Nursing Care of The New Born Infant
advertisement

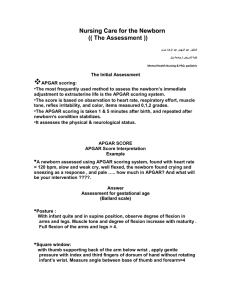
Nursing Care of The New Born Infant Retnayu Pradanie 01/04/09 Introduction The neonatal periode is the time from birth through the twenty day of life. During this time the newborn must accomplish a number of physiologic and behavioral adjusments in order to establish and maintain an extrauterine life Transition Period: Phases of instability during the first 6-8 hours after birth Nurses play a vital role during the transition periode Help the newborn infant make a safe transition to extrauterine life Perform the initial assessment of the newborn infant Provide a physical environment conducive to adaptation Monitor the newborn infant’s condition during the early adaptation phases Immediate Care of the Newborn Start by congratulating the mother on the arrival of her new baby and ask if she has any concerns. The mother is usually the first person to notice any problems. Doing initial newborn assessment Initial Newborn assessment Stimulate and dry infant Asses ABCs Encourage skin-to-skin contact Assign APGAR score Give eye prophylaxis & vit K • sterile ophthalmic ointment containing 1% tetracycline or 0.5% erythromycin • 1 mg of Vit K IM to prevent hemorhagic Initial assessment: Apgar Scoring The most frequently used method to assess the newborn's immediate adjustment to extrauterine life. The score is based on observation of : Heart rate. Respiratory effort. Muscle tone. Reflex irritability. Color. ● Each item is given a score of 0, 1,or 2. Apgar Scoring SIGN SCORE 0 1 2 Heart Rate Absent Slow (<100) Over 100 Raespiratory Rate Absent Slow, weak cry Good cry Muscle Tone Flaccide Some flexion of extremities Well flexed No response Grimace Cry Blue, pale Body pink, extremities blue Completely pink Reflex irritability Color Initial assessment: Apgar Scoring Evaluation of all five categories are made at 1 and 5 minutes after birth and repeated until the infant's condition stabilized. Total scores of 0-3 represent severe distress. Scores of 4-6 signify moderate difficulty. Scores of 7-10 indicate absence of difficulty in adjusting to extrauterine life Initial assessment: Apgar Scoring The Apgar score is affected by the degree of : - Physiologic immaturity. - Infection. - Congenital malformations. - Maternal sedation or analgesia. - Neuromuscular disorders. Transitional assessment Periods for reactivity: First period of reactivity: For 6-8 hours after birth. Initial stage of alertness and activity: - During the first 30 minutes. - The infant is very alert, cries vigorously, very interest in the environment. - Neonate's eyes are usually open; - The newborn has a vigorous suck; this is an opportune time to begin breastfeeding Transitional assessment - physiologically, the resp rate is high as 80 breath/min, crackles may be heard, heart rate reach 180 beat/min, bowel sound are active , mucus secretions are increased, and temp may decrease. 2. Second stage: - Lasts to 2-4 hours, - Heart and resp rate decrease, temp continues to fall, mucus production decreases ,and urine or stool is usually not passed. - The infant is in state of sleep and relative calm. - Undressing or bathing is avoided during this time Transitional assessment - The second period of reactivity: begins when the infant awakes from this deep sleep. It lasts about 2-5 hours and The infant is again alert and responsive, Heart and resp rates increase. The gag reflex is active gastric and respiratory secretions are increased, Passage of meconium frequently occurs. This period is usually over when the amount of respiratory mucus has decreased. Clinical assessment of gestational age A frequently used method of determining gestational age is the simplifies Assessment of Gestational Age by Ballard(1979): - It assess six external physical and six neuromuscular signs - Each sign has a number score, and the cumulative score correlate with a maturity rating of from 20 to 44 weeks of gestation. Weight Related to Gestational Age: ● Birth weight alone is a poor indicator of gestational age and fetal maturity . ● Maturity: functional capacity: the degree to which the neonate's organ systems are able to adapt to the requirements of extrauterine life ● Classification of infants at birth by both birthweight and gestational age provides amore satisfactory method for predicting mortality risks and providing guidelines for management of the neonate than estimating gestational age or birth weight alone. Clinical assessment of gestational age ● Appropriate for gestational age (AGA) :the infant whose weight is between 10th and 90th percentiles. Can be presumed to have grown at a normal rate regardless of the time of birth_ preterm, term, or post term. ● Large for gestational age (LGA): above 90th percentile can be presumed to have grown at an accelerated rate during fetal life ● Small-for-gestational-age (SGA) infant below 10th percentile can be assumed to have intrauterine growth retardation or delay. Clinical assessment of the newborn (General Examination) Examine skin for prematurity or dismaturity Thin, transparent skin in preterm infants Wrinkled peeling skin of dysmaturity in an IUGR infant Pale pink skin of a term infant (hair shaved to site IV line) Skin: some common normal findings Vernix caseosa: a cream/white cheesy material on the skin at birth which cleans off easily with oil. Lanugo; fine downy hairs seen on the back and shoulders especially in preterm infants. Milia: pinpoint whitish papules on nose and cheeks due to blocked sebaceous glands. Mongolian blue spots: grey/bluish pigment patches seen in the lumbar area, buttocks and extremities in dark skinned babies.They usually disappear by one year. Skin: some common normal findings Capillary heamangiomas (“stork bite” naevi): red flat patches which blanch with gentle pressure. Commonly occur on upper eyelids, forehead and nape of the neck. Erythema toxicum: small white/yellow papules or pustules on a red base seen on face, trunk and limbs. Develop 1 – 3 days after birth and usually disappear by one week. Colour Note palor or plethora Cyanosis: the baby should be uniformly pink Blueness of the hands and feet (peripheral cyanosis) may be due to cold extremeties. Blueness of the mucous membranes and tongue is central cyanosis and is usually due to lung or heart problems Bruising (ecchymosis) is common after birth trauma. Unlike cyanosis, bruising does not blanch on gentle pressure. Jaundice Jaundice is common in the first week of life and may be missed in dark skinned babies Blanch the tip of the nose or hold baby up and gently tip forward and backward to get the eyes to open. Teach mother to do the same at home in the first week and report to hospital if significant jaundice is observed. After general examination After these general observations, examine the infant starting with the head and moving down the body (Head to toe examination) Count the respiratory rate normal 30 – 40 breaths/min in term infants faster in preterms. > 60 / minute abnormal After general examination… Measure: Weight normal 2.5 – 3.99 kg Length normal 48 – 52 cm Occipitofrontal circumference (OFC) normal 33 – 37 cm Infants at Risk gagging --> turning blue (esp. after feeding) generalized cyanosis weak cry grunting or respiratory distress decreased or absent movements excessive twitching or trembling Nursing Diagnosis: Ineffective Airway Clearance R/T excessive oropharyngeal mucus Ineffective Thermoregulation R/T newborn transition to extrauterine life High Risk for infection R/T maturational factors, immature immune system PC: Hypoxemia PC: Hyperbilirubinemia (W) Beginning Integration of NB into Family Unit Nursing care of the newborn The major elements of routine care: Cord care Thermal control 24 hour rooming in Feeding Immunization Maternal education on hygiene Cord Care The umbilical stump needs particular attention as there are risks of bleeding and infection. Good cord care includes: Cutting cord with sterile equipment or a new razor blade depending on the setting Ligation with a sterile plastic clamp or clean thread Keeping cord stump exposed, clean (with 70% alcohol, 4% chlorhexidine or simple soap and water) and dry Cord Care and Research 1,811 NB’s- 2 groups - one receiving cord care with alcohol and one group not: equal # infections in infants who received and did not receive cord care cord separation ~ alcohol use: 9.8 days and no alcohol use: 8.16 days Thermal Control The causes of heat loss at birth: Evaporation: the lost of heat through moisture (a major cause). Radiation: the lost of heat to cooler solid objects in the environment that are not in direct contact with the infant. Conduction: loss of heat from the body because of direct contact of skin with a cooler solid object Convection is similar to conduction, except that heat loss is aided by surrounding air currents; as direct flow of air from air conditioner vent. Measures to prevent hypothermia include: Delivery in a warm environment Immediate drying of the infant to minimize heat loss by evaporation Bath after temperature is stable Keep out of drafts Skin to skin contact with mother Proper clothing and wrapping up with linen including use of booties and bonnets Regular feeds A well dressed baby Rooming In refers to the practice of nursing babies with their mothers rather than keeping them in a separate nursery Advantages: Promotes bonding Makes exclusive breastfeeding easy Mother is able to keep a close watch on her infant. She should be encouraged to report any concerns that she has to the health care staff. Feeding Breast feeding remains the best method of feeding the newborn and has the following advantages: Breastmilk is nutritionally balanced It reduces the risk of infection especially in unhygienic situations Protects against diarrhoea and other infections in infancy Promotes mother-child bonding It is readily available It helps in child spacing Immunization Example of an immunisation schedule At birth 6 weeks 10 weeks 14 weeks 9 months BCG, Oral polio & HBV1 DPT1, Oral polio & HBV2 DPT2, Oral polio DPT3, Oral polio & HBV3 Measles, yellow fever Hygiene and prevent infection Hand washing. A common practice in many newborn nurseries is the use of cover gowns to prevent infection. Eye care, umbilical care, bathing, care of the circumcision. Vitamin K is administered to protect against hemorrhage. Proper identification. No tub baths until cord off and healed clean around organs of elimination and mouth after soiling to prevent skin break down fold diapers away from umbilicus Questions and Discussions Thank You