Week 12 Treatment
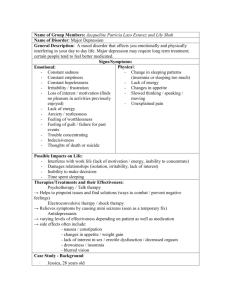
advertisement
TREATMENT OF PSYCHOLOGICAL DISORDERS WEEK 12: JULY 29, 2015 OUTLINE Historical treatments Behavioural Cognitive Medical Prevention Evaluating effectiveness HISTORICAL TREATMENT METHODS the teachings of the Roman Catholic ter the decline of on preceded the eek writings, the hoice for possessuade evil spirits bitable. Methods ng a cross at the im. If the victim yet more persuaNo doubt, recipivil would vacate earning, art, and ead throughout sidered the trane fear of witches re especially bad of massive persed of witchcraft. s with the devil, crops. In 1484, Exorcism. This medieval woodcut illustrates the practice of exorcism, which was used to expel the evil spirits that were believed to have possessed people. n s n r n e e s e t . e Introduction and Methods of Research BEDLAM 13 REFORMS IN TREATMENT This chair was designed to have a calming effect on people with mania. Other Reforms in Treatment § Seeing the “insane” as ill instead of “possessed” § Trea2ng them with tenderness, not harshness § Housing them in hospitals rather than locking them up in asylums § Developing psychotherapeu2c treatments, medica2ons, and community supports to allow life outside hospitals The unchaining of inmates at La Bicêtre by 18th-century French reformer Philippe Pinel. Continuing the work of Jean-Baptiste Pussin, Pinel stopped harsh practices, such as bleeding and purging, and moved inmates from darkened dungeons to sunny, airy rooms. Pinel also took the time to converse with inmates, in the belief that understanding and concern would help restore them to normal functioning. Current Forms of Therapy Psychotherapy: an interactive experience with a trained professional, working on understanding and changing behavior, thinking, relationships, and emotions Biomedical therapy: the use of medications and other procedures acting directly on the body to reduce the symptoms of mental disorders Medica2ons and psychotherapy can be used together, and may help the each other achieve be?er reduc2on in symptoms. GOALS OF TREATMENT Reduction of suffering Maximize independent functioning Provide/teach skills BEHAVIOURAL THERAPY 17-10 • Therapy that applies principles of classical and operant conditioning to help people change selfdefeating or problematic behaviours BEHAVIOURAL TECHNIQUES 1. Exposure Graduated exposure (Systematic desensitization): method where a person suffering from a phobia or panic attacks is gradually taken into the feared situation or exposed to a traumatic memory until the fear subsides • Attempt to counteract tendency to avoid feared object/situation 17-11 • BEHAVIOURAL TECHNIQUES 2. Exposure Flooding: a form of exposure treatment in which the client is taken directly into the feared situation until his or her anxiety subsides 17-12 • BEHAVIOURAL TECHNIQUES 3. Behavioural self-monitoring • • A method of keeping careful data on the frequency and consequences of the behaviour to be changed Identify situation in which behaviour takes place, and the reinforcers that keep it recurring Change by removing situational cues and reinforcers 17-13 • BEHAVIOURAL TECHNIQUES 4. Skills training • An effort to teach the client skills the he or she may lack, as well as new constructive behaviours to replace self-defeating ones Includes: • Modelling • Role-playing • Operant conditioning 17-14 • BEHAVIOURAL TECHNIQUES 5. Skills training Token economy 17-15 • Behavior modifica2on based on operant condi2oning principles that rewards desired behaviors • Pa2ent exchanges a token of some sort, earned for exhibi2ng the desired behavior, for various privileges or treats COGNITIVE THERAPY • Form of therapy designed to identify and change irrational, unproductive ways of thinking and, hence, to reduce negative emotions • Teaches people new, more adaptive ways of thinking. COGNITIVE THERAPIES • Identify irrational assumptions and biases • Examine evidence (reality-test) • Consider other interpretations for other people’s behaviour 17-17 • Reward for replacing irrational assumptions with realistic beliefs ROLE-PLAYING EXERCISE Volunteer(s) play the role of someone who is suffering from depression speak with a depressive explanatory style Class play the role of therapist offer challenges to unrealistic assumptions underlying this pattern of thinking DEPRESSIVE EXPLANATORY STYLE Problema2c event: Assump2ons about the problem The problem is: The problem is: The problem is: Mood/result that goes along with these views: E.G. PROCRASTINATION Failure to accept limitations leads to impossible standards (rather than rational responses) 17-20 Many procrastinators are perfectionists (if you can’t do it perfectly, then don’t do it at all) BIOMEDICAL TREATMENTS Drug treatments Direct brain interventions TRANQUILIZERS Drugs commonly prescribed for treatment of anxiety Increases activity of gamma aminobutyric acid (GABA) Not for long term use, and does not treat underlying cause, only symptoms 17-22 E.g. Valium, Xanax ANTIDEPRESSANTS Drugs used primarily in the treatment of mood disorders, especially depression & anxiety Produce unpleasant physical reactions: dry mouth, headache, constipation, nausea, gastrointestinal problems, weight gain, decreased sexual desire Three classes of antidepressants: 17-23 • Monoamine oxidase inhibitors (MAOIs) • Tricyclic antidepressants • Selective serotonin reuptake inhibitors (SSRIs) ANTIPSYCHOTIC DRUGS Used in treatment of schizophrenia & other psychotic disorders (also prescribed for severe depression, impulsivity, dementia, bipolar disorder) Reduces the sensitivity of dopamine brain Reduces agitation, delusions, and hallucinations Does not provide relief from jumbled thoughts, difficulties with concentration, emotional flatness 17-24 Side effects such as muscular rigidity, tremors, and involuntary muscle movements (tardive dyskinesia) LITHIUM 17-25 • Treatment for bipolar disorder • Moderates norepinephrine & stops overstimulation from glutamate • Side effects include muscle tremors, kidney damage 17-26 DRUG TREATMENTS CAUTIONS ABOUT DRUG TREATMENTS The placebo effect • Positive effects due to expectations about the effect of the drug • Approx 50% depressed patients respond to antidepressants; 40% of the responsive patients are actually responding to the drug 17-27 High relapse and dropout rates • Approx 50% to 70% of patients put on medication stop taking them, and relapse, often due to negative side effects CAUTIONS ABOUT DRUG TREATMENTS Dosage problems (therapeutic window) • Appropriate amount that alleviates symptoms, but not toxic • The same dose of a drug may be metabolized differently in men and women, old people and young people, and different ethnic groups. Unknown long-term risks DIRECT BRAIN INTERVENTION Psychosurgery 17-29 • Any surgical procedure that destroys selected areas of the brain believed to be involved in emotional disorders or violent, impulsive behaviour (e.g., prefrontal lobotomy) • Last resort treatment for OCD and epilepsy • No controlled studies to assess effectiveness ELECTROCONVULSIVE THERAPY (ECT) • Electroconvulsive therapy [ECT] induces a mild seizure that disrupts severe depression for some people. • This might allow neural re-­‐wiring, and might boost neurogenesis. REPEATED TRANSCRANIAL MAGNETIC STIMULATION Another opJon is repeated deep-­‐ brain sJmulaJon using implanted electrodes. Like ECT, these techniques may disrupt depressive electrochemical brain pa?erns. BIOLOGICAL & CBT TREATMENTS OF DEPRESSION PET scans indicate that both medical and therapeutic interventions are influencing the brain, but perhaps in different ways & regions 17-32 Mood regulation PREVENTION: LIFESTYLE CHANGES 20-30 minutes of moderate exercise (walking, gardening, moving stuff) • reduces onset of depression • promotes better emotion regulation abilities in response to stress • decreases duration of feelings of anxiety • reduces risk of dementia • reduces symptoms of ADHD in children (comparable to drugs) EVALUATING THERAPY How do we know if it works? Randomized controlled trials = gold standard for evaluation 17-34 • People with a given problem or disorder are randomly assigned to one or more treatment groups or to a control group; designed to evaluate effectiveness of new medication or form of therapy EVALUATING THERAPY Critical Incident Stress Debriefing (CISD) used as an intervention immediately following disasters to decrease rates of PTSD 17-35 Found that highly emotional reactions to incidents + CISD showed higher stress symptoms WHEN THERAPY HARMS Risks to clients increase under these conditions: 17-36 1. The use of empirically unsupported, potentially dangerous techniques (e.g., rebirthing, recovered memory therapies) 2. Prejudice or cultural ignorance on the part of the therapist 3. Inappropriate or coercive influence, which can create new problems for the client 17-37 PROBLEMATIC TECHNIQUES 17-38 FACTORS IN SUCCESSFUL THERAPY