Ossification Process and Bone Repair Mechanisms
advertisement

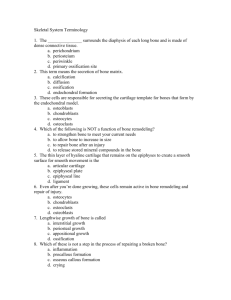
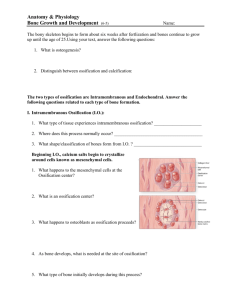
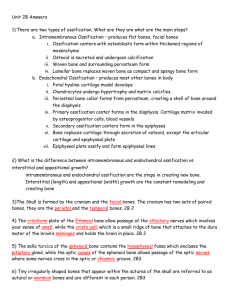
Ossification Process and Bone Repair Mechanisms Bones form in two ways. A process known as intramembranous ossification forms bones that develop from layers of connective tissue. Flat bones such as those found in the skull develop through this process. Endochondral ossification (from the word roots endo-, meaning "within," and chondral, meaning "cartilage") is bone formation from a hyaline cartilage blueprint or template, which determines the future bone shape. Bones of the limbs and extremities develop through endochondral ossification. For example, an infant's arm and leg bones contain only small amounts of actual hard bone material; they are primarily made of cartilage. As the child grows, bone replaces the cartilage. Ossification is the process of forming bone. You learned that there are two types of ossification: • • intramembranous ossification, which is direct synthesis of bone by specialized stem cells (mesenchymal cells) from fibrous connective tissue; and endochondral ossification, which is synthesis of bone from a (hyaline) cartilage template. • Intramembranous Ossification Intramembranous ossification is the process that forms and repairs the flat bones of the skull, clavicles and other irregularly shaped bones. In some situations of bone repair and adaptation to excessive force, intramembranous ossification generates new bone. The process of intramembranous ossification involves multiple steps: 1. 2. 3. 4. Increased vascularization. Recruitment of mesenchymal stem cells Differentiation Secretion of osteoid 5. Mineralization 6. Formation of trabeculae 7. Formation of outer compact bone First, the site for future bone formation increases in vascularization— new blood vessels form near the site where the bones will grow. Mesenchymal stem cells, which originate in the embryonic mesoderm, become active and travel through the blood vessels to the future site of bone formation. Chemical messages then cause the mesenchymal stem cells to differentiate: they change into osteoprogenitor cells, which may divide and differentiate into osteoblasts. The osteoblasts deposit osteoid (the unmineralized bone extracellular matrix) and are then trapped in the matrix, where they differentiate into osteocytes. Inorganic salts in the blood travel through the blood vessels to mineralize the bone matrix. As a result, hydroxyapatite crystals form within the osteoid. On the interior of the tissue, small clusters of bone begin to connect with other clusters to form trabeculae. Osteoblasts near the surface of the bone deposit matrix in organized lamellae and form a thin outer layer of compact bone. The periosteum ("peri-" means "surrounding" and "osteum" means "bone") is living membrane composed of fibrous connective tissue that forms on the outside of the compact bone. Its inside layer has osteoblasts for bone growth and repair. Endochondral Ossification Most bones of the skeleton below the skull develop through endochondral ossification. This process involves the following steps: 1. 2. 3. 4. 5. 6. Formation of a cartilage template Growth of the template Differentiation Vascularization Calcification Bone formation The first step is formation of a hyaline cartilage template, which is the shape of the desired new bone. The cartilage template grows in size and thickens through the production of new chondroblasts at the perichondrium. The perichondrium is the cartilage equivalent of the periosteum. Chondroblasts differentiate into chondrocytes, which produce chemical messages that stimulate the increase of vascular supply at the perichondrium. This increase in vascular supply brings in inorganic salts, which mineralize the central cartilage matrix. Cartilage is laid down as a template that provides some mechanical stability. This is like when designers and architects build a template out of balsa wood, clay or foam because it is easy to quickly remodel and manipulate those substances. Then, once the template is worked out, they will remodel it using a stronger material. In bone, the 'model' cartilage is remodeled over time and osteoblasts produce a full bone matrix with new collagen and hydroxyapatite. In this way, biology works more efficiently than any engineered tissue graft.