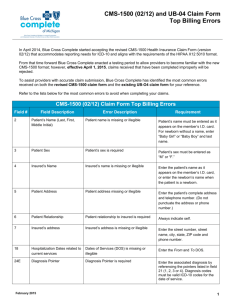
Additional Paper CMS-1500 and UB-04 Field
advertisement

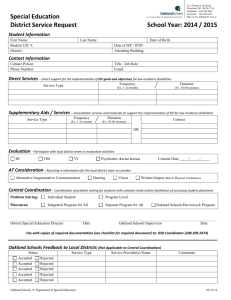
April 3, 2013 -Additional Paper CMS-1500 and UB-04 Field RequirementsDear Keystone Mercy Provider and Billing Staff: Keystone Mercy is adopting the required HIPAA 5010 X12 electronic claims submission format for both the CMS-1500 and UB-04 paper claim forms. Effective with claims received on July 1, 2013, paper claims that do not meet HIPAA 5010 X12 compliancy will be rejected. Keystone Mercy must convert paper claims data into electronic claim information. All electronic healthcare transactions are to be transmitted in compliance with standards set forth by The Health Insurance Portability and Accountability Act (HIPAA) and the United States Department of Health and Human Services (HHS). In addition, the federal mandate requires health plans, clearinghouses and providers to use new standards when electronically submitting information. Therefore, we are implementing this billing requirement to align the conversion of paper claims to the mandated 5010 837 formats. Please see the attached grids for both the CMS-1500 and UB-04 additional required fields and billing guidelines that will make all provider claims submitted to Keystone Mercy compliant with the 5010 837 Federal mandate. Claims can be submitted now with these additional fields, but please note that effective with claims received on July 1, 2013, additional data elements for the 837 format will be required fields on all paper claims and will be rejected if missing. If you have any questions, please contact Keystone Mercy Provider Services at 1-800-521-6007 or your Provider Account Executive. Sincerely, Paul L. Staudenmeier Director, Provider Network Management CMS-1500 Required Fields CMS 1500 Field # Field/Data Element Required Rejection Billing Guidance 2 Patient Name "Member name is missing or illegible" Claims wil be rejected if the first and/or last name are missing or illegible. SAME or SAME AS INSURED is acceptable and will not reject. 3 Patient Birth Date "Member DOB is missing" Claims will be rejected if the month and/or day and/or year is missing. 3 Patient Sex "Member's sex is required" One box must be checked. "Insured name missing or illegible" Claims will be rejected if first and/or last name is missing or illegible. SAME or SAME AS PATIENT is acceptable and will not reject. Claims will be rejected if any one of the following are missing: street #, street name, city, state, zip 4 Insured Name 5 Patient Address (#, Street, city, state, zip) phone "Patient address missing" 6 Patient Relationship to Insured "Patient relationship to insured is required" 7 Insured's Address (#, street, city, state, zip) phone "Insured address missing" Date of Service "DOS is missing or illegible" 24a One of the four boxes must be checked Claims will be rejected if any one of the following are missing: street #, street name, city, state, zip. SAME or SAME AS PATIENT is acceptable and will not reject. Claims will be rejected if the if the From and To date of service are missing or illegible. CMS-1500 Required Fields CMS 1500 Field # Field/Data Element Required Rejection 24E Diagnosis Pointer "Diagnosis Pointer is required on Line(s) %Line%" 24F Line Item Charge Amount "Line item charge amount is missing on line(s) %Line%" 24G Days/Units "Days/units are required on line(s) %Line%" 26 Patient acct # 27 Assignment # "Patient Account/Control number is missing or illegible" "Assignment acceptance must be indicated on the claim" Billing Guidance Each service line with a From date of service, requires at least one (1) diagnosis pointer. Enter a value of greater than or equal to zero on each valid service line. Blank is not acceptable and will be rejected. Claims without a numeric value on each valid service line will be rejected. Claim will be rejected if missing or illegible. Yes or No must be checked. 28 Total Claim Charge Amount "Total charge amount is required" Claims will be rejected is a value greater than or equal to zero is not entered. Blank is not an acceptable value. For multipage claims, the total charge amount is only required on the last page of the claim. 33 Billing Provider Info & Ph# "Billing Provider name and/or address missing" Claims will be rejected if any one of the following are missing: name, street #, street name, city, state, zip. 33 Billing Provider Info & Ph# "P.O. Box is not permitted as a billing Claims will be rejected that are address" submitted with a P.O. Box UB-04 Required Fields UB04 Field # 1 1 3a 8b Field/Data Element Required Billing Provider Name, Address and Telephone Number Billing Provider Name, Address and Telephone Number Patient Control No. Patient Name Rejection "Billing Provider name and/or address missing" "P.O. Box is not permitted as a billing address" "Patient Account/Control number is missing or illegible" Claims will be rejected if a P.O. Box is submitted. Claim will be rejected for missing or illegible patient account/control number. "Member name is missing or illegible" Claims will be rejected if first and/or last name are missing or illegible; however SAME or "SAME AS INSURED" is acceptable. Patient Address "Patient address missing" 10 11 Patient Birth Date Patient Sex "Member DOB is missing" "Member's sex is required" 12 Admission Date "Admission Date is missing or illegible" 9a-e Billing Guidance Claims will be rejected if any one of the following are missing: name, street #, street name, city, state, zip. 13 Admission Hour "Admission Hour is required" 14 Admission Type "Admission Type is required" 15 Source of Referral for Admission or Visit "Source of Referral for Admission or Visit missing" Claims will be rejected if any one of the following are missing: street #, street name, city, state, zip. Claim will be rejected if missing month and/or day and/or year. Claim will be rejected if missing. Inpatient claims will be rejected when a valid date is missing or illegible. Inpatient claims (other than bill type 21X) will be rejected when a valid numeric value is missing or illegible. Claims will be rejected if a numeric value in missing. Claims will be rejected (other than bill type 14X) when the field is blank. 16 17 Discharge Hour Patient Discharge Status "Discharge Hour is required" "Patient discharge status is required" 45 Serv. Date "DOS is missing or illegible" Inpatient claims (other than bill type 21X) with frequency codes 1 or 4 will be rejected if a discharge hour is missing. Claims will be rejected if missing. Outpatient claims will be rejected if the field is blank on any service line. 45 Creation Date "Creation date is missing or illegible" Claims will be rejected when missing or illegible. "Days/units are required on line(s) %Line%" Claims will be rejected for each line with a from date of service that is missing a numerice value. A zero or negative value is not allowed and will be rejected. 46 Serv. Units UB-04 Required Fields UB04 Field # 47 Field/Data Element Required Line Item Charges 47 50 Total Charges Payer 52 Rel. Info 53 Asg. Ben. Rejection "Line item charge amount is missing on line(s) %Line%" "Total charge amount is missing" "Payer name is required" "Release of Information Certification Indicator is required" "Assignment of Benefits Certification Indicator is required" Billing Guidance Claims will be rejected if a value greater than or equal to zero is not present. Blank is not an acceptable value. For multipage claims, the total charge amount is only required on the last page of the claim. Claims will be rejected if a value greater than or equal to zero is not present. Blank is not an acceptable value. For multipage claims, the total charge amount is only required on the last page of the claim. Claims will be rejected if missing. Claims will be rejected if missing Claims will be rejected if missing Claims will be rejected if first and/or lst name is missing or illegible; however SAME or "SAME AS PATIENT" is acceptable. 58 Insured's Name 59 P. Rel "Member name is missing or illegible" "Patient's relationship to insured is required" (If blank, reject claim) Claims will be rejected if missing. 69 Admitting Diagnosis Code "Admitting diagnosis code is missing or illegible" Inpatient claims will be rejected when the admitting diagnosis code is missing or illegible. 70 Patient’s Reason for Visit "Patient’s Reason for Visit is missing" Required for all outpatient visits. If reason is missing claims will be rejected. "Attending Provider Qualifier is missing/ invalid" If other provider ID is present, two (2) character qualifier is required or claim will be rejected. "Attending Provider Other ID# Missing" If other provider ID qualifer is present, and other provider ID is blank, claim will be rejected. Attending Provider Qualifier 76 Attending Provider Other ID# 76