VACCINES, THE HUMAN IMMUNE SYSTEM,
AND IMMUNE RESPONSES
by
George A. Wistreich
Ph.D., F(AAM)
RC Educational Consulting Services, Inc.
16781 Van Buren Blvd, Suite B, Riverside, CA 92504-5798
(800) 441-LUNG / (877) 367-NURS
www.RCECS.com
Vaccines, The Human Immune System,
And Immune Responses
BEHAVIORAL OBJECTIVES
UPON COMPLETION OF THE READING MATERIAL, THE PRACTITIONER WILL BE
ABLE TO:
1. Describe the components of the human immune system and their respective functions.
2. Briefly describe the general features of innate and acquired immune responses.
3. Discuss the components involved in the innate and acquired immune responses.
4. Distinguish among the different cells involved with immune responses.
5. Describe the states of immunity.
6. Distinguish between active and passive forms of immunity.
7. List the major infectious diseases that are preventable by immunization.
8. Briefly describe the components of the different categories of vaccines currently in-use.
9. Briefly describe the different, general types of bacterial and viral vaccines currently inuse.
10. Discuss the causes and the means of transmission and reservoirs of infection for the
major infectious diseases that are preventable by immunization.
11. Briefly describe the major features of vaccines that are routinely used for the prevention
of infectious disease as well as those that are of a non-routine use.
12. Discuss the various risk factors and groups at risk for infectious diseases.
13. Describe the types of side effects that can occur with vaccines.
COPYRIGHT © 2007 By RC Educational Consulting Services, Inc.
TX 6-578-642
Authored by: George A. Wistreich, Ph.D., F(AAM) 2007
ALL RIGHTS RESERVED
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
2
Vaccines, The Human Immune System,
And Immune Responses
This course is for reference and education only. Every effort is made to ensure that the clinical
principles, procedures and practices are based on current knowledge and state of the art
information from acknowledged authorities, texts, and journals. This information is not intended
as a substitution for a diagnosis or treatment given in consultation with a qualified health care
professional.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
3
Vaccines, The Human Immune System,
And Immune Responses
TABLE OF CONTENTS
PREFACE ............................................................................................................................9
INTRODUCTION ...............................................................................................................9
A BRIEF HISTORY OF VACCINATION .......................................................................10
BASIC IMMUNOLOGY TERMS ....................................................................................13
THE IMMUNE SYSTEM .................................................................................................13
THE INNATE IMMUNE SYSTEM ............................................................................13
SELECTED INNATE RESPONSE COMPONENTS..................................................14
INNATE IMMUNITY DYSFUNCTION.....................................................................19
THE ADAPTIVE (ACQUIRED) IMMUNE SYSTEM ...............................................19
SELECTED ACQUIRED RESPONSE COMPONENTS............................................20
T- AND B- LYMPHOCYTES......................................................................................20
A BRIEF EXPLANATION OF ANTIBODY-MEDIATED (HUMORAL)
AND CELL-MEDIATED RESPONSES .....................................................................21
VACCINE TYPES.............................................................................................................24
COMBINED OR SINGLE-DOSE VACCINES...........................................................26
EXAMPLES OF ROUTINELY USED VACCINES ...................................................26
ROUTES OF VACCINE ADMINISTRATION ..........................................................26
VACCINE SIDE EFFECTS .........................................................................................27
AN EXAMPLE OF A RECOMMENDED IMMUNIZATION SCHEDULE .............28
STATES OF IMMUNITY............................................................................................30
THE ROLE OF SUBCLINICAL INFECTIONS ....................................................31
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
4
Vaccines, The Human Immune System,
And Immune Responses
EXAMPLES OF SELECTED BACTERIAL DISEASES AND
ROUTINELY USED VACCINES ....................................................................................31
MENINGOCOCCAL MENINGITIS ...........................................................................31
THE CAUSE............................................................................................................32
TRANSMISSION ....................................................................................................32
RESERVOIRS .........................................................................................................33
RISK FACTORS .....................................................................................................33
VACCINES AND RECOMMENDATIONS FOR USE.........................................33
THE QUESTION OF REVACCINATION.............................................................34
PERTUSSIS..................................................................................................................34
THE CAUSE............................................................................................................34
TRANSMISSION ....................................................................................................34
VACCINES..............................................................................................................35
PNEUMOCOCCAL LOBAR PNEUMONIA AND MENINGITIS............................35
THE DISEASES AND THE CAUSATIVE AGENT .............................................35
TRANSMISSION ....................................................................................................36
THE PNEUMOCOCCAL POLYSACCHARIDE VACCINE-23 (PPV-23) ..........36
CURRENT RECOMMENDATIONS FOR USE...............................................36
THE PNEUMOCOCCAL-CONJUGATE VACCINE-7 (PCV-7).....................37
IMMUNIZATION SCHEDULE ........................................................................37
SIDE EFFECTS .............................................................................................38
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
5
Vaccines, The Human Immune System,
And Immune Responses
EXAMPLES OF SELECTED VIRAL DISEASES AND ROUTINELY
USED VACCINES ............................................................................................................38
HEPATITIS A INFECTION ........................................................................................38
THE CAUSE............................................................................................................38
TRANSMISSION ....................................................................................................38
GROUPS AT RISK .................................................................................................39
HAV VACCINES....................................................................................................39
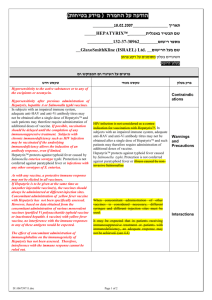
HEPATITIS B...............................................................................................................39
THE CAUSE............................................................................................................40
TRANSMISSION ....................................................................................................40
VACCINES..............................................................................................................41
VACCINE RECOMMENDATIONS IN CASES OF
PERINATAL HEPATITIS B ..................................................................................42
RECOMMENDED DOSES.....................................................................................43
SIDE EFFECTS .......................................................................................................43
PASSIVE IMMUNIZATION..................................................................................43
INFLUENZA ................................................................................................................44
THE CAUSE-INFLUENZA VIRUS TYPES..........................................................44
TRANSMISSION ....................................................................................................45
GROUPS AT RISK .................................................................................................45
VACCINES..............................................................................................................45
PERSONS WHO SHOULD NOT BE GIVEN LAIV.............................................46
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
6
Vaccines, The Human Immune System,
And Immune Responses
POLIO...........................................................................................................................47
THE CAUSE............................................................................................................47
TRANSMISSION ....................................................................................................47
THE VACCINES.....................................................................................................47
VARICELLA-ZOSTER ...............................................................................................48
THE CAUSE............................................................................................................48
TRANSMISSION ....................................................................................................48
THE VACCINES.....................................................................................................49
ADVERSE REACTIONS........................................................................................49
THE USE OF VARICELLA-ZOSTER IMMUNOGLOBULIN ............................49
EXAMPLES OF NON-ROUTINELY USED VACCINES ..............................................50
ANTHRAX ...................................................................................................................50
THE CAUSE............................................................................................................50
TRANSMISSION ....................................................................................................50
HUMAN ANTHRAX VACCINE ...........................................................................50
THE IMMUNIZATION SCHEDULE ....................................................................50
SIDE EFFECTS .......................................................................................................51
RABIES ........................................................................................................................51
THE CAUSE............................................................................................................51
TRANSMISSION ....................................................................................................51
VACCINES..............................................................................................................52
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
7
Vaccines, The Human Immune System,
And Immune Responses
PRE-EXPOSURE ....................................................................................................52
EXPOSURE.............................................................................................................52
POST-EXPOSURE..................................................................................................52
SMALLPOX .................................................................................................................52
THE CAUSE............................................................................................................53
TRANSMISSION ....................................................................................................53
THE VACCINE .......................................................................................................53
VACCINES UNDER DEVELOPMENT ................................................................54
ROUTES OF ADMINISTRATION ........................................................................55
RESPONSES TO SMALLPOX VACCINATION.......................................................55
COMPLICATIONS .................................................................................................55
IMMUNITY.............................................................................................................56
THE CURRENT PICTURE OF SMALLPOX........................................................56
VACCINES IN DEVELOPMENT...............................................................................56
CONCLUDING STATEMENTS ......................................................................................57
GLOSSARY ......................................................................................................................58
SUGGESTED READING AND REFERENCES .............................................................60
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
8
Vaccines, The Human Immune System,
And Immune Responses
PREFACE
F
ooling the human immune system is not a simple matter, but that is what a successful
vaccine must do. In reality, vaccines are impostors, harmless in nature, but intended to be
recognized by the human immune system as being foreign and a potential threat to the
body. If the deception works, a harmless vaccine offers an effective means of self-defense that is
remembered for years to come. This course presents concise descriptions of how the human
immune system works, the bases of immune responses to pathogens and their products, and the
range of vaccines that are currently available to combat a large number of infectious disease
agents.
INTRODUCTION
I
mmunization is one of the great success stories in the history of public health. That success
is the result of the administration of safe and highly effective vaccines, which are provided
through the collaboration between government and industry and are used widely in the
populations for whom they are intended. The availability and appropriate use of vaccines are the
first critical components of a successful public health immunization program. Continued success
of such a program depends on an available supply of vaccines that are recommended for routine
use. This course first presents a brief history of vaccination and selected basic immunologic
concepts and related factors to provide a basis for understanding how vaccines work and
recognizing their value to the public. This presentation is followed by descriptions of routinely
used vaccines together with brief considerations of the associated diseases. Attention is also
given to recommendations for immunization schedules for children, adolescents, and adults, and
some vaccines under development. Brief consideration also is given to the complexities and
problems associated with vaccine development and production.
Abbreviations Used
ACIP:
aP:
AVA:
BCG:
CD:
DNA:
DPT:
HAV:
HBV:
Hep A:
Hep B:
Hib:
IG:
IL:
Advisory Committee for Immunization Practices
acellular pertussis (vaccine)
aluminum-hydroxide-precipitated
bacillus of Calmette and Guerin
cluster of differentiation
deoxyribonucleic acid
diphtheria, pertussis, tetanus
hepatitis A
hepatitis B
hepatitis A
hepatitis B
Haemophilus influenzae, type b
immune globulin
interleukin
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
9
Vaccines, The Human Immune System,
And Immune Responses
MHC:
MMR:
MSM:
MVA:
PPV:
RNA:
Tc:
Td:
TOP:
VAERS:
VZIG:
major-histocompatibilty-complex
measles, mumps, and rubella
men who have sex with men
modified vaccinia Ankara
pneumococcal polysaccharide vaccine
ribonucleic acid
cytotoxic T-cell
tetanus-diphtheria toxoids
trivalent polio preparation
Vaccine Adverse Event Reporting System
varicella-zoster immunoglobulin
A BRIEF HISTORY OF VACCINATION
A
common practice among ancient peoples to protect themselves against venomous snakes
was to introduce small amounts of venom in scratches made on the skin. The Chinese
used this form of immunization to protect themselves against smallpox more than 2,000
years ago. The procedure used involved exposure to skin scabs from infected individuals who
had survived the disease in the hope that it had been caused by a relatively milder form of
disease agent. This practice spread through Asia by trade routes and, in spite of its failure rate of
one percent or more, was well accepted in the Middle East, and eventually also reached Europe.
At the end of the eighteenth century the English physician Edward Jenner noticed that milkmaids
many of whom while carrying out their milking chores developed cowpox, were immune to
smallpox. Armed with some of the fluid from the vesicles on the hands of the milkmaids found
that he was able to protect susceptible individuals against smallpox by inoculating them with this
material (Figure 1).
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
10
Vaccines, The Human Immune System,
And Immune Responses
Figure 1. One of several paintings showing Dr. Jenner injecting cowpox material into the arm of
a child. A milkmaid and a cow can be seen in the open upper doorway on the left-side of this
painting.
Jenner coined the term variolae vaccinae, which means smallpox of the cow, and from it the term
vaccination was derived and used by surgeon Richard Dunning of Plymouth, England. Dunning
in his pamphlet “Some Observations on Vaccination,” published in London in 1800. Later in
1877, Louis Pasteur developed a chicken cholera vaccine, which consisted of old weakened
(attenuated) bacteria. Inoculated chickens developed a mild form of the disease, but more
importantly became immune to future exposures. Pasteur adopted the term vaccination in 1881
as a tribute to Jenner, for any protective inoculation. Also in 1881, applying the same concept of
attenuation Pasteur developed a vaccine to protect sheep against anthrax.
Starting in 1799, Dr. Benjamin Waterhouse popularized vaccination against smallpox in the
United States. On July 8, 1800, Waterhouse started his own vaccination program with the
inoculation of three of his own children and three servants. At the request of Waterhouse,
one of his inoculated children was kept in a hospital bed alongside a smallpox patient for 12 days
without developing the disease. The results of this event were reported in the pamphlet “A
Prospect of Extinguishing the Smallpox,” written by Waterhouse. Copies were sent to President
John Adams and Vice-President Thomas Jefferson. Later, as President, Jefferson played a major
role in the introduction and acceptance of vaccination into the United States.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
11
Vaccines, The Human Immune System,
And Immune Responses
In 1966, with Jenner’s concept of eradicating smallpox in mind, and having a cash input of only
twelve dollars, 687 WHO workers from 73 countries, the World Health Organization mounted a
coordinated global search and destroy operation against smallpox. This intensive
vaccination program resulted in the eradication of smallpox in May, 1980. The last known
human casualty of the disease was found in the Merca District of Somalia on October 26, 1977.
The last case of smallpox in the United States occurred in 1949. Figure 2 shows the appearance
of one of the last victims of smallpox.
Figure 2. One of the last victims of the virus disease, smallpox.
(Since the use of smallpox virus as a bioterrorists weapon does exist, additional details of this
disease agent, the disease, and aspects of immunization related to it are presented in a later
section.)
The next sections present some of the basic terminology immunologic concepts associated with
immunity, and explanations of how vaccines contribute to an individual’s protection against
infectious diseases.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
12
Vaccines, The Human Immune System,
And Immune Responses
BASIC IMMUNOLOGY TERMS
T
he ability of an organism’s immune system to resist infection caused by most pathogenic
microorganisms and to counter the effects of other cells and substance considered to be
foreign is generally referred to as immunity. Cells and molecules recognized as being
foreign collectively are known as immunogens and are usually protein, polysaccharide, or
nucleic acid in nature. (Foreign molecules also are known as antigens when they are detected by
the immune system). Once pathogens break through first lines of defense such as the skin,
mucous membranes and other anatomical barriers, these macromolecules trigger highly
sophisticated immune responses. One of these responses involves the interactions immune
system cells such as T- and B-lymphocytes, with the end result being the production of specific
proteins known as antibodies or immunoglobulins (IGs). Generally, antibodies occur as
soluble proteins in blood serum or other body secretions, and react in some manner with the
antigen that provoked their formation and production.
THE IMMUNE SYSTEM
T
he human immune system is an organization of cells and molecules with specialized roles
in detecting cells and/or substances that are foreign to the body and defending against
them. Such foreign materials include invading pathogenic microorganisms and/or their
toxic products. The immune system has traditionally been divided into innate and adaptive
subdivisions, each with different functions and roles.
There are two fundamentally different types of responses to materials recognized as being
foreign by the immune system. These are the natural (innate) and acquired (adaptive)
responses, which originate from the innate and adaptive immune systems, respectively. Both of
these responses which usually work together to eliminate pathogenic microorganisms and other
cells and/or substances considered to be foreign by the human immune system. The main
distinction between the innate and adaptive immune systems lies in the mechanisms and
receptors used for the recognition of foreign cells and molecules.
In order to establish an infection, a pathogen must first overcome a number of initial barriers,
which depending on the site of the attack could include mucus, gastric juices, and a variety of
host enzymes. Such host factors are either directly anti-microbial or prevent the pathogen’s
attachment to body surfaces. Pathogens capable of breaking through such barriers, then
encounter the two further levels of defense, the innate and acquired immune responses. These
responses use a number of different body cells and molecules.
The Innate Immune System
The operating mechanisms involved with the innate are activated immediately after an infection
process begins and is rapidly directed toward controlling the reproduction of the invading
pathogen. Containing the infectious agent serves as a delaying action until lymphocytes arrive
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
13
Vaccines, The Human Immune System,
And Immune Responses
and can begin to deal with the invader. Various types of receptors are found among the cellular
and related components involved in the innate response. Most important among the so-called
effector cells are B-type lymphocytes, macrophages and dendritic cells. They are also known as
antigen-presenting cells (APCs), and are used to carry out the innate response strategy, namely
to detect and bind with specific molecular structures present in large groups of pathogens. These
structures are referred to as pathogen-associated molecular patterns, and the receptors of the
innate immune system that interact with them are called pattern-recognition receptors. The
best-known examples of the pathogen-associated molecular patterns include the various
molecules found in bacterial cell walls and capsules (lipopolysaccharides, peptidoglycans, etc.),
bacterial DNA, and certain forms of viral nucleic acids. Pathogen-associated molecular patterns
are usually:
1) manufactured only by pathogens and not the infected host; for example,
lipopolysaccharides are only synthesized by bacteria, thus their presence alerts the
immune system to the presence of a pathogen,
2) essential for the survival or disease-causing capability of the microorganisms, and
3) invariant structures formed and found with an entire group of pathogens; for example,
all gram-negative bacteria have lipopolysaccharides, therefore detection of this
pathogen-associated molecular pattern signals the presence of virtually any gramnegative bacterial infection.
Once the pathogen-associated molecular pattern receptors on a macrophage or dendritic cells
identify a pathogen-associated molecular pattern signals the presence of infection and, in turn
induces the activation of an adaptive immune response. The adaptive immune system
responds to a pathogen only after it has been detected and recognized by the innate
immune system. Involved in this activation of the adaptive immune system are a number of
lymphocyte products such as cytokines and chemokines. Cytokines are low-molecular weight
proteins that are involved in regulating cellular activities. Chemokines are cytokines that
regulate the movement of white blood cells from the circulatory system into tissues. Generally
each type of white blood cell, eosinophil, lymphocyte, and neutrophil posses chemokine
receptors on their surfaces that guide them to specific chemokines located within body tissues.
Selected Innate Response Components
The cellular representatives used during this type of immune response include:
1. phagocytic cells such as neutrophils, monocytes , and macrophages,
2. cells that release substances involved in causing and/or regulating inflammation such
as basophils, eosinophils, and mast cells,
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
14
Vaccines, The Human Immune System,
And Immune Responses
3. dendritic cells, and
4. natural killer cells
The molecular components of innate immune responses include:
1. acute-phase proteins,
2. complement,
3. cytokines such as interleukins and the interferons.
Phagocytosis is the process by which white blood cells such as neutrophils and monocytes engulf
various types of particles, microorganisms and a variety of other cells (Figure 3). Such cells are
frequently referred to as phagocytes. After attachment to the phagocytic cell surface, the cell
extends a portion of itself in the form of a pseudopodium around the foreign particle or
microorganism and engulfs it. Once inside the phagocyte, a digestive process ensues with the
end result being the destruction of engulfed material. Bacteria and the remains of dead cells
resulting from infection commonly undergo phagocytosis. It should be noted that in certain
situations certain pathogens are not destroyed by phagocytic cells. On the contrary, pathogens
such as the meningococcus (one bacterial cause of meningitis), gonococcus (the cause of
gonorrhea), tubercle bacillus, and even the human immunodeficiency virus can use phagocytes
for 1) protection against host immune system defenses, 2) reproduction, and even 3) transport.
Monocytes that migrate to areas of infection differentiate (transform) into wandering
macrophages.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
15
Vaccines, The Human Immune System,
And Immune Responses
Figure 3. A scanning micrograph showing a phagocyte extending a portion of itself
(pseudopodium) and beginning the process of phagocytosis by attaching it to a clump of bacteria.
Macrophages are derived from blood-borne monocytes and possess receptors for carbohydrates
that are not normally exposed on human body cells. These receptors enable monocytes to
distinguish between foreign cells (those with the carbohydrates) and normal body (self) cells. In
addition, both macrophages and neutrophils have receptors on their surfaces for
immunoglobulins and a specific protein known as complement, both of which enhances
phagocytosis.
Neutrophils, eosinophils, and basophils are the white blood cells that possess different chemicalcontaining granules within their respective cytoplasms. In recent years, studies of these
granulocytes have shown them to participate in innate responses. For example, eosinophils are
known to be phagocytic in cases of worm infections and to release substances that are involved
in allergic reactions. The numbers of these granulocytes increase substantially in such situations.
Basophils also are involved in allergic and inflammatory reactions. Basophils are in some ways
similar to mast cells, another cell type that plays an important role in allergic reactions. Mast
cells are present in most tissues adjoining blood vessels. They contain numerous granules
containing chemicals such as heparin and histamine that are important participants in host
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
16
Vaccines, The Human Immune System,
And Immune Responses
cellular defense mechanisms. Neutrophils as described earlier are also phagocytic. They
respond quickly to tissue destruction caused by bacteria.
Dendritic cells which include the Langerhans’ cells in the skin are other key components of
innate immune system. These cells constantly, which quietly engulf extracellular antigens,
become activated when their pattern-recognition receptors recognize distinctive pathogenassociated molecular patterns on the surfaces of microorganisms. Activated dendritic cells
migrate to the local draining lymph node, where they present antigens to T-type lymphocytes
which serves to initiate the adaptive immune response.
Natural killer cells destroy infected and malignant cells (Figure 4). They recognize their targets
in one of two ways. One of these involves the linking of killer cells to foreign cells coated with
specific antibody molecules. The coated cells are destroyed by a process known as antibodydependent cellular cytotoxicity. The second recognition system used by and characteristic of
killer cells relies on killer-activating receptors and killer-inhibitory receptors. The killeractivating receptors recognize a number of different molecules present on the surface of all
nucleated cells, whereas the killer inhibitory receptors also recognize major-histocompatibiltycomplex (MHC) class I molecules which are also normally present on human nucleated cells.
(There are two classes of MHC protein molecules, Class I and Class II. Class 1 consists of
integral surface proteins found on all nucleated cells. This class of proteins are the antigens
involved in tissue graft rejection reactions. MHC Class 2 molecules are expressed on a
number of body cells including B lymphocytes, macrophages, monocytes, various antigenpresenting cells, and some T lymphocytes. The MHC molecules are the products of the
major histocompatibility complex which is made up of a cluster of genes important to the
recognition of foreign cell and substance and to signaling mechanisms between cells of the
immune system.)
If killer-activating receptors are engaged, a “KILL” order is issued to the natural killer cell.
However, this signal is normally stopped by an inhibitory signal sent by the killer-inhibitory
receptor caused by recognition of the MHC class I molecules. As indicated earlier MHC class I
molecules are normally found on nucleated cells, however, these molecules may not be
expressed as a result of an infection or a malignant transformation. Therefore, cells that lack
MHC class I surface molecules are considered abnormal targets and are killed by natural killer
cells. Natural killer cells kill abnormal targets by inserting the pore-forming molecules known as
perforin, into the membrane of the target cell, and subsequently injecting cell destroying
enzymes (Figure 4). Herpesvirus-infected cells and various types of cancer cells are subject to
natural killer cell actions.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
17
Vaccines, The Human Immune System,
And Immune Responses
Figure 4. A scanning electron micrograph showing the attachment of a small natural killer cell
to a much larger abnormal target cell.
Acute-phase proteins enhance resistance to infection and promote the repair of damages tissue.
Blood levels of these proteins change rapidly in response to infection, inflammation, and tissue
injury. This group of innate immune system components include C-reactive proteins (a useful
indicator, or marker of inflammation, particularly in diseases such as rheumatoid arthritis),
serum amyloid A protein, coagulation proteins, and inhibitors of enzymes such as
proteinases.
In addition to acute-phase proteins innate responses also involve complement and cytokines.
Complement consists of a series of proteins that react in a sequential manner when activated by
the presence of antigen-antibody complexes (combinations). Activation of what is frequently
called the complement cascade of events brings about the generation of a number of
immunologically active complement components and substances including inflammatory
compounds from mast cells. Certain complement components play an extremely important role
in the destruction of pathogenic bacteria and other cells considered to be targets of the immune
system.
Cytokines are an important group of immune response regulators (mediators). They function as
messengers both within the immune system and other body systems, thus forming an integrated
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
18
Vaccines, The Human Immune System,
And Immune Responses
network that is highly involved in the regulation of immune responses. The presence of a
cytokine is detected by specific cytokine receptors. In addition to serving as messengers, certain
cytokines such as the interferons that are released by virus-infected cells establish a state of virus
resistance in neighboring cells. Certain cytokines including combinations of interleukin-2 and
interferon-alpha have proved valuable in the treatment of a number of diseases including
melanomas, viral hepatitis, and acquired immune deficiency syndrome (AIDS). Chemokines
represent another group of cytokines.
Innate Immunity Dysfunction
Considering the importance of innate immunity, it is conceivable that the dysfunctioning of one
or more of its components could contribute to the establishment of certain diseases. Two general
types of permanent genetic changes (mutations) could result in such immunologic
abnormalities, namely, 1) mutations that inactivate receptors on cellular components or the
signaling molecules associated with the activation of the adaptive system, and 2) mutations that
would render such receptors or signaling molecules active with all types of cells and substances
regardless of the source. The first form of mutation would be expected to result in various types
of immunodeficiencies. The second form of mutation would trigger inflammatory reactions and
could contribute to a number of conditions having an inflammatory component such as asthma,
allergic states, arthritis, and autoimmune disorders.
The Adaptive (Acquired) Immune System
The main distinction between the innate and the adaptive immune systems lies in the mechanisms
and components used for the recognition of foreign cells and substances. The adaptive system is
organized around two classes of specialized cells, namely, T-and B-type lymphocytes. Each
lymphocyte type is equipped with a single kind of structurally unique antigen receptor. The
repertoire of such receptors in the entire population of lymphocytes is very large and extremely
diverse. The enormity and diverse nature of this repertoire increase the probability that an
individual lymphocyte will encounter and antigen that binds to its receptor, thereby triggering
activation and proliferation of a specific lymphocyte. This process known as clonal selection,
accounts for most of the basic properties of the adaptive immune system. Increasing the number
of activated lymphocytes (clonal expansion) in response to infection is an absolute requirement
for the generation of an effective immune response. Unfortunately, it takes 3 to 5 days for the
immune system to produce a sufficient number of lymphocyte clones and for the cells of such
clones to become functional. This production time situation allows more than enough time for
most pathogens to cause damage to a host.
Adaptive immune responses are generated in the lymph nodes, spleen, and mucosa-associated
lymphoid tissue such as the tonsils, adenoids, and Peyer’s patches. These areas are referred to as
secondary lymphoid tissues. Diffuse collections of lymphoid cells also are present throughout
the lung and portions of the intestinal wall.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
19
Vaccines, The Human Immune System,
And Immune Responses
(The adaptive immune system has a tremendous capacity to recognize almost any antigen, and
thus can bind to antigens regardless of their source. It should be noted that activation of the
adaptive immune system response can be harmful to a host when the antigens are self (of the
host) or environmental antigens (pollens, etc.). Immune responses to such antigens can lead to
autoimmune disorders and allergies.
Selected Acquired Response Components
The cell types of major importance to the adaptive immune system develop from stem cells
having the potential to develop in several different ways. These cells, known as T-and B-type
lymphocytes, T and B cells, respectively, arise in the bone marrow and then circulate throughout
the body’s extracellular fluid. T cells travel to the thymus to complete their development, while
B cells achieve their mature state within the bone marrow.
T and B Lymphocytes
T Lymphocytes develop in the thymus gland which is seeded during embryonic development by
lymphocyte stem cells provided by bone marrow. Immature T lymphocytes occupy the outer
cortex region of the thymus, while mature cells are found in the inner medulla area. During
maturation, a variety of identifying protein molecules (antigens) known as Cluster of
Differentiation (CD) markers are expressed on T cell membranes and result in the formation of
T lymphocyte subsets. These surface proteins are unique and serve as specific antigen receptors
that make identification of subsets possible.
Two main subsets of T lymphocytes are recognized, Th 1 and Th2. These subsets are
distinguished by the presence of cell surface markers, CD4 (CD4+) and CD8 (CD8+). As T
cells mature in the thymus, the expression of one of these molecules is lost, resulting in a
single-positive CD4 or CD8 cells. T lymphocytes expressing the CD4 marker are also
known as T helper cells, and are regarded as being the most prolific producers of
cytokines. Cytokines as indicated earlier are the protein messenger molecules responsible
for most of the biological effects in the immune system. The general properties of the T
lymphocyte subsets are as follows:
1. Th1 cells produce important cytokines such as interferon-gamma, interleukin-2, and
tumor necrosis factor-beta. These proteins are important participants in phagocytosis and
the destruction of microbial pathogens. Th1 cells also promote the development of CD8
cytotoxic cells and activate antigen-presenting macrophages.
2. Th2 cells produce cytokines such as interleukin 4 stimulate B cells to produce
antibodies and are involved in related immune and allergic responses. This CD4+
lymphocyte subset also functions as T helper cells in specific immune responses
involving antibodies and antigen recognition.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
20
Vaccines, The Human Immune System,
And Immune Responses
Many CD8+ lymphocytes act as cytotoxic T (Tc) cells in the cellular immune response. Some
other lymphocytes act as suppressor (Ts) cells, or T-regulatory cells, to suppress immune
responses.
Th1 cells play an important role in cell-mediated immunity, the direct destruction of body cells
that have been invaded by various infectious disease agents or that undergo degeneration.
Other T cell types play a significant regulatory role in the development and activation of various
types of immune responses, by either providing help to other cells capable of killing infected or
defective cells.
B Lymphocytes mature in the bone marrow and are responsible for the humoral response or
antibody (immunoglobulin) production. B cells are identified by the presence of
immunoglobulins on their surfaces. Each B cell expresses only the single specific antibody
molecule it will eventually secrete. Five different major or general classes of immunoglobulins
are known:
1. IgG-the smallest immunoglobulin,
2. IgM-the largest of the immunoglobulins,
3. IgA,
4. IgD, and
5. IgE.
A Brief Explanation Of Antibody-Mediated (Humoral) And Cell-Mediated Responses
Most antigens must be picked up, processed, and carried by means of the body’s
lymphatic system to lymphoid organs such as lymph nodes and the spleen before they are
presented to T lymphocytes in a form they can recognize. These functions are carried out by
antigen-presenting cells such as dendritic cells in the medulla area of lymph nodes and the large
phagocytic macrophages found in most tissues, the lungs, and in the linings of certain body
cavities. The anatomy of a lymph node permits various types of cells including lymphocytes,
dendritic cells to come into contact with antigens, or to communicate by means of cytokine
molecules. Both humoral (antibody) and cell-mediated immune responses develop in the
lymphoid follicles of any secondary lymphoid tissue such as lymph nodes, spleen, tonsils, and
Peyer’s patches in the intestine.
Following successful recognition of antigen on the surface of an antigen presenting cell,
a single Th (naïve) cell responds by secreting the cytokine interleukin -2 or IL-2. IL-2 signals
the Th cell which produced it to undergo cell division, thus giving rise to a number of
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
21
Vaccines, The Human Immune System,
And Immune Responses
descendants. The resulting Th cells are specific for the same antigens as the original parent cell.
In addition, IL-2 can diffuse to nearby B or CD8+ T cells that have recognized an antigen, and
deliver critical signals in the form of other cytokines which are necessary for such cells to
respond to the antigen’s presence. The presence of Th cells with the ability to secrete IL-2 in
response to antigen is essential to initiate both humoral and cell-mediated responses.
Following the initial secretion of IL-2 response to antigen, Th cells secrete additional cytokines
to further the maturation of B and/or CD8+ T cells that have bound antigen. B cells fully
develop into antibody-secreting plasma cells (PC), and CD8+ T cells become cytotoxic T
lymphocytes (CTLs) capable of killing. This process of maturing and acquiring new functions is
known as differentiation. In the case of B cells, Th cells provide help by establishing antigenspecific cell-to-cell contact, delivering both cell-surface signals and cytokines. In the case of
CD8+ T cells, no physical contact is necessary, and Th cells provide help solely through the
secretion of cytokines in the vicinity of a CD8+ T cell that has recognized an antigen on the
surface of a cell. As a result of one or the other or both of these types of interactions, humoral
and/or cellular immunity is/are generated in response to an antigen, which serve to eliminate or
lead to the destruction or other effects on an antigen or pathogen.
In addition to dealing with the antigen at the time of first exposure, antigen-specific
immune responses by Th and B lymphocytes also give rise to immunologic T- and Bmemory cells. The existence of these cells allows the immune system to mount a faster,
and much more effective response on subsequent exposures to the same antigen(s). It is
the immunologic memory in these cells which provides the protection from the same
infectious disease after initial exposure and recovery, otherwise referred to as immunity.
Both the cell-mediated and the humoral (antibody) immune responses are specifically
acquired functions of the immune system and selectively recognize, eliminate, and
remember individual antigens. These immune responses are the same as the ones that result
from immunizations. The effectiveness of vaccines is dependent on these responses.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
22
Vaccines, The Human Immune System,
And Immune Responses
CELL-MEDIATED IMMUNITY AND INFLAMATION
INFLAMMATION
Macrophages
Th1 Cell
Memory
T Cell
IL-12
Antigen
Antigen
Presenting
Cells
Naïve
Th Cell
IL-2
Helper
Memory
Cell
IL-4
Memory
B Cell
Th2 Cell
B Cell
Plasma Cell
Immunoglobulins
HUMORAL IMMUNITY
Figure 5: A general view of the cells and events involved with immune responses showing the
involvement of antigen. Explanation of abbreviations: IL, interleukin; Th, T-helper.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
23
Vaccines, The Human Immune System,
And Immune Responses
VACCINE TYPES
A
vaccine is a preparation that contains one of more antigens to which the immune system
responds. A large number of vaccines are currently available for use for immunizations
against a variety of infectious diseases. Vaccines can consist of the entire or whole
microorganism in either the killed state or an attenuated or weakened condition. Attenuated
vaccines contain specific bacteria or viruses that are living, but have lost their capability of
causing disease. One particular advantage associated with attenuated preparations is that the
microorganisms in the preparation are able to multiply for a limited period of time in the body,
thus increasing the dose available for an immune response. It is also possible for the organisms
in attenuated vaccines to serve as an immunizing dose for other individuals. Examples of
attenuated vaccines include mumps, measles, Bacilus of Calmette and Guerin, and the Sabin
polio vaccine.
Certain parts of bacteria also are used for vaccines and primarily include capsules, the outer
structures of certain bacterial species. Such bacteria include Streptococcus pneumoniae,
Hemophilus influenzae, type b, and Neisseria meningitis.
Toxins of certain bacterial species are another source for vaccines. Several bacterial species
secrete toxins capable of causing a disease state. The toxins known as exotoxins are released by
bacteria such as Clostridium botulinum (the cause of botulism), Clostridium tetani (the cause of
tetanus), and Corynebacterium diphtheriae (the cause of diphtheria). Sufficient treatment of the
exotoxins with a chemical such as formaldehyde inactivates their harmful property and makes
them effective immunizing agents against the respective toxins. Such inactivated toxins are
called toxoids.
Preparations also known as subvirion( a component a virus particle), sub-unit, or purifiedsurface-antigen vaccines are designed to contain only the parts of viruses involved in eliciting an
immune response. One current example of a successful preparation is the genetically engineered
recombinant vaccine for hepatitis B. The vaccine is prepared by the insertion of hepatitis B
virus genes into the genetic make-up of a nonpathogenic microorganism such as a yeast cell.
This technique has also been used for a rabies vaccine. In this case the genes for specific rabies
virus antigens are introduced into cowpox virus particles. .
The following section summarizes the common types of vaccines available for current use. It is
important to note that these preparations contain antigenic materials in several different forms.
They include:
1. whole or entire microorganisms either inactivated (killed), or attenuated (live but
weakened);
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
24
Vaccines, The Human Immune System,
And Immune Responses
Examples:
killed bacterial preparations - cholera, epidemic typhus fever, plague, Q-fever,
Rocky Mountain spotted fever, typhoid fever
killed viral preparations - hepatitis A, influenza, polio (Salk vaccine), rabies
attenuated bacterial preparation - tuberculosis (BCG, Bacillus of Calmette and
Guerin,), typhoid fever
attenuated viral preparations - adenovirus infections, chickenpox (varicella),
influenza, measles, mumps, polio (Sabin vaccine),
rubella, smallpox, shingles (zoster), yellow fever.
2. microbial components:
Examples:
bacterial polysaccharide capsules - meningococcal meningitis, Hemophilus
influenzae type b meningitis, pneumococcal
pneumonia, pertussis,
isolated bacterial protective antigens - anthrax.
3. toxoids (formaldehyde-inactivated bacterial exotoxins);
Examples:
botulism, diphtheria, tetanus.
4. recombinant subunit (genetically-engineered) vaccine:
Example:
hepatitis B.
5. subvirion or purified-surface-antigen:
Example:
influenza.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
25
Vaccines, The Human Immune System,
And Immune Responses
Combined or Single-Dose Vaccines. The use of combining certain vaccines into a single dose
has proved to be advantageous from several standpoints. These include avoiding multiple
injections of separate vaccines, and the overall costs associated with production and the
personnel need to administer the vaccines. Examples of combined preparations include: 1)
diphtheria-pertussis-tetanus (DPT) vaccine, 2) the newer diphtheria-tetanus-acellular pertussis
(DTaP) vaccine, 3) the measles-mumps-rubella (MMR) vaccine, and 4) trivalent oral polio
(TOP) vaccine. The trivalent valent poliovaccines come in two different forms, a live attenuated
oral polio vaccine (OPV) and an inactivated polio vaccine (IPV). Both preparations contain
representatives of the three major serotypes of polio virus.
Examples Of Routinely Used Vaccines. Table 1 lists the routinely used vaccines in the United
States and several industrialized countries.
Table 1: Routinely Used Vaccines
Diphtheria
Hepatitis A
Hepatitis B
Haemophilus influenzae, type b
Influenza
Measles (rubeola)
Meningococcal disease
Mumps
Pertussis (whooping cough)
Pneumococcal disease
Poliomyelitis (polio)
Rotavirus
Rubella
Tetanus
Varicella
Additional details concerning selected diseases, vaccines, and dosages associated with
prevention and control are presented later.
Two vaccines have recently been added to the list of available vaccines, namely, human
papilloma vaccine which is directed toward the prevention of certain strains of human papilloma
viruses known to cause genital warts, cervical cancer, and penile cancer in infected persons, and
RotaTeq, a preparation for routine use to prevent severe gastroenteritis in young children.
Routes Of Vaccine Administration
Appropriate aseptic precautions must be taken during any type of immunization procedure. The
precautions include:
1. the proper washing and drying the hands of the individual administering a vaccine,
2. the wearing of sterile disposable gloves in the handling of vaccine-associated
materials,
3. disinfecting (if appropriate) containers of immunizing materials,
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
26
Vaccines, The Human Immune System,
And Immune Responses
4. adequately sterilizing any body surface to used for immunization, and
5. the proper disposal of materials such as containers, syringes, etc.
Among the possible routes for the introduction of vaccines are the following:
1. intramuscular route,
2. subcutaneous (under the skin surface) route,
3. oral administration, and
4. aerosol administration with the aid of a nebulizer device.
Other routes of vaccine administration such as intraperitoneal, intravenous and intrathecal also
have been used on rare occasions. These routes of administration can be used to inject antibody
preparations (antisera) such as gamma globulin and related materials.
The route of vaccine administration can affect the quality of the immune response. For example,
when compared with intramuscular injecting of a vaccine, immunity is longer lasting when oral
vaccines are used against gastrointestinal infections and intranasal aerosols are administered
against respiratory infections.
Vaccine Side Effects
Vaccines in general are of significant importance and value in the prevention and control of a
number of infectious diseases. However, side effects are known to occur, and to some
individuals pose serious dangers to their well-being. Side effects have been reported ever since
Jenner introduced vaccination in 1796. Live vaccines for example can be hazardous to
individuals such as expectant women, or persons with immunodeficiencies, or receiving
immunosuppressive therapy involving drugs and/or radiation.
It is important to note that some side-reactions or-effects can be prevented. For example, before
any vaccine is administered, individuals should be questioned as to the history of any previous
reactions associated to immunizations. Obtaining such information is especially important when
immunizations involve the use of vaccines produced in eggs. Details of an individual’s health,
age, and family history are also significant. In the event a side effect does occur after the
administration of a specific vaccine or related preparation, it must be fully documented on the
individual’s health record.
Representative reactions reported to have occurred with certain vaccines include:
1. anaphylaxis ( a life-threatening allergic reaction caused by certain chemicals released
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
27
Vaccines, The Human Immune System,
And Immune Responses
by cells of the immune system and resulting in smooth muscle contractions
throughout the body, such as the lungs and intestines),
2. a body rash,
3. diarrhea,
4. soreness and reddening at the site of the injection,
5. fever,
6. encephalitis, and
7. local lymph node enlargement.
Additional aspects of side-reactions are discussed with individual vaccines in later sections.
An Example Of A Recommended Immunization Schedule
Recommended immunization schedules vary between industrialized and developing countries.
The addition of new vaccines and recommendations as to changes of doses and/or age groups to
receive a specific vaccine occur from time-to-time. Most industrialized nations use
approximately the same immunizations for specific age groups as shown in Table 2.
State or local health departments should be consulted for guidance as to the appropriate
dosage and age group to receive a vaccine.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
28
Vaccines, The Human Immune System,
And Immune Responses
Table 2. An Example Of Recommended Immunizations
Vaccine
Diphtheria and tetanus toxoids, and pertussis (DTaP)
Haemophilus influenzae, type b (Hib)
Hepatitis A a (HepA)
Hepatitis B (HepB)
Measles, Mumps, Rubella (MMR)
Polio (IPV, OPV) b
Varicella
Age Group
All children
All children
All children
All children
All children
All children
All children
Hepatitis A (Hep A)
Hepatitis B (Hep B)
Influenza
Tetanus and Diphtheria toxoids (Td)
Zoster
All adults aged 19 to 49
All adults aged 19 to 49
All adults aged 19 to 49
All adults aged 19 to 49
All adults aged 19 to 49
Diphtheria-Tetanus toxoids
Influenza
Pneumococcal polysaccharide vaccine (PPV)
All adults 50 years of age and above
All adults 50 years of age and above
All adults 50 years of age and above
Pneumococcal polysaccharide vaccine (PPV)
All adults 65 years of age and above
Hepatitis B (Hep B)
Previously unvaccinated or partially
vaccinated adolescents
Previously unvaccinated or partially
vaccinated adolescents
Previously unvaccinated or partially
vaccinated adolescents
Previously unvaccinated or partially
vaccinated adolescents
Measles, Mumps, Rubella (MMR)
Tetanus and Diphtheria toxoids (Td)
Varicella
a
Hepatitis A vaccine has been recommended for 1-year-olds by the Advisory Committee for
Immunization Practices (ACIP)
b
IPV, inactivated polio virus vaccine containing representative viral strains from 3 serotypes;
OPV, attenuated polio virus vaccine containing representative viral strains from 3 serotypes
Since no vaccine produces life-long protection against a pathogen or its products, it may be
necessary from time-to-time to activate B-and T-type memory cells in order to raise the level of
antibodies. Such preparations are referred to as booster shots.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
29
Vaccines, The Human Immune System,
And Immune Responses
States Of Immunity
The main function of the immune system is to provide protection against cells and/or substances
considered to be foreign to the body, which of course includes pathogenic microorganisms.
Special terminology is used to indicate an individual’s immune state and the type of existing
protection.
The resistance to disease possessed by individuals varies considerably because it is greatly
affected by numerous innate (genetically determined)) or acquired (adapted) factors. Innate or
native immunity as it is also called includes specific genetic factors related to species, ethnicity,
and individual resistance to infectious agents. Acquired immunity may be either natural or
artificial, depending on the processes involved in producing immunity. Immunization to an
infectious disease through the introduction of a vaccine by injection or aerosol is an artificially
produced contact with the disease agent or its products, in contrast to a natural exposure. (In
short, immunizations are the human attempts to duplicate in some manner what occurs
naturally.)
Both natural and acquired states of immunity are further subdivided into active and passive
types. In an active state, the individual manufactures immunoglobulins in response to an
immunogenic stimulus, while in the passive state, immunoglobulins are obtained through
transfer from an immunized person (an individual already having immunoglobulins). The
following descriptions provide additional details of these states of immunity:
1. naturally acquired active immunity - an individual recovering from most
infections usually manufactures immunoglobulins against the pathogen by bringing
into action T- and B- lymphocytes as described earlier. Depending on the
immunogenic nature and dosage of the infecting pathogen and related factors, the
resulting naturally acquired immune state may last for a period ranging from a few
months to several years.
Examples of diseases to which an individual can develop a naturally acquired
immunity towards include: chickenpox, mumps, influenza, polio, and typhoid
fever.
2. naturally acquired passive immunity - an individual receiving immunoglobulins
through a natural transfer mechanism has a naturally acquired immune state. Such a
transfer can occur between a mother and her fetus when certain immunoglobulins
pass from the maternal circulation through the placenta into the fetal circulation
during pregnancy. The immunoglobulins, specifically IgGs which are the smallest of
the immunoglobulins, pass through the single layer of cells making up the placenta.
Thus, an expectant mother having immunoglobulins against such diseases as polio,
diphtheria, tetanus, and measles can impart a share of these protective proteins to her
unborn child.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
30
Vaccines, The Human Immune System,
And Immune Responses
Another form of naturally acquired passive immunity also can occur during breast
feeding of a newborn via colostrum, a protein-rich fluid produced by a mother.
While the duration of naturally acquired passive immunity ranges only from a few
weeks to a few months, it is an important form of protection for newborns.
3. artificially acquired active immunity - an individual receiving any one of the
following human-made preparations that imitates and duplicates, the natural exposure
of a pathogen and/or its products, and manufacture immunoglobulins. Preparations
that are used to induce an artificially acquired active immunity include: a) killed
microorganisms, b) attenuated microorganisms, c) toxoids, d) parts of
microorganisms, and e) recombinant vaccines.
4. artificially acquired passive immunity -this form of immunity is immediate, but
only temporary, because no active immunoglobulin production toward a pathogen or
its products occurs. Artificially acquired passive immunity results from the
injection of appropriate levels of immunoglobulins. Such preparations are referred by
several terms including therapeutic serum, antisera, gamma globulin, or hyperimmune
serum. It is important to note that subsequent injections of the same preparation may
cause severe allergic reactions, including anaphylaxis and serum sickness.
The Role of Subclinical Infections. Some individuals have a fairly high level of
immunoglobulins to a pathogen, and never knowingly experienced an infection with the
pathogen, nor been given a related vaccine preparation. Such persons develop their immune
state as a consequence of an exposure to an infected person, or contaminated objects without
experiencing any specific signs or symptoms of a disease state other than a possible slight fever,
or mild rash. Repeated exposures of this kind are called subclinical infections, and can induce a
strong immunity.
EXAMPLES OF SELECTED BACTERIAL DISEASES AND ROUTINELY USED
VACCINES
T
he following section presents some of the specifics with respect to selected bacterial and
viral diseases that are vaccine-preventable. Schedules are included for only a few of
entries.
Meningococcal Meningitis
Few diseases ignite the fear that develops when bacterial meningitis strikes a community. Its
potential for communicability and fatality greatly frightens families, public health personnel and
health care workers alike. Physicians, particularly pediatricians, recognize bacterial meningitis
as a disease with potentially subtle presentation but devastating consequences if misdiagnosed.
Over the last twenty years or so, advances in understanding the pathophysiological aspects of the
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
31
Vaccines, The Human Immune System,
And Immune Responses
disease, and in vaccine development and usage not only have provided opportunities to improve
outcome but have markedly changed the demographics of bacterial meningitis.
In recent years, bacterial meningitis has dramatically changed to become a disease largely of
adults. This situation emphasizes important problem areas in the management of the disease.
These include:
1) recognition of the disease in older patients who present with fewer than the classic
signs and symptoms,
2) the increasing number of possible causative agents,
3) the prompt initiation of appropriate treatment against microorganisms with
increasing antibiotic resistance, and
4) disease prevention through the development and use of effective vaccines.
The Cause. Neisseria meningitidis, known also as meningococcus is an exclusively human
pathogen. Meningococcal disease occurs worldwide as endemic infections. Strains of the
pathogen can be distinguished from one another by using antibodies that recognize chemical
groups known as epitopes on an organism’s capsule or outer membranes. By this technique 13
serogroups are recognized. Strains such as serogroups B and C cause the majority of infections in
industrialized countries. Strains of serogroups A and to a lesser degree C are found
predominantly in third-world countries. During the 1990s, the frequency of meningococcal
disease outbreaks increased in many developed counties, with serogroup C being the most
noticeable cause, especially among teenagers and young adults. This was the observation
particularly in the United Sates and Canada. Since 1996 there have also been outbreaks caused
by serogroup Y. Although such outbreaks cause great public concern and attract considerable
media attention, they account for only 2 to 3 percent of the total number of cases in the United
States.
Transmission. Most individuals with meningococcal disease acquire their invading strain from
asymptomatic carriers. Meningococci lodge in the nose and throat of an exposed person and are
spread through face-to-face contact, which can include coughing, kissing, sharing of drinks,
food, and cigarettes, and sneezing.
Meningococcal disease occurs as both endemic and epidemic disease in most parts of the world,
with significant implications for morbidity and mortality. The worldwide incidence of
meningococcal meningitis is believed to exceed 100,000 cases on an annual basis. The disease
occurs year-round, but the majority of cases occur during the winter and early spring.
In the United States the rates of meningococcal disease are highest among infants in whom
protective antibodies have not developed. The rates drop after infancy and then increase during
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
32
Vaccines, The Human Immune System,
And Immune Responses
adolescence and early childhood. Although the rates once again after early adulthood, more
cases occur in persons 23 to 64 years old than in any other age group.
Certain world areas have special epidemiological patterns. For example, sub-Saharan Africa,
which has been designated as the meningitis belt, experiences meningococcal disease caused by
serogroup A in yearly recurrent waves. The disease attack rate rises at the end of the dry season
and declines very quickly after the beginning of the rainy season. The majority of
meningococcal disease cases in sub-Saharan African countries occur as explosive epidemics.
Small epidemics of meningitis is a worldwide problem and can affect any country.
Reservoirs. The human naso-oropharyngeal mucosa is the only natural reservoir of
meningococci. N. meningitidis can be transferred from one person to another by direct contact or
via droplets for a distance up to 1 meter away. Why certain strains of the pathogen colonize the
naso-oropharyngeal mucosa and other do not is not known and is the subject of extensive
research.
The carriage rate for N. meningitidis appears to be higher in lower socioeconomic classes
(probably because of crowding), and under conditions where people from different geographical
areas are brought together, as is the case for military recruits, prisoners, or students living in
dormitories and related facilities.
Risk Factors. A number of factors are considered to increase the risk for humans to harbor N.
meningitidis and invasive disease. These include secondhand or active smoking, stressful events
and preceding viral respiratory tract infections or infection with the bacterium Mycoplasma
pneumoniae which either change the integrity of mucosal surfaces, or affect local or systemic
immunity in some way. Moreover, the risk of invasive disease is influenced by age, the absence
of a functioning spleen, host immune defense mechanisms, and bacterial virulence factors.
Vaccines and Recommendations for Use. Routine vaccination of high-risk populations is
likely to be the most effective public health strategy for the control of meningococcal disease. In
2000, the Advisory Committee on Immunization Practice and the American Academy of
Pediatrics issued revised guidelines for the use of meningococcal vaccine. They recommend that
health care providers and colleges inform and educate freshmen, especially those living in
dormitories, and their parents about the increased risk of meningococcal disease, and the
potential benefits of immunization, so that they can make informed decisions about availing
themselves of currently approved vaccines.
N. meningitidis vaccine is available and used in cases of outbreaks of invasive disease or to
protect some travelers and longer-term visitors and residents in areas where meningococcal
disease is highly endemic. There are no recommendations for routine immunization, especially
for older-adult populations. Immunization is recommended, however, for persons who have
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
33
Vaccines, The Human Immune System,
And Immune Responses
experience prior serious N. meningitidis infections and those persons with certain immune
system defects.
A quadravalent (also referred to as a tetravalent) vaccine is currently in use. It contains the N.
meningitidis polysaccharide capsular antigens for groups A, C, Y, and W135. The vaccine is
effective in bringing about the production of antibodies in adults. It also has been successful in
eliminating epidemics among military recruits. Unfortunately the vaccine is less effective in
young children, the population at greatest risk for meningococcal disease. The group C
polysaccharide is not an effective immunogen in children under 2 years of age.
While effective vaccines are available for A and C serogroups, group B meningococci present a
problem because their capsules are composed of sialic acid, a polysaccharide that is chemically
very similar to polysaccharides found on human cell surfaces. Consequently, these bacteria
effectively escape detection by the human immune system. Thus strategies for developing
vaccines against serogroup B have focused primarily on noncapsular antigens such as the outer
membrane proteins. New serogroup B vaccines, now under development, may not be available
for some time.
The Question of Revaccination. Revaccination may be indicated for persons at high risk such
as persons living in areas in which meningococcal disease is endemic, and in particular for
children who were first vaccinated when they were less than 4 years of age. Revaccination
should be considered for such children after 2 to 3 years in the event they remain at high risk.
The need for the revaccination of older children and adults is not known. Since antibody levels
decline over a 2 to 3 year period, revaccination may be a consideration 3 to 5 years after the
initial administration of the vaccine, and especially if indications still exist.
Pertussis
The Cause. Pertussis (whooping cough) is an acute bacterial infection of the respiratory tract
caused by the gram-negative bacterium Bordetella pertussis.
Transmission. B. pertussis is transmitted from an infected individual to a susceptible one
mainly through aerosolized respiratory secretions, or by direct contact with such infectious
material.
Adolescents and adults with unrecognized or untreated pertussis contribute to reservoir of B.
pertussis in communities. Infected persons are most infectious during the catarrhal stage, the
signs and symptoms of which include nasal congestion, runny nose, mild sore throat, mild dry
cough, and minimal or no fever. This stage of the disease lasts approximately 1 to 2 weeks.
Infected individuals also are a source of the pathogen during the first 3 weeks after the onset of
the cough.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
34
Vaccines, The Human Immune System,
And Immune Responses
Pertussis is a highly infectious disease. Secondary attack rates exceed 80 percent among
susceptible persons. Unvaccinated or incompletely vaccinated infants aged less than 12 months
have the highest risk for severe and life-threatening complications and death.
Vaccines. Pertussis vaccines have been in routine pediatric use for more than 50 years, and have
dramatically decreased the incidence of whooping cough. It is important to realize that neither
vaccination nor natural infection with Bordetella pertussis induces long-lived immunity, thus
reinfections at older ages are common. Moreover, pertussis is being increasingly recognized as a
source of infection in adults who then commonly infect young children. Infants are at greatest
risk for morbidity and mortality with this disease.
Since the 1970s, the reported incidence of pertussis, especially among adolescence and adults,
has increased. Some of this increase can be credited to increased awareness, better diagnostic
methods, and improved approaches to surveillance and data gathering. Nevertheless, there are
increasing trends in the incidence of pertussis in all age groups.
Concerns about the safety of whole-cell pertussis vaccines have existed in the past. However,
safer acellular pertussis (aP) vaccines have been developed and are currently in widespread
pediatric use. These newer versions of pertussis vaccines have been evaluated in adolescents and
adults, and determined to be safe and immunogenic.
Pertussis infections in older persons are largely without signs and symptoms. The use of
pertussis immunization with an aP vaccine can confer protection for adolescents and adults
against the such hidden (asymptomatic) forms of the disease, and probably reduce its
transmission
Pneumococcal Lobar Pneumonia and Meningitis
The Diseases and the Causative Agent. In the United States and Europe, Streptococcus
pneumoniae is the leading bacterial cause of pneumonia, meningitis, and otitis media (middle ear
infection). In developing countries of the world, the burden of pneumococcal disease is even
greater. Currently there are 90 serotypes of pneumococci, which are distinguished by variations
in the polysaccharide capsule (outer structure of individual cells) of the organism; and these
serotypes are further divided into 46 serotypes. The majority of disease, however, is caused by a
handful of serotypes. The 7 serotypes included in licensed heptavalent pneumococcal protein
conjugate vaccine (PCV7) account for approximately 80 percent of cases of invasive disease in
the United States.
These serotypes also are responsible for one-half of the invasive pneumococcal disease in adults
in the United States. In Europe the 7 serotypes cause the majority of cases of pneumococcal
disease among children.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
35
Vaccines, The Human Immune System,
And Immune Responses
Transmission. Pneumococci are transmitted through droplets, oral contact with infected
persons, or indirectly through fomites freshly contaminated with respiratory discharges. Personto-person spread of the pathogens is common.
The human nasopharynx is the primary reservoir for S. pneumoniae and the main source of
person-to-person transmission. Furthermore, nasopharyngeal carriage of this pathogen is more
common in young children than adults and varies by geographic region. Variations of such
carriage may be associated with genetic differences in the host that affect the likelihood of
nasopharyngeal colonization and to socioeconomic conditions including crowding, day care
contact, family size, and sanitation. The duration of carriage also varies, depending on the host’s
age and the serotype of the colonizing pneumococcus strain, and typically ranges between 1 and
17 months.
While the factors responsible for the transition from carriage to disease remain poorly
understood, disruption of natural barriers appears to be among them. One example of such a
situation leading to invasive pneumococcal infections would be the resulting damage from
bronchial epithelium following influenza virus infection
The Pneumococcal Polysaccharide Vaccine-23 (PPV-23). Since a significant number of
bacterial meningitis cases are caused by S. pneumoniae, especially in older adults, prevention of
the disease should be a high priority. The therapeutic problems connected with penicillinresistant Streptococcus pneumoniae (PRSP) infections have renewed the interest in the
prevention of pneumococcal disease by active immunization. Studies have shown the currently
two licensed 23-valent polysaccharide pneumococcal vaccines to be about 56 to 81 percent
effective in preventing invasive forms of S. pneumoniae disease, including meningitis. The
preparations are Pneumovax, the vaccine manufactured by Merck & Company, Incorporated and
Pneu-Immune 23, manufactured by Wyeth-Ayerst Laboratories. Both contain 23 purified
capsular polysaccahride antigens of the pathogen that represent 85 to 90 percent of the serotypes
that cause invasive infections.
These polysaccharide vaccines have been found to be safe and well-tolerated. However, the
preparations are not prescribed for children younger than 2 years of age due to poor antibody
responses to the pneumococcal polysaccharides.
Current Recommendations for Use. In the United States, use of pneumococcal polysaccharide
vaccine is recommended by several governmental and professional groups, including the CDC’s
Advisory Committee on Immunization Practices (ACIP), the United States Preventive Services
Task Force, the American College of Physicians, the Infectious Diseases Society of America, the
American College of Preventive Medicine, and the American Academy of Family Physicians.
Although there are some minor differences in their respective recommendations, all of these
groups, recommend immunization for all adults 65 years of age and older, and for selected
persons less than 65 years of age. In addition, persons in the any of the risk groups for
pneumococcal disease described earlier and individuals who are unsure if they have previously
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
36
Vaccines, The Human Immune System,
And Immune Responses
received the vaccine should also be immunized. While the ACIP does not recommend routine
revaccination, it does recommend a second dose of vaccine 5 years after the first dose for
persons with asplenia, or for immunocompromised individuals.
The ACIP does not recommend multiple revaccinations largely because of insufficient
information on the protection and safety of polysaccharide vaccines as of 2001.
The Pneumococcal-Conjugate Vaccine-7 (PCV-7). A new vaccine, known as Prevnar, is a 7valent pneumococcal-conjugate preparation manufactured by Wyeth Lederle Vaccines was
approved by the Food and Drug Administration in February, 2000. The vaccine includes seven
purified capsular pneumococcal polysaccharides from serotypes 4, 6B, 9V, 18C,19F, and 23F,
each coupled (combined) with a different form of the diphtheria toxin cross-reactive material 197
(CRM 197). The Centers for Disease Control and Prevention (CDC) and other agencies,
emphasize the need for an increased use of the licensed polyvalent (heptavalent) pneumococcalconjugate vaccine.
Prevnar is estimated through vaccine trials to be 90 percent protective against the seven most
common serotypes S. pneumoniae seen in young children 6 years of age and younger. Unlike the
polysaccharide pneumococcal vaccines, the new conjugate vaccine in protective in children
under 2 years of age. This is an important feature of the preparation since 80 percent of
childhood pneumococcal disease occurs in children under 2 years of age.
Immunization Schedule. Table 3 provides an immunization schedule for the pneumococcalconjugate vaccine.
Table 3. Pneumococcal-Conjugate Immunization Schedule For Previously Unvaccinated
Infants And Children By Age At Time Of First Vaccination
Age at First Dose
2 to 6 months
7 to 11 months
12 to 23 months
24 to 59 months
Healthy children
Children with asplenia,
chronic illness, HIV
infection,
immunocompromising
conditions d
Total Number Of Doses
Schedule (in months)
a
Additional Dose
3
2
2
2 months apart
2 months apart
2 months apartc
1 dose at 12-15 monthsb
1 dose at 12-15 monthsb
none
1
2
--2 months apart
none
none
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
37
Vaccines, The Human Immune System,
And Immune Responses
a
For children immunized at less than one year of age, minimum interval between doses is 4
weeks.
b
The additional dose (booster) should be given about 8 weeks after the primary series has been
completed.
c
The minimum time interval between doses is 8 weeks.
d
These recommendations do not include children having undergone a bone marrow transplant.
Side Effects. The most common side effect reported for the vaccine is the appearance of redness
and/or soreness at the injection site. The reaction is generally mild and occurs in about 10 to 30
percent of vaccine recipients. A low-grade fever has been reported to occur in some cases, but it
usually disappears within one day.
EXAMPLES OF SELECTED VIRAL DISEASES AND ROUTINELY USED VACCINES
Hepatitis A Infection
H
epatitis A infection is an important public health problem, and occurs worldwide with
both sporadic and epidemic outbreaks. Clearly overcrowding and poor sanitation often
lead to epidemics in developing countries. In the United States hepatitis A continues to
be one of the most frequently reported vaccine-preventable diseases, despite the licensing of
hepatitis A vaccine in 1995.
In the United States, cyclic increases in the occurrence of hepatitis A infections have appeared
about every ten years. In addition, infections continue to occur at relatively high rates between
epidemics. HAV infection is a reportable disease in almost all countries.
The Cause. Hepatitis A is the result of an infection with a 27-nanometer ribonucleic acid
(RNA)-containing virus. This pathogen, hepatitis A virus (HAV) is classified as a picornavirus,
and is known to cause either asymptomatic or symptomatic human infections. Hepatitis A virus
has been placed into the genus Hepatovirus and is currently the only member of this genus.
However, the genus contains four genetically different strains of hepatitis A, as I, II, III, and IV.
Transmission. In infected individuals, HAV replicates (multiplies) in the liver, is excreted in
bile, and is shed in stools. Peak infectivity of infected persons occurs during the 2-week period
before the onset of jaundice (yellowing of body tissues) or the elevation of liver enzymes as
determined by laboratory tests. Virus concentration is highest in stool specimens during this
time.
The major means of HAV transmission is through the fecal-oral route from person-to-person.
Such transmission occurs most frequently among close contacts, especially in household and
extended family settings. Children with asymptomatic or unrecognized infections play a key role
in HAV transmission and serve as a source of infection for others. Outbreaks of HAV infection
are reported from time-to-time resulting from household or sexual contact with infected persons.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
38
Vaccines, The Human Immune System,
And Immune Responses
Cyclic outbreaks also have occurred among users of injection and non-injection drugs and
among men who have sex with men.
Groups at Risk. Persons in groups shown to be at high risk for HAV infection include: 1)
travelers to countries with high or intermediate rates of hepatitis A, 2) men who have sex with
men, 3) injecting - drug users, 4) persons with blood clotting-factor disorders, 5) persons with
chronic liver disease, and 6) children living in communities with high rates of disease.
Individuals from developed or industrialized countries traveling to developing countries are at a
substantial risk for acquiring HAV infection. The risk varies with the region visited and length
of stay, and may even be present among travelers and others who take measures to protect
themselves against enteric infection or stay only in luxury hotels or in urban areas.
HAV Vaccines. Screening of individuals that are to receive a HAV vaccine should be screened
for not only for the presence of antibodies, but also for the concentration (titer) of HAV
antibodies. Considerable differences exist in recommendations for the serologic screening
(determining the presence and level of antibody) before vaccination. The aim of this procedure
is to reduce the cost of vaccination by eliminating those individuals with previous natural
infection.
HAV vaccines are available in two formulations, namely the HAVRIX (GlaxoSmithKline
Biologicals, Rixensart, Belgium) and VAQTA (Merck & Company, Inc., Whitehouse Station
Jersey) preparations. Both of these vaccines contain formaldehyde-inactivated hepatitis A virus
grown in specific human cell cultures. The dosages for the HAVRIX vaccine are given in
dosage terms enzyme - linked immunosorbent assay units (EL.U), while those for the VAQTA
vaccine are given in dosage terms of units (U). Both vaccines have been shown to be well
tolerated, and to be immunogenic.
HAV vaccines should be given intramuscularly into the deltoid muscle, with needle lengths
appropriate for the recipient’s age and size. Table 2 shows the recommended dosages.
Hepatitis B
Although human immunodeficiency virus (HIV) is the infection people fear most, the hepatitis B
virus (HBV) is both more common and more easily transmitted. The Centers for Disease
Control and Prevention (CDC) estimates that about 250,000 - 300,000 Americans become
infected with HBV every year. Among them are about 10,000 health care workers, most of
whom are infected because of an injury from a hypodermic needle, or other sharp object, in the
work place. HBV is a well recognized occupational risk for health care personnel. The risk of
HBV infection for such individuals is primarily related to the degree of contact with blood in the
work place and also to the status of the specific hepatitis B e antigen (HBeAg). The HBeAg is
an indicator (marker) of infectivity, and blood and/or related body fluids containing it are highly
infectious.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
39
Vaccines, The Human Immune System,
And Immune Responses
The first recorded epidemic of probable HBV infection was among shipyard workers following
immunization against smallpox with a vaccine developed from material obtained from humans.
During World War II, a HBV outbreak was again traced to a vaccine contaminated with human
serum, hence the disease was given the designation of “serum hepatitis”. However, the specific
cause of the disease continued to elude investigators until 1964, when B.S. Blumberg discovered
a new antigen in the blood of an Australian aborigine. This antigen, named Au for Australia,
was very rare in some populations such as those in the United States, but common in certain
tropical and Asian populations. In testing various human blood specimens, Blumberg and his
associates found Au more common in persons who had received transfusions and in children
with Down Syndrome. A clue as to the relationship of the Au antigen and serum hepatitis was
found when one of these children not only converted from Au - antigen negative to Au - positive,
but also had hepatitis. This discovery led to the testing of large numbers of stored blood
specimens from mentally disadvantaged children for Au - antigen and corresponding antibody.
Au - antigen was found to be present only during hepatitis. Subsequently Au - antigen became
known as the surface antigen, (HBsAg) of HBV, and its presence served as an indication of the
infectivity of a hepatitis patient’s blood.
The Cause. The cause of hepatitis B infection is a complex, 42 nanometer (nm) double-shelled
virus. The outer surface of the virus, or envelope, contains the HBV surface antigen (HBsAg)
and surrounds a 27 nm inner core antigen, (HbcAg). HBsAg is produced in excess amounts, and
appears circulating in blood as 22nm spherical and tubular particles. A HBV antigen (HBcAg) is
also found in the core of the virus. The e antigen appears when high concentrations of HBV
particles are present and serves to indicate a high degree of infectivity. The genetic material
(genome) of HBV consists of a double - stranded DNA molecule.
Transmission. For many years it was thought that HBV infection occurred only by injection or
infusion of contaminated blood or blood products; however, transmission has been found to be
possible by other means as well. This includes parenteral routes such as tattooing, acupuncture,
ear piercing, shaving, manicuring, illicit drug injections, accidental needle sticks, hemodialysis,
finger-stick devices, and transfusion of contaminated blood or blood products. In the United
States transmission of HBV by the transfusion of blood or blood products is rare because of
routine testing of blood for the HBV surface antigen (HBsAg), and because of current blood
donor selection procedures. Nevertheless HBV is considered as a blood-borne pathogen spread
by permucosal (e.g. sexual) exposure to infectious blood or body fluids
As indicated above transmission by close contact with contaminated body secretions (fluids) also
occurs. Examples of body fluids in which HBV surface antigens (HBsAg) may be found include
ascitic fluid, cerebrospinal fluid, saliva, semen, sweat, tears, and urine. Infection by
contaminated secretions occurs in a variety of ways, from children exchanging toys
contaminated with oral secretions, to contact with urine from infected dialysis and renal
transplant patients, to sexual intercourse. HBV circulates in high concentrations in blood and
lower concentrations in other body fluids. The virus is approximately 100 times more infectious
than HIV and 10 times more infectious than HCV.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
40
Vaccines, The Human Immune System,
And Immune Responses
Unprotected sex is the predominant mode of HBV transmission among adults and adolescents,
accounting for more than half of newly acquired infections. According to studies of reported
cases of acute hepatitis B conducted by S.T. Goldstein and associates, 40 percent of heterosexual
infections were the result of exposure to an infected partner or multiple partners, and 15 percent
were the result of exposure in cases involving men having sex with men (MSM). In addition, 14
percent of persons with acute hepatitis B reported injection drug use.
A variable proportion of persons infected with HBV will become chronically infected with the
virus. Such HBV carriers are central to virus transmission. A carrier is a person who is found
to be either HBsAg - positive for two blood tests conducted at least 6 months apart, or who is
HBsAg- positive, and negative for IgM anti-HBc antibody when a single blood specimen is
tested. Any person positive for HBsAg is potentially infectious. The likelihood of becoming
chronically infected with HBV varies inversely with the age at which infection occurs. HBV
transmitted from HBsAg - positive mothers to their newborns results in HBV carriage for up to
90 percent of infants. Between 25 and 50 percent of children infected before 5 years of age
become carriers, whereas only 6 - 10 percent of acutely infected adults become carriers. HBV
carriers have a risk of developing primary liver cancer that is 12 - 300 times higher than that of
other persons. An estimated 4,000 persons die each year from hepatitis B - related cirrhosis, and
more than 800 die from hepatitis B - related liver cancer. Women who are pregnant and who are
chronic HBV carriers or have acute HBV infection in the third trimester can transmit the virus to
their infants. Infection probably occurs during birth by contact with contaminated vaginal
secretions or shortly after birth via breast milk. Infection is more likely if the mother is HBeAg positive.
Vaccines. Since 1981, safe, immunogenic, and effective hepatitis vaccines have been
commercially available. Two types of hepatitis B vaccines are currently licensed in the United
States. One of these products is a plasma-derived preparation consisting of an inactivated
suspension of 22 - nm, HBsAg particles that have been purified from human plasma. The
commercial treatment steps have been shown to inactivate all classes of viruses found in human
blood, including HIV. The plasma-derived vaccine is no longer being produced in the United
States, and is now limited to hemodialysis patients, other immunocompromised hosts, and
persons with a known allergy to yeast.
Another type vaccine is a genetically engineered product and is referred to as a recombinant
vaccine. It is produced by common baker’s yeast (Saccharomyces cerevisiae) into which the
gene for the HBsAg has been inserted. Purified HBsAg is obtained by disrupting the yeast cells
and separating HBsAg from yeast parts by biochemical and biophysical procedures.
Recombinant vaccines undergo various inactivation steps, are highly purified, and mixed with
chemical ingredients such as aluminum phosphate or aluminum hydroxide to increase their
immunogenic effectiveness. Thimerosal is used as a preservative. The inactivation process used
is designed to inactivate all living blood-borne organisms previously known to infect humans.
The licensed vaccines in use are, Engerix B, Heptavax B, and Recombivax B. On March 28,
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
41
Vaccines, The Human Immune System,
And Immune Responses
2000 FDA approval was obtained for a thimerosal-free vaccine for pediatric use. A
Haemophilus influenzae, type b and hepatitis B combined vaccine also is available.
Twinrix (GlaxoSmithKline Biologicals), a new preparation combining hepatitis A
inactivated and hepatitis B recombinant vaccines is currently available for the active
immunization of individuals 18 years of age or older. This combination vaccine is
contraindicated for persons who are allergic to yeast or any other component of the new
vaccine.
The need for booster doses of hepatitis B vaccine after a primary inoculation series has been the
subject of considerable debate. Currently, vaccine advisory groups in the United States do not
recommend routine booster doses of hepatitis B vaccine in persons who have responded to
vaccination. Ongoing studies should provide information on the need for booster doses during
the second decade after vaccination.
Vaccine Recommendations In Cases of Perinatal Hepatitis B. Several groups including the
CDC, the Advisory Committee on Immunization Practices, and the American Academy of
Family Physicians, have issued recommendations for the immunoprophylaxis of infants born to
mothers whose HBsAG status is positive or unknown at the time of delivery. These are
summarized in the following table.
Table 4. Perinatal Hepatitis B Vaccine Recommendations
Immunization Preparations a
Mother’s HbsAg
Status
HBIG
Infant born to
HBsAg positive
mother
Infant born to
mother with
unknown HBsAg
statusc
Less than 2000 g
premature infant
born to HBsAg
mother
Less than 2000 g
premature infant
born to mother
with unknown
HBsAg status
Hep B Vaccine
Dose #2
1-2 months of age
Hep B Vaccine
Dose # 3
6 months of ageb
Hep B Vaccine
Dose #4
n/a
within 7 days within 12 hrs
of birth
of birth
1-2 months of age
6 months of age
n/a
within 12 hrs
of birth
within 12 hrs
of birthd
1 month of age
2 months of age
6 months of
ageb
within 12 hrs
of birthe
within 12 hrs
of birthc,e
1 month of age
2 months of age
6 months of age
within 12 hrs
of birth
Hep B Vaccine
Dose #1
within 12 hrs
of birth
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
42
Vaccines, The Human Immune System,
And Immune Responses
a
Explanation of abbreviations: HBIG, hepatitis B immune globulin; Hep, hepatitis; b Serologic
testing for HBsAg and anti-HBs is recommended at 9 to 15 months of infant’ age after the
completion of the hepatitis B vaccine series; c The mother should be tested during hospital stay;
d
This initial hep B vaccine dose does not count towards completion of hep B vaccine series, 3
additional doses of the vaccine should be given starting when the infant is 1 month of age;
e
immunoprophylaxis with hep B vaccine with HBIG must be given to these infants within 12
hours after birth unless the mother’s HBsAG test results is available in less than 12 hours after
the birth of her infant.
Recommended Doses. Table 5 lists the recommended doses of currently licensed HB vaccines.
The usual schedule for the plasma-derived vaccine (Heptavax-B) and the two recombinant
vaccines Engerix - B and Recombivax HB involves a total of three doses, given at 0,1, and 6
months. It is important to note that special formulations and different injection and dose
schedules are recommended for dialysis patients and immunocompromised patients. In addition,
persons with a known yeast allergy should only be given Heptavax - B.
Table 5. Recommended Doses of Currently Licensed HB Vaccines
Group
Hepatavax-B Dose
(ug) (ml)
Infants of HBV- carrier mothers
10 (0.5)
Other infants and children
10 (0.5)
<11 years
Children and adolescents
20 (1.0)
11 - 19 years
Adults >19 years
20 (1.0)
Dialysis patients and other
40 (2.0)
immunocompromised persons
Vaccine
Engerix-B Dose Recombivax HB Dose
(ug) (ml)
(ug) (ml)
10 (0.5)
5 (0.5)
10 (0.5)
2.5 (0.25)
20
(1.0)
5
(0.5)
20 (1.0)
40 (2.0)
10
40
(1.0)
(1.0)
Side Effects. Soreness at the injection site has been the most common side effect reported
following vaccination with each of the available vaccines. Early concerns about the safety of the
plasma derived vaccine have proven to be unfounded. This has been especially true with respect
to possible contamination of the vaccines with pathogens such as HIV from the donor plasma
pools. The recommended series of three intramuscular doses of hepatitis B vaccine induces a
protective antibody responses in more than 90 percent of healthy adults younger than 40 years.
After age 40, the cumulative age-specific decline in immunogenicity drops below 90 percent,
and by age 60 only 75 percent of individuals develop protective levels of anti-HBs. In infants
born to HBeAg- positive mothers, combined treatment with either plasma or recombinant
vaccines and HBIG is 79 to 98 effective in preventing chronic HBV infection.
Passive Immunization. Passively acquired anti-HBs (antibodies against HBV) can protect
individuals from developing acute clinical hepatitis B and chronic HBV infection if given soon
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
43
Vaccines, The Human Immune System,
And Immune Responses
after exposure (preferably within 24 hours). The preparation used in such situations is a high
immunoglobulin concentration called anti-HBs (HBIG). It is prepared by a commercial
fractionation procedure from serum containing high concentrations of anti-HBs and is
standardized to 100,000 International Units (IU) of anti-HBs/ ml. The use of HBIG is
recommended as a postexposure, prophylactic measure in situations such as the following:
1. Perinatal exposure for an infant born to an HBsAg- positive mother,
2. Percutaneous or mucous membrane exposure to HBsAg - positive blood,
3. Sexual exposure to a HBs - Ag - positive person,
4. For the protection of patients from severe recurrent HBV infection following liver
transplantation.
When hepatitis B vaccine is indicated, it should be administered simultaneously with HBIG at a
separate body location.
Influenza
Few viruses have played a more central role in the historical development of virology than that
of influenza. The pandemic that swept the world in 1918, just as the Great War (World War I)
ended, killed more people than the war itself. In some of the more recent severe epidemics in the
United States, influenza viruses attacked over 25 percent of the population and killed over
40,000 individuals.
While epidemics can occur at any time, but usually do not spread unless conditions or
environments exist for large numbers of person-to-person transmission to take place. Schools in
session present an excellent example.
The Cause-Influenza Virus Types. The first influenza virus was isolated by E. Centanni and
associates in 1901 from chickens with the disease known as fowl plague. This virus was later
recognized in 1955 as an influenza virus A by W. Schafer. (This virus is now classified as
H7N7. The importance of this designation is discussed in a later section). In 1931 R.E. Shope
isolated the swine influenza virus. This discovery was of great significance because veterinarians
of that era believed that influenza was transmitted to swine during the 1918 pandemic.
The first influenza B virus was isolated by T. Francis, Jr. in 1940, while the first influenza C
virus was discovered some seven years later in 1947 by R. Taylor.
Epidemics of influenza A occur yearly and coincide with the peak occurrence of acute
respiratory illnesses that cause individuals to seek medical care, while those caused by
influenza B somewhat more sporadically. New antigenic strains of influenza A are spread
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
44
Vaccines, The Human Immune System,
And Immune Responses
with such speed through susceptible populations that an epidemic may run its course in a
major city within two or three months. Up to 70 percent of the population may become
infected before the epidemic burns itself out. The situation is not helped by the fact that
many of the infected individuals are neither sick enough nor thoughtful enough to remove
themselves from contact with others.
Transmission. The transmission of influenza viruses is direct, by infectious droplet nuclei, or
indirect by hand transfer of contaminated nasal or conjunctival secretions. Small-particle
aerosols generated by sneezing, coughing, and even speaking serve as the main transmission
vehicles. Transmission is most likely at the onsets of signs and symptom of the disease, when
infected individuals shed large amounts of infectious virus in respiratory secretions. Influenza
virions remain infectious in small droplets, particularly in cold temperatures and in environments
with low humidity. The ability of the virus to survive under such conditions may partly explain
the winter occurrence of influenza epidemics.
Maximum communicability of influenza occurs 1 to 2 days before the onset of the disease to 4 to
5 days thereafter. There is no carrier state.
Groups At Risk. High risk individuals for influenza include persons with chronic health
conditions such as anemia, asthma, cardiovascular disease, pulmonary diseases, metabolic
diseases such as diabetes, renal dysfunction, and immunosuppression. Healthy persons over the
age of 65 years are considered as moderate risks for an influenza attack. Health-care personnel
with close patient contact and activity are also vulnerable.
Any situation that allows daily mixing of large numbers of susceptible individuals will increase
the risk of influenza virus infection. Such high-risk groups include children in day care or
boarding schools, college students, military recruits, and residents of nursing homes. No special
susceptibility has been reported for any ethnic group or for either gender.
Vaccines. A major problem in the development and provision of highly functional immunizing
agents for influenza prevention is the antigenic changes (mutations) that occur with influenza
viruses.
Current vaccine preparations are trivalent (also referred to as being multivalent) and contain
inactivated purified virions of influenza virus strains specified by the Centers for Disease Control
and Prevention (CDC) in the Spring of each year. For example, the vaccine preparation used
during the 1994-1995 influenza season contained the following three influenza virus strains:
1. A/Texas/36/91 (H1N1),
2. A/Shangdong/9/93 (H3N2),
3. B/Panama/45/90
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
45
Vaccines, The Human Immune System,
And Immune Responses
Inactivated influenza vaccines are standardized typically to contain hemagglutinins from two
type A and one type B strains. (On the basis of their respective nucleoprotein content,
influenza viruses are grouped into the major classes A, B, or C). T he Food and Drug
Administration (FDA) must also approve any vaccine used for immunization purposes.
Influenza vaccines are about 80 percent effective. However, the effectiveness is variable since it
depends on the immune response of individuals and on how closely the vaccine strains resemble
the influenza virus strains circulating within the population.
The influenza vaccines available in the United States contain either inactivated or live, weakened
(attenuated) influenza virus (LAIV). Two types of inactivated preparations are available, namely
whole-virus and disrupted or split-virus vaccines. Whole-virus vaccines are prepared using
embryonated hen eggs. Split vaccines have fewer side effects and are most useful in children 12
years of age or younger, in whom whole-cell vaccines have side-effects.
Inactivated vaccines should be given by the intramuscular route.
The live, attenuated influenza virus vaccine is intended only for intranasal administration and
should not be given by intramuscular, intradermal, or intravenous routes. The intranasal use of
this vaccine can be accomplished by holding an individual sprayer device in the palm of the hand
until thawed, and followed by the immediate administration of its contents.
Other types of vaccines are under study or being clinically tested. Such preparations include
attenuated vaccines. With the great concern of an avian influenza worldwide epidemic
(pandemic), vaccines are under study also, and may be available by 2007.
Annual immunization with the currently available influenza vaccine is considered an effective
preventative measure. The killed vaccine must be given yearly because antibody response is
short-lived and because of the yearly antigenic variation in the circulating strains of influenza
viruses within the population. Immunization is most effective when it precedes influenza virus
exposure by no more than 2 to 4 months.
Persons Who Should Not Be Given LAIV. As with a number of other vaccine preparations
certain groups of individuals should not receive LAIV. These include:
1. persons aged less than 5 years or older than 50 years,
2. persons with asthma, reactive airways disease or other chronic disorders involving the
cardiovascular or pulmonary systems,
3. persons with underlying medical conditions such as diabetes, renal dysfunction, or
some form of immunodeficiency,
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
46
Vaccines, The Human Immune System,
And Immune Responses
4. children or adolescents receiving aspirin or other salicylates,
5. persons with a history of Guillain-Barre syndrome,
6. pregnant women, persons with a history of hypersensitivity to eggs, or to any other
component of LAIV,
7. persons who have close contact with severely immunosuppressed individuals.
LAIV may be used for the immunization of healthy, nonpregnant persons aged from 5 to 49
years of age. Health care personnel who are not among the groups of individuals who should not
be given this type of vaccine also are eligible candidates.
Polio
The term polio is a shortened version of poliomyelitis, a word derived from the Greek “polios”
for gray and myelon for matter. Gray matter refers to the nerve tissue of the spinal cord and
brain attacked by polio viruses. Many years ago when the major group of victims were children
the disease was called infantile paralysis.
The Cause. Polio is caused by a small ribonucleic virus belonging to the family Picornaviridae.
Transmission. Polio is usually acquired through the consumption of contaminated food or
water. Infecting viruses multiply in the tonsils first and then attack other lymphoid tissues of the
gastrointestinal tract, causing cramps, nausea, and vomiting. Spreading from this area to other
body sites can result in meningitis, and paralysis of body limbs and the brain.
The Vaccines. Two vaccine preparations are available for the prevention and control of
poliomyelitis. These are a live attenuated oral vaccine (OPV) and an inactivated (killed virus)
polio vaccine (IPV). Both preparations contain one strain from each of the known polio virus
serotypes.
The oral vaccine reduces a gastrointestinal infection that induces a long-lasting immunity and
has the added advantage of immunizing individuals in close contact with the vaccine recipient.
This last effect is known as herd immunity.
The inactivated vaccine is recommended for primary immunization of those persons with
impaired immunity, and the oral vaccine is only recommended for booster immunizations.
The World Health Organization has listed polio as one of the diseases to be eradicated from the
planet Earth in much the same way as smallpox was eliminated through immunization.
Unfortunately, wild poliovirus (type 1) has interfered with this intention during the period from
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
47
Vaccines, The Human Immune System,
And Immune Responses
2003 to 2004. This natural form of the virus was imported into eight previously polio-free
African countries. Attempts to meet the World Health Organization’s goal by interrupting polio
virus transmission through immunization and increased surveillance are ongoing. A new
vaccine, a monovalent polio preparation against only type 1, has been developed to root out the
virus in parts of Africa where it is most entrenched such as overcrowded slums, with extremely
poor sanitation and booming birthrates.
Varicella-Zoster
Varicella-zoster virus (HZV) is a herpes virus, and related to a degree to the viruses known to
cause fever blisters, and genital herpes. The Varicella-zoster virus causes two distinct diseases:
chickenpox (varicella) and shingles (zoster). These diseases, which occur throughout the world,
were thought to be unrelated for a long time. Historically, Von Bakay first suggested the
relationship between the causes of varicella and herpes zoster in 1892, from the observation that
young children often develop chickenpox after exposure to an adult with shingles. Today,
chickenpox generally is considered to be the initial disease, while shingles results from the
activation of HZV infection that has survived in an inactive or latent form following an attack of
chickenpox. Shingles is a highly painful infection. Certain adults who have had the disease
compare the painful experience to such events as giving birth and a heart attack.
The Cause. The infectious nature of chickenpox was shown in 1875 by Steiner, who produced
the disease in volunteers inoculated with vesicular fluid from infected patients. While shingles
was described in pre-medieval times, it was not distinguished from another virus-caused disease,
smallpox until the end of the 19th century. The two viral diseases were frequently confused with
one another. In 1943, J. Garland suggested that shingles resulted from the activation of a latent
varicella virus much like the situation with the herpes simplex viruses.
Varicella virus was isolated and cultured in vitro in 1952 by T.H. Weller and B.D. Stoddard.
This achievement was of major importance to M. Takahashi and his colleagues who were able to
grow the virus and produce a live, attenuated strain for use as an appropriate vaccine.
Transmission. Chickenpox is primarily a disease of childhood. It is acquired through inhalation
of respiratory secretions containing VZV, or through direct contact with the lesions of infected
persons. VZV probably enters via the upper respiratory tract, the throat, the inner lining of the
eye, or, less likely the skin.
Varicella infection also may occur in newborns as a consequence of acquiring the virus either
during the pregnancy period or at birth if the mother is experiencing an acute attack shortly
before or during labor. A varicella-complicated pregnancy is referred to as congenital varicella
syndrome.
Viral replication occurs at the site of infection, with subsequent cycles of reproduction involving
neighboring cells. The virus spreads to the local lymphoid tissue and then through the
bloodstream to a number of target organs, including the skin, liver, lungs, and brain.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
48
Vaccines, The Human Immune System,
And Immune Responses
Shingles develops when the host defense mechanisms weaken below the level needed to keep the
latent virus in-check. Various studies indicate that age-related changes in cellular immunity
levels correlated with the increasing risk of infection in the later decades of life. In a like
manner, impaired cellular immunity is believed to increase the risk of shingles at any age in
individuals who have certain types of cancer such as Hodgkin’s disease and lymphatic leukemia,
experienced severe body injury, received metal drugs (especially those containing lead and
arsenic), or who are immunosuppressed. It should be noted that an individual with shingles is
infectious and can be the source of a varicella outbreak among susceptible persons. The
transmission mechanism is probably similar to that for chickenpox.
The Vaccines. In 1974, M. Takahashi and his associates developed an attenuated
Oka-varicella-strain vaccine. After finding it to be effective in high-risk children, the vaccine
was approved in both Japan in 1986, and in Korea in 1992. About one million children received
the preparation in these two countries.
In 1980, a major study was undertaken to determine if the Oka-strain vaccine was protective as
well as safe for high-risk children. With positive findings in-hand the study was expanded to
include children and adults with normal functioning immune systems. Because of these studies
the Federal Drug Administration approved the attenuated vaccine Varivax (VARIVAX) in 1995
for general use. Merck Research Laboratories, Merck & Co., Inc. located at West Point,
Pennsylvania produces the vaccine. While the vaccine is not recommended for children under 1
year of age, a single injection is recommended for children between the ages of 1 and 12 and
who have no history of chickenpox. Two doses of the vaccine given 4 to 8 weeks apart are
currently recommended for individuals over 12 years of age.
Immunizing the elderly with the Oka-strain vaccine to prevent shingles is now possible with an
attenuated vaccine manufactured by Merck Research Laboratories. The preparation is known as
Zostavax also contains the Oka-strain.
Adverse Reactions. According to data collected by the Vaccine Adverse Event Reporting
System (VAERS), the most frequently reported consequence was rash. Thirty-seven cases were
reported per 100,000 vaccine doses distributed. Further investigation showed that the adverse
reaction was the result of infections with the wild or naturally occurring virus and not the
attenuated strain used in the vaccine. Other adverse reactions reported by VAERS and the
vaccine manufacturer includes, encephalitis, defective muscular coordination, seizures,
pneumonia, and a reduction in platelet numbers.
The Use of Varicella-Zoster Immunoglobulin. Passive immunization with varicella-zoster
immune globulin (VZIG) is recommended for immunocompromised persons expose to VZV,
near-term expectant mothers, and newborns of mothers who contract varicella shortly before or
soon after delivery.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
49
Vaccines, The Human Immune System,
And Immune Responses
The use of VZIG has certain drawbacks including the need for its administration within 96 hours
of exposure and its cost. These factors together with well-documented reports of protection
failures with VZIG have prompted attempts to use acyclovir as post-exposure prophylaxis either
alone or with the administration of VZIG.
EXAMPLES OF NON-ROUTINELY USED VACCINES
Anthrax
A
nthrax is primarily a disease of cattle, sheep, goats and horses (a zoonosis). It can also
occur in birds, guinea pigs, mice, and other animals.
The Cause. The cause agent of anthrax is the bacterium Bacillus anthracis. The heat-and
chemical resistant structures of this microorganism, known as spores can be found in soil and on
plants, where they may remain viable and capable of causing disease for decades. Animals
become infected via the gastrointestinal tract by eating contaminated food products or
cutaneously by some type of penetrating inoculation into the skin or hide. Anthrax usually ends
with a rapidly acting septicemia, sometimes just a few hours after the first symptoms appear.
Urine, feces, and eventually the blood and body remains of the infected animal contain B.
anthracis that re-contaminate the surrounding environment.
Transmission. Human infections result from contact with contaminated animals or animal
products such as hides, wool, bone, or hair. Although moderately resistant to anthrax compared
to plant eating animals, humans are still susceptible to the disease in industrial and non-industrial
settings. While there have been no known cases of human-to-human transmission, a few cases
of laboratory-acquired infections have been reported.
Humans become infected through the skin by contact with contaminated animal products or by
inhaling Bacillus anthracis spores.
Human Anthrax Vaccine. The standard anthrax vaccine used in the United States was
developed during the 1950’s and 1960’s. It was approved by the Food and Drug Administration
in 1970, and primarily given to persons at risk for exposure to anthrax spores which would
include veterinarians and livestock handlers. The vaccine is an aluminum-hydroxideprecipitated (AVA) preparation of protective antigens from an attenuated, non-capsulated B.
anthracis Sterne stain. Currently the vaccine is manufactured by one company, the Bioport
Corporation, and existing supplies are being used to immunize all military personnel.
The Immunization Schedule. The AVA is administered subcutaneously in 0.5ml doses. The
first three inoculations are given at 0, 2, and 4 weeks. Three additional inoculations are
administered at 6, 12, and 18 months. Booster shots are given on an annual basis. Individuals
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
50
Vaccines, The Human Immune System,
And Immune Responses
undergoing antibiotic prophylaxis in cases of suspected exposure can be given the vaccine
concurrently.
Side Effects. Reactions to the vaccine generally have been mild with only 0.2 percent of
immunized persons showing systemic reactions. Table 6 lists the general types of reactions.
There have been no long-term side effects reported.
Table 6. Reactions to Anthrax Vaccine
Reaction Type
Mild local
Moderate local
Severe local
Systemic
Signs and Symptoms
redness, minor swelling and
tenderness at site of injection
redness, minor swelling and
tenderness at site of injection and
forearm
low grade fever, swelling at site of
injection and forearm
Rarely occurs, flu-like symptoms
Percentage of persons affected
30.0
4.0
Less than 1.0
0.2
Rabies
Some of the earliest accounts of rabies appeared thousands of years ago in the writings from
Mesopotamia and Egypt. The term “rabies” is derived from the Sanskrit word “rabhas” and from
the Greek words “lyssa” or “lytta.” These terms mean “rage or to do violence or madness, and
describe the classic clinical accounts of what is known as furious (encephalitic) rabies in
humans. Quite obviously rabies is an ancient disease that remains a modern problem in much of
the developing world and in various industrialized countries.
The Cause. Rabies is caused by number of different strains of highly nervous system
destructive viruses. Most belong to a single serotype in the genus Lyssavirus. The virus particle
(virion) is bullet-shaped, and contains ribonucleic acid, a single that is enclosed in a double
layered envelope with spike-like projections.
Transmission. The important source of the rabies virus is the saliva of infected animals. A
wide range of mammals are susceptible to rabies virus infection. These include dogs, cats, bats,
skunks, and raccoons. Dogs remain the primary reservoir in developing countries. During the
21st century, bats have accounted for the majority of human rabies cases in the United States and
California.
Humans acquire rabies usually through the bite of a rabid animal. The rabies virus cannot
penetrate intact skin. Rabies has also been contracted from transplanted solid organs and a
vascular graft from donors with rabies. Infections via broken skin and mucous membranes such
as those lining the eyelids, is possible as well.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
51
Vaccines, The Human Immune System,
And Immune Responses
Transmission of the rabies virus by aerosol has been reported. The resulting infections were
associated with individuals collecting bat waste materials in caves.
It should also be noted that human-to-human transmission of rabies is possible, although quite
rare.
Vaccines. Three human rabies vaccines are currently available in the United States. These are
the human diploid-cell rabies vaccine, purified chick embryo cell culture vaccine, and the rabies
vaccine absorbed. Human rabies immune globulin is also available for passive immunization
purposes.
Three different situations may require the use of the rabies vaccine. These are as follows:
Pre-exposure. The rabies vaccine generally is recommended for individuals considered to be
high risk for exposure. Such individuals include veterinarians, animal handlers, laboratory
workers involved with the diagnosis of the disease, and wildlife officers. The procedure here
consists of 3 intramuscular injections of rabies vaccine.
Exposure. Individuals bitten by a rabid animal are given 5 intramuscular injections of the newer
rabies vaccine. The arm is used for these injections. The procedure followed with the older
versions of rabies vaccine required painful, daily subcutaneous injections along the abdomen,
and unfortunately produced severe side effects.
Post-Exposure. The post-exposure approach to the prevention of rabies consists of 1 injection
of rabies immune globulin (RIG) and 5 injections of a rabies vaccine over a 28-day period. RIG
is obtained from blood donors who were given rabies vaccine. This preparation can also be
injected into the site of injury in order to reduce the amount of rabies virus that is able to enter
nerve cells and start the infection process.
Smallpox
The term smallpox was initially used to distinguish this viral disease from the “great
pox” which was observed on individuals infected with syphilis. Two basic forms of smallpox
are recognized: variola major, a highly virulent form, and variola minor or alastrim, a less
dangerous variety.
As mentioned earlier Dr. Edward Jenner introduced vaccination using vaccinia (cowpox) virus
instead of the virus of smallpox some years later. As a result of widespread vaccination,
smallpox cases declined steadily in Europe and North America.
Jenner’s epoch-making advance not only protected countless millions of persons from the
disease but also provided the example used by L. Pasteur and others to develop other vaccines
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
52
Vaccines, The Human Immune System,
And Immune Responses
that would reduce and potentially eliminate other infectious diseases. Unfortunately, death from
the smallpox continued elsewhere in the world.
The Cause. Smallpox virus is representative of the poxviruses, a group of pathogenic agents
that can infect both humans and lower animals. The group is widely distributed in nature and
nearly every type of animal is susceptible to infection by some kind of poxvirus. Diseases such
as cowpox (vaccinia), monkeypox, camelpox, rabbitpox, racoonpox, tanapox, mousepox, and
buffalopox are caused by poxviruses. The viruses causing these diseases are all members of the
genus Orthopoxvirus. Infection by a poxvirus typically results in the formation of vesicular
(blister-like) lesions. Such lesions may be localized or may be part of a generalized rash, as in
the case of smallpox.
Poxviruses are classified into the family of Poxviridiae, which are the largest group of animal
viruses known.
Transmission. Smallpox is spread from person-to-person, primarily by respiratory tract
secretions. Even though smallpox virus is considered to be highly contagious, spread is slow,
and the probability of infection from a single exposure is considered to be low.
Initially smallpox virus is spread by droplet secretions from upper respiratory tract lesions or by
contaminated inanimate objects (fomites) such as drinking or eating utensils. Oropharyngeal
secretions, however, are the main source of contaminating the face, body, clothes and other
bedding of the infected individuals. Direct face-to-face contact with an infected person via
infectious droplets and physical contact with such an individual or contaminated articles are
usually responsible for the transmission of smallpox. Later in the infection cycle, skin lesions
including vesicles, pustules, and crusts may become a source of virus. Airborne spread of
variola virus is unusual, but can occur. Although any smallpox-infected individual is potentially
contagious, the most dangerous transmitters of smallpox are persons with unrecognized disease.
Such individuals can be easily overlooked or perhaps misdiagnosed, and can introduce smallpox
into populations free of the disease.
The Vaccine. Attenuated vaccinia virus is used for immunization (Figure 6). This virus in its
present form is different from both the original cowpox, and smallpox virus. (Cowpox, which is
found only in Britain and Western Europe, is a rare disease; its causative agent is isolated from
cattle and farm workers dealing with these animals).
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
53
Vaccines, The Human Immune System,
And Immune Responses
Figure 6. An electron micrograph showing a number of vaccinia virus particles originally
magnified 75, 000X.
The smallpox vaccines last used in the United States, known as DryVax, were mainly glycerine
containing fluid (lymph) obtained from vesicles on the infected skins of calves or sheep. In
addition, vaccines derived from infected embryonated eggs, and cell culture-grown vaccines
were also available. Currently, the CDC has sufficient DryVax in storage to inoculate several
million individuals in the event of an emergency. More vaccine is being prepared to provide
protect for over 20 million persons.
Vaccines Under Development. Various groups of scientists are searching for alternative forms
of smallpox vaccine in efforts to reduce or eliminate side-effects. One group at the U.S. Army
Medical Research Institute of Infectious Disease in Fort Detrick, Maryland, developed a vaccine
composed of the genes for four vaccinia virus proteins that were thought to be important in
producing immunity to smallpox. The vaccine, which represents a deoxyribose acid (DNA)
approach and is referred to as 4pox shows promise, but as yet has not been found to be as
effective as the DryVax preparation.
A derivative of the DryVax vaccine known as the modified vaccinia Ankara (MVA) is also
under study and in development. This vaccine is produced by passing a vaccina virus
preparation 574 times in chicken embryo tissue cells. The MVA was widely used in Germany in
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
54
Vaccines, The Human Immune System,
And Immune Responses
the 1970s and has a much better safety record than DryVax. The U.S. National Institute of
Allergy and Infectious Diseases plans to purchase more than 50 million doses of MVA, which
should be enough to vaccinate those individuals in the United States who can’t take the DryVax
vaccine.
Route of Administration. The method of vaccine administration has changed since the times of
Drs. Jenner and Waterhouse. In 1967 the jet (pressurized air) injector was introduced at the start
of the WHO global eradication program. At approximately the same time in 1966 Wyeth
Laboratories in Philadelphia Pennsylvania developed a highly efficient immunizing device,
which was adopted later in 1968. The device consists of a bifurcated needle that can be used to
apply the multiple pressure technique described below.
Vaccination has been generally performed by the multiple pressure technique using the Wyeth
bifurcated needle. After cleansing the skin (upper arm or thigh areas) with acetone, ether, soap
and water, or other suitable disinfecting agent, and allowing the site to dry completely, 1 drop of
the vaccine is placed on the skin. The side of the bifurcated needle is then pressed firmly (at
least 5 times) through the vaccine drop into the superficial skin layers. The point of the needle
should draw no blood. Excess vaccine is then removed from the skin with a sterile dry gauze
pad and the needle disposed of appropriately. No dressing is applied to the inoculation site. As
the risk of acquiring smallpox in the United States became essentially zero in the late 1960s,
routine vaccination of children was discontinued in 1971. The routine vaccination of health care
personnel, military personnel, and travelers was likewise discontinued a short time later.
However, in view of the current possible use of smallpox virus as a bioterrorist weapon may
reverse the practice of routine immunization against smallpox.
Responses to Smallpox Vaccination
Three types of responses are known to occur with smallpox vaccination. These are referred to
primary vaccination site reactions, which develop in previously unvaccinated individuals, and
accelerated and immediate reactions in persons undergoing revaccination. (It should be noted
that smallpox vaccination does not provide life-long protection. In general, immunity lasts for
about ten years. The major or primary reactions generally develop during a three week period
following primary vaccination or in cases the revaccination of individuals after a prolonged time
period between vaccinations.
Complications. Although vaccination is relatively safe, rare but occasionally complications
affecting the skin or central nervous system have occurred, especially with initial vaccinations.
Table 7 lists these complications together with brief descriptions.
When the United States government started vaccinating civilians and military personnel using
the DryVax vaccine in 2003, a small number of recipients developed a heart inflammation,
which dampened enthusiasm for the ambitious national campaign.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
55
Vaccines, The Human Immune System,
And Immune Responses
Table 7. Possible Complications with Smallpox
Complication
eczema vaccinatum
generalized vaccinia
erythrematous urticaria
vaccinia gangrenosa
postvaccinal encephalitis
Brief Description
Usually results from extensive secondary spread of vaccinia virus
on existing skin diseases such as eczema or diaper rash.
Viremia (virus in the blood stream) develops in individuals with
some form of immunological defect or deficiency. The condition
can progress and be fatal.
A more frequent and less serious form of generalized vaccinia. The
condition appears to be related to an allergic reaction. Other
features include the absence of a viremia, skin vesicles and virus in
other skin lesions.
Progressive spread of a primary vaccination response resulting in
extensive tissue destruction (necrosis) of skin and muscle. Usually
develops in individuals unable to develop cellular immunity.
A serious and often fatal form of central nervous system disease
resulting in the destruction of myelin sheaths of nerves.
With the exception of post-vaccinial encephalitis, all complications are caused by the escape of
virus from the inoculation site. The most common side effect results from the accidental transfer
of virus to other areas on the body of the vaccinee or his or her close contacts. Less often,
internal viral spread produces generalized vaccinia, in which additional pocks appear on
scattered locations during the first two weeks following vaccination. The number of pocks tends
to be small, and they usually resolve quickly without scarring. This finding suggests that the
number and size of the lesions are limited by the development of immune responses of the
vaccinee.
Immunity. Vaccination against smallpox does not reliably confer lifelong protection against the
disease. Even previously vaccinated persons should be considered susceptible to smallpox.
The Current Picture of Smallpox. With the passage of time the majority of countries
discontinued vaccination, although special groups of individuals such as those working with the
virus or at risk of exposure may still be immunized. In addition, global efforts were made to
restrict storage of all remaining stocks to only two WHO Collaborating Centers. Such Centers
were the CDC in Atlanta, Georgia and the Research Institute of Viral Preparations in Moscow,
formerly in the Union of Soviet Socialist Republics (USSR), which is now Russia.
Vaccines in Development
Developing an effective vaccine is no small challenge. Considering the large numbers of
diseases posing significant threats to the well being of humans, at lease 20 or more vaccines are
needed. The current wish list includes vaccines for diseases that take a heavy toll of human lives
each year and includes malaria, HIV, and tuberculosis. Table 8 lists a number of vaccines that
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
56
Vaccines, The Human Immune System,
And Immune Responses
are under development and in several cases being clinically tested.
Table 8. Vaccines Currently in Development and Associated Disease States
Vaccine
Chlamydia
Cytomegalovirus (CMV)
Ebola virus
Group B streptococci
Helicobacter pylori
Hepatitis C and E
Herpes simplex virus (HSV)
Human immunodeficiency Virus (HIV)
Malaria
Plague
Respiratory syncytial virus
Examples of Associated Disease States
various bacterial sexual transmitted diseases
retinitis, newborn abnormalities, transplantation abnormalities
virus hemorrhagic fever
septic shock, kidney infections, encephalitis
peptic ulcers, gastric carcinoma
viral acute and chronic forms of hepatitis
fever blisters, and sexually transmitted herpes type 2
acquired immune deficiency syndrome (AIDS)
malaria, and complications
Plague
respiratory infection in newborns and older children
CONCLUDING COMMENTS
U
nfortunately, society has traditionally preferred to pay for treating a disease rather than
preventing it. Many people are prepared to spend a fair amount of money per year on a
drug after contracting a disease, but will balk at spending a lesser amount to prevent
contracting the disease. The development of vaccines for prevention of infectious diseases has
revolutionized the approach to public health. In many countries individuals enjoy better health
because of effective immunization programs which have lowered the morbidity and mortality of
certain infectious diseases. Unfortunately, a number of infectious diseases continue to cause
significant morbidity and mortality despite the availability of effective vaccines for the
prevention of such diseases. If the potential of vaccines is to be realized, society needs to change
that thinking. There clearly needs to be sufficient support for the development and effective
dispensing of preventative measures such as vaccines.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
57
Vaccines, The Human Immune System,
And Immune Responses
GLOSSARY
capsule:
a surface layer found surrounding the cells of certain bacterial species; this
structure interferes with phagocytosis
CD antigen: refers to a system of cell-surface antigens that are classified according to
the cluster of differentiation, in which individual molecules are assigned a CD
number on the basis of their reactivity with specific (monoclonal) antibodies
chemokines: cellular protein products that regulate the movement of white blood cells
from the circulatory system into tissues
clone:
a group of genetically identical cells with a common ancestor
cytokines:
a large group of low-molecular weight proteins involved with regulating
cellular activity; particularly associated with the immune system
endemic:
chronic, low-level presence of a disease, or disease-causing agents in a defined
area
epidemic:
an infectious disease or condition that attacks many individuals at the same time
in the same geographical area
epitope:
any component of an antigen that functions to stimulate antibody formation by
allowing attachment to certain antibodies
helper T cell: a T-type lymphocyte (that usually possess CD4) that secretes the various
cytokines required fro the functional activity of other cells of the immune system
IgG:
one of the five classes of immunoglobulins, the other being IgM, IgA, IgD, and
IgE; IgG is the smallest of the immunoglobulins.
Immunologic
memory:
the ability of the immune system to recall contact with a specific antigen and to
mount a quantitatively and qualitatively secondary response on re-contact with
the original stimulating antigen
immunogen: any substance that stimulates antibody formation
immunogenic: refers to substances that stimulate an immune response
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
58
Vaccines, The Human Immune System,
And Immune Responses
natural
antibody:
antibody that occurs naturally without apparent antigenic stimulation from a
pathogen or immunization
natural killer
(NK) cell:
a cellular component of the innate immune system that recognizes and
subsequently kills abnormal cells that lack cell-surface major histocompatibilitycomplex class I molecules
serogroup:
subtype of a particular species of microorganism detectable with the use of
specific antibodies against a particular protein or polysaccharide component
serotype:
subtype of species detectable with specific antibodies (antisera)
Type 1 (Th1)
helper cell: T-type lymphocyte that is chiefly involved in cell-mediated immunity, which
includes the activation of macrophages and cytotoxic T cells; secretes the
cytokines interleukin-2 and interferon-gamma, but does not secrete interleukins 4,
5,or 6; inhibits type-2 helper T-cells
Type 2 (Th2)
helper cell: T-type lymphocyte that is chiefly involved in the production of immunoglobulins;
secretes interleukins –4-5,6 and 10, but not interleukin-2 or interferon-gamma;
inhibits type 1 helper T-cells
virulence:
relative degree of disease causing capability of a pathogen
viremia:
the presence of viruses in the circulatory system
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
59
Vaccines, The Human Immune System,
And Immune Responses
SUGGESTED READING AND REFERENCES
Purdy, K.W. et al., “Evaluation of Strategies For Use of Acellular Pertussis Vaccine In
Adolescents and Adults: A Cost-Benefit Analysis.” Clinical Infectious Disease. 2004; 38:2028.
Tanaka, M. et al., “Trends in Pertussis Among Infants In the United States, 1980-1999.” Journal
of American Medical Association. 2003; 290:2968-2975.
Van Effelterre, T.P., et al., “ A Mathematical Model of Hepatitis A Transmission in the United
States Indicates Value of Universal Childhood Immunization.” Clinical Infectious Disease.
2006; 43:158-164.
Ward, J. I., et al., “ Bordetella Pertussis Infections in Vaccinated and Unvaccinated Adolescents
and Adults, as Assessed in a National Perspective Randomized Acellular Pertussis Vaccine Trial
(APERT),” Clinical Infectious Disease. 2006; 43:151-157.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
60
Vaccines, The Human Immune System,
And Immune Responses
POST TEST
DIRECTIONS: IF COURSE WAS MAILED TO YOU, CIRCLE THE MOST CORRECT
ANSWERS ON THE ANSWER SHEET PROVIDED AND RETURN TO: RCECS, 16781
VAN BUREN BLVD, SUITE B, RIVERSIDE, CA 92504-5798 OR FAX TO: (951) 789-8861.
IF YOU ELECTED ONLINE DELIVERY, COMPLETE THE TEST ONLINE – PLEASE
DO NOT MAIL OR FAX BACK.
1. Which of the following diseases have been eradicated from the planet through
immunization?
a.
b.
c.
d.
e.
influenza
hepatitis A
pertussis
smallpox
herpes
2. Immunogens occur as soluble proteins in blood serum or other body secretions, and react in
some manner with the antigen that provoked their formation and production.
a. True
b. False
3. Which of the following choices IS NOT a characteristic property of pathogen-associated
molecular patterns?
a.
b.
c.
d.
e.
manufactured only by pathogens
manufactured only by the infected host
essential for the survival or disease-causing capability of the microorganisms
invariant structures formed and found with an entire group of pathogens
not manufactured by the infected host
4. The adaptive immune system responds to a pathogen only after it has been detected and
recognized by the innate immune system.
a. true
b. false
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
61
Vaccines, The Human Immune System,
And Immune Responses
5. Macrophages are derived from which of the following cell types?
a.
b.
c.
d.
e.
neutrophils
eosinophils
monocytes
T-type lymphoytes
None of these
6. Which one of the following cell types is not an antigen-presenting cell?
a.
b.
c.
d.
e.
dendritic cell
macrophage
B-type lymphocyte
natural killer cell
choices a and b only
7. Which one of the following choices is an innate immune system component that serves as a
useful indicator or marker of inflammation particularly in diseases such as rheumatoid
arthritis?
a.
b.
c.
d.
e.
dendritic cell
complement
C-reactive proteins
cytokines
natural killer cells
8. Which of the following cell types is directly responsible for the production of antibodies
(humoral immunity)?
a.
b.
c.
d.
e.
Th1 cell
dendritic cell
natural killer cell
B cell
Th 2 cell
9. Which of the following cell types is chiefly involved in the destruction of virus-infected cells
(cell-mediated immunity)?
a.
b.
c.
d.
e.
Th1 cell
dendritic cell
natural killer cell
B cell
Th 2 cell
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
62
Vaccines, The Human Immune System,
And Immune Responses
10. Which of the following cell types allows the immune system to mount a faster, and much
more effective response on subsequent exposures to the same antigen(s)?
a.
b.
c.
d.
e.
Th 2 cells
macrophages
natural killer cells
immunologic T- and B-memory cells
plasma cells.
11. Which of the following vaccines an example of an attenuated virus preparation?
a.
b.
c.
d.
e.
Salk polio vaccine
a Pertussis vaccine
tetanus toxoid
pneumococcal pneumonia vaccine
chickenpox (varicella) vaccine
12. Which of the following preparations consists of killed whole viruses?
a.
b.
c.
d.
e.
bacillus of Calmette and Guerin
Sabin polio vaccine
Salk polio vaccine
diphtheria toxoid
measles vaccine
13. Which of the following preparations consists of a formaldehyde-inactivated bacterial
exotoxin?
a.
b.
c.
d.
e.
anthrax vaccine
measles vaccine
tetanus toxoid
pneumococcal pneumonia vaccine
meningococcal meningitis vaccine
14. Which of the following vaccines is not an example of a combined or single-dose
preparation?
a.
b.
c.
d.
e.
DPT
DTaP
MMR
TOP
BCG
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
63
Vaccines, The Human Immune System,
And Immune Responses
15. An attenuated preparation such as the mumps vaccine contains which of the following?
a.
b.
c.
d.
e.
a toxoid
an exotoxin
a killed virus
a weakened virus generally incapable of causing mumps
a weakened virus incapable of causing polio
16. In which of the following immune states does the individual manufacture immunoglobulins?
a.
b.
c.
d.
e.
natural acquired passive immunity
artificially acquired passive immunity
any and all passive states of immunity
both naturally acquired active immunity and artificially acquired immunity
all of the above
17. Which of the following preparations will provide an individual with a passive form of
immunity?
a.
b.
c.
d.
e.
a toxoid injection
immunization with a killed preparation of polio
injection of gamma globulin
injection of a combined vaccine
immunization with BCG
18. Which of the following immunoglobulins are known to pass through the placenta from a
mother to her fetus and thus provide some degree of immunity against certain pathogens?
a.
b.
c.
d.
e.
IgA
IgG
IgM
IgD
IgE
19. The transmission of which of the following infectious diseases IS NOT acquired through the
inhalation of the pathogenic microorganism?
a.
b.
c.
d.
e.
hepatitis A
meningococcal meningitis
pneumococcal pneumonia
anthrax
chickenpox
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
64
Vaccines, The Human Immune System,
And Immune Responses
20. Which of the following is the only natural reservoir of meningococcus?
a.
b.
c.
d.
e.
cats
dogs
plants
humans
birds
21. Meningococci can be generally transferred from one person to another by which of the
following means?
a.
b.
c.
d.
e.
blood transfusion
food
flies
direct contact or nasal droplets
fomites
22. Which of the following vaccines is heptavalent, conjugated with diphtheria toxin crossreacting material, and provides protection against pneumococcal infection for children
under 2 years of age?
a.
b.
c.
d.
e.
Prevnar
Pneu-Immune
Hib
Pneumovax
None of these
23. Which of the following serve as the major source of rabies virus in an infection?
a.
b.
c.
d.
e.
saliva of infected animals
fecal matter of infected animals
fomites
flies
bird droppings
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
65
Vaccines, The Human Immune System,
And Immune Responses
24. An individual belonging to which of the following groups is a likely candidate to receive
live, attenuated, influenza vaccine?
a. persons aged less than 5 years or older than 50 years
b. a healthy, nonpregnant person aged 5 to 49 years
c. a person with asthma, reactive airways disease or other chronic disorders
involving the cardiovascular or pulmonary systems
d. a person with underlying medical conditions such as diabetes, renal
dysfunction, or some form of immunodeficiency
e. children or adolescents receiving aspirin or other salicylates
25. Which of the following methods is used to administer the smallpox vaccine?
a.
b.
c.
d.
intramuscular injection
intravenous injection
introduction of the vaccine material subcutaneously
the introduction of the vaccine material by means of a multiple pressure
technique using the Wyeth bifurcated needle
e. either choices a or b
GW: Test Version A
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
66
Vaccines, The Human Immune System,
And Immune Responses
ANSWER SHEET
NAME____________________________________ STATE LIC #_______________________
ADDRESS_________________________________ AARC# (if applic.)___________________
DIRECTIONS: (REFER TO THE TEXT IF NECESSARY – PASSING SCORE FOR CE
CREDIT IS 70%). IF COURSE WAS MAILED TO YOU, CIRCLE THE MOST CORRECT
ANSWERS AND RETURN TO: RCECS, 16781 VAN BUREN BLVD, SUITE B,
RIVERSIDE, CA 92504-5798 OR FAX TO: (951) 789-8861. IF YOU ELECTED ONLINE
DELIVERY, COMPLETE THE TEST ONLINE – PLEASE DO NOT MAIL OR FAX BACK.
1.
a b c d e
16. a b c d e
2.
a b
17. a b c d e
3.
a b c d e
18. a b c d e
4.
a b
19. a b c d e
5.
a b c d e
20. a b c d e
6.
a b c d e
21. a b c d e
7.
a b c d e
22. a b c d e
8.
a b c d e
23. a b c d e
9.
a b c d e
24. a b c d e
10. a b c d e
25. a b c d e
11. a b c d e
12. a b c d e
13. a b c d e
14. a b c d e
15. a b c d e
GW: Test Version A
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
67
Vaccines, The Human Immune System,
And Immune Responses
EVALUATION FORM
NAME:____________________________________________ DATE:______________
AARC # (if applic.)________________________ STATE LICENSE #:______________
RC Educational Consulting Services, Inc. wishes to provide our clients with the highest quality
CE materials possible. Your honest feedback helps us to continually improve our courses and
meet CE regulations in many states. Please complete this form and return/submit it with your
answer sheet. Thank you.
YES
NO
Were the objectives of the course met?
Was the material clear and understandable?
Was the material well-organized?
Was the material relevant to your job?
Did you learn something new?
Was the material interesting?
Were the illustrations, if any, helpful?
Would you recommend this course to a friend?
What was the most valuable portion of the material?
________________________________________________________________________
What was the least valuable portion of the material?
________________________________________________________________________
Suggestions for future courses: ______________________________________________
Comments: ______________________________________________________________
What is your specialty area?______________________________ Credentials?________
How did you hear about RCECS?____________________________________________
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
68