Resources for Cultural and Linguistic Services
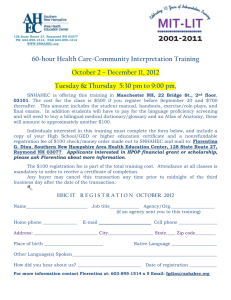
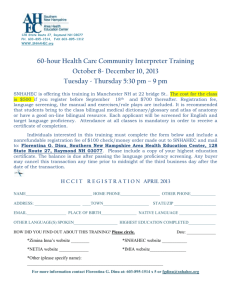
advertisement

Caring for Diverse Populations Better Communication, Better Care: A Toolkit for Physicians and Health Care Professionals Table of Contents Introduction for Healthcare Professionals: Why Was This Toolkit Created? How Can It Help My Practice? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2 Improving Communications with a Diverse Patient Base . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3 Tips for Successful Encounters with Diverse Patients. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4 Tips for Office Staff to Enhance Communication with Diverse Patients . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5 Nonverbal Communication and Patient Care. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6 “D-I-V-E-R-S-E” – A Mnemonic for Patient Encounters . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8 Tips to Identify and Address Health Literacy Issues . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10 Planning Effective Written Patient Communications. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12 Tools and Training for Your Office in Caring for a Diverse Patient Base . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13 Interview Guide for Hiring Office/Clinic Staff with Diversity Awareness. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14 Online Medical Consumer Training Resources for Health Educators to Share with Patients. . . . . . . . . . . . . . . . . . . . . . . . . . . . 15 Resources to Communicate Across Language Barriers. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17 Tips for Communicating Across Language Barriers. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18 10 Tips for Working with Interpreters. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 19 Tips for Locating Interpreter Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20 U.S. Census Language Identification Flashcards . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 21 Common Signs in Multiple Languages. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25 Common Sentences in Multiple Languages . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26 Employee Language Skills Self-Assessment Tool. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28 Employee Language Skills Self-Assessment. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29 Employee Language Skills Self-Assessment Key . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 30 Primer on How Cultural Background Impacts Health Care Delivery. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 31 Cultural Background—Information on Special Topics . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32 Regulations and Standards for Cultural and Linguistic Services. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 37 Standards to Provide Culturally and Linguistically Appropriate Services (CLAS) . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 38 Title VI of the Civil Rights Act of 1964. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 39 Executive Order 13166, August 2000, Improving Access to Services for Persons With Limited English Proficiency . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 40 Resources for Cultural and Linguistic Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42 Cultural Competence Website Links to Other Organizations. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 43 Our Health Plan’s Cultural and Linguistic Resources . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 47 Sources Used in the Production of This Toolkit. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 48 Bibliography of Major Hard-Copy Sources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 49 Bibliography of Major Internet Sources. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50 Introduction for Healthcare Professionals: Why Was This Toolkit Created? How Can It Help My Practice? This set of materials was produced by a team of healthcare professionals from across the country who, like you, are dedicated to providing quality, effective, and compassionate care to their patients. Changes in U.S. demography, in our awareness of differences in individual belief and behavior, and new legal mandates continuously present new challenges to deliver access to health care to a diverse patient population. This toolkit was developed to provide you with resources to help address the very specific operational needs that often arise in a busy practice because of the changing service requirements and legal mandates. The toolkit contents are organized into several sections, each containing helpful background information and tools that can be reproduced and used as needed. Here are a list of the section topics and a small sample of their contents. Resources to Assist with a Diverse Patient Population Base: Tips for providers and their clinical staff, a mnemonic to assist with diverse patient interviews, help in identifying literacy problems, and an interview guide for hiring clinical staff with an awareness of cultural competency issues. Resources to Communicate Across Language Barriers: Tips for locating and working with interpreters, common signs and common sentences in many languages, language identification flashcards, and language skill self-assessment tools. Resources to Increase Awareness of Cultural Background and Its Impact on Health Care Delivery: Tips for talking with a wide range of peoples across cultures about a variety of culturally sensitive topics, and information about health care beliefs of various cultural backgrounds. Regulations and Standards for Cultural and Linguistic Services: Some key legislation and a summary of federal “Culturally and Linguistically Appropriate Service (CLAS) Standards,” which serve as a guide on how to meet these requirements. Resources for Cultural and Linguistic Services: A bibliography of print and Internet resources for conducting an assessment of the cultural and linguistic needs of your own practice’s patient population, staff and physician cultural and linguistic competency training resources - plus links to additional tools in multiple languages and/or written for limited English proficiency. This toolkit contains materials developed by and used with the permission of the Industry Collaboration Effort (ICE) Cultural and Linguistics Workgroup, a “volunteer, multi-disciplinary team of providers, health plans, associations, state and federal agencies and accrediting bodies working collaboratively to improve health care regulatory compliance through education of the public.” More information on the ICE Workgroup may be obtained at its website: www.iceforhealth.org. 2 Improving Communications with a Diverse Patient Base Tips for Successful Encounters with Diverse Patients To enable effective patient/provider communication and to avoid being unintentionally insulting or patronizing, be aware of the following: Styles of Speech People vary greatly in length of time between comment and response, the speed of their speech, and their willingness to interrupt. • Tolerate gaps between questions and answers, impatience can be seen as a sign of disrespect. • Listen to the volume and speed of the patient’s speech as well as the content. Modify your own speech to more closely match that of the patient to make them more comfortable. • Rapid exchanges, and even interruptions, are a part of some conversational styles. Don’t be offended when a patient interrupts you if no offense is intended. • Stay aware of your own pattern of interruptions, especially if the patient is older than you are. Eye Contact The way people interpret various types of eye contact can be tied to cultural background and life experience. • Most non-Hispanic Whites expect to look people directly in the eyes and interpret failure to do so as a sign of dishonesty or disrespect. • For many other cultures, direct gazing is considered rude or disrespectful. Never force a patient to make eye contact with you. • If patients seem uncomfortable with direct gazes, try sitting next to them instead of across from them. Body Language Sociologists say that 70% to 90% of communication is nonverbal. The meaning of body language varies greatly by culture, class, gender, and age. • Follow the patient’s lead on physical distance and touching. If the patient moves closer to you or touches 4 Improving Communications with a Diverse Patient Base you, you may do the same. However, stay sensitive to those who do not feel comfortable, and ask permission to touch them. • Gestures can mean very different things to different people. Be very conservative in your own use of gestures and body language. Ask patients about unknown gestures or reactions. • Do not interpret a patient’s feelings or level of pain just from facial expressions. The way that pain or fear is expressed is closely tied to a person’s cultural and personal background. Gently Guide Patient Conversation English predisposes us to a direct communication style; however, other languages and cultures differ. • Initial greetings can set the tone for the visit. Many older people from traditional societies expect to be addressed more formally, no matter how long they have known their physician. If the patient’s preference is not clear, ask how he or she would like to be addressed. • Patients from other language or cultural backgrounds may be less likely to ask questions and more likely to answer questions through narrative than with direct responses. Facilitate patient-centered communication by asking open-ended questions whenever possible. • Avoid questions that can be answered with “yes” or “no.” Research indicates that when patients, regardless of cultural background, are asked, “Do you understand?” many will answer “yes,” even when they really do not understand. This tends to be more common in teens and older patients. • Steer the patient back to the topic by asking a question that clearly demonstrates that you are listening. Some patients can tell you more about their health through storytelling than by answering direct questions. Tips for Office Staff to Enhance Communication with Diverse Patients Build rapport with the patient. • Address patients by their last names. If the patient’s preference is not clear, ask, “How would you like to be addressed?” • Focus your attention on patients when addressing them. Determine if the patient needs an interpreter for the visit. • Document the patient’s preferred language in the patient chart. • Learn basic words in your patient’s primary language, like “hello” or “thank you.” • Have an interpreter access plan. An interpreter with a medical background is preferred, rather than family or friends of the patient. • Recognize that patients from diverse backgrounds may have different communication needs. • Assess your bilingual staff for interpreter abilities. (See Employee Language Skills Self-Assessment Tools.) • Explain to the patient the different roles performed by people who work in the office. • Possible resources for interpreter services are available from health plans, the state health department, and the Internet. (Some resources are listed at the end of this toolkit.) Make sure patients know what you do. • Take a few moments to prepare a handout that explains office hours, how to contact the office when it is closed, and how the doctor arranges for care (when the doctor is the first point of contact and then refers to specialists). • Have instructions translated by a professional translator and available in the common language(s) spoken by your patient base. Recognize that patients from diverse backgrounds may have different communication needs. Keep patients’ expectations realistic. • Inform patients of delays or extended waiting times. If the wait is longer than 15 minutes, encourage the patient to make a list of questions for the doctor, review health materials or view waiting room videos. Give patients the information they need. • Have topic-specific health education materials in languages that reflect your patient base. • Offer handouts such as immunization guidelines for adults and children, screening guidelines, and culturally relevant dietary guidelines for diabetes or weight loss. Make sure patients know what to do. • Review any follow-up procedures with the patient and family before they leave your office. • Verify call back numbers, the locations for follow-up services such as labs, X-ray or screening tests, and whether or not a follow-up appointment is necessary. • Develop pre-printed simple handouts of frequently used instructions, and translate the handouts into the common language(s) spoken by your patient base. NOTE: See commonly used sentences and signs provided in this toolkit. Work to build patients’ trust in you. • Inform patients of office procedures, such as when they can expect a call with lab results, how follow-up appointments are scheduled, and routine wait times. Improving Communications with a Diverse Patient Base 5 Nonverbal Communication and Patient Care Nonverbal communication is a subtle form of communication that is initiated in the first three seconds upon meeting someone for the first time and continues through the entire interaction. Research indicates that nonverbal communication accounts for approximately 70% to 90% of a communication episode. Nonverbal communication can impact the success of communication more acutely than the spoken word. Our culturally informed unconscious framework evaluates gestures, appearance, body language, the face, and and never met her eyes. She reasoned from this that he was uninterested and therefore not listening to her.1 how space is used. Yet, we are rarely aware of how persons from other cultures may perceive our nonverbal communication or the subtle cues we have used to assess the person. Touch and Use of Space The following are case studies that provide examples of nonverbal miscommunication that may sabotage a patient-provider encounter. Broad cultural generalizations are used for illustrative purposes. They should not be mistaken for stereotypes. A stereotype and a generalization may appear similar, but they function very differently: • A stereotype is an ending point; no attempt is made to learn whether the individual in question fits the statement. • A generalization is a beginning point; it indicates common trends, but further information is needed to ascertain whether the statement is appropriate to a particular individual. Generalizations can serve as a guide to be accompanied by individualized in-person assessment. As a rule, ask the patient, rather than assume you know the patient’s needs and wants. If asked, patients will usually share their personal beliefs, practices and preferences related to prevention, diagnosis and treatment. Eye Contact Ellen was trying to teach her Navajo patient, Jim Nez, how to live with his newly diagnosed diabetes. She soon became extremely frustrated because she felt she was not getting through to him. He asked very few questions 6 Improving Communications with a Diverse Patient Base It is rude to meet and hold eye contact with an elder or someone in a position of authority such as health professionals in most Latino, Asian, American Indian and many Arab countries. It may be also considered a form of social aggression if a male insists on meeting and holding eye contact with a female. A physician with a large medical group requested assistance encouraging young female patients to make and keep their first well-woman appointment. The physician stated that this group had a high no-show rate and appointments did not go as smoothly as the physician would like. Talk the patient through each exam so that the need for the physical contact is understood, prior to the initiation of the examination. Ease into the patients’ personal space. If there are any concerns, ask before entering the three-foot zone. This will help ease the patient’s level of discomfort and avoid any misinterpretation of physical contact. Additionally, physical contact between a male and female is strictly regulated in many cultures. An older female companion may be necessary during the visit. Gestures A non-Hispanic White patient named James Todd called out to Elena, a Filipino nurse: “Nurse, nurse.” Elena came to Mr. Todd’s door and politely asked, “May I help you?” Mr. Todd beckoned her to come closer by motioning with his right index finger. Elena remained where she was and responded in an angry voice, “What do you want?” Mr. Todd was confused. Why had Elena’s manner suddenly changed? 2 Gestures may have dramatically different meanings across cultures. It is best to think of gestures as a local dialect that is familiar only to insiders of the culture. Conservative use of hand or body gestures is recommended to avoid misunderstanding. In the case above, Elena took offense to Mr. Todd’s innocent hand gesture. In the Philippines (and in Korea) the “come here” hand gesture is used to call animals. Body Posture and Presentation Carrie was surprised to see that Mr. Ramirez was dressed very elegantly for his doctor’s visit. She was confused by his appearance because she knew that he was receiving services on a sliding fee scale. She thought the front office either made a mistake documenting his ability to pay for service, or that he falsely presented his income. Many cultures prioritize respect for the family and demonstrate family respect in their manner of dress and presentation in public. Regardless of the economic resources that are available or the physical condition of the individual, going out in public involves creating an image that reflects positively on the family—the clothes are pressed, the hair is combed, and shoes are clean. A person’s physical presentation is not an indicator of their economic situation. Use of Voice Dr. Moore had three patients waiting and was feeling rushed. He began asking health-related questions of his Vietnamese patient, Tanya. She looked tense, staring at the ground without volunteering much information. No matter how clearly he asked the question, he couldn’t get Tanya to take an active part in the visit. The use of voice is perhaps one of the most difficult forms of nonverbal communication to change, as we rarely hear how we sound to others. If you speak too fast, you may be seen as not being interested in the patient. If you speak too loud, or too soft for the space involved, you may be perceived as domineering or lacking confidence. Expectations for the use of voice vary greatly between and within cultures, for male and female, and the young and old. The best suggestion is to search for nonverbal cues to determine how your voice is affecting your patient. 1, 2 Galanti, G. (1997). Caring for Patients from Different Cultures. University of Pennsylvania Press. Hall, E.T. (1985). Hidden Differences: Studies in International Communication. Hamburg: Gruner & Jahr. Hall, E.T. (1990). Understanding Cultural Differences. Yarmouth, ME: Intercultural Press. Improving Communications with a Diverse Patient Base 7 “D-I-V-E-R-S-E” – A Mnemonic for Patient Encounters A mnemonic will assist you in developing a personalized care plan based on cultural/diversity aspects. Place in the patient’s chart or use the mnemonic when gathering the patient’s history. Assessment D I 8 Demographics - Explore regional background, level of acculturation, age and sex as they influence health care behaviors. Sample Questions • Where were you born? • Where was “home” before coming to the U.S.? • How long have you lived in the U.S.? • What is the patient’s age and sex? Ideas - Ask the patient to explain • What do you think keeps you healthy? his/her ideas or concepts of health • What do you think makes you sick? and illness. • What do you think is the cause of your illness? • Why do you think the problem started? V Views of health care treatments Ask about treatment preference, use of home remedies, and treatment avoidance practices. E Expectations - Ask about what your • What do you hope to achieve from today’s visit? patient expects from his/her doctor? • What do you hope to achieve from treatment? • Do you find it easier to talk with a male/female? Someone younger/older? R Religion - Ask about your patient’s religious and spiritual traditions. • Will religious or spiritual observances affect your ability to follow treatment? How? • Do you avoid any particular foods? • During the year, do you change your diet in celebration of religious and other holidays? S Speech - Identify your patient’s language needs, including health literacy levels. Avoid using a family member as an interpreter. • What language do you prefer to speak? • Do you need an interpreter? • What language do you prefer to read? • Are you satisfied with how well you read? • Would you prefer printed or spoken instructions? E Environment - Identify patient’s home environment and the cultural/ diversity aspects that are part of the environment. Home environment includes the patient’s daily schedule, support system and level of independence. • Do you live alone? • How many other people live in your house? • Do you have transportation? • Who gives you emotional support? • Who helps you when you are ill or need help? • Do you have the ability to shop/cook for yourself? • What times of day do you usually eat? • What is your largest meal of the day? • Are there any health care procedures that might not be acceptable? • Do you use any traditional or home health remedies to improve your health? • What have you used before? • Have you used alternative healers? Which? • What kind of treatment do you think will work? Improving Communications with a Diverse Patient Base Assessment Information/ Recommendations Improving Communications with a Diverse Patient Base 9 Tips to Identify and Address Health Literacy Issues Low health literacy can prevent patients from understanding their health care services. Health Literacy is defined by the National Health Education Standards as “the capacity of an individual to obtain, interpret, and understand basic health information and services and the competence to use such information and services in ways which are health-enhancing.” This includes the ability to understand written instructions on prescription drug bottles, appointment slips, medical education brochures, doctors' directions, consent forms and the ability to negotiate complex health care systems. Health literacy is not the same as the ability to read and is not necessarily related to years of education. A person who functions adequately at home or work may have marginal or inadequate literacy in a health care environment. 10 Improving Communications with a Diverse Patient Base Barriers to Health Literacy • The ability to read and comprehend health information is impacted by a range of factors including age, socioeconomic background, education and culture. Example: Some seniors may not have had the same educational opportunities afforded to them. • A patient’s culture and life experience may have an effect on their health literacy. Example: A patient’s background culture may stress verbal, not written, communication styles. • An accent, or a lack of an accent, can be misread as an indicator of a person’s ability to read English. Example: A patient, who has learned to speak English with very little accent, may not be able to read instructions on a prescription bottle. Health literacy is not the same as the ability to read and is not necessarily related to years of education. A person who functions adequately at home or work may have marginal or inadequate literacy in a health care environment. • Ask patients to repeat back to you important information. • Ask open-ended questions. • Use medically trained interpreters familiar with cultural nuances. • Give information in small chunks. • Articulate words. • Different family dynamics can play a role in how a patient receives and processes information. • “Read” written instructions out loud. • In some cultures it is inappropriate for people to discuss certain body parts or functions leaving some with a very poor vocabulary for discussing health issues. • Use body language to support what you are saying. • In adults, reading skills in a second language may take 6–12 years to develop. • Use video and audio media as an alternative to written communications. • Speak slowly (don’t shout). • Draw pictures; use posters, models or physical demonstrations. Possible Signs of Low Health Literacy Your patients may frequently say: • I forgot my glasses. • My eyes are tired. • I’ll take this home for my family to read. • What does this say? I don’t understand this. Your patients’ behavior may include: • Not getting their prescriptions filled, or not taking their medications as prescribed. • Consistently arriving late to appointments. • Returning forms without completing them. • Requiring several calls between appointments to clarify instructions. Tips for Dealing with Low Health Literacy • Use simple words and avoid jargon. • Never use acronyms. • Avoid technical language (if possible). • Repeat important information—a patient’s logic may be different from yours. Improving Communications with a Diverse Patient Base 11 Planning Effective Written Patient Communications All medical offices have written communication campaigns to their diverse patient base, whether it is to announce business operation changes, or health improvement reminders about routine vaccinations or the importance of preventive health screenings. Here are some tips to help increase the effectiveness of your office’s written communication campaign. When developing your message, think through what you expect the outcome to be. Ask: • Who is your target audience? • What is the objective of the communication? • What does a patient need to know to get the result you want? • What is the call to action or the desired behavior? • How will you best clarify the benefit of taking this action? If yours is a more targeted mailing campaign, think about gender, age, stage of life (single, family, empty nesters), geography, the type of insurance coverage, and even race/ ethnicity where appropriate. Our health plan conducted extensive research with racial and ethnic minority group patients and found that the most effective communication materials that engaged patients and induced action shared several key elements. These themes are integral components of culturally relevant communication initiatives. We call these themes the “5 F’s”: Food, Family, Faith, Fear, and Finances. • Food. Affinity to cultural foods and difficulties in changing dietary habits • Family. Particularly “being there” for children and grandchildren • Faith and Spirituality. Respecting life as a gift; recognizing faith-based entities as trusted sources of health information 12 Improving Communications with a Diverse Patient Base • Fear. Disease complications, especially amputations, blindness, and kidney disease, or myths regarding adverse outcomes from treatments • Finances. Affordability of health care and healthy lifestyles (e.g., food, gym membership, testing strips, and copays) While all these themes may not always be relevant to a specific communication topic, framing the benefits to the patient -- from defining a call to action to weaving in culturally appropriate and sensitive discussions of the relevant 5 F themes -- may help your message resonate more effectively with your diverse patient base. Tools and Training for Your Office in Caring for a Diverse Patient Base Interview Guide for Hiring Office/Clinic Staff with Diversity Awareness The following set of questions is meant to help you determine whether a job candidate will be sensitive to the cultural and linguistic needs of your patient population. By integrating some or all of these questions into your interview process, you will be more likely to hire staff that will help you create an office/clinic atmosphere of openness, affirmation, and trust between patients and staff. Remember that bias and discrimination can be obvious and flagrant or small and subtle. Hiring practices should reflect this understanding. Sample Interview Questions Q: What experience do you have in working with people of diverse backgrounds, cultures and ethnicities? The experiences can be in or out of a health care environment. The interviewee should demonstrate understanding and willingness to serve diverse communities. Any experience, whether professional or volunteer, is valuable. Q: Please share any particular challenges or successes you have experienced in working with people from diverse backgrounds. You will want to get a sense that the interviewee has an appreciation for working with people from diverse backgrounds and understands the accompanying complexities and needs in an office setting. Q: In the health care field we come across patients of different ages, language preferences, sexual orientations, religions, cultures, genders, and immigration status, etc. all with different needs. What skills from your past customer service or community/healthcare work do you think are relevant to this job? This question should allow a better understanding of the interviewee's approach to customer service across the spectrum of diversity, his or her previous experience, and if his or her skills are transferable to the position in question. Look for examples that demonstrate an understanding of varying needs. Answers should demonstrate listening and clear communication skills. Q: What would you do to make all patients feel respected? For example, some Medicaid or Medicare recipients may be concerned about receiving substandard care because they lack private insurance. The answer should demonstrate an understanding of the behaviors that facilitate respect and the type of prejudices and bias that can result in substandard service and care. 14 Tools and Training for Your Office in Caring for a Diverse Patient Base Online Medical Consumer Training Resources for Health Educators to Share with Patients Racial and ethnic minority communities as a whole have had greater difficulty with the American health care system than white Americans. One in three Hispanics and one in four African Americans and Asian Americans report experiencing difficulties communicating with health care providers as opposed to one in six white Americans (The Commonwealth Fund, 2002). More recently, the 2010 National Healthcare Disparities Report (NHDR), which tracked patient-provider communication, found that between 2002 and 2007, the percentage of White, middle-income, and high-income adults who reported poor communication with their health providers significantly decreased. Such reticence often leads to a common scenario in which a doctor would say, “but the patient seemed like he understood my instructions; why didn’t he follow my treatment plan?” Research has shown that successful programs to close the gap in chronic disease-related health disparities in various racial and ethnic populations are built on strengthening the links between health care providers and their patients (Roe & Thomas, 2002). However, racial and ethnic disparities in patient reports of provider communication have persisted over the past decade. • In all years, Hispanics were significantly more likely than non-Hispanic Whites to report poor communication. • In 4 of 6 years, Black patients were more likely than Whites to report poor communication with health providers; the exceptions were 2006 and 2007. • In 5 of 6 years, Asians were more likely than Whites to report poor communication; the exception was 2007. Patients may not have the communication skills needed to share information vital to accurate diagnosis or optimal treatment. In cases of patients with diverse ethnic backgrounds, linguistic, cultural and/or health literacy may be barriers to being active participants of their own health care. These same barriers may also keep patients from speaking up to: • Ask questions to fully understand their medical conditions or treatment instructions • Share personal challenges in adhering to recommended treatment Tools and Training for Your Office in Caring for a Diverse Patient Base 15 On the one hand, while training courses abound for clinicians on effective cross-cultural communication skills, there are scant few resources that guide patients to be more empowered health care consumers. We support health care professionals and health educators in encouraging patients to be more active, engaged and empowered health care consumers. We have created a web-based resource to help health care professionals guide patients toward improving their medical consumerism skills such as: • How to prepare for health care visits • How to communicate effectively with health care professionals • How to navigate of the U.S. health care system • Different types of medical providers and care settings • U.S. concepts of health, wellness and medicine • Patient’s rights and responsibilities • Access to health education program offerings (public sources as well as those from health plans such as disease management or health coaching programs) This course is available at no cost to all health care professionals at BridgingHealthCareGaps.com. _________________________________________________ Agency for Healthcare Research and Quality (2010 June). The 2010 National Healthcare Disparities Report (NHDR). The Commonwealth Fund (2002, March). Diverse communities, common concerns: Assessing health care quality for minority Americans. Roe, K., & Thomas, S. (2002). Acknowledgements. Health Promotion Practice, 3(October), 106-107. 16 Tools and Training for Your Office in Caring for a Diverse Patient Base Resources to Communicate Across Language Barriers Tips for Communicating Across Language Barriers Limited English Proficient (LEP) patients are faced with language barriers that undermine their ability to understand information given by healthcare providers as well as instructions on prescriptions and medication bottles, appointment slips, medical education brochures, doctors' directions, and consent forms. They experience more difficulty (than other patients) processing information necessary to care for themselves and others. Tips to Identify a Patient’s Preferred Language • Ask the patient for his or her preferred spoken and written language. • Display a poster of common languages spoken by patients; ask them to point to their language of preference. • Post information relative to the availability of interpreter services. • Make available and encourage patients to carry “I speak…” or “Language ID” cards. (Note: Many phone interpreter companies provide language posters and cards at no charge.) Tips to Document Patient Language Needs • For all Limited English Proficient (LEP) patients, document preferred language in paper and/or electronic medical records. • Post color stickers on the patient’s chart to flag when an interpreter is needed. (e.g., Orange=Spanish, Yellow=Vietnamese, Green=Russian). Tips to Assess Which Type of Interpreter to Use • Telephone interpreter services are easily accessed and available for short conversations or unusual language requests. • Face-to-face interpreters provide the best communication for sensitive, legal or long communications. • Trained bilingual staff provides consistent patient interactions for a large number of patients. • For reliable patient communication, avoid using minors and family members. 18 Resources to Communicate Across Language Barriers Tips to Overcome Language Barriers • Use simple words; avoid jargon and acronyms. • Limit/avoid technical language. • Speak slowly (don’t shout). • Articulate words completely. • Repeat important information. • Provide educational material in the languages your patients read. • Use pictures, demonstrations, video or audiotapes to increase understanding. • Give information in small chunks and verify comprehension before going on. • Always confirm that the patient understands the information— the patient’s logic may be different from yours. 10 Tips for Working with Interpreters 1. Choose an interpreter who meets the needs of the patient, considering age, sex and background. A patient might be reluctant to disclose personal and sensitive information, for example, in front of an interpreter of a different sex. 2. Hold a brief introductory discussion with the interpreter. If it is your first time working with a professional interpreter, briefly meet with the interpreter first to agree on basic interpretation protocols. Let the interpreter brief the patient on the interpreter’s role. 3. Allow enough time for the interpreted sessions. Remember that an interpreted conversation requires more time. What can be said in a few words in one language may require a lengthy paraphrase in another. 4. Speak in a normal voice, clearly, and not too fast or too loudly. It is usually easier for the interpreter to understand speech produced at normal speed and with normal rhythms, than artificially slow speech. 5. Avoid acronyms, jargon, and technical terms. Avoid idioms, technical words, or cultural references that might be difficult to translate. Some concepts may be easy for the interpreter to understand but extremely difficult to translate (e.g., positive test results). 6. Face the patient and talk to the patient directly. Be brief, explicit and basic. Remember that you are communicating with the patient through an interpreter. Pause after a full thought for the interpretation to be accurate and complete. If you speak too long, the interpreter may not remember and miss what was said. 7. Don’t ask or say anything that you don’t want the patient to hear. Expect everything you say to be interpreted, and everything the patient and his or her family says. 8. Be patient and avoid interrupting during interpretation. Allow the interpreter as much time as necessary to ask questions, for repeats, and for clarification. Be prepared to repeat yourself in different words if your message is not understood. Professional interpreters do not translate word-for-word but rather concept-by-concept. Also remember that English is a direct language, and may need to be relayed into complex grammar and a different communication pattern. 9. Be sensitive to appropriate communication standards. Different cultures have different protocols to discuss sensitive topics and to address physicians. Many ideas taken for granted in America do not exist in the patient’s culture and may need detailed explanation in another language. Take advantage of your interpreter’s insight and let the interpreter be your “Cultural Broker.” 10.Read body language in the cultural context. Watch the patient’s eyes, facial expression, or body language when you speak and when the interpreter speaks. Look for signs of comprehension, confusion, agreement, or disagreement. Note: When working with interpreters, reassure the patient that the information will be kept confidential. Resources to Communicate Across Language Barriers 19 Tips for Locating Interpreter Services First, assess the oral linguistic needs of your Limited English Proficient (LEP) patients. Second, assess the services available to meet these needs. Assess the language capability of your staff (See Employee Language Skills Self-Assessment) • Keep a list of available bilingual staff who can assist with LEP patients on-site. • Assess services available through patient health plans. • Ask all health plans you work with if and when they provide interpreter services, including American Sign Language interpreters, as a covered benefit for their members. Keep an updated list of specific telephone numbers and health plan contacts for language services. • Identify the policies and procedures in place to access interpreter services for each plan you work with. • Keep an updated list of specific telephone numbers and health plan contacts for language services. • Ask the agency providing the interpreter for their training standards and methods of assessing interpreter quality. • Don’t forget to inquire about Telecommunication Device for the Deaf (TDD) services for the hard of hearing/deaf. If services are covered, identify the appropriate contact and request the health plan’s process to access services. • Determine if face-to-face and/or telephone interpreters are covered. • If face-to-face interpreters are covered, have the following information ready before requesting the interpreter: gender, age, language needed, date/time of appointment, type of visit, and office specialty. 20 Resources to Communicate Across Language Barriers - Remember to follow all HIPAA regulations when transmitting any patient-identifiable information to parties outside your office. • If telephone interpreters are covered, relay the pertinent patient information which will help the interpreter better serve the needs of the patient and the provider. If interpreter services are NOT covered by the patient’s health plan, find other resources to meet the linguistic needs of your LEP patients. • Use trained/capable internal staff. • Consider contracting with a telephonic interpreting company. • Check for services available through Community Based Organizations. Some provide free face-to-face interpreter services for the community or they may offer low fees. • Depending on the linguistic needs of your LEP population, you may have to consider hiring a professional interpreter. • For further information, you may contact the National Council on Interpretation in Health Care, the Society of American Interpreters, the Translators & Interpreters Guild, the American Translators Association, or any local Health Care Interpreters association in your area. U.S. Census Language Identification Flashcards The sheets in this tool can be used to assist the office staff or physician in identifying the language that your patient is speaking. Pass the sheets to the patient and point to the English statement. Motion to the patient to read the other languages and to point to the language that the patient prefers. (Conservative gestures can communicate this.) Record the patient’s language preference in his or her medical record. The Language Identification Flashcards were developed by the U.S. Census Department and can be used to identify most languages that are spoken in the United States. Resources to Communicate Across Language Barriers 21 2004 Census Test 2010 LANGUAGE IDENTIFICATION FLASHCARD .á«Hô©dG çóëàJ hCG CGô≤J âæc GPEG ™HôŸG Gòg ‘ áeÓY ™°V 1. Arabic 2. Armenian 3. Bengali QUmbJÇak'kñ¨g®b/b'enH ebI/ñk/an …niXaXPasa e‡oµe . 4. Cambodian Motka i kahhon ya yangin ûntûngnu' manaitai pat ûntûngnu' kumentos Chamorro. 5. Chamorro 6. Simplified Chinese 7. Traditional Chinese Označite ovaj kvadratić ako čitate ili govorite hrvatski jezik. 8.Croatian Zaškrtněte tuto kolonku, pokud čtete a hovoříte česky. 9. Czech Kruis dit vakje aan als u Nederlands kunt lezen of spreken. 10. Dutch Mark this box if you read or speak English. 11. English 12. Farsi DB-3309 U.S. DEPARTMENT OF COMMERCE Economics and Statistics Administration U.S. CENSUS BUREAU 22 Resources to Communicate Across Language Barriers Cocher ici si vous lisez ou parlez le français. 13. French Kreuzen Sie dieses Kästchen an, wenn Sie Deutsch lesen oder sprechen. 14. German 15. Greek 16. Haitian Creole Make kazye sa a si ou li oswa ou pale kreyòl ayisyen. 17. Hindi Kos lub voj no yog koj paub twm thiab hais lus Hmoob. 18. Hmong Jelölje meg ezt a kockát, ha megérti vagy beszéli a magyar nyelvet. 19. Hungarian Markaam daytoy nga kahon no makabasa wenno makasaoka iti Ilocano. 20. Ilocano Marchi questa casella se legge o parla italiano. 21. Italian 22. Japanese 23. Korean 24. Laotian Prosimy o zaznaczenie tego kwadratu, jeżeli posługuje się Pan/Pani językiem polskim. DB-3309 25. Polish U.S. DEPARTMENT OF COMMERCE Economics and Statistics Administration U.S. CENSUS BUREAU Resources to Communicate Across Language Barriers 23 26. Portuguese Assinale este quadrado se você lê ou fala português. 27. Romanian �ометьте этот квадратик, если вы читаете или говорите по-русски. 28. Russian 29. Serbian Označte tento štvorček, ak viete čítať alebo hovoriť po slovensky. 30. Slovak Marque esta casilla si lee o habla español. 31. Spanish Markahan itong kuwadrado kung kayo ay marunong magbasa o magsalita ng Tagalog. 32. Tagalog 33. Thai Maaka 'i he puha ni kapau 'oku ke lau pe lea fakatonga. 34. Tongan �ідмітьте цю клітинку, якщо ви читаєте або говорите українською мовою. 35. Ukranian 36. Urdu Xin ñaùnh daáu vaøo oâ naøy neáu quyù vò bieát ñoïc vaø noùi ñöôïc Vieät Ngöõ. 37. Vietnamese 38. Yiddish DB-3309 U.S. DEPARTMENT OF COMMERCE Economics and Statistics Administration U.S. CENSUS BUREAU 24 Resources to Communicate Across Language Barriers Common Signs in Multiple Languages (English-Spanish-Vietnamese-Chinese) You may wish to use this tool to mark special areas in your office to help your Limited English Proficient (LEP) patients. It is suggested that you laminate each sign and post it. English Español Tieáng Vieät 中文 Welcome Spanish Vietnamese Chinese English Español Tieáng Vieät 中文 Tieáng Vieät 中文 Spanish Vietnamese Chinese 中文 Spanish Vietnamese Chinese Tieáng Vieät 中文 Oficina de Registro QuaÀy tieáp khaách 登記處 Cajera Quaày traû tieàn 收銀部 Enter Spanish Entrada Vietnamese Loái vaøo Chinese English Español 歡迎 Cashier English Español Haân haïnh tieáp ñoùn quyù vò Registration English Español Bienvenido/a 入口 Restroom Spanish Vietnamese Chinese Baños Phoøng veä sinh 洗手間 Resources to Communicate Across Language Barriers 25 Common Sentences in Multiple Languages (English-Spanish-Vietnamese-Chinese) This tool is designed for office staff to assist in basic entry-level communication with Limited English Proficient (LEP) patients. Point to the sentence you wish to communicate and your LEP patient may read it in his/her language of preference. The patient can then point to the next message. English Chinese / 中文 Spanish / Español ☛ ☛ ☛ ☛ ☟ Point to a sentence Señale una frase Xin chæ vaøo caâu 指向句子 Instructions Instrucciones Chæ Daãn 指示 We can use these cards to help us understand each other. Point to the sentence you want to communicate. If needed, later we will call an interpreter. Chuùng ta coù theå duøng nhöõng theû naøy ñeå giuùp chuùng ta hieåu nhau. Xin chæ vaøo caâu ñuùng nghóa quyù vò muoán noùi. Chuùng toâi seõ nhôø moät thoâng dòch vieân ñeán giuùp neáu chuùng ta caàn noùi nhieàu hôn. Podemos utilizar estas tarjetas para entendernos. Señale la frase que desea comunicar. Si necesita, después llamaremos a un intérprete. 這卡可以幫助大家更明白 對方。請指向您想溝通的 句子, 如有需要,稍後我 們可以為您安排傳譯員。 ☟ Courtesy statements Frases de cortesía Töø ngöø lòch söø 禮貌敘述 Please wait. Por favor espere (un momento). Xin vui loøng chôø. 請等等 Thank you. Gracias. Caùm ôn. 多謝 One moment, please. Un momento, por favor. Xin ñôïi moät chuùt. 請等一會 ☛ Point to a sentence Señale una frase Xin chæ vaøo caâu 指向句子 Patient may say… El paciente puede decir… Beänh nhaân coù theå noùi… 病人可能會說… ☛ ☟ ☛ ☛ 26 ☛ 指向句子 ☛ Xin chæ vaøo caâu ☛ Señale una frase ☛ ☟ Point to a sentence My name is… Mi nombre es... Toâi teân laø... 我的名字是… I need an interpreter. Necesito un intérprete. Chuùng toâi caàn thoâng dòch vieân. 我需要一位傳譯員… I came to see the doctor, because… Vine a ver al doctor porque… Toâi muoán gaëp baùc só vì… I don’t understand. No entiendo. Toâi khoâng hieåu. 我不明白 Please hurry. It is urgent. Por favor apúrese. Es urgente. Vui loøng nhanh leân. Toâi coù chuyeän khaån caáp. 請盡快,這是非常緊急。 Where is the bathroom? ¿Dónde queda el baño? Phoøng veä sinh ôû ñaâu? 洗手間在那裏? How much do I owe you? ¿Cuánto le debo? Toâi caàn phaûi traû bao nhieâu tieàn? 可否找一位傳譯員? Is it possible to have an interpreter? ¿ Es posible tener un intérprete? Coù theå nhôø moät thoâng dòch 傳譯員就快到。 vieân ñeán giuùp chuùng ta khoâng? Resources to Communicate Across Language Barriers 我來見醫生是因為… English Chinese / 中文 Spanish / Español ☛ ☛ ☛ ☛ ☟ Point to a sentence Señale una frase Xin chæ vaøo caâu 指向句子 Staff may ask or say… El personal del médico le puede decir… Nhaân vieân coù theå hoûi hoaëc noùi… 職員可能會問或說… How may I help you? ¿En qué puedo ayudarle? Toâi coù theå gíup ñöôïc gì? 我怎樣可以幫您呢? I don’t understand. Please wait. No entiendo. Por favor espere. Toâi khoâng hieåu. Xin ñôïi moät chuùt. 我不明白,請等等。 What language do you prefer? ¿Qué idioma prefiere? Quí vò thích duøng ngoân ngöõ naøo? 您喜歡用什麼語言呢 : • Cantonese 廣東話 • Mandarin 國語 We will call an interpreter. Vamos a llamar a un intérprete. Chuùng toâi seõ goïi thoâng dòch vieân 我們會找一位傳譯員。 An interpreter is coming. Ya viene un intérprete. Seõ coù moät thoâng dòch vieân ñeán giuùp chuùng ta. 傳譯員就快到。 What is your name? ¿Cuál es su nombre? Quùy vò teân gì? 您叫什麼名字 ? ¿Quién es el paciente? Ai laø beänh nhaân? 誰是病人 ? Please write the patient’s: Por favor escriba, acerca del paciente: Xin vieát lyù lòch cuûa beänh nhaân: 請寫出病人的 : Name Nombre Teân 姓名 Address Dirección Ñòa Chæ 地址 Telephone number Número de teléfono Soá Ñieän Thoaïi 電話號碼 Identification number Número de identificación Soá ID 醫療卡號碼 Birth date: Fecha de nacimiento: Ngaøy Sinh: 出生日期 : Who is the patient? Month/Day/Year Mes/Día/Año Thaùng/Ngaøy/Naêm 月/日/年 Now, fill out these forms, please Ahora, por favor conteste estas formas. Baây giôø xin ñieàn nhöõng ñôn naøy. 現在,請填寫這表格 ☟ Resources to Communicate Across Language Barriers 27 Employee Language Skills Self-Assessment Tool The attached self-assessment tool can assist you in identifying language skills and resources existing in your health care setting. This simple tool will provide a basic and subjective idea of the bilingual capabilities of your staff. We recommend that you distribute the tool to all your clinical and non-clinical employees using their non-English language skills in the workplace. The information collected may be used as a first step to improve communication with your diverse patient base. You may wish to write an introductory note along the following lines: “We are committed to maintaining our readiness to serve the needs of our patients. Many of our employees could use their skills in languages other than English. We are compiling information about resources available within our work force. Please complete and return this survey to <department/contact> no later than <date>. This survey will not affect your performance evaluation. It is just a way for us to improve our customer service, and to make you part of such efforts. Thank you for your assistance.” Once bilingual staff have been identified, they should be referred to professional assessment agencies to evaluate the level of proficiency. There are many sources that will help you assess the bilingual capacity of staff. Depending on their level of confirmed fluency, your practice would be able to make use of this added value to help your practice better communicate with your patients in the client’s language of preference. 28 Resources to Communicate Across Language Barriers Employee Language Skills Self-Assessment Thank you for participating in this survey process. This survey is for staff who currently use their skills in languages other than English to communicate with our patients. Be assured that this survey will not affect your performance evaluation. This is a way for us to identify our linguistic strengths, determine training opportunities, improve our customer service and include you in our diversity efforts. Employee Name:_____________________________ Department:__________________________ Work hours:q 8am–5pm q9am-6pm Directions: (1) Write any/all language(s) or dialects you know. qother_____ (2) Indicate how fluently you speak, read and/or write in that language. (see attached key) (3) Specify if you currently use this language regularly in your job. E X A M P L E Language Dialect, region… Speaking Reading Writing do you speak… do you read… do you write… Spanish Mexico 12345 12345 12345 Yes No Yes No Yes No As part of your job, do you use this language to speak with patients? (Circle) As part of your job, do you read this language? (Circle) As part of your job, do you write this language? (Circle) Language Dialect, region or country Fluency: see attached key (Circle) Speaking Reading Writing 1. 12345 12345 12345 Yes No Yes No Yes No 2. 12345 12345 12345 Yes No Yes No Yes No 3. 12345 12345 12345 Yes No Yes No Yes No 4. 12345 12345 12345 Yes No Yes No Yes No Resources to Communicate Across Language Barriers 29 Employee Language Skills Self-Assessment Key Key for Spoken Language Capability Key Spoken Language (1) Satisfies elementary needs and minimum courtesy requirements. Able to understand and respond to 2-3 word entry-level questions. May require slow speech and repetition. (2) Meets basic conversational needs. Able to understand and respond to simple questions. Can handle casual conversation about work, school, and family. Has difficulty with vocabulary and grammar. (3) Able to speak the language with sufficient accuracy and vocabulary to have effective formal and informal conversations on most familiar topics related to health care. (4) Able to use the language fluently and accurately on all levels related to work needs. Can understand and participate in any conversation within the range of his/her experience with a high degree of fluency and precision of vocabulary. Unaffected by rate of speech. (5) Speaks proficiently equivalent to that of an educated native speaker. Has complete fluency in the language such that speech in all levels is fully accepted by educated native speakers in all its features, including breadth of vocabulary and idioms, colloquialisms, and pertinent cultural preferences. Usually has received formal education in target language. Key for Reading Capability Key Reading (1) No functional ability to read. Able to understand and read only a few key words. (2) Limited to simple vocabulary and sentence structure. (3) Understands conventional topics, non-technical terms and health care terms. (4) Understands materials that contain idioms and specialized terminology; understands a broad range of literature. (5) Understands sophisticated materials, including those related to academic, medical and technical vocabulary. Key for Writing Capability 30 Key Writing (1) No functional ability to write the language and is only able to write single elementary words. (2) Able to write simple sentences. Requires major editing. (3) Writes on conventional and simple health care topics with few errors in spelling and structure. Requires minor editing. (4) Writes on academic, technical, and most health care and medical topics with few errors in structure and spelling. (5) Writes proficiently equivalent to that of an educated native speaker/writer. Writes with idiomatic ease of expression and feeling for the style of language. Proficient in medical, healthcare, academic and technical vocabulary. Resources to Communicate Across Language Barriers Primer on How Cultural Background Impacts Health Care Delivery Cultural Background— Information on Special Topics Use of Alternative or Herbal Medications • People who have lived in poverty, or come from places where medical treatment is difficult to get, will often come to the doctor only after trying many traditional or home treatments. Usually patients are very willing to share what has been used if asked in an accepting, nonjudgmental way. This information is important for the accuracy of the clinical assessment. • Many of these treatments are effective for treating the symptoms of illnesses. However, some patients may not be aware of the difference between treating symptoms and treating the disease. • Some treatments and “medicines” that are considered “folk” medicine or “herbal” medications in the United States are part of standard medical care in other countries. Asking about the use of medicines that are “hard to find” or that are purchased “at special stores” may get you a more accurate understanding of what people are using than asking about “alternative,” “traditional,” “folk,” or “herbal” medicine. Pregnancy and Breastfeeding • Preferred and acceptable ages for a first pregnancy vary from culture to culture. Latinos are more accepting of teen pregnancy; in fact it is quite common in many of the countries of origin. Russians tend to prefer to have children when they are older. It is important to understand the cultural context of any particular pregnancy. Determine the level of social support for the pregnant woman, which may not be a function of age. • Acceptance of pregnancy outside of marriage also varies from culture to culture and from family to family. In many Asian cultures there is often a profound stigma associated with pregnancy outside of marriage. However, it is important to avoid making assumptions about how welcome any pregnancy may be. • Some Vietnamese and Latino women believe that colostrum (a fluid in the breasts that nourishes the baby until the 32 breast milk becomes available) is not good for a baby. An explanation from the doctor about why the milk changes can be the best tool to counter any negative traditional beliefs. • The belief that breastfeeding works as a form of birth control is very strongly held by many new immigrants. It is important to explain to them that breastfeeding does not work as well for birth control if the mother gets plenty of good food, as they are more able to do here than in other parts of the world. Some treatments and “medicines” that are considered “folk” medicine or “herbal” medications in the United States are part of standard medical care in other countries. Weight • In many poor countries, and among people who come from them, “chubby” children are viewed as healthy children because historically they have been better able to survive childhood diseases. Remind parents that sanitary conditions and medical treatment here protect children better than extra weight. • In many of the countries that immigrants come from, weight is seen as a sign of wealth and prosperity. It has the same cultural value as thinness has in our culture— treat it as a cultural as well as a medical issue for better success. Infant Health • It is very important to avoid making too many positive comments about a baby’s general health. - Among traditional Hmong, saying a baby is “pretty” or “cute” may be seen as a threat because of fears that spirits will be attracted to the child and take it away. Resources to Increase Awareness of Cultural Background and Its Impact on Health Care Delivery - Some traditional Latinos will avoid praise to avoid attracting the “evil eye.” - Some Vietnamese consider profuse praise as mockery. • It is often better to focus on the quality of the mother’s care—“the baby looks like you take care of him well.” • Talking about a new baby is an excellent time to introduce the idea that preventive medicine should be a regular part of the new child’s experience. Well-baby visits may be an entirely new concept to some new mothers from other countries. Protective immunizations are often the most accepted form of preventive medicine. It may be helpful to explain well-baby visits and check-ups as a kind of extension of the immunization process. Substance Abuse • When asking questions regarding issues of substance (or physical) abuse, concerns about family honor and privacy may come into play. For example, in Vietnamese and Chinese cultures family loyalty, hierarchy, and filial piety are of the utmost importance and may therefore have a direct effect on how a patient responds to questioning, especially if family members are in the same room. Separating family members, even if there is some resistance to the idea, may be the only way to accurately assess some of these problems. • Women may have been raised with different standards of personal control and autonomy than we expect in the United States. They may be accepting physical abuse not because of feelings of low self-esteem, but because it is socially accepted among their peers, or because they have nobody they can go to with their concerns. It is important to treat these cases as social rather than psychological problems. • Immigrants learn quickly that abuse is reported and will lead to intervention by police and social workers. Even victims may not trust doctors, social workers, or police. It may take time and repeated visits to win the trust of patients. Remind patients that they do not have to answer questions (silence may tell you more than misleading answers). Using depersonalized conversational methods will increase success in reaching reluctant patients. • Families may have members with conflicting values and rules for acceptable behavior that may result in conflicting reports about suspected physical abuse. This does not necessarily mean that anyone is being deceptive, just seeing things differently. This may cause special difficulties for teens who may have adopted new cultural values common to Western society, but must live in families that have different standards and behaviors. • Gender roles are often expressed in the use or avoidance of many substances, especially alcohol and cigarettes. When discussing and treating these issues the social component of the abuse needs to be considered in the context of the patient’s culture. • Behavioral indicators of abuse are different in different cultures. Many people are not very emotionally and physically expressive of physical and mental pain. Learn about the cultural norms of your patient populations to avoid overlooking or misinterpreting unknown signs of trauma. • Alcohol is considered part of the meal in many societies and should be discussed together with eating and other dietary issues. • Do not confuse physical evidence of traditional treatments with physical abuse. Acceptable traditional treatments, such as coin rubbing or cupping, may leave marks on the skin, which look like physical abuse. Always consider this possibility if you know the family uses traditional home remedies. Physical Abuse • Ideas about acceptable forms of discipline vary from culture to culture. In particular, various forms of corporal punishment are accepted in many places. Emphasis must be placed on what is acceptable here, and what may cause physical harm. Resources to Increase Awareness of Cultural Background and Its Impact on Health Care Delivery 33 Cultural Background—Information on Special Topics (continued) Communicating with the Elderly Gender roles • Always address older patients using formal terms of address unless you are directly told that you may use personal names. Also remind staff that they should do the same. • Gender roles vary and change as the person ages (e.g., women may have much more freedom to openly discuss sexual issues as they age). • Stay aware of how the physical setting may be affecting the patient. Background noise, glaring or reflecting light, and small print forms are examples of things that may interfere with communication. The patients may not say anything, or even be aware that something physical is interfering with their understanding. • Stay aware that many people believe that giving a patient a terminal prognosis is unlucky or will bring death sooner and families may not want the patient to know exactly what is expected to happen. If the family has strong beliefs along these lines the patient probably shares them. Follow ethical and legal requirements, but stay cognizant of the patient’s cultural perspective. Offer the opportunity to learn the truth, at whatever level of detail desired by the patient. • It is important to explain the specific needs for having an advance directive before talking about the treatment choices and instructions. This will help alleviate concerns that an advance directive is for the benefit of the medical staff rather than the patient. • Elderly, low-literacy patients may be very skilled at disguising their lack of reading skills and may feel stigmatized by their inability to read. If you suspect this is the case you should not draw attention to this issue but seek out other methods of communication. Talking About Sex Consider the following strategies when navigating the cultural issues surrounding the collection of sexual health histories. Areas of cultural variation points to consider are: 34 • A patient may not be permitted to visit providers of the opposite sex unaccompanied (e.g., a woman’s husband or mother-in-law will accompany her to an appointment with a male provider). • Some cultures prohibit the use of sexual terms in front of someone of the opposite sex or an older person. • Several family members may accompany an older patient to a medical appointment as a sign of respect and family support. • Before entering the exam room, tell the patient and their companion exactly what the examination will include and what needs to be discussed. Offer the option of calling the companion(s) back into the exam room immediately following the physical exam. • As you invite the companion or guardian to leave the exam room, have a health professional of the same gender as the patient standing by and re-assure the companion or guardian that the person will be in the room at all times. • Use same sex non-family members as interpreters. Sexual health and patient cultural background • If a sexual history is requested during a non-related illness appointment, patients may conclude that the two issues— for example, blood pressure and sexual health are related. • In many health belief systems there are connections between sexual performance and physical health that are different from the Western tradition. Example: Chinese males may discuss sexual performance problems in terms of a “weak liver.” Resources to Increase Awareness of Cultural Background and Its Impact on Health Care Delivery • Printed materials on topics of sexual health may be considered inappropriate reading materials. • Explain to the patient why you are requesting sexually related information at that time. • For young adults, clarify the need for collecting sexual history information and consider explaining how you will protect the confidentiality of their information. • Offer sexual health education verbally. Whenever possible, provide sexual health education by a health care professional who is the same gender as the patient. Confidentiality preferences • Patients may not tell you about their preferences and customs surrounding the discussion of sexual issues. You must watch their body language for signals of discomfort, or ask directly how they would like to proceed. • A patient may be required to bring family members to their appointment as companions or guardians. Printed materials on topics of sexual health may be considered inappropriate reading materials. • Be attentive to a patient’s body language or comments that may indicate that they are uncomfortable discussing sexual health with a companion or guardian in the room. • It may help to apologize for the need to ask sexual or personal questions. Apologize and explain the necessity. • Try to offer the patient a culturally acceptable way to have a confidential conversation. Example: “To provide complete care, I prefer one-on-one discussions with my patients. However, if you prefer, you may speak with a female/male nurse to complete the initial information.” • Inform the patient and the accompanying companion(s) of any applicable legal requirements regarding the collection and protection of personal health information. Pain Management Across Cultures Your ability to provide adequate pain management to some patients can be improved with a better understanding of the differences in the way people deal with pain. Here is some important information about the cultural variations you may encounter when you treat patients for pain management. These tips are generalizations only. It is important to remember that each patient should be treated as an individual. Do not mistake lack of verbal or facial expression for lack of pain. Under-treatment of pain is a problem in populations where stoicism is a cultural norm. Reaction to pain and expression of pain • Cultures vary in what is considered acceptable expression of pain. As a result, expression of pain will vary from stoic to extremely expressive for the same level of pain. • Some men may not verbalize or express pain because they believe their masculinity will be questioned. • Do not mistake lack of verbal or facial expression for lack of pain. Under-treatment of pain is a problem in populations where stoicism is a cultural norm. • Because the expression of pain varies, ask the patient what level, or how much, pain relief they think they need. • Do not be judgmental about the way someone is expressing their pain, even if it seems excessive or inappropriate to you. The way a person in pain behaves is socially learned. Spiritual and religious beliefs about using pain medication • Members of several faiths will not take pain relief medications on religious fast days, such as Yom Kippur or daylight hours of Ramadan. For these patients, religious observance may be more important than pain relief. • Other religious traditions forbid the use of narcotics. Resources to Increase Awareness of Cultural Background and Its Impact on Health Care Delivery 35 Cultural Background—Information on Special Topics (continued) • Spiritual or religious traditions may affect a patient’s preference for the form of medication delivery, oral, IV, or IM. • Consultation with the family and Spiritual Counselor will help you assess what is appropriate and acceptable. Variation from standard treatment regimens may be necessary to accommodate religious practices. • Accommodating religious preferences, when possible, will improve the effectiveness of the pain relief treatment. • Offer a choice of medication delivery. If the choice is less than optimal, ask why the patient has that preference and negotiate treatment for best results. Use of alternative pain relief treatment • Your patient may be using traditional pain relief treatment, such as herbal compresses or teas, massage, acupuncture or breathing exercises. • Respectfully inquire about all of the ways the patient is treating his or her pain. • Use indirect questions about community or family traditions for pain management to provide hints about what the patient may be using. There may be some reluctance to tell you about alternative therapies until they feel it is “safe” to talk about them. • Accommodate or integrate your treatments with alternative treatments when possible. Methods needed to assess pain • Most patients are able to describe their pain using a progressive scale, but others are not comfortable using a numerical scale, and the scale of facial expressions (smile to grimace) may be more useful. • Ask the patient specifically how they can best describe their pain. Beliefs about drug addiction • Use multiple methods of assessing pain—scales and analogies, if you feel the assessment of pain is producing ambiguous or incorrect results. • Recent research has shown that people from different genetic backgrounds react to pain medication differently. Family history and community tradition may contain evidence about specific medication effects in the population. • Once the severity of the pain can be assessed, explain in detail the expected result of the use of the pain medication in terms of whatever descriptive toolsthe patient has used. Check comprehension with teach-back techniques. • Past negative experience with pain medication shapes current community beliefs, even if the medications and doses have changed. • Instead of using scales, which might not be known to the patient, asking for comparative analogies, such as “like a burn from a stove,” “cutting with a knife,” or “stepping on a stone,” may produce a more accurate description. • Be aware of potential differences in the way medication acts in different populations. A patient’s belief that he or she is more easily addicted may have a basis in fact. • Explain how the determination of type and amount of medication is made. Explain changes from past practices. Accommodate or integrate your treatments with alternative treatments when possible. • Assure your patient you are watching his or her particular case. 36 Resources to Increase Awareness of Cultural Background and Its Impact on Health Care Delivery Regulations and Standards for Cultural and Linguistic Services Standards to Provide Culturally and Linguistically Appropriate Services (CLAS) Below is an informal summary of excerpts from the Office of Minority Health’s publication entitled “Assuring Cultural Competence in Health Care: Recommendations for National Standards and an Outcomes-Focused Research Agenda.” 1. Patients/consumers must receive from all staff: effective, understandable, and respectful care that is provided in a manner compatible with their cultural health beliefs and practices of preferred language. 9. Organizational self-assessments must be conducted regarding CLAS-related activities, and cultural and linguistic competence measures should be incorporated into internal audits, performance improvement programs, patient satisfaction assessments, and outcome-based valuations. 2. Strategies should be implemented to recruit, retain, and promote a diverse staff and organizational leadership that are representative of the demographic characteristics of the service area. 10. Data on race, ethnicity, and language difference should be collected in patient/consumer health records, integrated into the information management systems and updated periodically. 3. Staff at all levels and across all disciplines should receive ongoing education and training in culturally and linguistically appropriate service delivery. 11. Current demographic, cultural, and epidemiological profiles of the communities served should be maintained, as well as needs assessments to accurately plan for and implement services that respond to the cultural and linguistic characteristics of the service area. 4. Language assistance services must be offered and provided, including bilingual staff and interpreter services, at no cost to each patient/consumer with limited English proficiency at all points of contact, in a timely manner, during all hours of operation. 5. Patients/consumers must be provided verbal and written notices about their right to receive language assistance services; these notices must be in their language of preference. 6. Language assistance provided to Limited English Proficient (known as “LEP”) patients must be provided by competent interpreters and bilingual staff. Family and friends should not be used for interpretation services. 7. Easily understood patient-related materials and signage must be made available/posted in languages of the commonly encountered groups represented in the service area. 8. A written strategic plan should be developed, implemented and promoted, outlining clear goals, policies, 38 operational plans, and management accountability/ oversight mechanisms to provide culturally and linguistically appropriate services. Regulations and Standards for Cultural and Linguistic Services 12. Participatory and collaborative relationships with communities should be established and a variety of formal and informal mechanisms should be used to facilitate community and patient/consumer involvement in designing and implementing CLAS-related activities. 13. Conflict and grievance resolution processes must be culturally and linguistically sensitive, and capable of identifying, preventing and resolving cross-cultural conflicts or complaints by patients/consumers. 14. Information should be made public regularly regarding progress and successful innovations in implementing CLAS standards, and inform the public and the impacted communities about the availability of such information. Title VI of the Civil Rights Act of 1964 “No person in the United States shall, on the ground of race, color or national origin, be excluded from participation in, be denied the benefits of, or be subjected to discrimination under any program or activity receiving federal financial assistance.” Under Title VI, any agency, program, or activity that receives funding from the federal government may not discriminate on the basis of race, color or national origin. This is the oldest and most basic of the many federal and state laws requiring “meaningful access” to healthcare, and “equal care” for all patients. Other federal and state legislation protecting the right to “equal care” outline how this principle will be operationalized. State and Federal courts have been interpreting Title VI, and the legislation that it generated, ever since 1964. The nature and degree of enforcement of the equal access laws has varied from place to place and from time to time. Recently, however, both the Office of Civil Rights and the Office of Minority Health have become more active in interpreting and enforcing Title VI. Additionally, in August 2000, the U.S. Department of Health and Human Services Office of Civil Rights issued “Policy Guidance on the Prohibition Against National Origin Discrimination As it Affects Persons with Limited English Proficiency.” This policy established “national origin” as applying to limited English-speaking recipients of federally funded programs. Regulations and Standards for Cultural and Linguistic Services 39 Executive Order 13166, August 2000, Improving Access to Services for Persons With Limited English Proficiency (Verbatim) By the authority vested in me as President by the Constitution and the laws of the United States of America, and to improve access to federally conducted and federally assisted programs and activities for persons who, as a result of national origin, are limited in their English proficiency (LEP), it is hereby ordered as follows: sets forth the compliance standards that recipients must follow to ensure that the programs and activities they normally provide in English are accessible to LEP persons and thus do not discriminate on the basis of national origin in violation of title VI of the Civil Rights Act of 1964, as amended, and its implementing regulations. As described in the LEP Guidance, recipients must take reasonable steps to ensure meaningful access to their programs and activities by LEP persons. Sec. 2. Federally Conducted Programs and Activities. Section 1. Goals. The Federal Government provides and funds an array of services that can be made accessible to otherwise eligible persons who are not proficient in the English language. The Federal Government is committed to improving the accessibility of these services to eligible LEP persons, a goal that reinforces its equally important commitment to promoting programs and activities designed to help individuals learn English. To this end, each Federal agency shall examine the services it provides and develop and implement a system by which LEP persons can meaningfully access those services consistent with, and without unduly burdening, the fundamental mission of the agency. Each Federal agency shall also work to ensure that recipients of Federal financial assistance (recipients) provide meaningful access to their LEP applicants and beneficiaries. To assist the agencies with this endeavor, the Department of Justice has today issued a general guidance document (LEP Guidance), which 40 Regulations and Standards for Cultural and Linguistic Services Each Federal agency shall prepare a plan to improve access to its federally conducted programs and activities by eligible LEP persons. Each plan shall be consistent with the standards set forth in the LEP Guidance, and shall include the steps the agency will take to ensure that eligible LEP persons can meaningfully access the agency’s programs and activities. Agencies shall develop and begin to implement these plans within 120 days of the date of this order, and shall send copies of their plans to the Department of Justice, which shall serve as the central repository of the agencies’ plans. Sec. 3. Federally Assisted Programs and Activities. Each agency providing Federal financial assistance shall draft title VI guidance specifically tailored to its recipients that is consistent with the LEP Guidance issued by the Department of Justice. This agency-specific guidance shall detail how the general standards established in the LEP Guidance will be applied to the agency’s recipients. The agency-specific guidance shall take into account the types of services provided by the recipients, the individuals served by the recipients, and other factors set out in the LEP Guidance. Agencies that already have developed title VI guidance that the Department of Justice determines is consistent with the LEP Guidance shall examine their existing guidance, as well as their programs and activities, to determine if additional guidance is necessary to comply with this order. The Department of Justice shall consult with the agencies in creating their guidance and, within 120 days of the date of this order, each agency shall submit its specific guidance to the Department of Justice for review and approval. Following approval by the Department of Justice, each agency shall publish its guidance document in the Federal Register for public comment. Sec. 4. Consultations. In carrying out this order, agencies shall ensure that stakeholders, such as LEP persons and their representative organizations, recipients, and other appropriate individuals or entities, have an adequate opportunity to provide input. Agencies will evaluate the particular needs of the LEP persons they and their recipients serve and the burdens of compliance on the agency and its recipients. This input from stakeholders will assist the agencies in developing an approach to ensuring meaningful access by LEP persons that is practical and effective, fiscally responsible, responsive to the particular circumstances of each agency, and can be readily implemented. Sec. 5. Judicial Review. This order is intended only to improve the internal management of the executive branch and does not create any right or benefit, substantive or procedural, enforceable at law or equity by a party against the United States, its agencies, its officers or employees, or any person. WILLIAM J. CLINTON THE WHITE HOUSE Office of the Press Secretary (Aboard Air Force One) _________________________________________________ For Immediate Release August 11, 2000 Reference: http://www.usdoj.gov/crt/cor/Pubs/eolep.htm Regulations and Standards for Cultural and Linguistic Services 41 Resources for Cultural and Linguistic Services Cultural Competence Website Links to Other Organizations General Cultural Competence Resources for Cross-Cultural Health Care http://www.diversityrx.org DHHS Health Resources and Services Administration http://www.hrsa.gov/healthliteracy/ Culture, Health and Literacy: A Guide to Health Education for Adults with Limited Literacy Skills http://healthliteracy.worlded.org/docs/culture/ National Academies Press http://books.nap.edu/books/0309071542/html/index.html National Center For Cultural Competence, Georgetown University http://www11.georgetown.edu/research/gucchd/nccc/ National Council on Interpreting in Health Care http://www.ncihc.org Department of Justice – Office of Civil Rights http://www.justice.gov/crt/about/cor/13166.php The State of Literacy in America http://nces.ed.gov/naal/estimates/ Office of Minority Health http://minorityhealth.hhs.gov/ Office of Minority Health – “A Physician’s Practical Guide to Culturally Competent Care” https://cccm.thinkculturalhealth.hhs.gov/ DHHS Office of Civil Rights http://www.hhs.gov/ocr/ The Cross Cultural Health Care Program http://www.xculture.org/ The Plain Language Association International http://www.plainlanguagenetwork.org/ Kaiser Family Foundation Minority Health http://www.kff.org/minorityhealth/index.cfm Yale University Cultural Competence Resources http://www.med.yale.edu/library/education/culturalcomp Agency for Healthcare Research and Policy: “Providing Care To Diverse Populations” http://www.ahcpr.gov/news/ulp/ulpcultr.htm AMSA Diversity in Medicine http://www.amsa.org/AMSA/Homepage/About/Priorities/ Diversity.aspx Resources for Cultural and Linguistic Services 43 Cultural Competence Website Links to Other Organizations (continued) General Cultural Competence (continued) Institute of Medicine: Unequal Treatment http://www.iom.edu/Reports/2002/Unequal-TreatmentConfronting-Racial-and-Ethnic-Disparities-in-Health-Care.aspx Robert Woods Johnson Foundation: Aligning Forces for Quality http://www.rwjf.org/newsroom/product.jsp?id=30951 Wall Street Journal, June 5, 2008: Health Care Has Racial, State Disparities http://online.wsj.com/article/SB121263635211447647.html? mod=dist_smartbrief AskMe3 Brochures - Partnership for Clear Health Communication http://www.npsf.org/for-healthcare-professionals/ programs/ask-me-3/ Aging Center on an Aging Society http://ihcrp.georgetown.edu/agingsociety/ AARP Aging and Minorities http://www.aarp.org/politics-society/rights/info-1995/a_portrait_ of_older_minorities.html African American 44 National Association of Black Cardiologists http://www.abcardio.org/ National Black Nurses Association http://www.nbna.org/ Resources for Cultural and Linguistic Services American Indian/Alaskan Native Association of American Indian Physicians http://www.aaip.org/ Native American Cancer Research http://natamcancer.org/ National Indian Council on Aging http://www.nicoa.org National Indian Health Board http://www.nihb.org/ National Resource Center on Native American Aging http://ruralhealth.und.edu/projects/nrcnaa/ Asian American/Pacific Islander American Asian & Pacific Islander American Health Forum http://www.apiahf.org/ Chinese American Medical Society http://www.camsociety.org/ Office on Women's Health http://www.womenshealth.gov/minority-health/asian-americans/ National Asian Pacific Center on Aging http://www.napca.org/ Resources for Cultural and Linguistic Services 45 Cultural Competence Website Links to Other Organizations (continued) Hispanic/Latino American National Alliance for Hispanic Health http://www.hispanichealth.org/ National Council of La Raza http://www.nclr.org National Hispanic Council on Aging http://www.nhcoa.org National Hispanic Medical Association http://www.nhmamd.org Free Patient Health Education Materials – Low Literacy and Other Languages National Institutes of Health – Health Information in English/Spanish http://www.health.nih.gov National Network of Libraries of Medicine – Easy to Read Health Brochures in Other Languages http://nnlm.gov/outreach/consumer/multi.html Remember, web pages can expire often. If the web address provided does not work, use a search engine and search under the organization’s name. This information is intended for educational purposes only, and should not be interpreted as medical advice. Please consult your doctor for advice about changes that may affect your health. Linkage to the websites listed is for educational purposes only and is not intended as a particular endorsement of any organization. 46 Resources for Cultural and Linguistic Services Our Health Plan’s Cultural and Linguistic Resources Visit our new website at BridgingHealthCareGaps.com! If you have any questions or comments about this toolkit, please contact your provider representative. Sources Used in the Production of This Toolkit Bibliography of Major Hard-Copy Sources Used in the Production of the ICE Toolkit Aguirre-Molina, M., et al. Health Issues in the Latino Community. San Francisco: Jossey-Bass. 2001 Avery, C. “Native American Medicine: Traditional Healing.” JAMA 265 (1991): 2271-2273. Baer, H. Biomedicine and Alternative Healing Systems in America. Madison, WI: University of Wisconsin Press. 2001 Bonder, B., Martin, L., & Miracle, A. (n.d.). Culture in Clinical Care. Thorofare, NJ: SLACK, Inc. Carillo, J.A., Green., & J. Betancourt. “Cross–Cultural Primary Care: A patient-based approach.” Annals of Internal Medicine 130, (1999): 829-834. California Healthcare Interpreters Association & CHIA Standards and Certification Committee (Eds.). California Standards for Healthcare Interpreters: Ethical Principal, Protocols, and Guidance on Roles and Interventions. Oxnard, CA: The California Endowment. Cross, T., Dennis, KW., et al. Towards a Culturally Competent System of Care. Washington, DC: Georgetown University. 1989 Doak, C., et al. Teaching Patients with Low Literacy Skills. Philadelphia: J.B. Lippincott Co. 1996 Duran, D., et al. (Eds.). A Primer for Cultural Proficiency: Towards Quality Health Services for Hispanics. Washington D.C.: National Alliance for Hispanic Health. 2001 Fadiman, A. The Spirit Catches You and You Fall Down. New York: Farrar, Strauss & Giroux. 1997 Galanti, G. Caring for Patients from Different Cultures. Pennsylvania, PA: University of Pennsylvania Press. 1997 Goodman, A., et al. Nutritional Anthropology: Biocultural Perspectives on Food and Nutrition. Mountainview, CA: Mayfield Publishing Company. 2000 Hall, E.T. Hidden Differences: Studies in International Communication. Hamburg, Germany: Gruner & Jahr. 1985 Hall, E.T. Understanding Cultural Differences. Yarmouth, ME: Intercultural Press. 1990 Harwood, A. (Eds.). Ethnicity and Medical Care. Cambridge, MA: Harvard University Press. 1981 Kaiser Permanente National Diversity Council. (1999). Provider’s Handbook on Culturally Competent Care. Oakland, CA: Kaiser Permanente. Kleinman, A. Patients and Healers in the Context of Culture. Berkeley, CA: University of California Press. 1980 Kleinman, A. Illness Narratives. New York: Perseus Publishing. 1990 Kleinman, A., & Good, B. (Eds.). Culture and Depression. Berkeley, CA: University of California Press. 1985 Leslie, C., & Young, A. (Eds.). Paths to Asian Medical Knowledge. Berkeley, CA: University of California Press. 1992 Leigh, JW. Communicating for Cultural Competence. New York: Allyn and Bacon. 1998 Lipson, J., Dibble, S., et al. (Eds.). Culture and Nursing Care: A Pocket Guide. San Francisco: UCSF Nursing Press. 1996 O’Conner, B. Healing Traditions: Alternative Medicine and the Health Professions. Philadelphia: University of Pennsylvania Press. 1995 Office of Minority Health, Department of Health and Human Services. “Assuring cultural competence in health care: Recommendations for national standards and an outcomes-focused research agenda.” Federal Register Volume 65, 247. (2000): 80865-80879. Office of Minority Health, Department of Health and Human Services. National standards for culturally and linguistically appropriate services in health care: Final Report. 2001 Purnell, L.D., & Paulanka, B.J. Transcultural Health Care: A Culturally Competent Approach. Philadelphia, PA: F.A. Davis Company. 1998 Salimbene, S. What Language Does Your Patient Hurt In? A Practical Guide to Culturally Competent Care. Northampton, MA: Inter-Face International, Inc. 2000 Smedley, B., Stith, A., & Nelson, A. (Eds.). Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press. 2002 Spector, R. Cultural Diversity in Health and Illness: a Guide to Heritage Assessment and Health Traditions. Boston: Appleton & Lange. 1996 Spector, R. Cultural Diversity in Health and Illness. Upper Saddle, NJ: Prentice Hall Health. 2000 U.S. Code. “Title VI of the Civil Rights Act of 1964.” Title 42 - The Public Health and Welfare. 42 U.S.C. § 2000d et seq. 1964 Walzer, J. “The Health of Hispanic Elders: The Intersection of Nutrition Culture and Diabetes.” Tufts Nutrition. 2 May 2002 Please refer to the “Web Resources” pages of this toolkit to find the Internet resources that informed the work of the ICE Committee. Sources Used in the Production of This Toolkit 49 Bibliography of Major Internet Sources Used in the Production of the ICE Toolkit “A Practical Guide for Implementing the Recommended National Standards for Culturally and Linguistically Appropriate Services in Health Care.” Office of Minority Health. December 2001 <http://minorityhealth.hhs.gov/assets/pdf/checked/CLAS_a2z.pdf> “Culturally Competent Organizations. CLAS Standards.” Management Sciences for Health. 2003 <http://erc.msh.org/mainpage.cfm?file=9.4.htm&module=provider&language=Englis> “Culturally and Linguistically Appropriate Standards of Care.” As approved by the Boston HIV Health Services Planning Council on 11 January 2001 <http://www.bphc.org> “Healthy People 2010.” Blue Cross and Blue Shield of Florida. 2002 <http:// www.bcbsfl.com> “Information and Guidance for Recipients of Federal Funds on Language Access to Federally Assisted Programs and Activities.” Department of Justice, Civil Rights Division, Executive Order 13166. 2003 <http://www.lep.gov> Office of the Press Secretary, The White House. "Improving Access to Services for Persons with Limited English Proficiency. (Verbatim)." Department of Justice, Civil Rights Division, Executive Order 13166. 11 August 2000 <http://www.usdoj.gov/crt/cor/Pubs/eolep.htm> “Operational Policy Letter #: OPL 2001.133.” Department of Health and Human Services Centers for Medicare & Medicaid Services. 16 July 2001 <http://web.archive.org/web/20050308051355/http://www.cms.hhs.gov/healthplans/opl/opl133.pdf> “Oral, Linguistic, and Culturally Competent Services: Guides for Managed Care Plans.” Agency for Healthcare Research and Quality. Rockville, MD. 2003 <http://www.ahrq.gov/populations/cultcomp.htm> “The Medicare Advantage Organization National QAPI Project for 2003.” Centers for Medicare and Medicaid Services. 2004 <http://www.ahrq.gov/populations/oralling.htm> 50 Sources Used in the Production of This Toolkit