Mammography I
advertisement

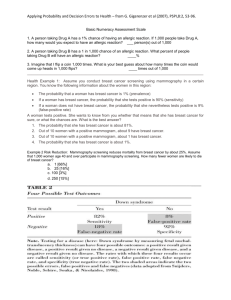
Mammography: Risks and benefits Zahra Anjomani Content • Overview of Breast Cancer • Mammography machine • Risks and Benefits of Mammography Overview of Breast Cancer • The most common form of cancer among women • The second most common cause of cancer related mortality • 1 of 8 women (12.2%) • One third of women with breast cancer die from breast cancer Risk Factors for Breast Cancer • Female (1% male) • Aging • Relative (mother or sister) • Menstrual history – early on set – late menopause • Child birth – After the age of 30 Risk Factors for Breast Cancer • Radiation exposure • Breast disease – Atypical Hyperplasia – Intraductal carcinoma in situ – Intralobular carcinoma in situ • Obesity • Diet – Fat – Alcohol Genetics • • • • BRCA-1 BRCA-2 P53, Rb-1 Her-2/neu, c-erB2, c-myc Anatomy • Breasts vary in size and shape! • Consist of glandular, fat, and muscle tissue Anatomy • Lymphatic vessels of breast drain into two sets of nodes – Axillary lymph nodes, laterally – Internal mammary lymph nodes, medially • Axillary nodes are often evaluated on mammograms Breast Cancer • There are two general categories of breast cancer: – Non-invasive (or in situ) cancer confined to lobules or ducts – Invasive cancer spread to fatty connective tissue Staging of Breast Cancer • The American Joint Committee on Cancer (AJCC) has designated staging by TNM – T= tumor size – N = lymph node involvement – M = metastasis Stage 1 • Tumor < 2.0 cm in greatest dimension • No nodal involvement (N0) • No metastases (M0) Stage II • 2.0< Tumor < 5 cm or • Ipsilateral axillary lymph node (N1) • No Metastasis (M0) Stage III • Tumor > 5 cm (T3) • or ipsilateral axillary lymph nodes fixed to each other or other structures (N2) • involvement of ipsilateral internal mammary nodes (N3) • Inflammatory carcinoma (T4d) Stage IV (Metastatic breast cancer) • Any T • Any N • Metastasis (M1) Abnormal signs and symptoms • • • • • Puckering Dimpling Retraction Nipple discharge Thickening of skin or lump or “knot” • Retracted nipple Principles Of Breast Cancer • Pt.s in early stages respond well to treatment • Patients with advanced disease do poorly • Earlier diagnosis, better chance of survival • Mammography is tool for early detection History of Mammography • 1913 – First attempt at mammography • 1950 – First utilized low kVp and high mAs techniques • 1960 – Development of xero-mammography • 1990 – Screen film mammography was accepted How does a mammography machine work? Differential attenuation • Small x-ray attenuation differences between normal and cancerous tissues in the breast require the use of x-ray equipment specially designed to optimize breast cancer detection • Attenuation differences between these tissues is highest at very low x-ray energies (10 to 15 keV) and is poor at higher energies (>35 keV) System design • Because of the risks of ionizing radiation, techniques that minimize dose and optimize image quality are essential, and have led to: – – – – – – Refinement of dedicated x-ray equipment Specialized x-ray tubes Compression devices Antiscatter grids Phototimers Detector systems Cathode & filament design • Mammographic x-ray tubes typically have dual filaments in a focusing cup that produces 0.3 and 0.1 mm nominal focal spot sizes – Minimize geometric blurring and maintain spatial resolution necessary for microcalcification detection Anode design • Mammographic x-ray tubes use a rotating anode • Molybdenum is the most common anode material; rhodium & tungsten also used • Source to image distance (SID) of 65 cm requires the effective anode angle to be at least 20º to avoid field cutoff for the 24 x 30 cm field area Heel effect • Lower x-ray intensity on the anode side of the field at short SID is very noticeable • Positioning the cathode over the chest wall of the patient and the anode over the nipple achieves better uniformity of the radiation transmitted through the breast • Orientation of the tube in this fashion also decreases the equipment bulk near the patient’s head for easier positioning Beam quality considerations • Computer modeling studies show that the optimal x-ray energy to achieve high subject contrast and the lowest radiation dose would be a monoenergetic beam of 15 to 25 keV, depending on breast composition and thickness • Optimal x-ray energy is achieved by the use of specific x-ray tube target materials and added filtration materials Filtration • Inherent filtration must be kept low; beryllium (Z = 4) is used for the tube port • Added tube filters of the same element as the target reduce the low- and high-energy x-rays in the spectrum and allow transmission of the characteristic x-ray energies Compression Device • Compression decreases thickness of breast, magnification and scatter • Increases contrast • Reduces motion unsharpness • Reduces dosage Compression Device • Made of firm plastic • Amount of compression: between 25 and 40 pounds pressure • Compression may be uncomfortable! Screen-Film Systems • Mammography cassettes contain a single screen • Film is single emulsion • Occasionally, extended time processing is used – (reduces dose and increases contrast) Digital mammography • Replaces the screen and film with a charged couple device (CCD) • CCD converts light into electrons • Electrons are sent to the computer where it is converted into a digital format and a radiographic image is produced on the CRT Digital versus Conventional Courtesy: Magee-Women’s Hospital of UPMC Craniocaudal Projection Mediolateral Oblique Radiography Of Augmented Breast (implants) • 8 projections must be obtained (2x4) Mammographer’s Nightmare Benefits versus Risks from Mammography • When breast cancer is detected before it has spread to lymph nodes or to other parts of the body, the 5-year survival rate is 97% • Early detection and early treatment can improve the chances of surviving breast cancer. Currently, mammography is the best tool available to detect the earliest warning signs of breast cancer Types of Mammography I) Diagnostic mammography Performed on patients with symptoms II) Screening mammography Performed as a preventative measure Usually done between the ages of 40 and 50 Risk v. Benefit • The most important benefit of mammographic examinations is detecting breast cancer at an early stage and perhaps reducing mortality I) Screening programs • Breast cancer screening programs rely on x-ray mammography because it is a low-cost, lowradiation-dose procedure with the sensitivity to detect early-stage breast cancer • American Cancer Society • National Cancer Institute • American College of Radiology encourage mammograms every two years for women ages 40 to 49 Screening program for woman between 40 and 50 is still controversial Screening mammography Risk factors • false-positive – mean greater expense • false-negative – a rate of missed tumors Likelihood of saving a life Four categories of cancers found by mammography : • a) cancers that are so easy to treat that a later detection would have produced the same total cure • b) cancers so aggressive that even "early" detection is too late • c) cancers that are so slow-growing that the woman would die of other causes before the cancer produces symptoms • e) cancers whose treatment outcome improves as a result of earlier detection. Only between 3% and 13% of breast cancers fall into the last category II) Diagnostic Mammogram • For woman presenting with clinical evidence of breast disease, palpable mass or other symptom • Uses specific projections to – Rule out cancer – Demonstrate suspicious area seen on screening mammogram Risk of Causing Breast Cancer by Mammography • Mammograms use doses of ionizing x-rays to create images. One of the potential risks of mammography is the radiation exposure associated with mammography. Dose from Mammography: • American College of Radiology The average dose at accredited mammography facilities was reported to be 1.38 mGy per view, or typically double this dose (2.8 mGy) per examination (because 2 views of each breast are typically obtained) Dose-Incidence Relationship The question of whether there is a practical threshold at low doses for radiation-induced breast cancer has been evaluated by a number of researchers, including Land et al., who inferred that the best statistical fit to the available data was a linear doseresponse curve Modifiers of dose response • exposure before the age of 20 years carries the greatest risk. • a history of benign breast disease • exposure to radiation while pregnant • genetic factors The magnitude of risk per unit dose depends strongly on when radiation exposure occurs Summery • The most important benefit – detecting breast cancer at an early stage. • For asymptomatic women under 35 the risk of breast cancer is not high enough to justify the risk of radiation exposure. • The evidence shows that there is small benefit in terms of early detection in screening of that woman between 40 and 50. • Ionizing radiation is a breast cancer risk factor – the risk increases linearly with dose. – Age at exposure is an important factor of the radiationrelated breast cancer risk. Risk v. Benefit • Breast cancer in United States in 2007 (estimated): New cases: 192,370 (female); 1,910 (male) Deaths: 40,170 (female); 440 (male) • Us population 306 million in 2007- 133 deaths /million • Mortality risk from mammography induced radiation is 5 deaths/ million pts. using screen film mammography • More risky to refuse mammography! THE END