Chapter 8: Special Senses - River Valley Local Schools
advertisement

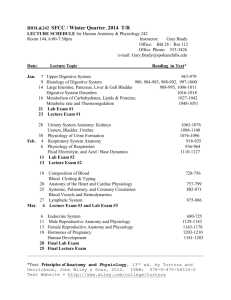
Anatomy and Physiology Chapter 8: Special Senses The Eye and Vision When provided with a model or diagram, identify the accessory eye structures and list the functions of each. Name the eye tunics and indicate the major function of each. Explain how rod and cone function differ. Describe image formation on the retina. Trace the pathway of light through the eye to the retina. Discuss the importance of an ophthalmoscopic examination. Define the following terms: accommodation, astigmatism, blind spot, cataract, emmetropia, glaucoma, hyperopia, myopia, and refraction. Trace the visual pathway to the optic cortex. Discuss the importance of the pupillary and convergence reflexes. The Ear: Hearing and Balance Identify the structures of the external, middle, and internal ear, and list the functions of each. Explain the function of the organ of Corti in hearing. Define sensorineural and conductive deafness and list possible causes of each. Explain how one is able to localize the source of a sound. Describe how the equilibrium organs help maintain balance. Chemical Senses: Taste and Smell Describe the location, structure, and function of the olfactory and taste receptors. Name the four basic taste sensations and list factors that modify the sense of taste. Developmental Aspects of the Special Senses Describe changes that occur in the special sense organs with age. 2009-2010 P. Holman Anatomy and Physiology Chapter 8: Special Senses The Eye and Vision When provided with a model or diagram, identify the accessory eye structures and list the functions of each. http://webvision.med.utah.edu/anatomy.html http://wps.aw.com/bc_marieb_ehap_8/25/6527/1671070.cw/index.html see figure 8.1 pg 253 of your text for external/accessory structures: eyelids, eyelashes, meibomian glands, ciliary glands, conjunctiva, lacrimal glands, lacrimal canals, lacrimal sac, nasolacrimal duct extrinsic eye muscles. Name the eye tunics and indicate the major function of each. Tunics or coats are (in order, exterior to interior): sclera (thick white connective tissue, called fibrous tunic = white of eye) of which the most anterior part is clear, forming the cornea; choroids (middle coat; blood rich, dark with pigments that prevent light scattering, forms the ciliary body attaching the lens and the iris, surrounds the pupil), retina (inner tunic; contains rods and cones the photoreceptors) No rods or cones at the optic disc (blind spot) – do the test on pg 257 of your book, under figure 8.5. Explain how rod and cone function differ. 2009-2010 P. Holman Anatomy and Physiology Rods are more concentrated at the periphery of the retina and allow us to see gray tones in dim light. They are responsible for our peripheral vision. Vitamin A is important for rod maintenance. Cones allow us to see color in bright light, are most dense near the center of the retina. The fovea centralis, lateral to each blind spot only contains cones. This is the area of greatest visual acuity. There are 3 types of cones, sensitive to blue light, to green light and a third ranging from green and red (these are called red cones). Am I colorblind? On-line test: http://colorvisiontesting.com/online%20test.htm#demonstration%20card Describe image formation on the retina. Light bends as it passes through the cornea, the aqueous humor, the lens and the vitreous humor. It bends more if the lens is thicker (more convex), less if the lens is thinner (less convex). Normal vision is set for distance vision. The light passes through the structures, focusing on the focal point at the back of the retina. The image is real and upside down. Trace the pathway of light through the eye to the retina. Light passes through the cornea, the aqueous humor, the lens and the vitreous humor before focusing on the retina. Discuss the importance of an ophthalmoscopic examination. This instrument illuminates the interior of the eye, showing the retina, optic disc and internal blood vessels. This allows one to detect diabetes, arteriosclerosis and degeneration of the optic nerve and retina. http://archopht.ama-assn.org/cgi/content/full/119/6/819?ck=nck http://archopht.ama-assn.org/cgi/content/full/119/6/819/FIGECS00089F1?ck=nck https://www.blueshieldca.com/hw/articles/hw_article.jsp?articleId=HWHW5223&fro mCategoryId=8&_requestid=1252309 http://www.cis.rit.edu/pelz/lab/papers/Hammer_Ferguson_Magill_White%20Image% 20stabilization%20for%20scanning%20laser%20ophthalmoscopy.pdf http://www.netterimages.com/image/15618.htm http://www.nlm.nih.gov/medlineplus/ency/article/003881.htm http://www.stlukeseye.com/Conditions/DiabeticRetinopathy.asp 2009-2010 P. Holman Anatomy and Physiology http://www.mdguidelines.com/atherosclerosis-and-arteriosclerosis http://www.merck.com/mmhe/sec20/ch225/ch225c.html http://www.i-care.net/faq-amd.htm http://webvision.med.utah.edu/index.html Define the following terms: accommodation, ac·com·mo·da·tion Pronunciation: \ə-ˌkäm-ə-ˈdā-shən\ Function: noun : an adaptation or adjustment especially of a bodily part (as an organ): as a : the automatic adjustment of the eye for seeing at different distances effected chiefly by changes in the convexity of the crystalline lens b : the range over which such adjustment is possible astigmatism, astig·ma·tism Pronunciation: \ə-ˈstig-mə-ˌtiz-əm\ Function: noun 1 : a defect of an optical system (as a lens) causing rays from a point to fail to meet in a focal point resulting in a blurred and imperfect image 2 : a defect of vision due to astigmatism of the refractive system of the eye and especially to corneal irregularity—compare EMMETROPIA, MYOPIA blind spot, blind spot Function: noun : the small circular area in the retina where the optic nerve enters the eye that is devoid of rods and cones and is insensitive to light—called also optic disk [blind spot illustration] cataract, cat·a·ract Pronunciation: \ˈkat-ə-ˌrakt\ Function: noun : a clouding of the lens of the eye or its surrounding transparent membrane that obstructs the passage of light emmetropia em·me·tro·pia Pronunciation: \ˌem-ə-ˈtrō-pē-ə\ Function: noun : the normal refractive condition of the eye in which with accommodation relaxed 2009-2010 P. Holman Anatomy and Physiology parallel rays of light are all brought accurately to a focus upon the retina—compare ASTIGMATISM, MYOPIA —em·me·trop·ic \-ˈträp-ik, -ˈtrōp-\ adjective glaucoma glau·co·ma Pronunciation: \glau̇-ˈkō-mə, glȯ-\ Function: noun : a disease of the eye marked by increased pressure within the eyeball that can result in damage to the optic disk and gradual loss of vision Physician-reviewed articles on glaucoma on Healthline. 1. Glaucoma (4 images) Glaucoma refers to a group of disorders that lead to dama... Visually explore glaucoma HealthMaps on Healthline: 1. Glaucoma 2. Hydrophthalmos hyperopia hy·per·opia Pronunciation: \ˌhī-pə-ˈrō-pē-ə\ Function: noun : a condition in which visual images come to a focus behind the retina of the eye and vision is better for distant than for near objects—called also farsightedness, hypermetropia —hy·per·opic \-ˈrō-pik, -ˈräp-ik\ adjective Physician-reviewed articles on hyperopia on Healthline. 1. Hyperopia (1 image) Hyperopia, also known as hypermetropia or farsightedness,... Visually explore hyperopia HealthMaps on Healthline: 1. Farsightedness 2. Eye Disorders myopia my·o·pia Pronunciation: \mī-ˈō-pē-ə\ Function: noun : a condition in which the visual images come to a focus in front of the retina of the eye because of defects in the refractive media of the eye or of abnormal length of the eyeball resulting especially in defective vision of distant objects—called also nearsightedness; compare ASTIGMATISM 2, EMMETROPIA Physician-reviewed articles on myopia on Healthline. 1. Nearsightedness (3 images) Nearsightedness is when the eyes focus incorrectly, makin... 2009-2010 P. Holman Anatomy and Physiology Visually explore myopia HealthMaps on Healthline: 1. Nearsightedness 2. Eye Disorders refraction re·frac·tion Pronunciation: \ri-ˈfrak-shən\ Function: noun 1 : the deflection from a straight path undergone by a light ray or a wave of energy in passing obliquely from one medium (as air) into another (as water or glass) in which its velocity is different 2 a : the refractive power of the eye b : the act or technique of determining ocular refraction and identifying abnormalities as a basis for the prescription of corrective lenses Source: http://www.merriam-webster.com/ Trace the visual pathway to the optic cortex. http://thalamus.wustl.edu/course/basvis.html Discuss the importance of the pupillary and convergence reflexes. Convergence reflexes cause both eyes to move medially when viewing something really close. This allows both eyes to aim at the object. The pupils also constrict when our eyes converge. This is called the accommodation pupillary reflex. The photopupillary reflex is when both pupils constrict when exposed to bright light. This prevents excess light from damaging the rods and cones (photoreceptors). The Ear: Hearing and Balance (http://mypages.iit.edu/~smile/bi8910.ht ml) Identify the structures of the external, middle, and 2009-2010 P. Holman Anatomy and Physiology internal ear, and list the functions of each. The external ear consists of the pinna or auricle (ear) and the external auditory canal. The auricle is designed to direct and collect sound waves into the canal of most animals, but does not do this in humans. The canal directs sound into the skull. It contains ceruminous glands that secrete cerumen or earwax. It ends at the tympanic membrane or eardrum. http://webschoolsolutions.com/patts/s ystems/ear.htm http://hyperphysics.phyastr.gsu.edu/HBASE/sound/earsens.h tml http://www.physicsclassroom.com/cl ass/sound/U11l2d.cfm 2009-2010 P. Holman Anatomy and Physiology The middle ear, or tympanic cavity, is filled with air within the temporal bone. It starts at the tympanic membrane and ends at the bony wall containing the oval window and the round window. It also has the auditory tube, running from the middle ear to the throat. The middle ear works when the pressure inside and outside the ear is equal. The tube helps with this. Otitis media or inflammation of the middle ear is common in children, because their auditory canal is more horizontal. The ossicles (hammer, anvil and stirrup or malleus, incus and stapes) span this area, transmitting movement from the tympanic membrane to the inner ear. The stirrup connects with the oval window. 2009-2010 P. Holman Anatomy and Physiology http://www.medicinenet.com/otitis_m edia/article.htm# http://www.vestibular.org/vestibulardisorders/specificdisorders/labyrinthitisvestneuritis.php The inner ear contains bony chambers or osseous labyrinth in shapes known as the cochlea the vestibule and the semicircular canals. It is filled with perilymph. The membranous labyrinth is filled with thicker endolymph. This is where the sounds are transmitted into neural signals sent to the auditory part of the brain. Explain the function of the organ of Corti in hearing. 2009-2010 P. Holman Anatomy and Physiology Housed in the cochlea, the organ of Corti contains hair cells or hearing receptors. The fluids move the hairs as they move in the tectorial membrane covering them. High pitches disturb receptors near the oval window, low pitches stimulate hairs farther away. The hairs transit impulses along the cochlear nerve, part of nerve VIII, the vestibulocochlear nerve). The sound reaches the ears at different times, creating a stereo effect. The receptors can become “immune” to a repetitive sound and stop signaling the brain. Hearing is the last sense to shut off and the first to turn on when we go to sleep and awaken. Define sensorineural and conductive deafness and list possible causes of each. 2009-2010 P. Holman Anatomy and Physiology Conduction deafness results from interruption of the sound vibrations to the inner ear fluids. It could be wax buildup, fusion of ossicles, ruptured eardrum, or otitis media. One may still be able to hear, with bone conduction apparatus (hearing aid). Sensorineural deafness happens with damage to receptor cells in the organ of Corti, to the cochlear nerve, or to neurons of the auditory cortex. This can result from really loud sounds. Equilibrium problems result in nausea, dizziness and balance problems because the vestibular apparatus impulses differ from visual cues. Meniere’s syndrome results in progressive deafness, causing nausea and vertigo. It is caused by 2009-2010 P. Holman Anatomy and Physiology arteriosclerosis, degeneration of cranial nerve VIII or pressure in the inner ear. Anti-motion-sickness drugs help. Am I deaf? http://www.phys.unsw.edu.au/jw/hear ing.html http://www.freehearingtest.com/test.s html http://www.rnid.org.uk/howwehelp/h earing_check/take_online_hearing_ch eck/?from=/hearing-check-homeright-bott-panel/ http://longislandaudiology.com/onlin e_test.php http://www.freehearingtest.ca/index_f lash.html 2009-2010 P. Holman Anatomy and Physiology http://www.handtronix.com/webdata/ flash/onlinescreener.html Explain how one is able to localize the source of a sound. http://en.wikipedia.org/wiki/Sound_loc alization http://www.cs.cmu.edu/~rms/Binaural Web/papers/SternWangBrownChapter. pdf http://www.plosbiology.org/article/info :doi/10.1371/journal.pbio.0030027 in bats: http://www.springerlink.com/content/c a965k6tk0ldf8cq/ http://www.sciencedaily.com/releases/ 1999/06/990617072054.htm 2009-2010 P. Holman Anatomy and Physiology in rats: http://www.ratbehavior.org/rathearing. htm http://www.physorg.com/news1191008 77.html prpt: http://psy2.ucsd.edu/~dmacleod/159/pr esentations05/MichaelSound%20Local ization%20of%20Humans.ppt Describe how the equilibrium organs help maintain balance. There are membrane sacs inside the vestibule of the inner ear. They contain hair cells, hair tufts, fluid and otoliths, tiny stones made of calcium salts. Gravity affects the movement of the thick fluid. When one tilts their head, the fluid moves the 2009-2010 P. Holman Anatomy and Physiology otoliths, which brush against the hair tufts signaling the nerve fibers blow the hair cells. This lets the brain know its position, with respect to gravity. Receptors in the semicircular canals (oriented x, y z) respond to angular movements. The receptor, crista amullaris, is a tuft of hair cells covered with a gel cap, or cupula. Since the fluid (endolymph) moves slower than your head, the cap shifts or lags behind your movement, stimulating hair cells which send impulses to the vestibular nerve and the cerebellum. When the movement stops, the fluid moves in the opposite direction, moves the cap the other way, causing the hair cells to slow their signaling. 2009-2010 P. Holman Anatomy and Physiology The signals from the vestibule, semicircular canals, eyes, and proprioceptors of muscles and tendons all provide information to the cerebellum regarding control of balance. Hearing loss websites: http://www.healthcentral.com/channe l/408/1191.html http://www.cdc.gov/niosh/docs/96115/diseas.html#hearings http://www.houseearclinic.com/heari ngloss.htm http://www.hearingaidscentral.com/h earingdiseasesanddisorders.asp http://www.asha.org/public/hearing/d isorders/causes.htm 2009-2010 P. Holman Anatomy and Physiology http://en.wikipedia.org/wiki/Hearing_ impairment common sounds and decibels: http://www.dangerousdecibels.org/tea chers_guide/DDB_TRG_Appendices _3.pdf http://www.deafness-andhearingaids.net/2007/03/07/howloud-is-too-loud-decibel-levels-ofcommon-sounds/ http://www.phys.unsw.edu.au/jw/dB. html http://explorersposts.grc.nasa.gov/pos t631/20072008/acoustic/AcousticSignalProc.pd f 2009-2010 P. Holman Anatomy and Physiology lab: http://www.dangerousdecibels.org/tea chers_guide/DDB_TRG_Activities_1 0.pdf Chemical Senses: Taste and Smell Describe the location, structure, and function of the olfactory and taste receptors. Name the four basic taste sensations and list factors that modify the sense of taste. Developmental Aspects of the Special Senses Describe changes that occur in the special sense organs with age. 2009-2010 P. Holman