Stomach: Normal Structures and Developmental Abnormalities
advertisement

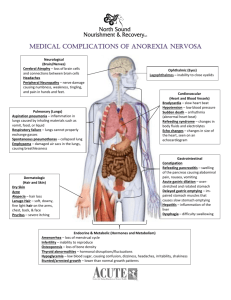
12 Stomach: Normal Structures and Developmental Abnormalities Chapter Outline EMBRYOLOGY Stomach Cardia Duodenum NORMAL STRUCTURE OF THE STOMACH Anatomy Gastric surfaces (relations of the stomach) Anatomic regions Blood vessels and lymphatics Nerve supply Histology EMBRYOLOGY Stomach The stomach appears at 14 weeks as a fusiform dilation of the caudal part of the foregut. The dorsal border grows faster than the ventral border, establishing the greater curvature of the stomach. As the stomach acquires its adult shape, it rotates 90 degrees in a clockwise direction on its longitudinal axis. The adult orientation of the stomach is established as the ventral border (lesser curvature) moves to the right, the dorsal border (greater curvature) moves to the left, the original left side becomes the ventral surface, and the original right side becomes the dorsal surface. These changes explain why the left vagus nerve supplies the anterior (ventral) wall of the adult stomach and the right vagus innervates the posterior (dorsal) wall (Fig. 12-1).1 The epithelial lining and gastric glands develop from foregut endoderm. Splanchnic mesoderm produces gastric smooth muscle, the lesser omentum, and the dorsal mesentery (dorsal mesogaster and greater omentum). Gastric epithelial cells express a range of peptide hormones known to regulate gastric functions including digestive enzymes, mucus, and hormones that regulate gastric motility. At 8 weeks, the developing human stomach has gastrin-containing cells in the antrum, and somatostatin cells in both the antrum and the fundus. At 10 weeks, glucagon-containing cells are seen the gastric fundus; these are preceded by glicentin ­(enteroglucagon—the precursor of glucagon) but have Mucosa Submucosa Muscularis propria, ICCs, and serosa DEVELOPMENTAL ABNORMALITIES OF THE STOMACH Pathogenesis and Clinical Features disappeared ­postnatally, although occasional glicentin or glucagon-containing cells can be found in various poly and cancers.2 Serotonin-containing cells are seen in the antrum and fundus by 11 weeks.3–6 Cardia There has been considerable controversy regarding whether the cardia is normal or is acquired in response to reflux.7,8 In embryos, there can be either a direct transition from oxyntic to esophageal squamous mucosa or a transition from oxyntic to cardiac to esophageal7,9 suggesting that cardia is physiological and may even develop in response to gastroesophageal reflux in utero. The issue assumes potential importance in adults, where a direct oxynto-squamous transition is rare, so that an argument can be made for the cardia being acquired in at least some adults. While this should be analogous to how much gastric metaplasia is present in the first part of the duodenum, which likely also develops in response to acid reaching that part of the duodenum, it assumes potential importance in the esophagus if it is acquired in response to gastroesophageal reflux disease. This could potentially be interpreted as acquired and therefore to have potential for neoplastic transformation—with or without goblet cells. It can therefore be argued that, unless this starts acquiring intestinal mucosa features, it likely has little risk.10 However, this is a moving target, as in some studies intestinal metaplasia can be present in over a third of the ­population if looked for.11 We therefore suspect that normal cardia has no increased risk of neoplasia. 552 Riddell_Chap12.indd 552 2/6/2014 12:40:56 PM Chapter 12 Stomach: Normal Structures and Developmental Abnormalities 553 that projects ventrally. The junction of the foregut and the midgut is at the apex of this embryonic duodenal loop usually immediately below the ampulla of Vater. Because of its derivation from both the foregut and the midgut, the duodenum is supplied by branches of the celiac and superior mesenteric arteries. During the 5th and 6th weeks, the duodenal lumen is reduced and may be obliterated by epithelial cells, but it recanalizes by the end of the embryonic period (8th week).1 Most of the duodenal ventral mesentery disappears, but the free border remains and forms the ventral border of the epiploic foramen. NORMAL STRUCTURE OF THE STOMACH Figure 12-1. The adult orientation of the stomach is established as the ventral border (lesser curvature) moves to the right, the dorsal border (greater curvature) moves to the left, the original left side becomes the ventral surface, and the original right side becomes the dorsal surface. Duodenum The duodenum develops from the most caudal part of the foregut and the most cranial part of the midgut. These parts grow rapidly and form a C-shaped loop The stomach is J-shaped, although there is considerable variation, depending on the degree of distention and the body habitus. Between its two areas of fixation at each end, the stomach is quite mobile. It is fixed above at the esophagogastric junction and below at the gastroduodenal junction. The two curvatures of the stomach are designated the lesser and greater curvatures (Fig. 12-2). Externally, the stomach is covered completely by peritoneum, except where the blood vessels run along its curvatures (Fig. 12-2), and a small bare area posterior to the cardiac orifice. The peritoneum is reflected at the lesser curvature forming the lesser omentum that extends to the liver. Likewise, the peritoneum is reflected at the greater curvature to become the greater omentum (a double layer of fatty peritoneum suspended from the greater Figure 12-2. Outline of the stomach with its rich blood supply from all three branches of the celiac trunk, namely the left gastric, splenic, and common hepatic arteries (a. = artery). Riddell_Chap12.indd 553 Chapter 12 Anatomy 2/6/2014 12:40:59 PM 554 Lewin, Weinstein, and Riddell’s Gastrointestinal Pathology and Its Clinical Implications curvature). The greater omentum is an apron-like structure hanging off the stomach that has a remarkable ability to stick to damaged or perforated parts of the gastrointestinal tract, sealing off leaks and giving some protection against peritonitis. Excess fat may be stored on the greater omentum, especially in men (hence beer belly).12 Gastric surfaces (relations of the stomach). The antero-superior surface of the stomach is in contact with the diaphragm (fundal region), gastric surface of the spleen, left and quadrate lobes of the liver, the anterior abdominal wall, and the transverse colon— when the stomach is empty. The postero-inferior ­surface (stomach bed) is formed by the posterior wall of the omental bursa and retroperitoneal structures between it and the posterior abdominal wall. Superiorly, the stomach bed includes part of the diaphragm (left crus), the spleen, the left suprarenal gland, and upper pole of the left kidney. Inferiorly, the stomach bed includes the body and tail of pancreas, transverse mesocolon, left colic flexure, the splenic artery, and, in some people, the transverse colon. Anatomic regions. Anatomically, the stomach is subdivided arbitrarily into four regions: the fundus, body (corpus), cardia, and antrum (Fig. 12-3). It connects with the esophagus and duodenum through the cardia and pyloric canal, respectively. The fundus (superior part of the stomach) is a dome-shaped area that lies above an imaginary horizontal plane passing through the cardiac orifice. The fundus extends to the left and superiorly from the cardia region. The body lies between the fundus and the antrum. It is the ­largest Figure 12-3. Areas of the stomach shown in this total gastrectomy specimen in a patient with an E-cadherin germline mutation but no gross abnormality. The pyloric sphincter is clearly identified on the left as a circular constriction. Riddell_Chap12.indd 554 part of the stomach and extends to the level of the incisura angularis on the lesser curve. Confusion can arise when fundus is used as a gross anatomic term including both the body and the fundus, and this use of the term should be avoided.13 The term “oxyntic mucosa” is a useful term to describe acid-producing mucosa. It is useful histologically when biopsies are clearly “oxyntic” but their precise site is unknown. The antrum occupies the lower one-quarter to onethird of the stomach. Its approximate boundaries can be defined by a line drawn from the incisura angularis to the opposite wall; its junction on the greater curve is determined by the approximate ends of the gastric rugae (Fig. 12-3). When the stomach is distended with air at endoscopy to permit visualization, the antrum is designated as beginning on the greater curvature at the point where the gastric body folds end and where the smooth, “foldless” antrum begins. The opening into the duodenum is the pyloric orifice, and its position is usually indicated by a circular groove on the surface of the organ, termed the pyloric constriction, which indicates the position of the pyloric sphincter. The pyloric sphincter is the most distal part of the antrum and controls the flow of gastric contents into the duodenum. The pyloric sphincter, similar to the lower esophageal sphincter, is several centimeters long (Fig. 12-3). Its narrow lumen, which passes between the antrum and the duodenum, is referred to as the pyloric canal. In endoscopic parlance, the term pylorus is commonly used interchangeably with pyloric canal and pyloric sphincter region. Some use the term pyloric antrum to designate the gastric antrum and pyloric canal to indicate the pyloric sphincter region. We prefer to avoid the prefix term pyloric in order to avoid confusion and to use the simpler terms antrum and pylorus. The cardia region refers to a short zone measuring from a few millimeters to several centimeters where the stomach immediately adjoins the esophagus. It is so named because of the mucus-secreting glands (cardiac glands) it contains. When the term cardia region is used in clinical or macroscopic terms, it usually denotes the most proximal (juxtaesophageal) stomach. The gastric cardia starts at the gastroesophageal junction where the squamous mucosa terminates (in patients in whom Barrett’s esophagus is not a consideration). There is no consensus on the endoscopic landmarks for the gastric cardia. Western gastroenterologists arbitrarily define the distal extent of the cardia as the level of the most proximal gastric folds (Fig. 12-4).14 Japanese gastroenterologists define the proximal extent of the EGJ as the distal end of the lower esophageal palisade vessels.15,16 These palisades are the termination of esophageal vessels that run longitudinally in the submucosal layer of the body of the esophagus, where their structure is truncal and consists of a few 2/6/2014 12:41:00 PM Chapter 12 Stomach: Normal Structures and Developmental Abnormalities Figure 12-4. Endoscopic image of the cardia region. In Western countries, the cardia begins distally at the proximal end of the gastric longitudinal folds in the partially deflated stomach (P). In Japan, the lower end of the cardia is determined by the lower limit of palisade vessels (L). While both of these definitions are almost the same, as can be seen here, the palisade vessels actually extend a little distal to the upper end of the gastric folds. The upper end of the cardia is the squamocolumnar junction or Z-line (Z). (Image courtesy of Dr. Worth Boyce.) large columns.16 At the cardia, the veins penetrate the muscularis mucosae and become s­ uperficial, forming the palisade vessels in the lamina propria beneath the epithelium. At the distal end of the palisade vessels, these veins merge with the submucosal venous network of the stomach. These two landmarks are similar but not always identical (Fig. 12-4). The squamocolumnar junction between the esophagus and the stomach is not an abrupt horizontal transition. Rather, there are grossly visible interdigitating tongues referred to as the ora serrata or, more commonly in endoscopic circles, as the Z-line (Fig. 12-4). As indicated subsequently in the section on histology, the histologic zones of the stomach do not ­correspond precisely to the gross anatomic regions. The mucosa in the body of the stomach, especially on the greater curvature, is thrown into numerous thick folds, or rugae, which run in a longitudinal direction. In the fundus, the lesser curvature of the body and, in the antrum, the mucosal folds commonly flatten when the stomach is distended with air or barium. With isotopically labeled meals, a midgastric transverse band can be identified in the food-filled stomach. There is no known anatomic correlate to explain its appearance.17 When the gastric body mucosa is viewed with a hand lens or close up at endoscopy, shallow slits or furrows, the areae gastricae, are seen. These represent the furrows between undulations of the mucosa that range up to 5 mm in diameter. Riddell_Chap12.indd 555 555 Blood vessels and lymphatics Arterial Supply The stomach has a rich blood supply from all three branches of the celiac axis (left gastric, splenic, and common hepatic arteries. The lesser curvature receives blood from two sources. The lesser curvature of the stomach is supplied by the right gastric artery (that arises from the hepatic branch of the celiac near the pylorus) inferiorly and the left gastric artery (that arises directly from the celiac artery) superiorly, which also supplies the cardiac region. The greater curvature receives blood from two sources. The greater curvature is supplied by the right gastroepiploic artery (that originates from the gastroduodenal branch of the hepatic artery) inferiorly and the left gastroepiploic artery (which arises from the splenic artery) superiorly. The fundus of the stomach is supplied by short gastric branches from the splenic artery. Venous Drainage The lesser curvature is drained by the right and left gastric veins, which run next to the arteries and drain into the portal vein. The fundus is supplied by short gastric veins that ultimately join the splenic vein, again finishing in the portal vein. Branches of the short gastric veins and the left coronary gastric vein at the cardia drain the lower esophagus. Blood from the lower portion of the greater curvature is drained by the right gastroepiploic vein, which enters the superior mesenteric vein and thence the portal vein. Lymphatics The lymphatic drainage from the stomach generally follows the main arteries and is named accordingly. Beginning in the gastric mucosa, the lymphatics pass through the gastric wall and go toward one or the other of the curvatures, draining to four main areas, along the routes of the arteries and veins. The largest is for most of the lesser curvature and the lower end of the esophagus, along the left gastric artery to the left gastric nodes. The distal portion of the lesser curvature in the region of the pylorus drains to the right gastric nodes that drain to the hepatic nodes. The proximal part of the greater curvature drains along the gastroepiploic and splenic vessels, terminating in splenic nodes in the hilum of the spleen. The distal portion of the greater curvature drains to the right gastroepiploic nodes in the greater omentum and to pyloric nodes at the head of the pancreas. Ultimately, the branches from all of these groups drain into the celiac nodes located around the celiac trunk as it arises from the abdominal aorta. From the celiac nodes, lymph drains directly into the thoracic duct. It is important to understand gastric lymphatic drainage as veins provide routes for spread of gastric cancer, when present, directly to the liver, while from the celiac nodes, the thoracic duct provides direct access to the systemic circulation. Chapter 12 2/6/2014 12:41:01 PM 556 Lewin, Weinstein, and Riddell’s Gastrointestinal Pathology and Its Clinical Implications Nerve supply. The parasympathetic nerve supply is from the vagus nerve and its branches. The right vagus nerve enters the abdomen as one or two trunks on the posterior side of the esophagogastric junction. It supplies branches to both surfaces of the stomach. The left vagus nerve also has one or two trunks, and it enters the abdomen on the anterior surface of the stomach, where it is present because of the rotation of the stomach early in its development (see “Embryology” section above). Shortly after entering the abdomen, the anterior vagal nerve gives off a hepatic branch and the posterior trunk gives off a celiac branch. Thus, transection of these trunks below these branches only results in gastric denervation. Even more selective denervation of the fundic gland mucosa (highly selective vagotomy) can be achieved by preserving the terminal portions of the vagal nerves that supply the gastric antrum. Vagal nerve fibers connect with ganglion cells located between the circular and longitudinal fibers of the muscularis propria (Auerbach’s plexus) and with submucosal ganglion cells (Meissner’s plexus). From these plexi, postganglionic fibers innervate both glands and muscle. The sympathetic nerve supply to the stomach is from the celiac plexus via branches that follow the gastric and gastroepiploic arteries. There are also sympathetic branches from the right and left phrenic nerves. These nerves contain afferent pain fibers as well as motor fibers to the pyloric sphincter region. Vagal stimulation from ghrelin mediated pituitary stimulation produces release of ghrelin and orexin that stimulates gastric secretion prior to food ingestion, the former resulting in increased gastric acid secretion via acetyl choline, and the latter that also stimulates a craving for food. At the microscopic level, this esophagogastric transition zone frequently contains alternating islands of squamous and columnar epithelium. Similarly, in the pyloric sphincter region, there may be short segments containing a blend of gastric columnar and small intestinal columnar epithelial cells. The Superficial Zone (Surface and Pit Epithelium) The gastric mucosa is covered by tall (20–40 mm) columnar mucous cells that are invaginated to form the pits or foveolae. The surface epithelial cells are replaced every 4 to 6 days.21 The mucus in the surface epithelial cells occupies the luminal part of the cells (Fig. 12-5), occupying up to about 80% of the cell. Nuclei are regularly oriented and are normally located in the basal part of the cell, and no more than one-fifth of the distance toward the lumen; when reactive changes are present, the A Histology This section focuses on the light microscopic appearance of the stomach. Comprehensive reviews of the electron microscopic appearance are available.18–20 All parts of the stomach have the same basic structural layers (mucosa, submucosa, muscularis propria, subserosa, and serosa). Mucosa. Traditionally, but for no good reason that we are aware of, the term crypt (crypts of Lieberkuhn) is applied to the small and large intestine, but in the stomach, they are pits. We are willing to accept either terminology but will use “pit” as terms such as “pit pattern” are now generally accepted. Gastric pits are divided into three histologic zones: superficial zone (surface and pit epithelium); neck zone, which is the regenerative region of the stomach; and deep or glandular zone. While the surface and neck zone cells are uniform throughout the stomach, the underlying glands differ in structure and function by region, and the ­histologic zones of the stomach are classified according to these types of glands: cardiac, oxyntic, antral. Riddell_Chap12.indd 556 B Figure 12-5. A: In the gastric pits (P), superficial cells in the stomach are mucin-producing throughout the entire stomach. Each nucleus has an apical mucin vacuole that usually occupies well over 50% of the cell (red arrows). Occasional intraepithelial lymphocytes are also visible (blue arrows). Depending on the staining technique employed, the mucous cells maybe almost clear as in (A), or eosinophilic as in (B). 2/6/2014 12:41:03 PM 557 Chapter 12 Stomach: Normal Structures and Developmental Abnormalities Table 12-1 Endocrine Cells of the Stomach HORMONE SILVER STAIN CELL TYPE CORPUS ANTRUM AMINE PEPTIDE MARKER (ANTIBODY) MASSON–FONTANA OTHERS ECL 30% 0 Histamine Unknown Negative Positive EC 7% 10% Serotonin (5HT) Unknown Positive Positive D 22% 20% Somatostatin Negative Positive G 0 60% Gastrin Negative Positive D1, A/X 20% Unknown Ghrelin Synaptophysin, Chromogranin A, VMAT2, Histamine Synaptophysin, Chromogranin A ­serotonin Synaptophysin, Chromogranin A somatostatin MAb Synaptophysin, Chromogranin A Gastrin Chromogranin, Ghrelin Negative Positive mucin is reduced and the nuclei occupy correspondingly more of the cell (see Chapter 13). Mucous cells lining the gastric lumen secrete mucus as well as bicarbonate ions. The bases of these pits are in direct continuity with the underlying glands. The surface epithelial cells appear similar to each other in all gland zones except those in the cardia region, where they may be taller and narrower. Occasional intraepithelial lymphocytes are normally present. Sometimes, the surface configuration of the mucosa of the antral and cardiac gland mucosa has a villous configuration. This appearance is a normal variant and should not be confused with intestinal metaplasia of the stomach, because the epithelial cells are normal, not metaplastic. The entire superficial zone of the stomach including the superficial part of the mucous secreting glands are immunoreactive to MUC5, and the deeper parts with MUC6, a staining pattern also seen in antral mucosa, Table 12-1, and illustrated in Chapter 14. These cells are strongly diastase PAS positive but do not stain with Alcian blue except in the cardia. Cardiac Gland Mucosa The gastric cardia has branched tubular glands that are primarily mucoustype glands, oxyntic-type glands, or both.22,23 Those that are mucous but clearly have residual specialized elements are called cardio-oxyntic. Unlike the antrum, in which the deep glands are diffuse, in the cardia, they often are compartmentalized, akin to lobules, which in normal stomachs allow ease of identification at low power. Mucus-secreting glands are similar in appearance on conventional stains to those of the gastric antrum and Brunner’s glands, except for the compartmentalization and lack of overt endocrine cells so readily seen in the gastric antrum (Fig. 12-7). In contrast to antral glands, portions of the cardiac glands may contain sialomucins that stain with Alcian blue at pH 2.5. Parietal cells are commonly ­scattered within the cardiac glands, although endocrine and chef cells are rare. Mucous cell–lined cysts are a frequent ­finding Chapter 12 Modified from Sachs G, Zeng N, Prinz C. Physiology of isolated gastric endocrine cells. Annu Rev Physiol. 1997;59:243–256; and Rindi G, Leiter AB, Kopin AS, et al. The “normal” endocrine cell of the gut: changing concepts and new evidences. Ann N Y Acad Sci. 2004;1014:1–12. The Neck Zone (Middle Zone) The neck zone (middle zone) has mucous cells as well as immature stem cells. This is the generative zone for the stomach, and all cells above and below are derived from this region. Mitotic figures are surprisingly sparse, although stains for Ki-67 show virtually all of the cells to be in the proliferative phase (Fig. 12-6). The immature stem cells migrate upward to renew the surface epithelium or downward to form the differentiated cells of the glands. These cells are also PAS positive. The Deep (Glandular) Zone Glands are found in the deep zone. In contrast to surface mucous cell that is continuous over the entire stomach surface, regional differences are mainly in the composition of gastric tubular glands within each compartment. Riddell_Chap12.indd 557 Figure 12-6. Mucous neck region stained with Mib-1 to show the marked proliferation of this region. The paradox is how inconspicuous mitotic figures are in this region. 2/6/2014 12:41:04 PM 558 Lewin, Weinstein, and Riddell’s Gastrointestinal Pathology and Its Clinical Implications Figure 12-9. Transitional mucosa (mutilayered epithelium) that is sometimes seen in the cardiac region. The most superficial cells are mucous secreting, but beneath that, the cells and their nuclei are stratified as seen in squamous mucosa of the esophagus. These are discussed further in Chapter 10. Figure 12-7. Cardiac gland mucosa. The glands in the bottom half of the section are a mix of mucous glands (cardiac glands) and fundic gland elements. Mucosal cysts, as seen here, are a common finding in cardiac gland mucosa. Note the vague lobularity that is very characteristic of cardia. Occasionally, ­pancreatic-type cells can be seen in these glands but appear to be without significance. (Fig. 12-7). The pits in the cardiac region are very shallow, occupying less than one-quarter of the overall mucosal thickness (Fig. 12-8)—ranging from 0.5 to 1.5 mm—and are immunoreactive with MUC6. There are at best rare endocrine cells in the gastric cardia—there are no data to suggest that they have physiologic or pathologic significance. Occasionally, pancreatic-type glands can be seen in the cardia in the form of exocrine cells that are ­immunoreactive with lipase or trypsin. They can be Figure 12-8. Cardiac glands with pancreatic-type cells (arrows). Riddell_Chap12.indd 558 admixed with simple mucous-producing cells or oxyntocardiac mucosa with parietal and mucous-producing glands. Chief cells appear to be rare in the cardia. Endocrine components admixed with heterotopic pancreas are vanishingly rare, and endocrine neoplasms even more so. Also, at the squamocolumnar junction, the so-called multilayered epithelium can be seen (Fig. 12-9), which seems to be associated with the development of Barrett’s esophagus. They are sometimes ciliated. They are discussed in more detail in Chapter 10. Oxyntic Mucosa (Fundic and Corpus Gland Mucosa) Oxyntic gland literally means acid producing so is a good name for normal corpus and fundic gland mucosa. Surprisingly, the thickness of the oxyntic mucosa varies. It is thickest in the greater curve, gradually thins as the antrum is approached, and is thinnest on the lesser curve (Fig. 12-10). In the oxyntic gastric corpus, pits have four major cell types (Fig. 12-11): chief cells responsible for pepsinogen production, which can be demonstrated using pepsinogen 1 (Fig. 12-11A), parietal (oxyntic) cells that secrete acid and the intrinsic factor necessary for vitamin B12 absorption and apart from antibodies to H+K+ ATPase can be demonstrated with PDGFRa (Fig. 12-11B), mucous neck cells, and a ­variety of endocrine cells (Fig. 12-11C,D). At the interface between the pits and the parietal cell zone, and scattered throughout it, are tiny (∼7 mm-wide) ­mucin-containing neck cells. They are not easily seen with conventionally stained sections, but they can be visualized with the use of the PAS (neutral mucin) stains and sometimes with Alcian blue pH 2.5. In addition, there are a ­scattering of mucous-­producing cells seen ­throughout 2/6/2014 12:41:07 PM Chapter 12 Stomach: Normal Structures and Developmental Abnormalities 559 Figure 12-10. Oxyntic mucosa varies in thickness depending on its location. vitamin B12, iron, and calcium. It also prevents bacterial overgrowth and reduces the chances of enteric infection. However, parietal cells also secrete intrinsic factor, transforming growth factor-alpha, amphiregulin, heparin-binding epidermal growth factor–like growth factor, and sonic hedgehog.25 The major stimulants of acid secretion are gastrin, histamine, and acetylcholine, along with ghrelin (centrally but also produced in the stomach) and orexin (produced ­centrally and stimulating a craving for food). Indeed, the weight loss following ­gastrectomy, ­especially proximal, is due to the loss of this stimulus to eat. The main inhibitor of acid secretion is somatostatin, along with nitric oxide and dopamine. Figure 12-11. Specialized cells of the oxyntic mucosa can be appreciated with (A) immunostains for pepsinogen 1, which stains chief cells and (B) platelet-derived growth factor receptor alpha (PDGFRa) that appears to outline the secretory apparatus (canliculi) of the parietal cells. In addition, (C) endocrine cells of the gastric body can be demonstrated with either argyrophylic stains, here surrounding chief cells at the base of the glands, or (D) overview of the numerous diffusely immunoreactive endocrine cells in the oxyntic mucosa, here stained with chromogranin A, which contrasts markedly with the band-like distribution consisting mainly of G cells, seen in the antrum. Riddell_Chap12.indd 559 Chapter 12 the specialized mucosa in a small proportion of patients, and they appear to be present and increase toward the distal end of the oxyntic mucosa. In the oxyntic mucosa, parietal cells predominate in the upper half of the glands, and chief cells dominate in the lower half Figure 12-12. The parietal cells have a round or pyramidal shape, an eosinophilic cytoplasm, and a centrally placed nucleus. The cytoplasm appears vacuolated or finely reticular, especially in the perinuclear area, because of the extensive secretory canaliculae. These can be demonstrated with electron microscopy,24 or as shown in Figure 12-12B. Parietal cells produce hydrogen ions as hydrochloric acid which facilitates the ­digestion of protein and absorption of 2/6/2014 12:41:10 PM 560 Lewin, Weinstein, and Riddell’s Gastrointestinal Pathology and Its Clinical Implications The chief cells contain zymogen granules that are basophilic, but the degree of basophilia can vary and can be quite faint, especially in transition zones. Chief cells have a large basal nucleus and a more cuboidal shape. They secrete pepsinogens I and II, and these products can be demonstrated immunocytochemically (Fig. 12-11A).26,27 However, in addition, chief cells also release pepsinogen, gastric lipase, and the protease chymosin (formerly known as ­ rennin—to be distinguished from renin), which commercially is used to produce cheese from milk. Chief cells release the zymogen pepsinogen when stimulated by a variety of factors including cholinergic activity from the vagus nerve and acidic condition in the stomach. Gastrin and secretin may also act as secretagogues. These cells have the same gastrin and CCK2 receptors found on parietal cells, enterochromaffin-like (ECL) cells, and D (somatostatin) cells suggesting similar control. The parietal and chief cell turnover rates have not been clearly defined because they are much slower. In rodents, the turnover for parietal cells has been estimated to be about 164 days.28 The key feature is that the specialized compartment in the stomach is renewed, but the turnover time is in months. Under stress, both parietal and chief cells appear to be able to undergo cell division, parietal cells with hypergastrinemia from, for example, PPIs, while chief cells may also be able to replicate. The endocrine cells of the fundic gland mucosa are distributed fairly diffusely throughout the ­oxyntic mucosa. The presence of endocrine cells is sometimes suggested by a degree of perinuclear clearing (halo), although far less than that seen in G-cells in the antrum, while the nuclei are far less hyperchromatic than the intraepithelial lymphocytes that may be ­present. ­ ndocrine cells can sometimes be identified on H&E E sections in the oxyntic mucosa as nuclei immediately above the basal lamina of the gland that are not in the middle of parietal cells and not clearly associated with chief cell granules (Fig. 12-6B). ­However, the nuclei need to be observed carefully, for, if very densely hyperchromatic, they could represent intraepithelial lymphocytes (demonstrable on CD3 immunostains). Antral Mucosa The antral glands are coiled branched tubular glands that appear diffusely located with no, or at best minimal, hint of the lobular compartmentalization seen in the cardia (Fig. 12-13B), unless atrophy is present. Glands are predominantly mucous, and while most are clear, in some patients, the mucous cells have distinctly eosinophilic granules that can be either very fine or almost as large as Paneth cell granules, which they can resemble. All (like Paneth cells) secrete lysozyme. Gastric cells can also upregulate specific defensins in response to Helicobacter infection, but it is so far unclear if these are produced by lysozyme-producing cells.29 Numerous endocrine cells are also present and are primarily gastrin-producing cells (G cells), sertonin-producing (EC) cells, and somatostatin-­ ­ producing cells (D cells) (Fig. 12-14). ­Endocrine cells appear more frequent in the antrum than in the corpus22 but are concentrated in a band (Fig. 12-12) rather than being diffusely dispersed (see Fig. 12-11D) and with a little practice are readily visible at scanning power on H&E sections (Fig. 12-13). They are easily seen at high power with virtually any stain (Fig. 12-14). Specific immunostaining for gastrin shows that the vast majority of these are G cells (Figs. 12-13 and 12-15). If there is any doubt about whether a specific biopsy is antral A Figure 12-12. Oxyntic mucosa. A: Sketch showing that most of the mucosa is composed of the glands with very shallow pits. Contrast this with the antral gland sketch in Figure 13-6A. (Courtesy of John Petrini, M.D.) B: Overview of oxyntic mucosa in which the pink parietal cells with their central nuclei (red arrow) predominate in the upper part of the glands and are readily distinguished from the more purple staining chief cells (dark blue arrow) with their nuclei against the edge of the gland. Probable ECL cells are insignificant but have a central nucleus and pale cytoplasm (light blue arrows) and occasional mucous-producing cells are also present (green arrow). Riddell_Chap12.indd 560 2/6/2014 12:41:13 PM Chapter 12 Stomach: Normal Structures and Developmental Abnormalities A 561 B Chapter 12 Figure 12-13. Antral gland mucosa. A: Sketch showing that the thickness of the mucosa is usually less than that of the fundic gland mucosa. The gastric pits occupy one-half or more of the mucosal thickness. (Courtesy of John Petrini, M.D.) B: Low-power histologic section in which the “fried egg” or “halo” (originally “waterclear” cells) are readily seen (arrowed). Figure 12-14. A: Antral mucosa with occasional endocrine “halo” cells scattered regularly down the sides of the midportion of each crypt. B–D: Immunostains for chromogranin A, which immunostains virtually all of the endocrine cells, and specific stains for gastrin (C) and serotonin (D), which make up about 2/3 and 1/3 of the cells, while somatostatin are about 5%. Riddell_Chap12.indd 561 2/6/2014 12:41:19 PM 562 Lewin, Weinstein, and Riddell’s Gastrointestinal Pathology and Its Clinical Implications Figure 12-15. Immunohistochemical stain for gastrin showing the band of G cells in the antrum, here accentuated as there is hyperplasia from long term PPIs. or not, additional immunostaining for pepsinogen 1, if available, help, as they stain oxyntic glands but are immunonegative in antral mucosa (Fig. 12-16). However, there is a transition zone between antrum and oxyntic mucosa; in this location, practically, the presence of gastrin cells puts the biopsy in the antrum. In chromogranin A stains staining (for some ­reason, this seems to detect G cells much more readily than synaptophysin, but this may vary from lab to lab), the band of G cells can be detected. Differences between these two endocrine cell stains are shown in Figure 12-17. However, in the transition zones, these become more diffuse and intermixed with oxyntic endocrine cells, so absolute distinction can be difficult. It also needs to be appreciated that the G-cell containing portion of the antrum is relatively distal in the “anatomical” antrum, the more proximal mucosa being more transitional as it acquires oxyntic characteristics. This becomes important as biopsies from histological antrum need to be taken quite distally—ideally from the prepyloric region, to guarantee getting the endocrine portion of the antrum. Whether this matters in looking at biopsies for Helicobacter has not been determined. Gastric endocrine cells are also discussed subsequently. Parietal cells can be quite conspicuous in the antrum and should not be taken as an indication that one is not in the antrum (Fig. 12-18); indeed, they often appear to increase in density toward the pylorus, rather than petering out as might be expected, but detection of the G-cells, even on H&E stains, is usually easy and confirms the location as being antrum. The density of parietal cells in the antrum decreases in the face of moderate to severe antral gland gastritis.30 Mucosal Transition Zones As indicated previously, all of the cardiac gland mucosa may contain scattered fundic gland elements, especially parietal cells. This mixed-gland phenomenon may be equally prominent in antral–fundic gland transition zones. The transition zone between fundic gland and antral gland mucosa does not usually follow the gross anatomic boundaries. It is not uncommon to find a mixed-gland mucosa extending 5 cm or more, especially along the lesser curvature. At endoscopy, biopsy specimens taken from what is considered to be the proximal third of the antrum may consist entirely of fundic gland mucosa, Figure 12-16. Typical immunophenotype of gastric antrum with no pepsinogen 1 immunoreactivity and strong gastrin immunoreactivity. Riddell_Chap12.indd 562 2/6/2014 12:41:21 PM Chapter 12 Stomach: Normal Structures and Developmental Abnormalities 563 which likely does matter if looking for Helicobacter in what is thought to be antral mucosa; these need to be taken more distally (we advise from the distal or prepyloric antrum). Furthermore, parietal cells are commonly found scattered throughout the antral gland mucosa down to the pylorus (Fig. 12-18).30 The presence of parietal cells in a biopsy does not therefore preclude an antral origin. Although chief cells may be found in the immediate transition zone between fundic gland and antral gland mucosae, they are usually absent in the more distal antrum. Gastric Mucins The gastric mucosa is covered by mucin-producing cells that play important roles in protecting gastrointestinal mucosa from a variety of physical, chemical, and microbial damage.31–33 Mucins are highly glycosylated glycoproteins and their core proteins (mucin core proteins: MUC).34 The expression A of these mucins and intestinal enzyme are cell-type specific; hence, they are useful phenotypic indicators of cell differentiation in normal, metaplastic, or neoplastic epithelial cells in the gastrointestinal tract.35–37 MUC5AC (sometimes just abbreviated to MUC5) is expressed in gastric surface mucous cells, MUC6 is expressed in gastric gland mucous cells (cardiac gland cells, mucous neck cells, and pyloric gland cells), and MUC2 is expressed in intestinal goblet cells,38–40 The histochemistry and immunohistochemistry of gastrointestinal mucins are discussed in Chapter 14. Histochemically, mucins of the surface and pit epithelium are predominantly of the neutral polysaccharide type and thus stain positively with the periodic acid–Schiff (PAS) stain.41 Much fainter staining with PAS is seen in parietal cells and in the mucous glands of the antral and cardiac gland regions. Acid, nonsulfated mucins (sialomucins) are absent from the Chapter 12 Figure 12-17. Comparative immunoreactivity of chromogranin A and synaptophysin in normal antrum and body. Synaptophysin seems to stain G cells preferentially, while in the oxyntic mucosa, they are much more similar, with perhaps chromogranin A getting the edge in numbers of endocrine cells stained. B Figure 12-18. Parietal cells in the antrum. A: At scanning power, numerous parietal cells are visible. B: Detail shows the parietal cells (red arrows) and endocrine cells (blue arrows), the latter confirming that this is antral mucosa. Riddell_Chap12.indd 563 2/6/2014 12:41:28 PM 564 Lewin, Weinstein, and Riddell’s Gastrointestinal Pathology and Its Clinical Implications surface epithelium but are present in small amounts in the deep pit regions and mucous neck cells. These can be highlighted by staining with Alcian blue at pH 2.5.41 Gastric Endocrine Cells Enteroendocrine cells (also defined as the diffuse endocrine system) are specialized endocrine cells of the gastrointestinal tract that produce hormones such as gastrin, histamine, ghrelin, serotonin, and somatostatin.42,43 The enteroendocrine cells are derived from the same stem cells as the rest of the epithelium and are not derived from the migratory neural crest source that provides the enteric nervous system.44 The enteroendocrine system of the gut is heterogeneous and is composed of as many as 14 highly specialized cells, some with unknown function.42,43 Table 12-2 lists gastric endocrine cells with known function. Most endocrine cells historically can be identified immunohistochemically or with silver stains, which were among the first methods to assess gastric ­endocrine cells. Endocrine cells in the antrum can be identified without special stains. The staining properties of endocrine cells displaying intrinsic silver ­reducing power either with or without ammonium ions being provided. Interaction of some of these cells with chromium salts (hence enterochromaffin [EC] cells) proved to be the same cells that could precipitate silver salts in the absence of ammonium ions (e.g., Masson–Fontana stain—argentaffin cells), while all other cells required the addition of ammonium ions for the silver to precipitate (e.g., Grimelius, or Sevier–Munger stains—argyrophil cells). (It will not have escaped some that the terms argyrophil and argentaffin have identical meanings, except that the first is of Greek derivation and the second of Latin.) The staining of endocrine cells requiring the ­ presence of added reducing agents (argyrophilia) resulted in the term enterochromaffin-like cells (ECL cells).43 Because silver stains tend to be capricious, numerous arghyrophil stains exist, and some were found to be more specific for certain cell types (e.g., Sevier–Munger for G cells). Silver impregnation techniques, although effective and reproducible, have now been largely replaced with immunohistochemistry (Table 12-1). In the antral mucosa, most endocrine cells are G cells, producing gastrin, while most of the remainder are D (somatostatin-producing) cells (see Table 12-1). In the oxyntic mucosa, ECL cells secrete histamine and directly stimulate acid secretion; they can specifically be demonstrated with antibodies to Human Vesicular Monoamine Transporter 2 (VMAT2). Ghrelin is a peptide hormone that has been localized to the oxyntic mucosa X/A-like (Gr) cells.45,46 X/A-like cells that resemble pancreatic A cell (glucagon-producing cells—hence the A part of the name) are the most abundant endocrine cells in the stomach after the Riddell_Chap12.indd 564 histamine-producing cells.46,47 Though ghrelin most widely known function is growth hormone release from the pituitary gland; it also plays a role in mediating immune and inflammatory processes.48 Ghrelin plays an important role in regulating appetite, feeding, and energy metabolism49 in addition to stimulating gastric motility.50 D cells are also the “turn-off” cell in the oxyntic mucosa. Acid Secretion Gastric acid secretion is regulated by a complex set of mechanisms acting at the central, peripheral, and cellular level. A detailed description of neural regulation (both central and peripheral) is beyond the scope of this chapter (interested readers should refer to 22,25). This section is a simplified view of acid secretion in the normal physiologic state, but is required to understand gastric pathophysiology. Though the capacity of the stomach to secrete acid is almost linearly related to parietal cell mass, the major endocrine cells known to play an important role in acid secretion are the ECL cell of the fundus, the gastrin (G) cell of the antrum, and the somatostatin (D) cells of the fundus and antrum. Physiologically, the thought of food enhances release of ghrelin that initiates acid secretion prior to food ingestion and orexin that stimulates a craving for food. Gastric distension and the presence of food in the stomach stimulate the release of gastrin from antral G cells. Gastrin diffuses into the circulation via an autocrine process to stimulate the parietal cell to produce gastric acid, both directly acting on parietal cells and indirectly by stimulating ECL cells to secrete histamine51 via the CCK2 receptors25 that are found on D cell, ECL cells, and parietal cells. Parietal cells specifically have the H2-histaimine receptor, which is why suppression of acid secretion with H2-receptor antagonists was key in acid suppressive therapy, especially prior to the PPI era. Histamine (and possibly gastrin directly) activates the parietal cell to secrete acid. Thus, in a normal physiologic state, acid secretion is directly related to histamine receptor stimulation by ECL cells. Histamine release from ECL cells is continuous in the presence of gastrin. As the acidity of the stomach and duodenum increases, further acid secretion is inhibited through the release of somatostatin by D cells.52–54 Somatostatin inhibits the secretion of gastrin and histamine and appears to have a direct inhibitory effect on the parietal cell.22 Figure 12-19 is a simplified diagram of mechanisms involved in gastric acid secretion. Lamina Propria The lamina propria is located between the pits and contains smooth muscle cells that have very eosinophilic, and sometimes wavy, ­cytoplasm and are 2/6/2014 12:41:28 PM Riddell_Chap12.indd 565 2/6/2014 12:41:28 PM Cephalad displacement of pancreatic bud during embryonic life Found in anencephalics Arrested phase of normal development; vascular factors; autosomal recessive Arrested Very rare development of foregut; familial; autosomal trait Embryonic epithelial Very rare account nodules that fail to for ~ 4% of regress gastrointestinal duplications; more common in females than in males As for duplications Very rare Pancreatic Heterotopias68,69 Microgastria74,75 Very rare Developmental defect in muscle Long gastric ligaments Muscle defect84,85 Volvulus86,87 Chapter 12 Very rare Very rare Very rare Rare 2% of population at autopsy Positional Defects83 Diverticula81,82 Duplications62,76–80 Atresia62,70–79 Aplasia62,70 Persistence of mild infantile form Adult67 CLINICAL FEATURES Gastric perforation more common in premature babies Vomiting Young patients; symptoms depend on location and size; most gastric emptying problems; upper abdominal mass; perforation; peritonitis As for duplications Depends on severity of lesion and age; infants: outlet obstruction, vomiting, gastric distention; older children and adults: peptic ulcer symptoms Feeding abnormalities Often asymptomatic; epigastric pain or outlet obstruction; 1–3 cm in diameter within 6 cm of pylorus 0.3% of live Projectile vomiting in births, mainly 3rd wk of life; visible firstborn and male; gastric peristalsis; rare in blacks palpable pylorus Very rare Nausea, vomiting May be familial Pyloric stenosis Infantile62–66 PREVALENCE PATHOGENESIS DISORDER (REF.) Table 12-2 Developmental Abnormalities of the Stomach Hypertrophy and hyperplasia of circular muscle; normal autonomic ganglia Hypertrophy and hyperplasia of circular muscle Usually submucosal; pancreatic ducts or acini; islets less common HISTOLOGY Antrum rotates up and to left or right Posterior wall 2 cm below esophagogastric junction Right-sided stomach Inversion: pylorus more cephalad than esophagogastric junction Mainly greater curvature rupture and perforation Variably sized cyst; often greater curvature Usually no communication with gastric lumen All layers of stomach; rarely lined by squamous epithelium Complete segmental defect; Gastric mucosa; stomach ends blindly rarely, squamous Fibrous cord. Atretic strand of epithelium mucosa and seromuscular layer Webs: by endoscopy, portion distal to web can be mistaken for duodenal bulb Small stomach Failure to rotate and differentiate into different parts Gastric filling defect with central umbilication; may be cystic Pyloric channel elongated and narrowed A 2- to 3-cm ovoid mass in ­pylorus; knob-like projection into duodenum GROSS APPEARANCES Situs inversus As for duplications May also involve esophagus; onethird of patients have other anomalies Other congenital malformations Pancreatitis, carcinoma (rare) Exclude peptic ulcer and malignancy COMMENT 566 Lewin, Weinstein, and Riddell’s Gastrointestinal Pathology and Its Clinical Implications Figure 12-19. Diagram of known mechanisms involved in gastric acid secretion. frequently confused with other cells, very few fibroblasts, macrophages, eosinophils, plasma cells, and lymphocytes. Mast cells are scattered in the interpit regions as well as between the fundic glands.55 In the gastric corpus, glands are so tightly packed that it may be hard to see the lamina propria, except just beneath the surface mucous cells. Small lymphoid follicles may be seen just above the muscularis mucosae; these are normal and physiological56—we disagree with the notion that no lymphoid aggregates are present normally. They are usually small but present nonetheless. There is also a finely dispersed network of reticulin and collagen fibers. These, as well as fibers of smooth muscle, extend upward from the muscularis mucosae and may appear as fern-like streamers in the lamina propria, reaching the superficial portion of the mucosa. This is a more prominent finding in the antrum, especially near the pylorus. Tiny vessels are seen in the lamina propria, but it may be impossible to differentiate lymph capillaries from blood capillaries without the use of immunohistochemistry. With electron microscopy, ­ it has been demonstrated that, like the large bowel, lymph capillaries are primarily confined to the basal portion of the mucosa just above the muscularis mucosae. In contrast, blood capillaries are distributed throughout the mucosa.57 There is considerable normal variation in the density of the lamina propria cells located between the pits. This variability is more prominent in antral gland mucosa, where the pits are longer. However, while occasional lymphocytes, histiocytes, mast cells, Riddell_Chap12.indd 566 and eosinophils are present, plasma cells are uncommon, and more that occasional cells reflect chronic inflammation. Neutrophils are normally absent. Muscularis Mucosae As elsewhere throughout the intestinal tract, the muscularis mucosae has both a thin layer of internal, primarily circular, muscle and an outer longitudinal layer. In the cardiac and antral glands, mucosal strands of muscle fibers may radiate into the lamina propria from the muscularis mucosae. This may be very prominent in the distal antrum and, on first glance, may be misinterpreted as fibrosis. Sometimes, lymphoid follicles are located at the bases of the glands above the muscularis mucosae, or they may actually breach it and occupy part of the upper submucosa. Submucosa. The submucosa consists of loose connective tissue, a rich plexus of blood vessels, sizable lymphatic vessels, the ganglion cells of Meissner’s plexus, scattered mast cells, and mononuclear cells. Muscularis propria, ICCs, and serosa. The muscularis propria consists of three layers: outer longitudinal, middle circular, and inner oblique. The outer longitudinal layer is most concentrated along both curvatures. The middle circular zone encircles the body of the stomach and is thickened distally to form the pyloric sphincter. The inner oblique fibers pass down from the fundus over both the anterior and posterior walls. 2/6/2014 12:41:30 PM Chapter 12 Stomach: Normal Structures and Developmental Abnormalities A 567 B Figure 12-20. Heterotopic islands of endocrine mucosa (A) in the oxyntic mucosa (adjacent normal oxyntic mucosa is seen right) and (B) in the antrum. In both, the waterclear “halo” cells are present in abundance. DEVELOPMENTAL ABNORMALITIES OF THE STOMACH With the exception of infantile pyloric stenosis and pancreatic heterotopia, most of the other developmental abnormalities of the stomach are rare. Some findings, such as goblet cells in the stomach of adults, are difficult to classify as a rare congenital cause,59,60 because intestinal metaplasia is such a common accompaniment of nonerosive gastritis or focal injury. Gastric heterotopias, in which gastric tissue is located outside of the stomach, are not discussed here. These are discussed in the chapters dealing with specific regions of the gastrointestinal tract as in gastric heterotopia in the upper esophagus and in Meckel’s diverticulum. Gastric heteroptopia occurs in a variety of organs and is discussed there. Gastric hamartomas are discussed in Chapter 14. Within the stomach, occasionally, small islands of islet tissue can be found in both the antral or oxyntic mucosa in the absence of any other features (Fig. 12-20). Riddell_Chap12.indd 567 Pathogenesis and Clinical Features The pathogenesis of developmental disorders is poorly understood.61 Table 12-2 outlines and references the various disorders. With the exception of pancreatic heterotopia, most congenital anomalies present in the postnatal period or in childhood. Rarely, pyloric stenosis gastric duplications and gastric webs present in adulthood. References 1. Moore KL, ed. The Developing Human: Clinically Oriented Embryology. 7th ed. Philadelphia, London, Toronto: W.B. Saunders Company; 2013. 2. Tsutsumi Y. Immunohistochemical studies on glucagon, glicentin and pancreatic polypeptide in human stomach: normal and pathological conditions. Histochem J. 1984;16(8):869–883. 3. Stein BA, Buchan AM, Morris J, et al. The ontogeny of regulatory peptide-containing cells in the human fetal stomach: an immunocytochemical study. J Histochem Cytochem. 1983;31(9):1117–1125. 4. Yasugi S. Regulation of pepsinogen gene expression in epithelial cells of vertebrate stomach during development. Int J Dev Biol. 1994;38(2):273–279. 5.Johnson LR. Functional development of the stomach. Annu Rev Physiol. 1985;47:199–215. 6. Deren JS. Development of structure and function in the fetal and newborn stomach. Am J Clin Nutr. 1971;24(1): 144–159. 7. Park YS, Park HJ, Kang GH, et al. Histology of gastroesophageal junction in fetal and pediatric autopsy. Arch Pathol Lab Med. 2003;127(4):451–455. 8. Chandrasoma PT. Fetal “cardiac mucosa” is not adult cardiac mucosa. Gut. 2003;52(12):1798; author reply 9. 9. De Hertogh G, Van Eyken P, Ectors N, Geboes K. On the origin of cardiac mucosa: a histological and immunohistochemical study of cytokeratin expression patterns in the developing esophagogastric junction region and stomach. World J Gastroenterol. 2005;11(29):4490–4496. Chapter 12 The muscularis propria is bounded on its outer surface by a serosa similar to that of the other regions of the gut. It consists of loose connective tissue and contains blood vessels, lymphatics, and nerve fibers. The muscularis propria is richly innervated with nerves, while interstitial cells of Cajal are present both in and immediately around the myenteric plexus, while intramuscular interstitial cells are also present in all layers of the muscle. If interstitial cells are being assessed, it is very wise to have normal controls, ideally from the same area of the stomach, with which they can be compared.58 2/6/2014 12:41:33 PM 568 Lewin, Weinstein, and Riddell’s Gastrointestinal Pathology and Its Clinical Implications 10. Riddell RH, Odze RD. Definition of Barrett’s esophagus: time for a rethink–is intestinal metaplasia dead? Am J Gastroenterol. 2009;104(10):2588–2594. 11. Ronkainen J, Aro P, Storskrubb T, et al. Prevalence of Barrett’s esophagus in the general population: an endoscopic study. Gastroenterology. 2005;129(6):1825–1831. 12. Schutze M, Schulz M, Steffen A, et al. Beer consumption and the ‘beer belly’: scientific basis or common belief? Eur J Clin Nutr. 2009;63(9):1143–1149. 13. Owen DA. Normal histology of the stomach. Am J Surg Pathol. 1986;10(1):48–61. 14.Gottfried MR, McClave SA, Boyce HW. Incomplete intestinal metaplasia in the diagnosis of columnar lined esophagus (Barrett’s esophagus). Am J Clin Pathol. 1989;92(6):741–746. 15. Ishimura N, Amano Y, Kinoshita Y. Endoscopic definition of esophagogastric junction for diagnosis of Barrett’s esophagus: importance of systematic education and training. Dig Endosc. 2009;21(4):213–218. 16. Sato T, Kato Y, Matsuura M, et al. Significance of palisading longitudinal esophagus vessels: identification of the true esophagogastric junction has histopathological and oncological considerations. Dig Dis Sci. 2010;55(11): 3095–3101. 17. Moore JG, Dubois A, Christian PE, et al. Evidence for a midgastric transverse band in humans. Gastroenterology. 1986;91(3):540–545. 18.Rubin W, Ross LL, Sleisenger MH, et al. The normal human gastric epithelia. A fine structural study. Lab Invest. 1968;19(6):598–626. 19. Helander HF. The cells of the gastric mucosa. Int Rev Cytol. 1981;70:217–289. 20. Day DW, Morson BC. Structure and infrastructure. Front Gastrointest Res. 1980;6:1–19. 21. Macdonald WC, Trier JS, Everett NB. Cell proliferation and migration in the stomach, duodenum, and rectum of man: radioautographic studies. Gastroenterology. 1964;46:405–417. 22. Hersey SJ, Sachs G. Gastric acid secretion. Physiol Rev. 1995;75(1):155–189. 23. el-Zimaity HM, Verghese VJ, Ramchatesingh J, et al. The gastric cardia in gastro-oesophageal disease. J Clin Pathol. 2000;53(8):619–625. 24. Helander HF, Leth R, Olbe L. Stereological investigations on human gastric mucosa: I. Normal oxyntic mucosa. Anat Rec. 1986;216(3):373–380. 25. Schubert ML. Gastric exocrine and endocrine secretion. Curr Opin Gastroenterol. 2009;25(6):529–536. 26. Samloff IM. Cellular localization of group I pepsinogens in human gastric mucosa by immunofluorescence. Gastroenterology. 1971;61(2):185–188. 27.Samloff IM, Liebman WM. Cellular localization of the group II pepsinogens in human stomach and duodenum by immunofluorescence. Gastroenterology. 1973;65(1): 36–42. 28. Li H, Helander HF. Parietal cell kinetics after administration of omeprazole and ranitidine in the rat. Scand J Gastroenterol. 1995;30(3):205–209. 29. Otte JM, Neumann HM, Brand S, et al. Expression of beta-defensin 4 is increased in human gastritis. Eur J Clin Invest. 2009;39(2):126–138. 30. Tominaga K. Distribution of parietal cells in the antral mucosa of human stomachs. Gastroenterology. 1975;69(6):1201–1207. 31. Slomiany BL, Slomiany A. Role of mucus in gastric mucosal protection. J Physiol Pharmacol. 1991;42(2):147–161. 32. Ota H, Katsuyama T. Alternating laminated array of two types of mucin in the human gastric surface mucous layer. Histochem J. 1992;24(2):86–92. Riddell_Chap12.indd 568 33. Matsuo K, Ota H, Akamatsu T, et al. Histochemistry of the surface mucous gel layer of the human colon. Gut. 1997;40(6):782–789. 34. Moniaux N, Escande F, Porchet N, et al. Structural organization and classification of the human mucin genes. Front Biosci. 2001;6:D1192–D1206. 35.Akamatsu T, Katsuyama T. Histochemical demonstration of mucins in the intramucosal laminated structure of human gastric signet ring cell carcinoma and its relation to submucosal invasion. Histochem J. 1990;22(8):416–425. 36. Tatematsu M, Tsukamoto T, Inada K. Stem cells and gastric cancer: role of gastric and intestinal mixed intestinal metaplasia. Cancer Sci. 2003;94(2):135–141. 37. Ota H, Katsuyama T, Ishii K, et al. A dual staining method for identifying mucins of different gastric epithelial mucous cells. Histochem J. 1991;23(1):22–28. 38.Buisine MP, Devisme L, Maunoury V, et al. Developmental mucin gene expression in the gastroduodenal tract and accessory digestive glands. I. Stomach. A relationship to gastric carcinoma. J Histochem Cytochem. 2000;48(12):1657–1666. 39. Buisine MP, Devisme L, Degand P, et al. Developmental mucin gene expression in the gastroduodenal tract and accessory digestive glands. II. Duodenum and liver, gallbladder, and pancreas. J Histochem Cytochem. 2000;48(12):1667–1676. 40. Nakajima K, Ota H, Zhang MX, et al. Expression of gastric gland mucous cell-type mucin in normal and neoplastic human tissues. J Histochem Cytochem. 2003;51(12):1689–1698. 41. Filipe MI. Mucins in the human gastrointestinal epithelium: a review. Invest Cell Pathol. 1979;2(3):195–216. 42. Sachs G, Zeng N, Prinz C. Physiology of isolated gastric endocrine cells. Annu Rev Physiol. 1997;59:243–256. 43. Rindi G, Leiter AB, Kopin AS, et al. The “normal” endocrine cell of the gut: changing concepts and new evidences. Ann N Y Acad Sci. 2004;1014:1–12. 44. Thompson M, Fleming KA, Evans DJ, et al. Gastric endocrine cells share a clonal origin with other gut cell lineages. Development. 1990;110(2):477–481. 45. Kojima M, Hosoda H, Date Y, et al. Ghrelin is a growthhormone-releasing acylated peptide from stomach. Nature. 1999;402(6762):656–660. 46. Date Y, Kojima M, Hosoda H, et al. Ghrelin, a novel growth hormone-releasing acylated peptide, is synthesized in a distinct endocrine cell type in the gastrointestinal tracts of rats and humans. Endocrinology. 2000;141(11):4255–4261. 47. Simonsson M, Eriksson S, Hakanson R, et al. Endocrine cells in the human oxyntic mucosa. A histochemical study. Scand J Gastroenterol. 1988;23(9):1089–1099. 48. Tesauro M, Schinzari F, Caramanti M, et al. Cardiovascular and metabolic effects of Ghrelin. Curr Diabetes Rev. 2010;6(4):228–235. 49. Suzuki K, Simpson KA, Minnion JS, et al. The role of gut hormones and the hypothalamus in appetite regulation. Endocr J. 201057(5):359–372. 50. Falken Y, Hellstrom PM, Sanger GJ, et al. Actions of prolonged ghrelin infusion on gastrointestinal transit and glucose homeostasis in humans. Neurogastroenterol Motil. 201022(6):e192–e200. 51. Prinz C, Zanner R, Gratzl M. Physiology of gastric enterochromaffin-like cells. Annu Rev Physiol. 2003;65:371–382. 52. Lloyd KC, Wang J, Aurang K, et al. Activation of somatostatin receptor subtype 2 inhibits acid secretion in rats. Am J Physiol. 1995;268(1 pt 1):G102–G106. 53. Martinez V, Curi AP, Torkian B, et al. High basal gastric acid secretion in somatostatin receptor subtype 2 knockout mice. Gastroenterology. 1998;114(6):1125–1132. 2/6/2014 12:41:33 PM Chapter 12 Stomach: Normal Structures and Developmental Abnormalities 54. Schubert ML, Edwards NF, Makhlouf GM. Regulation of gastric somatostatin secretion in the mouse by luminal acidity: a local feedback mechanism. Gastroenterology. 1988;94(2):317–322. 55.Steer HW. Mast cells of the human stomach. J Anat. 1976;121(pt 2):385–397. 56. Graham DY, Opekun AR, Osato MS, et al. Challenge model for Helicobacter pylori infection in human volunteers. Gut. 2004;53(9):1235–1243. 57. Lehnert T, Erlandson RA, Decosse JJ. Lymph and blood capillaries of the human gastric mucosa. A morphologic basis for metastasis in early gastric carcinoma. Gastroenterology. 1985;89(5):939–950. 58. Harberson J, Thomas RM, Harbison SP, et al. Gastric neuromuscular pathology in gastroparesis: analysis of fullthickness antral biopsies. Dig Dis Sci. 2010;55(2):359–370. 59. Kimura K. Chronological transition of the fundic-pyloric border determined by stepwise biopsy of the lesser and greater curvatures of the stomach. Gastroenterology. 1972;63(4):584–592. 60. Salenius P. On the ontogenesis of the human gastric epithelial cells. A histologic and histochemical study. Acta Anat Suppl (Basel). 1962;50(46):1–76. 61. Berant M, Aviad I, Jacobs J. Heterotopic duodenal mucosa in the stomach. Am J Dis Child. 1965;110(5):566–569. 62.Simstein NL. Congenital gastric anomalies. Am Surg. 1986;52(5):264–268. 63. Shim WK, Campbell A, Wright SW. 276 cases of pyloric stenosis in Hawaii. II. Racial aspects. Hawaii Med J. 1970;29(4):292–295. 64. Friesen SR, Pearse AG. Pathogenesis of congenital pyloric stenosis: histochemical analyses of pyloric ganglion cells. Surgery. 1963;53:604–608. 65.Grant GA, McAleer JA. Increasing incidence of infantile hypertrophic pyloric stenosis, 1971–1983. Ir Med J. 1986;79(5):118–119. 66. Leahy PF, Farrell R, O’Donnell B. 300 infants with hypertrophic pyloric stenosis: presentation and outcome. Ir Med J. 1986;79(5):114–116. 67. Wellmann KF, Kagan A, Fang H. Hypertrophic Pyloric Stenosis in Adults. Survey of the Literature and Report of a Case of the Localized Form (Torus Hyperplasia). Gastroenterology. 1964;46:601–608. 68. Dolan RV, ReMine WH, Dockerty MB. The fate of heterotopic pancreatic tissue. A study of 212 cases. Arch Surg. 1974;109(6):762–765. 69.Rose C, Kessaram RA, Lind JF. Ectopic gastric pancreas: a review and report of 4 cases. Diagn Imaging. 1980;49(4):214–218. Riddell_Chap12.indd 569 569 70. Guttman FM, Braun P, Garance PH, et al. Multiple atresias and a new syndrome of hereditary multiple atresias involving the gastrointestinal tract from stomach to rectum. J Pediatr Surg. 1973;8(5):633–640. 71. Bar-Maor JA, Nissan S, Nevo S. Pyloric atresia. A hereditary congenital anomaly with autosomal recessive transmission. J Med Genet. 1972;9(1):70–72. 72. Clements JL Jr, Jinkins JR, Torres WE, et al. Antral mucosal diaphragms in adults. Am J Roentgenol. 1979;133(6): 1105–1111. 73.Feliciano DV, van Heerden JA. Pyloric antral mucosal webs. Mayo Clin Proc. 1977;52(10):650–653. 74. Shackelford GD, McAlister WH, Brodeur AE, et al. Congenital microgastria. Am J Roentgenol Radium Ther Nucl Med. 1973;118(1):72–76. 75.Kessler H, Smulewicz JJ. Microgastria associated with agenesis of the spleen. Radiology. 1973;107(2):393–396. 76.Chen YM, Teague RS, Ott DJ, et al. Gastric duplication cyst simulating leiomyoma. Gastrointest Endosc. 1987;33(3):250–252. 77.Bidwell JK, Nelson A. Prenatal ultrasonic diagnosis of congenital duplication of the stomach. J Ultrasound Med. 1986;5(10):589–591. 78. Tihansky DP, Sukarochana K, Hanrahan JB. Pyloroduodenal duplication cyst. Am J Gastroenterol. 1986;81(3): 189–191. 79. Abrami G, Dennison WM. Duplication of the stomach. Surgery. 1961;49:794–801. 80. Wieczorek RL, Seidman I, Ranson JH, et al. Congenital duplication of the stomach: case report and review of the English literature. Am J Gastroenterol. 1984;79(8):597–602. 81. Meeroff M, Gollan JR, Meeroff JC. Gastric diverticulum. Am J Gastroenterol. 1967;47(3):189–203. 82. Mc LN, Purves JK, Saunders RL. The genesis of gastric and certain intestinal diverticula and enterogenous cysts. Surg Gynecol Obstet. 1954;92(2):135–141. 83.Hewlett PM. Isolated dextrogastria. Br J Radiol. 1982; 55(657):678–681. 84. Shaw A, Blanc WA, Santulli TV, et al. Spontaneous rupture of the stomach in the newborn: a clinical and experimental study. Surgery. 1965;58:561–571. 85. Bayatpour M, Bernard L, McCune F, et al. Spontaneous gastric rupture in the newborn. Am J Surg. 1979;137(2): 267–269. 86.Patel NM. Chronic gastric volvulus: report of a case and review of literature. Am J Gastroenterol. 1985;80(3): 170–173. 87. Idowu J, Aitken DR, Georgeson KE. Gastric volvulus in the newborn. Arch Surg. 1980;115(9):1046–1049. Chapter 12 2/6/2014 12:41:33 PM