 2007 Jul;157(1):133–41.
50. Jorizzo J, Dinehart S, Matheson R, et al. Vehicle-controlled, double-blind,
randomized study of imiquimod 5% cream applied 3 days per week in one
or two courses of treatment for actinic keratoses on the head. J Am Acad
Dermatol. 2007 Aug;57(2):265–8.
51. Korman N, Moy R, Ling M, et al. Dosing with 5% imiquimod cream
3 times per week for the treatment of actinic keratosis: results of two
phase 3, randomized, double-blind, parallel-group, vehicle-controlled trials.
Arch Dermatol. 2005 Apr;141(4):467–73.
52. Lebwohl M, Dinehart S, Whiting D, et al. Imiquimod 5% cream for the
treatment of actinic keratosis: results from two phase III, randomized,
double-blind, parallel group, vehicle-controlled trials. J Am Acad Dermatol.
2004 May;50(5):714–21.
53. Tanghetti E, Werschler P. Comparison of 5% 5-fluorouracil cream and 5%
imiquimod cream in the management of actinic keratoses on the face and
scalp. J Drugs Dermatol. 2007 Feb;6(2):144–7.
54. Krawtchenko N, Roewert-Huber J, Ulrich M, Mann I, Sterry W, Stockfleth E.
A randomised study of topical 5% imiquimod vs. topical 5-fluorouracil vs.
cryosurgery in immunocompetent patients with actinic keratoses: a comparison of clinical and histological outcomes including 1-year follow-up.
Br J Dermatol. Dec 2007;157 Suppl 2:34–40.
55. Geisse J, Caro I, Lindholm J, Golitz L, Stampone P, Owens M. Imiquimod
5% cream for the treatment of superficial basal cell carcinoma: results from
two phase III, randomized, vehicle-controlled studies. J Am Acad Dermatol.
2004 May;50(5):722–33.
56. Geisse JK, Rich P, Pandya A, et al. Imiquimod 5% cream for the treatment
of superficial basal cell carcinoma: a double-blind, randomized, vehiclecontrolled study. J Am Acad Dermatol. 2002 Sep;47(3):390–8.
57. Gollnick H, Barona CG, Frank RG, et al. Recurrence rate of superficial
basal cell carcinoma following treatment with imiquimod 5% cream: conclusion of a 5-year long-term follow-up study in Europe. Eur J Dermatol.
2008 Nov–Dec;18(6):677–82.
58. Schulze HJ, Cribier B, Requena L, et al. Imiquimod 5% cream for the treatment
of superficial basal cell carcinoma: results from a randomized vehicle-controlled
phase III study in Europe. Br J Dermatol. 2005 May;152(5):939–47.
59. Shumack S, Robinson J, Kossard S, et al. Efficacy of topical 5% imiquimod
cream for the treatment of nodular basal cell carcinoma: comparison of
dosing regimens. Arch Dermatol. 2002 Sep;138(9):1165–71.
60. Spencer JM. Pilot study of imiquimod 5% cream as adjunctive therapy to
curettage and electrodesiccation for nodular basal cell carcinoma. Dermatol
Surg. 2006 Jan;32(1):63–9.
61. Rigel DS, Torres AM, Ely H. Imiquimod 5% cream following curettage
without electrodesiccation for basal cell carcinoma: preliminary report.
J Drugs Dermatol. 2008 Jan;7(1 Suppl 1):s15–6.
62. Hengge UR, Esser S, Schultewolter T, et al. Self-administered topical 5%
imiquimod for the treatment of common warts and molluscum contagiosum. Br J Dermatol. 2000 Nov;143(5):1026–31.
63. Grussendorf-Conen EI, Jacobs S, Rubben A, Dethlefsen U. Topical 5%
imiquimod long-term treatment of cutaneous warts resistant to standard
therapy modalities. Dermatology. 2002;205(2):139–45.
1574
64. Schacker TW, Conant M, Thoming C, Stanczak T, Wang Z, Smith M.
Imiquimod 5-percent cream does not alter the natural history of recurrent
herpes genitalis: a phase II, randomized, double-blind, placebo-controlled
study. Antimicrob Agents Chemother. 2002 Oct;46(10):3243–8.
65. Theos AU, Cummins R, Silverberg NB, Paller AS. Effectiveness of
imiquimod cream 5% for treating childhood molluscum contagiosum
in a double-blind, randomized pilot trial. Cutis. 2004 Aug;74(2):134–8,
141–32.
66. 3M.
Aldara
Prescribing
Information.
http://www.accessdata.fda.
gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.Label_
ApprovalHistory#apphist; 2007.
67. Patel GK, Goodwin R, Chawla M, et al. Imiquimod 5% cream monotherapy
for cutaneous squamous cell carcinoma in situ (Bowen’s disease): a randomized, double-blind, placebo-controlled trial. J Am Acad Dermatol. 2006
Jun;54(6):1025–32.
68. Li VW, Ball RA, Vasan N. Antiangiogenic therapy for squamous cell
carcinoma using combinatorial agents. J Clin Oncol. 2005;23(16):199.
69. Naylor MF, Crowson N, Kuwahara R, et al. Treatment of lentigo maligna
with topical imiquimod. Br J Dermatol. 2003 Nov;149 Suppl 66:66–70.
70. Fleming CJ, Bryden AM, Evans A, Dawe RS, Ibbotson SH. A pilot study
of treatment of lentigo maligna with 5% imiquimod cream. Br J Dermatol.
2004 Aug;151(2):485–8.
71. Powell AM, Russell-Jones R, Barlow RJ. Topical imiquimod immunotherapy in the management of lentigo maligna. Clin Exp Dermatol. 2004
Jan;29(1):15–21.
72. Wolf IH, Cerroni L, Kodama K, Kerl H. Treatment of lentigo maligna
(melanoma in situ) with the immune response modifier imiquimod. Arch
Dermatol. 2005 Apr;141(4):510–4.
73. Green DS, Bodman-Smith MD, Dalgleish AG, Fischer MD. Phase I/II
study of topical imiquimod and intralesional interleukin-2 in the treatment
of accessible metastases in malignant melanoma. Br J Dermatol. 2007
Feb;156(2):337–45.
74. Kowalzick L, Eickenscheidt L. Progress of multiple cutaneous and subcutaneous melanoma metastases of the face during imiquimod treatment.
J Dtsch Dermatol Ges. 2009 Jun;7(6):538–40.
75. Marchitelli C, Secco G, Perrotta M, Lugones L, Pesce R, Testa R. Treatment
of bowenoid and basaloid vulvar intraepithelial neoplasia 2/3 with imiquimod 5% cream. J Reprod Med. 2004 Nov;49(11):876–82.
76. Le T, Hicks W, Menard C, Hopkins L, Fung MF. Preliminary results of 5%
imiquimod cream in the primary treatment of vulva intraepithelial neoplasia
grade 2/3. Am J Obstet Gynecol. 2006 Feb;194(2):377–80.
77. Todd RW, Etherington IJ, Luesley DM. The effects of 5% imiquimod
cream on high-grade vulval intraepithelial neoplasia. Gynecol Oncol. 2002
Apr;85(1):67–70.
78. Wendling J, Saiag P, Berville-Levy S, Bourgault-Villada I, Clerici T,
Moyal-Barracco M. Treatment of undifferentiated vulvar intraepithelial
neoplasia with 5% imiquimod cream: a prospective study of 12 cases. Arch
Dermatol. 2004 Oct;140(10):1220–4.
79. Buck HW, Guth KJ. Treatment of vaginal intraepithelial neoplasia
(primarily low grade) with imiquimod 5% cream. J Low Genit Tract Dis.
2003 Oct;7(4):290–3.
80. Chong A, Loo WJ, Banney L, Grant JW, Norris PG. Imiquimod 5% cream
in the treatment of mycosis fungoides—a pilot study. J Dermatolog Treat.
2004 Apr;15(2):118–9.
81. Celestin Schartz NE, Chevret S, Paz C, et al. Imiquimod 5% cream for
treatment of HIV-negative Kaposi’s sarcoma skin lesions: A phase I to II,
open-label trial in 17 patients. J Am Acad Dermatol. 2008 Apr;58(4):585–91.
82. McCuaig CC, Dubois J, Powell J, et al. A phase II, open-label study of the
efficacy and safety of imiquimod in the treatment of superficial and mixed
infantile hemangioma. Pediatr Dermatol. 2009 Mar–Apr;26(2):203–12.
83. Welsh O, Olazaran Z, Gomez M, Salas J, Berman B. Treatment of infantile
hemangiomas with short-term application of imiquimod 5% cream. J Am
Acad Dermatol. 2004 Oct;51(4):639–42.
84. Barry RB, Hughes BR, Cook LJ. Involution of infantile haemangiomas after
imiquimod 5% cream. Clin Exp Dermatol. 2008 Jul;33(4):446–9.
85. Fallah H, Fischer G, Zagarella S. Pyogenic granuloma in children: treatment
with topical imiquimod. Australas J Dermatol. 2007 Nov;48(4):217–20.
Clinical Medicine: Therapeutics 2009:1
Topical imiquimod: mechanism of action and clinical uses
86. Georgiou S, Monastirli A, Pasmatzi E, Tsambaos D. Pyogenic granuloma: complete remission under occlusive imiquimod 5% cream. Clin Exp
Dermatol. 2008 Jul;33(4):454–6.
87. Gilson RJ, Shupack JL, Friedman-Kien AE, et al. A randomized, controlled,
safety study using imiquimod for the topical treatment of anogenital warts
in HIV-infected patients. Imiquimod Study Group. Aids. 1999 Dec 3;13(17):
2397–404.
88. Ulrich C, Bichel J, Euvrard S, et al. Topical immunomodulation under
systemic immunosuppression: results of a multicentre, randomized, placebo-controlled safety and efficacy study of imiquimod 5% cream for the
treatment of actinic keratoses in kidney, heart, and liver transplant patients.
Br J Dermatol. 2007 Dec;157 Suppl 2:25–31.
89. Brown VL, Atkins CL, Ghali L, Cerio R, Harwood CA, Proby CM. Safety
and efficacy of 5% imiquimod cream for the treatment of skin dysplasia
in high-risk renal transplant recipients: randomized, double-blind, placebocontrolled trial. Arch Dermatol. 2005 Aug;141(8):985–93.
90. Firooz A, Khamesipour A, Ghoorchi MH, et al. Imiquimod in combination with meglumine antimoniate for cutaneous leishmaniasis: a randomized assessor-blind controlled trial. Arch Dermatol. 2006 Dec;142(12):
1575–9.
91. Miranda-Verastegui C, Llanos-Cuentas A, Arevalo I, Ward BJ,
Matlashewski G. Randomized, double-blind clinical trial of topical
imiquimod 5% with parenteral meglumine antimoniate in the treatment
of cutaneous leishmaniasis in Peru. Clin Infect Dis. 2005 May 15;40(10):
1395–403.
92. Berman B, Kaufman J. Pilot study of the effect of postoperative imiquimod
5% cream on the recurrence rate of excised keloids. J Am Acad Dermatol.
2002 Oct;47(4 Suppl):S209–11.
93. Cacao FM, Tanaka V, Messina MC. Failure of imiquimod 5% cream to
prevent recurrence of surgically excised trunk keloids. Dermatol Surg. 2009
Apr;35(4):629–33.
94. Berman B, Frankel S, Villa AM, Ramirez CC, Poochareon V,
Nouri K. Double-blind, randomized, placebo-controlled, prospective study
evaluating the tolerability and effectiveness of imiquimod applied to postsurgical excisions on scar cosmesis. Dermatol Surg. 2005 Nov;31(11 Pt 1):
1399–403.
95. Ben M’barek L, Mebazaa A, Euvrard S, et al. 5% topical imiquimod
tolerance in transplant recipients. Dermatology. 2007;215(2):130–3.
96. Yang FC, Jessup C, Dahiya M, Reynolds R. Pityriasis rubra pilaris exacerbation with topical use of imiquimod. Int J Dermatol. 2008 Oct;47(10):
1076–8.
97. Gilliet M, Conrad C, Geiges M, et al. Psoriasis triggered by tolllike receptor 7 agonist imiquimod in the presence of dermal plasmacytoid
dendritic cell precursors. Arch Dermatol. 2004 Dec;140(12):1490–5.
98. Rajan N, Langtry JA. Generalized exacerbation of psoriasis associated
with imiquimod cream treatment of superficial basal cell carcinomas.
Clin Exp Dermatol. 2006 Jan;31(1):140–1.
99. Bauza A, Del Pozo LJ, Saus C, Martin A. Pemphigus-like lesions induced
by imiquimod. Clin Exp Dermatol. 2009 Jul;34(5):e60–2.
100. Campagne G, Roca M, Martinez A. Successful treatment of a high-grade
intraepithelial neoplasia with imiquimod, with vulvar pemphigus as a
side effect. Eur J Obstet Gynecol Reprod Biol. 2003 Aug 15;109(2):
224–7.
101. Lin R, Ladd DJ Jr, Powell DJ, Way BV. Localized pemphigus foliaceus induced by topical imiquimod treatment. Arch Dermatol. 2004 Jul;
140(7):889–90.
102. Smorlesi A, Papalini F, Orlando F, Donnini A, Re F, Provinciali M.
Imiquimod and S-27609 as adjuvants of DNA vaccination in a transgenic
murine model of HER2/neu-positive mammary carcinoma. Gene Ther.
2005 Sep;12(17):1324–32.
103. Craft N, Bruhn KW, Nguyen BD, et al. The TLR7 agonist imiquimod
enhances the anti-melanoma effects of a recombinant Listeria monocytogenes vaccine. J Immunol. 2005 Aug 1;175(3):1983–90.
Publish with Libertas Academica and
every scientist working in your field can
read your article
“I would like to say that this is the most author-friendly
editing process I have experienced in over 150
publications. Thank you most sincerely.”
“The communication between your staff and me has
been terrific. Whenever progress is made with the
manuscript, I receive notice. Quite honestly, I’ve
never had such complete communication with a
journal.”
“LA is different, and hopefully represents a kind of
scientific publication machinery that removes the
hurdles from free flow of scientific thought.”
Your paper will be:
•
Available to your entire community
free of charge
•
Fairly and quickly peer reviewed
•
Yours! You retain copyright
http://www.la-press.com
Clinical Medicine: Therapeutics 2009:1
1575