Integumentary
advertisement

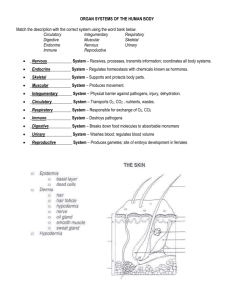
ANAT D502 – Basic Histology revised 11.17.15 Integumentary System Reading Assignment: Outline: I. II. III. IV. I. Chapter 15 – Integumentary System; pay special attention to Clinical Correlations (Boxes 15.1, 15.5 and 15.6) Introduction Layers of the skin A. Epidermis B. Dermis C. Hypodermis Epidermal cells Skin structures A. Nerve supply B. Hair C. Nails D. Glands Introduction The integumentary system consists of the integument (skin; L, covering) and its derivatives. The system is an important boundary layer that separates the organism from the outside world. It is the largest organ of the human body. As such, it has multiple functions that include: 1. Protective – the skin is a water-resistant barrier that protects against dehydration, abrasions, UV light and toxins. 2. Immunological – the skin serves as a passive barrier to pathogens but also contains antigenpresenting cells. 3. Sensory – nerve receptors within the skin relay information about the environment. 4. Exocrine – exocrine glands include eccrine sweat glands (excretory and cooling), apocrine sweat glands (signaling), sebaceous glands (lubrication) and mammary glands (nutritive). 5. Endocrine – the photolytic phases of the vitamin D synthetic pathway occur in the epidermis of the skin. 6. Homeostasis – elements of homeostasis involving the skin include thermoregulation, water conservation, gas exchange, and excretion. 7. Communication – these include non-verbal changes in coloration, expression, as well as “goosebumps.” II. Layers of skin The skin consists of two main layers, the epidermis and dermis. The epidermis is the outer avascular epithelial layer. It consists of a keratinized stratified squamous epithelium that provides the skin’s barrier functions. This layer is constantly being replaced by a system of proliferation and desquamation. The dermis is the inner layer and consists of a dense irregular connective tissue. It provides the skin’s mechanical support and strength. The glands and hair follicles mostly reside here. The hypodermis is a transitional layer of loose connective and adipose tissue between the dermis and underlying structures, permitting movement between the two. The hypodermis is not considered to be part of the skin proper; in gross anatomy it is referred to as the superficial fascia. 1 Skin is classified as thick or thin depending upon the thickness of the epidermis. Thick skin covers the palms (vola) and soles (planta), areas subject to abrasion. It is typically glabrous (hairless). Thin skin covers basically everywhere else and is typically pileous (haired). A. Epidermis The epidermis is composed of a keratinized stratified squamous epithelium. Its cells, keratinocytes, are arranged into 4 (thin skin) or 5 (thick skin) layers. The outermost layer is always composed of non-living, highly keratinized (cornified) cells that function to reduce water loss. After keratinocytes leave the germinal layer, they undergo a specialized form of cell death known as anoikis. Anoikis is initiated when cells detach from their surrounding environment and loose communication with it. In keratinocytes, this programmed cell death is accompanied by the accumulation of keratin to the exclusion of all other products and organelles. From basal to apical, the layers or strata of the epidermis are as follows: i. stratum basale (or stratum germinativum). This is the proliferative layer resting on the basement membrane. It consists of a single layer of cuboidal cells with sparse, basophilic cytoplasm and variable amounts of the pigment melanin. These cells are connected to one another by desmosomes and to the basal lamina by hemidesmosomes. ii. stratum spinosum. This stratum is typically several cells thick but does vary with location. Its polygonal cells have a central nucleus and exhibit numerous cytoplastmic processes (spines) which attach to reciprocating processes of adjacent cells by desmosomes. iii. stratum granulosum. Usually 1-3 cell layers thick, the keratinocytes in this layer are flattened, nucleated cells containing basophilic keratohyalin granules. iv. stratum lucidum. Characteristic of only thick skin, this thin layer of consists of flat, eosinophilic, enucleated cells. v. stratum corneum. The cells of this layer are filled with keratin and devoid of all organelles. Their plasma membranes are coated with an extra-cellular lipid layer (see below). The thickness of this stratum is variable, being thin in thin skin, thicker in thick skin and hypertrophied in calluses. B. Dermis The dermal-epidermal interface is not planar but marked by elaborate interdigitations between the two layers that strengthen their connection. The projections of the dermis into the epidermis are called dermal papillae and the complementary projections of the epithelium are the rete ridges. On the volar (palmar) and plantar surfaces these interdigitations are elaborated and organized to produce the external epidermal ridges (cristae cutis) that provide increased traction (and forensic identification). The dermis is comprised of two layers: (1) papillary and (2) reticular. The superficial papillary layer is thinner, more cellular, and contains small diameter reticular and type I collagen fibers. It is richly vascularized (for thermoregulation) and innervated (sensory and autonomic). The reticular layer lies deep to the papillary layer and is typically thicker and less cellular. It has larger diameter type I collagen and elastic fibers. In the areolae and perineum, this layer contains smooth muscle. Cells of the dermis are typical of collagenous connective tissues: fibroblasts, lymphocytes, macrophages and mast cells. C. Hypodermis The hypodermis is comprised of adipose and loose connective tissues. Its thickness varies with location on the body, sex and nutritional status. It is the principal area of fat storage, providing both 2 energy reserves and insulation. Its cells include adipocytes, fibroblasts, lymphocytes, macrophages, and mast cells. In humans a thin layer of skeletal muscle is present in the hypodermis of the face and neck and this layer forms the muscles of facial expression (e.g., orbicularis oris of the lips, orbicularis orbis of the eyelids). III. Epidermal cells Four types of cells are found within the epidermis: keratinocytes, dendritic (Langerhans’) cells, melanocytes and tactile epithelial (Merkel) cells. Keratinocytes are the most abundant cells of the epidermis. They are attached to one another by desmosomes and to the basal lamina by hemidesmosomes. Their shape transforms from cuboidal to polygonal to squamous during their apical migration and differentiation. They serve two major functions, both related to water conservation: (1) keratin production and (2) formation of the epidermal water barrier. Keratin is a protein family of some 11+ members. Keratin filaments (a type of intermediate filament) are first synthesized in the stratum basale where they form tonofilaments. As the keratinocytes migrate apically, keratin filaments in the cell continue to accumulate. In the strata spinosum and granulosum keratohyalin granules are synthesized. These granules are rich in filaggrin and trichohyalin which when released to the cytoplasm cause the tonofilaments to aggregate into tonofibrils (= keratin fibrils). In the stratum corneum the keratin fibrils (tonofibrils) completely replace the cytoplasmic contents of the cell. The epidermal water barrier of the epidermis is formed by two components found in the differentiating keratinocytes: (1) the cell envelope and (2) the lipid envelope. The cell envelope consists of a 15nm thick layer of insoluble protein attached to the inner surface of the plasma membrane; its major protein is loricrin. The lipid envelope is a 5 nm thick layer of lipids attached to the outer surface of the plasma membrane. This lipid layer is produced by exocytosis of lamellar bodies in the keratinocytes in the strata spinosum and granulosum. These lamellar bodies contain glycosphingolipds, phospholipids and ceramides. The life cycle of a keratinocyte begins by mitosis in the stratum basale. Once contact with the basal lamina is severed the cells are post-mitotic and differentiation begins. As differentiation progresses, cells are pushed towards the surface by basal cell division and growth. Differentiation includes the accumulation of keratin filaments (tonofilaments) and their aggregation into tonofibrils, and the synthesis of lamellar bodies. In the outer layer of the stratum granulosum anoikis begins as nuclei begin to degenerate and organelles are degraded by lysosomal enzymes. The process is complete in the stratum corneum which consists of completely keratinized “cells” that are continuously desquamated. Melanocytes are derived from neural crest cells and account for about 5% of the living cells in the epidermis. Found near the base of the epidermis [and in the hair bulb (see below)], they are attached to the basal lamina by hemidesmosomes but do not attach to neighboring keratinocytes. Their dendritic processes extend into the stratum spinosum. Melanocytes synthesize melanin and distribute it to the keratinocytes to protect them from the mutagenic effect of ultraviolet (UV) radiation. Melanin comes in two different forms, (1) eumalenin (brown pigment) and pheomelanin (red pigment) and is produced in membrane-bound vesicles called melanosomes by a series of enzymatic reactions. This enzymatic process occurs while the melanosomes move apically thought the dendrites. The melanosomes and their contents (pigment granules) are transferred (“pigment donation”) by phagocytosis of the tips of the melanocytes by the keratinocytes. Dendritic cells (or Langerhans’ cells) account for 2-3 % of the living epidermal cells. Unlike melanocytes, these immune system cells can be found through out the epidermis. These are antigenpresenting cells, part of the mononuclear phagocytotic system (MPS). Derived from stem cells in the bone marrow, they migrate into the epithelium. Antigens entering through the skin are taken-up and 3 transported via lymph channels to local lymph nodes for presentation to T-cells. These cells are important in contact (allergic) dermatitis and other cell-mediated immune responses in the skin. Tactile epithelial cells (Merkel cells) are relatively rare (<1% of the living epidermal cells) and are most abundant in areas with acute sensory perception (e.g., finger tips, lips). They are a modified keratinocyte found in the stratum basale. While containing tonofilaments and desmosomes, these cells also contain small dense granules characteristic of neuroendocrine cells. In combination with lensshaped sensory neuron endings in the basal lamina, sensory epithelial cells form a mechanoreceptor called a tactile meniscus (Merkel’s corpuscle). IV. Skin structures A. Nerve supply The integument is richly innervated with both motor and sensory modalities. Autonomic motor nerve endings provide innervation to the numerous 1) glands and 2) smooth muscle of the blood vessels and arrector pili (see below). Peripheral terminals of sensory nerves provide information about the environment to the organisms. The sensory nerve terminals are classified as either encapsulated (invested by CT and/or Schwann cells) or free. However, in both types of terminals the nerve endings loose their myelin sheath. Encapsulated terminals include tactile (Meissner’s) corpuscles, bulboid corpuscles (Krause’s end bulb), lamellar (Pacinian) corpuscles, and Ruffini’s corpuscles. Free terminals include free endings, tactile menisci (Merkel’s corpuscles) and hair follicle receptors. In free endings nerve terminals loose their myelin sheath at the epidermal / dermal junction and pass into the epidermis, ending in the stratum granulosum. These receptors sense pain and temperature. Hair follicle receptors also loose their myelin sheath and coil their bare axons around the hair shaft within the external root sheath (see below). These mechanoreceptors sense the presence and direction of hair displacement. Axons projecting to tactile epithelial cells (Merkel’s cells) loose their myelin sheath and form a disc-like structure within the basal lamina of the epidermal cell. Together they form the mechanoreceptor known as the tactile meniscus (Merkel’s corpuscle). Tactile corpuscles (Meissner’s corpuscles) are Schwann cell-encapsulated nerve endings in the dermal papilla. These touch receptors are most sensitive to low frequency stimuli. Bulboid corpuscles (Krause’s end bulbs) contain multiple bare branches from a single axon enclosed within a CT capsule. These mechanoreceptors are found in the papillary layer of the dermis and in the epithelium of the oral mucosa of the oral cavity and tongue. Lamellar corpuscles (Pacinian corpuscles) contain a single unbranched nerve terminal invested in a concentrically layered capsule formed by CT and Schwann cells. Found deep in the dermis or hypodermis, these receptors sense vibration and pressure. Ruffini’s corpuscles contain multiple bare branches from a single axon within an oblong, fluidfilled CT sac. Found deep in the dermis and hypodermis of the planta (sole), these mechanoreceptors are sensitive to sustained or continuous stress. B. Hair Structure Hairs are slender, keratinous filaments projecting above the surface of the skin. Each hair is produced by a hair follicle found within the dermis. The keratin of hair (and nails) is hard keratin that 4 differs from the soft keratin of the epidermis in that it develops without keratohyalin granules. The resulting hard keratin consists of densely packed keratin filaments in a matrix of amorphous keratin with high sulfur content. Each hair is divisible into a (1) root and (2) shaft. The root is the developing portion of the hair found in the lower follicle. The shaft is the free portion of the hair that extends through the upper follicle and onto the free surface. In cross-section, each hair is divisible into 3 concentric layers, which from internal to external are the (1) medulla, (2) cortex and (3) cuticle. The medulla consists of a core of large, vacuolated cells. It is present, however, only in the thickest hairs. The cortex surrounds the medulla and contains pigmented, keratin-filled cells. The cuticle forms the outer-most layer and consists of scale-like, heavily keratinized cells whose free edges face the direction of hair growth. Distribution and types Hairs are present over almost the entire surface of humans except on the vola, planta, lips and urogenital orifices. However, their density is variable between regions. Four types of hair can be defined in man: i. Lanugo are fine, fetal hairs formed and shed (usually) in utero. They lack a medulla. ii. Vellus are the short, fine (small diameter without medulla), non-pigmented hairs that cover most of the body. These are visible only upon close examination. iii. Terminal are the long, coarse (large diameter with medulla), pigmented hairs that are easily observed. iv. Intermediate hairs are intermediate in morphology between vellus and terminal forms. Hair follicle The hair follicle is the epithelial organ responsible for production and growth of hair. It is divisible into three longitudinal segments: infundibulum, isthmus and inferior segment. The infundibulum extends from the surface of the epidermis to the opening of the sebaceous gland. The lumen of the infundibulum (occupied by the hair shaft) is lined by the external root sheath and it is in this region the hair is coated with sebum (see below). In the isthmus and the inferior segment, the internal root sheath becomes interposed between the hair root and the external root sheath. The isthmus extends from the base of the infundibulum to the insertion of the arrector pili muscle. The inferior segment continues internally and at the base of the follicle expands to form the bulb that surrounds a dermal papilla. External to the external root sheath of the follicle, is a connective tissue cover called the dermal sheath. A bundle of smooth muscle fibers, the arrector pili muscle, attaches to the dermal sheath of the follicle just below the sebaceous gland. Contraction of this muscle produces “goose bumps.” The sebaceous gland develops as a side branch (diverticulum) of the external root sheath. The follicle develops by an in-growth of epithelial ectodermal cells into the underlying mesenchyme during fetal development. The ectoderm will form the epithelial structures (the external root sheath (and sebaceous gland), bulb, internal root sheath and the hair proper). The mesenchyme will give rise to the dermal papilla. Thus, hairs are a classic example of structures that arise through a process called epithelial – mesenchymal interaction. In such an interaction, an epithelium from a lining surface invaginates into the underlying undifferentiated mesoderm (mesenchyme) inducing formation of the structure. In addition to hair, other examples of structures resulting from epithelial – mesenchymal interactions include glands, teeth, scales, feathers, eyes, etc. Growth of the hair occurs at the hair bulb (base of the inferior segment) which surrounds the dermal papilla. The dermal papilla is rich in capillaries which provide the nutrients for growth of the hair and follicle. Contained within the bulb are the proliferative matrix cells (basically dividing keratinocytes) which give rise to both the hair and inner root sheath: The matrix cells adjacent to the tip of the papilla give rise to the cells of the medulla; the adjoining matrix cells gives rise to the cells of the cortex and the matrix cells furthest from the tip give rise to the cells of the cuticle. The matrix cells at the base of the 5 papilla give rise to the internal root sheath. The bulb also contains dendritic cells and melanocytes (what is their origin?), the latter providing melanosomes for hair coloration to the cortical hair cells. The functionally enigmatic internal root sheath contains three layers that surround and grow with the hair root; from internal to external these layers are the cuticle, inner (Huxley’s) layer and outer (Henle’s) layer. The cuticle is a single layer of squamous cells that are linked to the cuticle of the hair root. The inner layer is the middle, more prominent layer of 2-3 cells thickness. The outer layer consists of a single thickness of cuboidal cells that interface with the external root sheath. In contrast to the hair, the keratin of the internal root sheath is soft keratin and the sheath is broken down at the level of the isthmus, i.e., only the hard keratin hair of the bulb emerges through the skin. Hair life cycle Individual hair follicles persist throughout the life of the organism during which time they produce multiple hairs. Thus, the life cycle of a hair can be divided into 4 stages: Anagen, catagen, telogen and exogen. Anagen is the period of hair growth, its duration determines the ultimate length of the hair. Catagen marks the cessation of hair growth; in this stage cell division ceases and the bulb regresses to a small strand of external root sheath. The dermal papilla similarly diminishes and the internal root sheath is lost by apoptosis. Telogen is the rest phase; the proximal end of the hair shaft migrates to the isthmus and has undergoes a change in morphology from bulb- to club-shaped (club hair). During exogen the hair exits the follicle and is shed. For those fortunate to be blessed with persistent, luxurious locks, exogen is usually simultaneous with anagensis of a new hair. C. Nails Nails and their relatives (claws and hooves) are basically localized growths of hard keratin in the epidermis. The nail plate consists of hard keratin and corresponds to the stratum corneum of the epidermis. Beneath the exposed nail plate is the non-proliferative nail bed over which the newly formed nail moves distally. The nail root is the unexposed, proximal end of the nail plate that is surrounded by nail matrix. Within the matrix keratinocytes proliferate, grow, synthesize hard keratin and die to form the nail plate. Note that the growth of nail is perpendicular to the growth of the adjacent epidermis. The root of the nail is overlain by a fold of skin called the eponychium; distally the hyponychium marks the junction of the skin and the free edge of the nail plate. The moon-shaped light region found at the base of the nail plates (produced by the newly formed immature hard keratin) is called the lunula. D. Glands of skin The integumentary glands are all multi-cellular and are embedded within the dermis. They include the sebaceous, sweat (eccrine and apocrine), ceruminous and mammary glands. Sebaceous glands are essentially part of the hair follicle; they develop as an outgrowth of the external root sheath and each follicle has one or more sebaceous glands. In some regions of the body sebaceous glands secrete directly onto the skin surface, for example, the tarsal glands of the palpebrae (eyelids) which secrete to the internal aspect of the eyelid are sebaceous glands. Sebaceous glands, logically enough, release sebum, an oily, waxy secretion that coats the hair and skin. Sebum is a complex mixture of lipids, triglycerides, waxes, squalene, cholesterol and cell remnants. A natural lubricant, sebum acts to protect skin and hair from moisture and desiccation and as a hair emollient; it is also a bacteriostat. Sebum is released by holocrine secretion and is another example of anoikis. Cell proliferation occurs at the base of the gland. As the cells detach and move toward the pilosebaceous canal, their normal cell contents are replaced by an accumulation of secretion products. Secretion and proliferation is under hormonal control. Inflammation of the gland results in acne. 6 Sweat glands are simple, coiled tubular glands. There are two types of sweat glands, eccrine and apocrine, which differ in (1) the nature of their secretion, (2) their association with or without hair and (3) age of functional onset. In humans eccrine sweat glands are distributed over the entire body except for the vermillion of the lips. They are unassociated with hairs and are functional at birth. Each gland consists of two segments, secretory and duct. The secretory segment is located in the deep dermis and contains 3 cell types arranged in a pseudostratified fashion: (1) Dark cells which secrete glycoprotein; (2) clears cells which secrete salts and the watery component of sweat; and (3) myoepithelial cells found along the perimeter of the basement membrane. As in the salivary glands, the contraction of the myoepithelial cells move the merocrine secretion of the glands through the duct segment. The duct segment is a stratified cuboidal epithelium that leads to the skin surface. The cells of the duct modify the secretion by resorbing some salt and water. Sweat is composed of water, salt, urea, ammonia and uric acid. Its minor function is the excretion of nitrogenous waste. Its major function (thermoregulatory sweating) is thermoregulation by means evaporative cooling. While these glands are under control of the sympathetic nervous system they are stimulated by cholinergic neurotransmitters. In stressful situations, eccrine sweat glands will also secrete in response to epinephrine (emotional sweating). Apocrine sweat glands empty their contents into hair follicles in the axillary, areolar and anal regions of the body. Like sebaceous glands, they are derived from an outgrowth of the external root sheath. They have secretory and ductal components. The secretory component consists of a simple epithelium surrounding a large lumen which stores the secretion. Myoepithelial cells found along the basement membrane move the secretion through the lumen. The duct component is a stratified cuboidal epithelium that runs straight to the infundibulum of the hair follicle; the duct does not modify the secretion. Apocrine sweat glands secrete a viscous product of complex composition that probably serves(d) behavioral functions. Unlike eccrine sweat glands, apocrine sweat glands are not functional at birth but become active at puberty. Like eccrine sweat glands, they are under control of the sympathetic nervous system but are stimulated by adrenergic neurotransmitters. The ceruminous glands will be examined with the ear and the nutritive mammary glands will be studied in the section on female reproduction. 7