Reading 3 Determine risks associated with providing personal care
advertisement

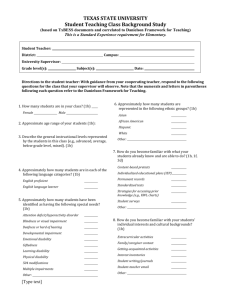
Determine risks associated with providing personal care support Contents Conduct environmental risk assessment for functions associated with personal care needs 3 Environmental risk assessment 4 Conduct risk assessment specific to client’s circumstances relevant to personal care needs 6 Skin 6 Infection control 7 Impaired judgement and problem-solving abilities 9 Discuss elements of risk with client (and carer) 13 Duty of care 14 Dignity of risk 14 Work with client (and carer) to identify strategies to remove or reduce risk 16 Develop strategies to remove or reduce risk according to organisation policy and procedures and legislative requirements 19 National Guidelines 19 State Guidelines 20 Local Guidelines 21 Prevention 21 Identify other risks to client and report accordingly 22 Assault, abuse and neglect 22 The role of services in creating or maintaining risk situations 24 Why should incidents be reported? 24 What incidents should be reported? 25 Reporting the incidents to the right person 25 How should incidents be reported? 25 Roles and responsibilities of services in keeping people safe 26 Responsibility of a service to ensure a safe environment 26 Roles and responsibilities 27 Adjust personal care support plan to include strategies to remove or reduce risk 28 Reasons for adjusting personal support plans 29 Conduct environmental risk assessment for functions associated with personal care needs Risks in our environment are part of life, and this is the case for the person with a disability or the older person as well. Risks which occur because of a disability or through the process of ageing can be physiological, psychological, emotional or environmental. Think of times when there has been an accident at your home, such as accidental burn to your hand from a hot iron or a hot water tap. Now imagine, for example, an elderly person with frail thin skin and how the burn could cause serious problems if they were less sensitive to pain or their eye sight had deteriorated. In this situation one of the strategies you could suggest is that the temperature of the hot water system be lowered to reduce the risk of serious burns. This is an example of how important it is to assess situations of risk and/or potential risk for the older person. If you find that your client has left the stove on, is drying their clothes too close to the heater, or is handling electrical equipment in a way that may put them to risk, you need first to bring it to their attention to make them aware of the potential risk. Then, if you find that you need to highlight your concerns again to the person, it may be a sign that the person is becoming forgetful and is placing themselves at risk more often. When this happens and the situation of risk and/or potential risk is likely to escalate, it is important that you report the situation to your supervisor immediately. If the person is living at home, some of the potential risks that could occur include: faulty wiring in the toaster, electrical heater, electrical blankets, etc clothes too close to the heater electrical equipment near the bath getting up at night to go to the toilet with inadequate lighting slippery floors, loose mats, floors too highly polished food and milk past the use by date food not reheated correctly loose or no hand rails in bathroom and toilet old medications steps without rails cockroach or mice infestations. A client risk profile looks at a range of areas of risk associated with: health conditions recreation activities community access activities challenging behaviour mobility and manual handling roads and safety in the community. Environmental risk assessment Environmental risk assessments allows for risks that might arise in daily activities to be identified and plans to be formulated to minimise these risks to allow the client to continue to participate in these activities. For example, maintaining skin integrity is an important consideration when undertaking functions associated with personal care needs particularly of the elderly who have a greater susceptibility to shearing-type injuries such as bruises, skin tears, rashes, excoriations and pressure areas than others. Frequent washing causes dry skin, which can lead to skin irritation and break down. Skin tears are painful and could cause major damage if not looked after appropriately. This places an elderly person at risk. In general, fragile skin, advanced age, use of assistive devices, cognitive/sensory impairment, and history of previous skin tears can put a client at risk of a skin tear. Research has shown that dependent residents who require total care for all activities of daily living are at greatest risk. Their injuries tend to result from such routine activities as dressing, bathing, positioning, and transferring. Should an issue arise regarding risk for functions associated with personal care needs, you with support from your supervisor should undertake an environmental risk assessment regarding the specific risks associated with a particular activity. This way the person is given support to engage in the experience that they have identified is beneficial and important to them rather than making a determination that they cannot do it. A specific environment risk assessment would then need to be developed and should be included as part of the person’s care plan. Table 1 is an example of such an individual environmental risk assessment. Table 1: Sample of an individualised environment risk assessment form for John Wright Specific Task/Activity Potential Hazards /Consequences Control Measures Transferring John from his wheelchair to a vehicle Manual handling causing injury to John Manual handling resulting in strain or back injury to worker Workers to use appropriate transfer aids provided (transfer belts, swivel seats in cars) Training to be provided on safe transfer techniques and methods Helping John in or out of the shower or bath Manual handling causing injury to John Manual handling resulting in strain or back injury to worker Rails to be attached to the wall for John to hold onto for extra support Non-slip mats to be placed on the floor inside and outside the shower or bath Bath seat placed across a bath to allow John access, usually used in conjunction with a hand held shower hose Use of shower chair [usually plastic with a hole in the middle so that water can escape]; specifically shower chair fitted with wheels which will allow John to be transported to and from the shower Use of commode chair [Commode chairs have a seat designed as a toilet seat. The chair is pushed over the toilet for use, these can also be used as shower chairs] All workers to gain an understanding of John’s level of independence Shaving Cuts and bleeding Encourage John to use an electric razor Physically assist John in shaving Use external professionals such as a barber Conduct risk assessment specific to client’s circumstances relevant to personal care needs Risks are a part of life. A risk describes a situation or potential situation of hazard to the person. The law does not expect you to provide absolute protection against all possible injury of the people to whom you owe a duty of care. It simply expects you to do whatever would be considered reasonable in the circumstances. Working out what is reasonable ultimately involves thinking through all the issues. Because care workers do not always work under direct supervision, they are often in a position where they need to make decisions around seeking help. Your organisation will want you, as a member of a team, to assist your client in maintaining an independent, healthy and productive life. The level of dependence varies according to the person’s disability, their personality, family situation, age and their state of health. For example, a person with a dual diagnosis, that is, an intellectual disability and a mental health issue, may have their judgement affected and therefore their ability to manage potential risk could be affected. Any goals decided through the care planning process should be assessed for potential risk. This could include skin integrity and cross-infections, as well as impaired judgement and problem solving abilities. These issues will need to be assessed and strategies devised so the person can participate in strategies that will help them reach their goals. We will now look at each of these risk areas and the strategies that can be put into place deal with the issues. Skin Part of daily activities includes ensuring good skin care. This care involves assessing the skin’s condition, maintaining the cleanliness of the skin and also protecting it from injury. People with a disability or who are aging are at a higher risk of skin injuries, often due to immobility and/or incontinence, so a thorough assessment as well as good skin care is vital. For the skin to remain healthy it requires adequate hydration, nutrition and circulation. Changes in client’s physical condition may be seen in changes to the skin, which is why it is important to assess client’s skin condition Assessing the skin As a care worker you will be the person most likely to notice any changes in your client’s skin condition. If you notice any change you must notify your supervisor and document it. So what are we going to assess? Changes in colour Redness could indicate several potential problems such as in infection, an injury or prolonged pressure (sitting or lying in a position for too long). Yellow colour (jaundice) could indicate problems with the liver. Blue/grey colour (cyanosis) could indicate a problem with circulation and this could be serious. Pale/white colour could indicate problems with the circulation; the client may be anaemic or unwell. Changes in hydration Excessive dryness may indicate dehydration. Notable fluid retention (swelling) may indicate circulation problems. Excessive moisture and or sweating could indicate the client has a temperature, is retaining fluid, or is wearing too many clothes. Changes in general skin condition Changes may include: skin tears/wounds rashes bruising. Remember any changes in skin condition must be documented and reported. Infection control Care workers in residential care settings who have direct contact with infectious people and/or bodily secretions are at increased risk of disease and infection. Therefore, cleanliness and hygiene are very important to prevent the risk of disease and infection spreading to employees, clients and others. Check that your organisation has polices and procedures in place, otherwise confer with you supervisor. Sources of infection Examples of reservoirs for germs in the residential setting can include: bodily fluids such as: – – – – – – – blood semen urine vaginal secretions faeces wound drainage sweat food and beverages which have been contaminated clients or staff who are carriers of an infectious disease, for example hepatitis B clients, staff or visitors to the facility who have an infection, for example the flu pets infested with parasites contaminated water in air conditioners or shower heads contaminated equipment, for example shower chairs not cleaned after use. Cross-infection Cross-infection is the spreading of infection from a client or staff member to others. Here are some examples of causes of cross-infection: not washing hands staff’s contaminated clothing sharing of personal items—combs, soap, toothbrushes etc poor cleaning of equipment—shower chairs, manual handling devices etc wearing rings and jewellery while working (germs are not easily removed even when hands are washed) shaking bed linen not keeping clean linen separate from soiled linen. Strategies to prevent cross-infection Precautions are in place at all times regardless of whether clients are known to have an infection or not. The precautions aim to reduce the likelihood of cross-infection (spreading infections from one person to another). Standard precautions apply to: blood all body substances, secretions and excretions except sweat, regardless of whether or not they contain visible blood cuts on the skin mucous membranes (the mouth, eyes). Standard precautions apply to all clients and residents receiving care in health care facilities, regardless of their diagnosis or presumed infection status. Standard precautions are: hand washing and hand care protective barriers—gloves, masks, gowns, eye shields correct sharps disposal (needles etc) correct disposal of contaminated waste (into appropriate bins) correct cleaning of equipment (sterilisation or disinfection). Personal protective equipment (PPE) Employers are required to provide personal protective equipment and clothing (PPE) when hazards in the workplace cannot be eliminated. Personal protective equipment and clothing include gloves, respirators, aprons, overalls, safety boots, safety glasses, goggles and ear muffs as appropriate. Employees should be instructed and trained in the correct use of any PPE provided by the employer. Impaired judgement and problem-solving abilities Confusion is not unusual at any age. Sometimes a client becomes confused, and does not recognise or react to situations that require attention. They could also become abusive towards you if they misinterpret your helping them with an activity. If while assisting the client you notice that their behaviour becomes challenging, it is important to be curious about why the behaviour is happening. Warning signals of potential risk Warning signs that can signal potential risk include the following. The client: shows a lack of interest in what he/she is wearing wears same clothes every day stops attending social functions without any clear reason struggles to deal with usual tasks experiences an increased difficulty in taking on new tasks needs more input from you than usual. Confused states can be caused by many factors. The confusion may be occurring because of a medical condition which may or may not be related to their disability. However, it is important to understand that confusion can also be a result of a poor diet, a situation that is causing stress to the person, depression, chronic pain, long-term alcohol consumption, Parkinson’s disease, tumours, chronic constipation or urinary tract infections. The parameters of your responsibilities As a care worker, you may not need to assume complete responsibilities for some tasks, such as full risk assessments or risk management, especially if there are more experienced workers on your team. In a residential facility, there will usually be a supervisor or senior worker at hand. However, if you are working in a HACC service (such as Home Care or Neighbour Aid) there may be times when you need to make an assessment and commit yourself to action without a supervisor’s direction. In both cases it is important to be observant, objective and to communicate well. You will also need to have a good understanding of the types of risks that arise for older people and people with a disability. You may need to be making suggestions to the supervisor based on what you have observed and what you have discussed with the client involved. Case study 1 Penny notices that Stan, who is usually quietly spoken with a peaceful manner, is becoming irritable towards other residents, particularly two women. Penny quietly asks him if anything is upsetting him, and mentions that she has noticed that when the two women are around he seems agitated. He becomes agitated and tells Penny to mind her own business. She mentions this to her supervisor, and notes it in the resident’s notes. Stan Penny is in a position to be able to consult with a supervisor. This may be an interpersonal conflict, or may be a change in behaviour for physiological reasons. She has flagged the change in behaviour, and other team members will be able to monitor it also. At times clients may not wish to take action to reduce risks to them. The worker needs to decide what action to take. This decision will be informed by a quick risk assessment: Are the consequences severe? Are the consequences likely? Does the risk outweigh the person’s dignity of choice? Case study 2 When Paul, a care worker, visits Barbara, he finds her confused and shaky. She can only intermittently remember who he is. She stumbles as she walks. Paul rings his supervisor to ask her to contact the family. His supervisor is out, but a co-worker checks the file and advises him that Barbara’s contact, her son, is away at present. Barbara starts crying and telling him not to get involved, and to leave. However, Paul and his colleague agree that given the severity of her symptoms, he should ring an ambulance. Barbara Paul has over-ridden Barbara’s wishes, because he has judged that he cannot leave her alone in the condition she is in. He feels uncomfortable about Barbara’s anger, but his supervisor assures him later that he had acted appropriately. Barbara’s son is also grateful that his mother, who had had a stroke, obtained medical treatment as quickly as she did. If Penny (in Case study 1), who is working in a residential facility, had come across a resident with the same symptoms, the limits of her responsibilities would probably be different, simply because there is a registered nurse at hand to assess and make the decision about what care is needed. There may also be times when the client will not want you to talk to your supervisor or for you to report what you observe. This may be because they fear being seen as silly or because they are worried about further loss of independence. Sometimes you may assess the issue is such that you can comply with their wishes. However, you will often need to use the communication skills that you have developed to encourage the client to allow you to be their advocate. To be sure of the parameters (borders, limitations) of your particular role, you will need to discuss it with your supervisor. Different organisations will have different expectations. If at any time you are unsure—check! Discuss elements of risk with client (and carer) A risk (situation of hazard) or potential risk can pose an immediate threat or danger to people and cause harm without the person even realising the situation. This is when you, the care worker, can assist the person to identify, respond to, and implement strategies to minimise or even eradicate the risk. Life is full of risks and risks are part of life. When we think of risks, we often think of environmental or physical risks such as skin tears from frail, thin skin; falls from an electrical cord lying on the floor or ill fitting shoes; or burns from a very hot shower. However, risks can also include many other aspects of the person’s life such as unusual behaviours, breach of confidentiality, lack of privacy, decline of socialising, boredom, risks to mental health and well being, abuse, and so forth. These risks are grouped into physiological, psychological, emotional or environmental. At risk behaviours can include confusion, depression, agitation, aggression, and memory loss. The care worker is in a favourable position to help detect risks and potential risks since it is part of the carer’s job role to continuously observe the person. This means watching out for the person’s health and safety even though the carer is not necessarily in a position to always prevent or fully eradicate the risks. It is important as you detect danger or potential danger that the person is consulted and the relevant issues are worked through in a calm and commonsense way. Sometimes it is just a matter of speaking with the person in an empathetic and non-judgemental manner, preferably face to face and providing them with enough information to respond to the risk appropriately. It is essential to observe the person and listen to them while being respectful of individual differences. Be sure to remember the following tips when communicating with your client: be on the same level as your client be aware of personal space and face the client use eye contact in a culturally appropriately way maintain an open, relaxed body posture do not rush the client use active-listening skills. Often you will find that the client wishes to discuss matters with family, and this may mean that you will be required to link the family with the client. Of course this will only happen with the client’s permission. Involving the family on a regular basis with the client’s day-to-day matters, such as social, recreational, religious and basic decision making can be highly beneficial for the client. To maintain empowerment and independence, it is the client’s choice how much the family is involved in their life and in which aspects. Providing vital information and encouraging discussion empowers clients to make their own decisions and this in turn allows them to maintain their dignity and independence. If, on the other hand, the care worker makes the decisions and responds to risks on behalf of the client without consultation, the client will then be at risk of becoming dependent on others. Clients have a right to have clear information about all the possible benefits and risks in maintaining their care. They should be told of the advantages and any dangers associated with their chosen activities. They should also be told about how the program they will enter into might change their behaviour or their relationships with others. Finally, they should be told how medication treatments and changes may make them feel and any side-effects they may have. Whenever the person needs to make a decision, a clear explanation of choices should be given in a way that they understand. When working with people who are unable to make informed choices you may need to use a key stakeholder. The law recognises that this may be necessary for some people so this is where the Guardianship Board may be contacted so a formal and legal process can be followed. Duty of care Duty of care means that you as a care worker have a duty to prevent any foreseeable harm to any clients or anyone else. People with a disability and older people are often vulnerable and it is important that all reasonable care is taken to ensure that the service offered does not harm or damage that person in any way. This also covers significant others who are also accessing the service provider. There might not be a specific organisational policy on duty of care, but it is a legal requirement. All organisational policies and procedures must be read with duty of care in mind. Dignity of risk Associated with duty of care is the concept of dignity of risk. Dignity of risk refers to a person’s right to experience all that life has to offer, such as learning a new skill or taking part in an activity that may entail some element of risk but that has benefits that might include gaining greater self-esteem and independence. Most people with a disability wish to lead a life which is as close as possible to that of people who do not have a disability and this inevitably involves taking some risks. Courts and the law of negligence do not, therefore, expect workers to shield their clients from all possible risks. They do, however, expect workers to take reasonable care (to be sensible and cautious) in their work. The Intellectual Disability Rights Service (IDRS) for example, encourages workers to weigh the benefits with the risks of any activity when assessing whether or not a person in your care may be harmed as a result of your actions or inactions. The IDRS have developed a ‘duty of care checklist’ in their book Questions of Rights which advises the worker to: 1. Assess the foreseeable harm and to see how likely it will be to occur and, if it does occur, to what extent. 2. Assess the likely benefits that the person might gain from the activity and the extent of these benefits. 3. Look for ways to reduce the risk of harm without losing the benefits of the activity. 4. Weigh up the foreseeable harm against the benefit. Work with client (and carer) to identify strategies to remove or reduce risk To maintain the client’s dignity, it is important that the process be a consultative one involving them and others (if appropriate) with the goal of maintaining their rights and needs. This process may be difficult and feel like a balancing act. However, current legislation and common sense will inform you that it is not necessary to go overboard in adjustments to a person’s lifestyle. It is important to let the person confront risks safely, and to take into account their personality. For example, they may have been natural risk takers in their life. A consultative approach means that after identifying a risk, you discuss your concerns with the client, supporting them in their decision wherever possible. It is beneficial to discuss with the client what they would like to do independently and what they may need assistance with. This respectful attitude helps to confirm for the client that you support their rights and independence. Remember, only a small change to how the client performs a task may be necessary. Clients have the right to make decisions that may include the acceptance of personal risk. Often workers can think that risk management means risk elimination. Care workers have a responsibility to ensure that safety hazards and situations of risk are minimised for clients, but it is not possible to protect them from all potential hazards. It is important that you understand the difference between the client’s rights to live with risk and staff neglect. It is important that you carefully consider all of the implications when considering preventing clients from fulfilling personal preferences or independence because of possible risk situations. The freedom that an individual is given should be balanced with stability and security. Whilst allowing clients to maintain their independence and fulfil personal preferences, it is essential that their own safety and the safety of others are taken into consideration. The perfect example to illustrate this is that of smoking. A client who lives in a residential care facility will have the right to smoke. However, they will only have the right to smoke in designated areas. This means they may not be allowed to smoke in public areas, their bedroom or in their bed. This rule will have been introduced in order to protect the safety of all residents and all staff rather than to limit the freedom of the individual. It is not always easy to respect the person’s needs and personal preferences while trying to ensure that they are safe. Case study 3 John is a home care worker. He has a client, Fran, who is 93 years old and requires a range of assistance. On Tuesday he goes for his regular visit to Fran. She proudly shows him a new rug her sister has given her, which she has laid along the wooden floor of the hallway. John is immediately concerned about the rug as a slip and a trip risk. However, Fran is so excited about the gift, and he doesn’t want to deflate this excitement. John As he works, he thinks about the problem, and decides to discuss his concerns with Fran. After he has finished his tasks, he sits down in the lounge room with Fran and gently tells her what his concerns are. He explains that he wants her to be safe. She seems a bit discouraged and at first dismisses his concerns, but agrees to think about it. John notes what he has done in the file when he gets back to work, and discusses it with his supervisor. When John goes back to see Fran later in the week, she says she has found the perfect place for her sister’s gift. John helps Fran to move it to a corner of the lounge room which is rarely used, but where she can see it whilst watching television. John, like many of the workers in this type of scenario, has used his communication skills to collaborate with the older person in reducing the risks. Fran has been able to find a solution which is not perhaps perfectly safe, but is significantly safer than it was originally. When people are told to do something, they sometimes comply happily. However, it is equally likely that they may resent being told what to do, and may actively avoid doing what they have been ‘told’. If John had said, ‘Fran, you really need to move that rug, its too dangerous. How about I roll it up and put it away in a cupboard?’ Fran’s response could well have been to say, ‘Mind your own business, its my house not yours!’ All care workers need to be particularly aware of the fact that they are visitors in another person’s home and need to show the appropriate respect. Residential workers need to be aware of showing respect for the small remaining environment and personal space which remains to their residents. All clients need to be included in decisions about their safety as much as their leisure times, treatment etc. If they are part of the decision, they are more likely to be happy with it and support it. At times clients may not wish to take action to reduce risks to them. The worker needs to decide what action to take. This decision will be informed by a quick risk assessment: Are the consequences severe? Are the consequences likely? Does the risk outweigh the older person’s dignity of choice? The organisation that you work for should have policies and procedures in place on how to respond to situations of risk. It will depend on the type of risk and the client involved as to how they will do this. If a client is at risk of abuse of any kind, there are mandatory reporting mechanisms in place that you need to follow, but what if it is like one of the example answers above, where it is a little more vague? We don’t want to wrap our clients up in cotton wool and keep them protected from society (which goes against the whole philosophy of normalisation), but we don’t want them to come to harm either. Develop strategies to remove or reduce risk according to organisation policy and procedures and legislative requirements As with most things in the workplace these days, there are procedures and policies to follow that guide support staff in their jobs and help staff understand what their place of work expects of them. When we are assessing clients and getting to know them we need to ensure that we work within organisational procedures. There are many national, state, and local statutory bodies that regulate the format of records (eg health care records). You have a responsibility to be aware of what they are and their impact on your work practices. Your employer will have a procedures and policy manual for you to read and abide by. If you are unclear, ask for clarification. There are many guidelines regarding reporting. If you want to further research this, the following information and links may be useful. However, for the most part you simply need to be accurate in your reporting and follow your organisation’s instructions. National Guidelines The Aged Care Act 1997 The Resident Classification Scale (RCS) is one of the major changes that came about as a direct result of the Act. This scale is a funding tool that seeks to allocate funding fairly for residents in residential aged care facilities. The RCS in its current format applies twenty questions to determine the aged persons care needs. The twenty, care-related questions each have four ratings, A to D, representing the degree of care required from lowest to highest. The RCS covers the following elements of care: 1. 2. 3. 4. 5. 6. 7. Communication Mobility Meals and drinks Personal hygiene Toileting Bladder management Bowel management 8. Understanding and undertaking living activities 9. Problem wandering or intrusive behaviour 10. Verbally disruptive or noisy 11. Physically aggressive 12. Emotional dependence 13. Danger to self or others 14. Other behaviour 15. Social and human needs-care recipient 16. Social and human needs-families and friends 17. Medication 18. Technical and complex nursing procedures 19. Therapy 20. Other services. Each question is accompanied by explanatory notes. The RCS is completed against a clearly defined and documented plan of care based on assessment of the care needs of each resident. The care plan will then clearly state the services that have been set into place to fulfil the needs of the older person. Other national guidelines Australian Standard AS 2828 – 1999 Commonwealth Department of Health and Aged Care (1999) Documentation and Accountability Manual (online) Available at: www.health.gov.au/internet/main/publishing.nsf/Content/ageing-manuals-damindex.htm Commonwealth Department of Health and Aged Care (2001) Residential Care Manual (online) Available at: www.health.gov.au/internet/main/publishing.nsf/Content/ageing-manuals-rcm-rcmindx1.htm Commonwealth Disability Act (1986) Available at: www.hreoc.gov.au/disability_rights/Standards/standards.html State Guidelines NSW Disability Services Act (1993) Department of Ageing, Disability and Home Care (DADHC). Available at: www.dadhc.nsw.gov.au/NR/rdonlyres/898B1EC7-FFED-4F87-83F0E7C25D504C61/668/Standardsinaction_93582882.pdf OHS – Workcover. Available at: www.workcover.nsw.gov.au/Documents/safebusiness/pdf/CommunityServicesSafetyPack_4421.pdf Local Guidelines Area Health Documentation Hospital and Residential Aged Care Facilities specific Procedure and Policy Manuals Local Council policies Prevention You may now be wondering about what you can do to help prevent people from living and working in unsafe and abusive situations. You need to think about ways in which you can contribute to making sure that the rights of older people and people with a disability are not ignored. This can be empowering for both the people you are working with and for you as a care worker. Ensuring that people are in safe environments, free from abuse and neglect, may include any or all of these preventative strategies: improving the physical environments of the places where people live and work empowering people through education so that they can stand up for their rights advocating on behalf of people so their rights are upheld having clear policies and guidelines about how to support clients employing staff with appropriate training, or providing training to staff. Identify other risks to client and report accordingly Historically, people with a disability have been a disempowered group in our society. Many people were separated from society by being placed in institutions. This was allowed to happen because of the stereotyped ways in which people with a disability were seen. Some of these stereotypes remain in our society today. These views have meant that people with a disability have had different life experiences to people who don’t have a disability. It has meant that they have been vulnerable to abuse and neglect. Assault, abuse and neglect It is important for you to have some understanding of what we mean when we talk about assault, abuse and neglect. This is because many of the practices described here are illegal and are covered by the NSW Crimes Act 1900. Others are covered by further government legislation such as the NSW Disability Services Act 1993 and the NSW Anti Discrimination Act 1997. Physical assault Physical assault is any touching of another person that is harmful, offensive or unwanted. Examples include: hitting, slapping, pushing, burning physical restraint over- or under-medication. Sexual assault Sexual assault is when a person is subjected to sexual activities without their consent. Examples include: penetration of the vagina, anus or mouth by a penis, by any part of the offender’s body or any object manipulated by the offender sexual and/or genital fondling unwilling exposure to exhibitionism and/or masturbation suggestive behaviours, and comments that are inappropriate or make the person feel uncomfortable or intimidated exposure to pornography. Emotional abuse Emotional abuse is abuse that causes a person to feel fear, anxiety, loss of self-worth or rejection through threats and humiliation. Examples include: severe verbal abuse continual rejection physical or social isolation threats of abuse harassment frightening, dominating or bullying actions humiliation withholding of affection threats of institutionalisation. Neglect Neglect is a lack of reasonable care or attention; carelessness can also be considered as neglect. Examples include: failure to provide adequate support, food, shelter, clothing or hygienic living conditions failure to provide adequate information and education in the use of poisons, alcohol or drugs nutritional, medical or other physical needs being ignored or withheld depriving an individual of the basic human interactions required for the development of social behaviour. Victimisation Victimisation means singling someone out for unfair punishment or treatment. Examples include: verbal and physical harassment inciting others to abuse or harm. The role of services in creating or maintaining risk situations Services do not always operate in ways that ensure people with a disability are protected from risks. They may not even be providing a service in a way that ensures people’s physical safety. For example: Services continue to house victims with perpetrators of abuse. Services continue to use behaviour management practices that deny human rights (eg using ‘time out’). The places where people are living and working are sometimes unsafe because of lack of fire safety, poorly maintained buildings and lack of privacy in bathrooms and bedrooms. Staff may be recruited without any checks on criminal records. Services may not provide adequate training and supervision to support their staff. Complaints procedures may not be in place. People are not being provided with skills training in protective behaviours or education about their rights. Why should incidents be reported? By reporting concerns you have about a person because of their behaviour, you will be letting the service know that there may be issues to do with a person’s safety and wellbeing. As the person who works regularly with clients, you may have got to know them quite well. They will be relying on you to understand what they are trying to tell you. It is not up to you to investigate what is happening. Depending on the situation, this is the responsibility of managers, the police or the Department of Community Services. What incidents should be reported? Past Auditor-General’s reports into large residentials have been critical of the lack of better systems for reporting incidents. As a result, all services are working to ensure best practice reporting systems are in place. While each service may have a different approach, they will all involve ensuring that the following situations are always reported: a crime has been alleged, such as assault critical incidents have occurred, such as a person harming themselves or others, threatening people with harm or damaging property dangerous environments exist, such as trip hazards or faulty electricals medical or dental problems are observed complaints have been made, such as those relating to staff and service delivery changes in a person’s behaviour have been observed. Reporting the incidents to the right person Report all incidents to your manager who will then determine what should be done. This may include reporting to more senior management, the Board, the police, or the Department of Community Services Child Protection and Family Crisis Service if the person is under eighteen years. You may also need to inform other significant people such as the person’s family, guardian or advocate, or the occupational health and safety (OHS) officer who will report to the OHS committee. The Commonwealth Department of Family and Community Services have funded an Australian Disability Services Abuse and Neglect Hotline for reporting neglect and abuse of people with a disability using government-funded services. Abuse and neglect cases include psychological, physical, sexual, civil, legal and financial abuse and restraint and restrictive practices. Withholding of support and care that exposes an individual to harm is also included. How should incidents be reported? Each service should have its own procedures and generally these will include: ensuring the person is safe putting the incidents in writing as a way of keeping a record of what is happening for a person keeping management informed through written incident reports—these reports should be factual and timely timeframes for making sure that everything necessary is done feedback processes so people know what is being done. If a service does not have a written procedure for staff to follow, you can still follow the basic guidelines of putting concerns in writing and giving these to your manager. Services are required by the government to make sure these procedures are in place. If a service you’re working for has not done this yet, you could talk to management about getting it done. Just some of the common reports that disability staff has to complete are OHS hazard reports, grievance and complaint forms, accident and injury reports and critical incident reports. Roles and responsibilities of services in keeping people safe Services have, or at least should have, lots of policies. These include how they provide a service to their clients, the roles and responsibilities of workers and how the service is administered. However, some services still lack policies and procedures in important areas such as how to support people with challenging behaviours, staff training, and supervision and monitoring of staff practices. Standard 10: Protection of human rights and freedom from abuse of the Disability Service Standards relates to the protection of people’s rights. This standard clearly tells services what they should be doing. To read this standard in detail refer to page 10.0.1 of the Standards in Action Manual, (1998) by the Ageing and Disability Department (1998). The main responsibilities of the agency identified in the minimum and enhanced standards of Standard 10 state that the service should have: policies and procedures in relation to prevention procedures for reporting and responding staff training on reporting incidents and supporting people service user training on protective behaviours and accessing information. Responsibility of a service to ensure a safe environment The NSW Occupational Health and Safety Act 2000 has very clear requirements of services in relation to the safety of their staff and clients. These requirements include what they should do about fire safety, maintenance of property and reporting and acting on hazards. It is also a part of the duty of care of staff to ensure that any foreseeable danger or risk is dealt with. An example of a service’s responsibility to keep people safe is in relation to fire safety. You may remember hearing a few years ago about a hostel in Victoria which burnt down and in which several men with a disability died. These sorts of tragedies highlight the need for services to be well prepared if they are going to ensure people are safe. This accident highlights the necessity of: making sure the environment is safe having policies and procedures to ensure things are done in the best possible way providing training for everyone involved. Roles and responsibilities You have already learnt about your responsibility to report abuse, neglect and situations of risk. While this is very important, it is not the only responsibility you have. If a person you are supporting has been abused, you may need to think about their immediate safety, their medical needs and their emotional wellbeing. If the situation has happened more than once, plans will need to be made to stop it. Adjust personal care support plan to include strategies to remove or reduce risk An important part of the care plan is to regularly evaluate the strategies being used. When a regular evaluation is undertaken, an idea of how the client copes with the plan over a period of time is gained. If an evaluation is undertaken every six to eight weeks, we can adjust the personal care support plan in terms of what needs to be added or removed to give the client a satisfactory level of care. For example, does additional equipment need to be used so the person does not fall or is there too much clutter in the person’s bedroom which poses a risk whilst they are trying to dress? Reviewing existing assessments may indicate that the person no longer requires the support indicated in the care plan. For example, since receiving physiotherapy, a person is now able to stand independently in the shower and no longer requires assistance with washing themselves. It is important to review the goals to ensure they are achievable. For example, do you, the client and or carer want this person to be showering themselves independently? Is this an obtainable goal? Are you the best person to support the client to reach this goal? What strategies are to be implemented? Is the person progressing well? If not, why not? A care plan is a cycle in which the stages are repeated over time, as shown in the figure below: A care plan cycle Reasons for adjusting personal support plans After a medical assessment has been conducted, a care plan is developed in consultation with the client to meet their personal lifestyle needs. Goals are established, activities and services are organised and client progress is monitored. The types of adjustments that older people need to make to how they participate in activities will vary from person to person. The physical changes that occur to the body will affect the ability to participate in and complete daily activities. The person generally needs to rely more on existing supports, like family, friends and neighbours, and may eventually require the assistance of community services to help maintain their independence. Physical changes as people age Here are some examples of why a personal care support plan may require adjustments to remove or reduce risk: Mobility can be reduced due to changes to bones/skeleton. The discs in the spine become thinner, bone density decreases, a person may shrink in height. A person may develop a stoop over time as muscle contract more slowly. Cartilage is worn away; tendons are less elastic, there is restricted movement in joints. The impact on mobility means less endurance for sustained exercise and activity, combined with a loss of strength, moderate physical activity is needed. The person may need assistance with cooking, shopping, domestic duties, community services may need to be introduced into lifestyle, modification of home and specialised equipment may be needed. As we age and for some people with a disability, there is a progressive loss of skeletal muscle strength, shape and size. As we become less active, muscle mass is replaced by fat. The impact on the person is tiredness and decreased physical strength. Maintaining a regular exercise regime has been shown to increase muscle strength and decrease the body fat to muscle ratio. Changes to eyesight and hearing can dramatically impact on a person’s life especially in terms of communication. Effects can often be minimised with spectacles and hearing aids, and adjustments in conversations with other people, watching TV, listening tasks etc. Computers can aid people with visual impairment with writing tasks, talking books may help when reading becomes too difficult. Long-term memory remains in tact, intelligence is generally unchanged, but the impact will show with slight impairment to short-term memory, new learning may take longer as ability to focus and concentrate lessens, reaction time slows, body temperature is less regulated. This may lead to frustration and discouragement for the person, may also impact on driving ability. Blood flow reduces from thickening arteries, heart respond slower to increased demands for blood when reacting to stress or exercise. Lungs: less air moves through the lungs, therefore less oxygen gets into bloodstream. The impact is a slowing down of daily activities and modifying fitness and exercise regimes. Teeth need constant maintenance or will decay, destabilise, discolour, gums recede as we age. A person’s diet and nutrition may decline if the range of foods they can eat is limited. Muscle is replaced with fatty tissue, middle age spread appears around waist and trunk, and obesity may develop. Body shape tends to change with age, arms and legs become thinner, and chest seems to cave in. This could impact on the person’s mobility, they will be slower and their psychological wellbeing, self-image, motivation may be effected if they cannot lose weight as easily as before. Skin becomes thinner, fatty tissue thins, skin wrinkles and bruises more easily, good skin care is required, intensive moisturising will prevent drying and cracking, client may need assistance to apply moisturiser. Protect arms, legs from bruising and injury as the healing process takes longer. Common health issues as people age Illness and disease all have an impact on the physical health of people. There is huge variance in the level of impact from person to person and needs to be medically assessed before activities are developed and implemented for each person. The examples listed below are some of the more common health issues that effect people, but are by no means an exhaustive list. They include: Arthritis affects the joints and is a common illness in older people. It impacts dramatically on mobility and limits the range of activities, social and domestic duties, a person can participate in. Specialised equipment is useful. Stroke results from a thrombosis, embolism or haemorrhage when a blood clot or blockage forms in an artery in the brain. A stroke can impact on communication, speech, mobility, motivation, self and body image, limit the range and type of activities, can also lead to permanent disability. Recovery is slow. Specialised equipment is very useful for rehabilitation purposes. It is a preventable illness which is related to a healthy lifestyle. Cancer can occur at any age, there are many types and each has a different impact on the person’s life. Ranging from slight interference to a dramatic and severe disruption, sometimes resulting in death. Supporting an older person with cancer, is an important role for care workers by offering psychological support and physical comfort. Coronary heart disease is one of the most common causes of death in our society. It is primarily a lifestyle related disease and highly preventable. It occurs when the flow of blood to the heart is restricted. The heart struggles to pump blood, oxygen and nutrients around the body, due to a build up of fatty substances that contain cholesterol on the artery walls. If a blood clot forms a heart attack can occur, or the person can develop angina. The impact on the body is dramatic and the person needs to adjust their daily activities and change their lifestyle. Depression is a mental illness. It can result from being unable to cope with the changes that the ageing process brings—such as change in life roles, loneliness, losing contact with friends or family, loss of loved ones, less physical activity, giving up recreational pursuits, illness and disease, retirement from work, financial issues etc. Depression requires medical attention and can be helped with medication and support with counselling. It can have a negative impact on a person’s life in a number of ways, such as restless sleep, pessimistic attitude, loss of appetite and weight, neglecting of self-care, continual tiredness, feeling emotionally upset, anxious, or flattened response, mood swings, suicidal thoughts, becoming housebound. Dementia: there are different types of dementia, Alzheimer’s disease being the most common form. It affects a quarter of people over the age of eighty-five. Dementia has a dramatic impact on a person’s lifestyle, activities of daily living and health status. It usually progresses slowly. The person gradually loses their independence. Symptoms include: o short-term memory loss, impaired judgement in decision making o confusion, change in behaviour, impaired decision-making processes o losing interest in recreational pursuits, unable to cope with change o sleeping difficulties, wandering away from home. Over time a person will need an increased amount of care. The main carer will need support in the form of community and respite care services. In the longer-term, residential care may be required as the disease progresses. Diabetes is another common health problem. It results when the supply of insulin is insufficient for the body’s needs. Insulin stimulates the transit of glucose from the blood and is utilised as fuel. Muscles are deprived of fuel when there is insufficient insulin produced, then blood sugar builds up and is excreted into the urine, taking water with it, thus resulting in general dehydration. The impact of diabetes can be minimal in a person’s life. It can be well managed through changes to lifestyle, like weight reduction, good nutrition, medication. Diabetes needs medical assessment.