Gastro15-GIMotilityII
advertisement
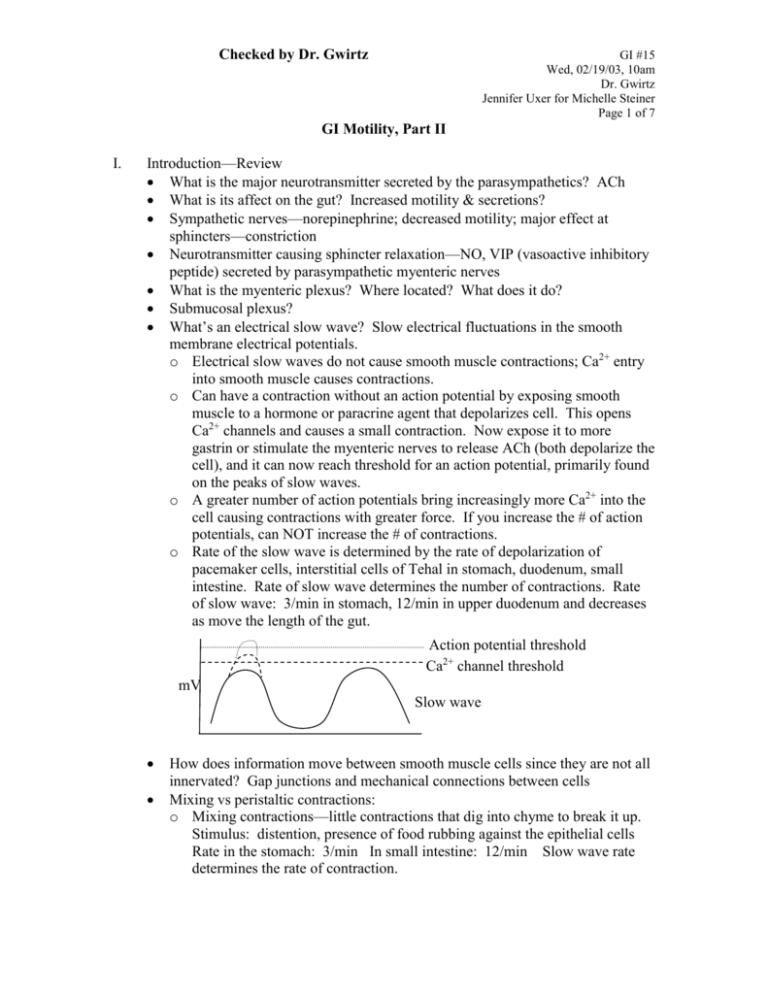
Checked by Dr. Gwirtz GI #15 Wed, 02/19/03, 10am Dr. Gwirtz Jennifer Uxer for Michelle Steiner Page 1 of 7 GI Motility, Part II I. Introduction—Review What is the major neurotransmitter secreted by the parasympathetics? ACh What is its affect on the gut? Increased motility & secretions? Sympathetic nerves—norepinephrine; decreased motility; major effect at sphincters—constriction Neurotransmitter causing sphincter relaxation—NO, VIP (vasoactive inhibitory peptide) secreted by parasympathetic myenteric nerves What is the myenteric plexus? Where located? What does it do? Submucosal plexus? What’s an electrical slow wave? Slow electrical fluctuations in the smooth membrane electrical potentials. o Electrical slow waves do not cause smooth muscle contractions; Ca2+ entry into smooth muscle causes contractions. o Can have a contraction without an action potential by exposing smooth muscle to a hormone or paracrine agent that depolarizes cell. This opens Ca2+ channels and causes a small contraction. Now expose it to more gastrin or stimulate the myenteric nerves to release ACh (both depolarize the cell), and it can now reach threshold for an action potential, primarily found on the peaks of slow waves. o A greater number of action potentials bring increasingly more Ca2+ into the cell causing contractions with greater force. If you increase the # of action potentials, can NOT increase the # of contractions. o Rate of the slow wave is determined by the rate of depolarization of pacemaker cells, interstitial cells of Tehal in stomach, duodenum, small intestine. Rate of slow wave determines the number of contractions. Rate of slow wave: 3/min in stomach, 12/min in upper duodenum and decreases as move the length of the gut. Action potential threshold Ca2+ channel threshold mV Slow wave How does information move between smooth muscle cells since they are not all innervated? Gap junctions and mechanical connections between cells Mixing vs peristaltic contractions: o Mixing contractions—little contractions that dig into chyme to break it up. Stimulus: distention, presence of food rubbing against the epithelial cells Rate in the stomach: 3/min In small intestine: 12/min Slow wave rate determines the rate of contraction. Checked by Dr. Gwirtz II. GI #15 Wed, 02/19/03, 10am Dr. Gwirtz Jennifer Uxer for Michelle Steiner Page 2 of 7 o Peristaltic contraction—stimulus: presence of food; distention. This leads to a reflex requiring myteric and parasympathetic nerves and the central nervous system. There’s a contraction (circular muscle contracts, longitudinal muscle relaxes) behind a bolus of food and receptor relaxation (circular muscle relaxes, longitudinal muscle contracts) in front of the bolus. The contraction moves down the gut. What is a primary peristaltic contraction? Location? Cause? Upper esophagus, stimulated by food touching the pharyngeal receptors initiating the swallowing reflex. What initiates a secondary contraction? Food stuck somewhere in the smooth muscle section of the esophagus. Substances causing the lower esophageal sphincter to relax: NO, fats, peppermint, caffeine, nicotine, alcohol, antacids, nitrates, anticholinergic drugs, progesterone, valsalva maneuver, carbohydrates Note: the tape stopped recording at this point. The rest of the lecture followed the power points closely. I had written most everything else down and have included it in the scribe. Name a swallowing disorder: achlasia—atony, no peristalsis; food stays in the esophagus; lower esophageal sphincter won’t relax. Pressure = 0 in the body; pressure is high in the LES and normal in the UES Stomach Body: has thin walls; location of most of the gastric secretory glands; mainly has mixing contractions Antrum: thick walls; peristaltic contractions that push chyme (a liquid of particles <2mm in diameter) against the pyloric sphincter. If the chyme is the right consistency and a contraction occurs at the right time, the chyme is pushed through the pyloric sphincter. A. Functions of the Stomach Store large quantities of food Mix food with gastric secretions until it forms a semifluid mixture, called chyme Slow emptying of the chyme into the small intestine at a rate suitable for proper digestion and absorption Dilutes or concentrates fluids so that they are the same concentration as the body fluids before reaching the intestine Forms intrinsic factor which is necessary for Vitamin Bl2 absorption B. Receptive relaxation of the Stomach Ability of the stomach to accommodate a large volume meal with only a small increase in intraluminal pressure. Function of all hollow organs due to vagal nerve mediated response and the ability of smooth muscles to slide on each other. Vagal fibers innervate intrinsic nerves to cause receptive relaxation via a transmitter (VIP or NO) Vagotomy greatly diminishes receptive relaxation Checked by Dr. Gwirtz GI #15 Wed, 02/19/03, 10am Dr. Gwirtz Jennifer Uxer for Michelle Steiner Page 3 of 7 C. Motility in the stomach [Electrical] Slow waves - 3 per min (Basic Electrical Rhythm) spontaneous fluctuations of membrane potential; ongoing waves Mixing waves - weak contractions which move toward antrum; mix food with gastric secretions Peristaltic constriction rings - force antral contents under pressure toward pylorus D. Emptying of the Stomach Promoted by intense peristaltic contractions of the stomach antrum. Increased intragastric pressure forces material across the pyloric sphincter. Opposed by varying degrees of resistance to the passage of chyme through the pyloric sphincter—influenced by nervous and humoral signals from the stomach and duodenum. These decrease the force of contractions and decrease emptying of the stomach. Begins 30-60 min after eating; complete within 4-4 1/2 hr after eating E. Factors Promoting Gastric Emptying Promoted by factors which cause antral pressure > duodenal pressure Interdigestive Phase: Motilin released into bloodstream, mediates IMMC— housekeeping functions. ↑ motilin in stomach and small intestine → peristaltic contraction sweeps through the gut from stomach to small intestine emptying them to prepare for the next meal. Cephalic Phase—thinking about eating, smelling, seeing, chewing food: o Vagal Reflexes (direct)—before swallowing o Vagal stimulated release of gastrin from G-cells. Motility and secretions are vagally mediated. Vagus releases ACh, which depolarizes smooth muscle → ↑ force of contraction → ↑ gut motility o Cephalic phase abolished by atropine or by cutting the vegus nerve. Gastric Phase: o Mediated by stretch—stimulates mechanoreceptors o Vagal Reflexes (ACh)— ↑ contractility o Myenteric Reflexes—local reflexes o Gastrin (release stimulated by food and vagal reflexes) o Partial Gastrectomy—lopping off part of the stomach decreases its volume and causes it to empty faster. F. Factors Which Delay Gastric Emptying See figure in power points for flow chart o There’s an error: Gastrin promotes emptying!! o Stomach secretes acid, mixes with food stuffs → small intestine → acid receptors → secretin release into blood → reaches targets in stomach → hyperpolarizes cells → decreases contractions in stomach and gastric emptying, decreases releases from g- and parietal cells o Proteins and amino acids → CCK and GIP release → stomach → cells hyperpolarized → decreases contractions in stomach and gastric emptying Checked by Dr. Gwirtz GI #15 Wed, 02/19/03, 10am Dr. Gwirtz Jennifer Uxer for Michelle Steiner Page 4 of 7 o G cells in small intestine secrete an intestinal gastrin which causes contraction of pyloric sphincter (delaying emptying) but also increases gastric motility (which will promote gastric emptying). o Release of an unknown hormone occurs in response to food and distention of the stomach and duodenum. Intestinal Phase: o Duodenal distension—myenteric nerve feedback o Duodenal irritation—myenteric nerve feedback o CCK (fats, proteins, amino acids)—hyperpolarize stomach o Gastrin ( via ↑ pyloric tone) o Secretin (acid, osmolality of lumen of stomach) o GIP (fat) o VIP (distension)—paracrine factor of duodenum, decreases activity of all smooth muscles o Enterogastric Reflexes (local myenteric, sympathetic, vagal, hormonal) o Diabetes mellitus (autonomic neuropathy) o Surgical vagotomy (gastroparesis) G. Gastric Emptying Rates Liquids (2-3 min) faster than solids (15 min) Small particles > larger Easily fragmented food (noodles > meat) Large, heavy persons faster than non-obese (greater pressure gradient) Inverse with caloric content, not meal weight (noncaloric liquids such as water empty first) Post-gastrectomy (resection), solids empty faster than before (8O% of contents in 10 min) due to the smaller stomach volume CHO > protein > fat CHO empty quickly; proteins trigger release of CCK and GIP to decrease the force of contractions and inhibit stomach release; fats float on top of the chyme and are the last to empty—cause a strong secretion of CCK Neutral acid Isotonic > hypo- or hypertonic—cause release of secretin—feeds back to stomach delaying release of contents For the graph: liquid glucose empties quickly. If liver is eaten, it takes longer to empty because it’s full of fat which causes the release of CCK. If spheres are ingested, they stay in the stomach because they’re too large to fit through the pyloric sphincter. H. Case Study: Dumping Syndrome 1. Case Study A 72 yr old man complains of tiredness, long standing symptoms of dizziness, sweating, and palpitations after meals. Had a partial gastrecomy 8 years earlier. Has become forgetful and forgets to take his medications, vit B12 injections. Has megoloblastic (pernicious) anemia (because he’s not getting his B12 injections) and mild metabolic acidosis, iron deficiency. Checked by Dr. Gwirtz III. GI #15 Wed, 02/19/03, 10am Dr. Gwirtz Jennifer Uxer for Michelle Steiner Page 5 of 7 Explained by the effects of the gastrectomy. Dumping syndrome explains dizziness, sweating, and palpitations. 2. Dumping Syndrome After gastrectomy, hypertonic/osmotic food empties (dumps) directly into duodenum/jejunum without mixing with gastric secretions. So, it’s not diluted and the small intesting doesn’t like anything that’s not isoosmotic. – nausea, epigastric pain, BP, sweating, vertigo, fainting – due to hypertonic chyme being dumped rapidly into duodenum or jejunum – fluid moves from blood stream into intestinal lumen to dilute contents BV (can lose lots of blood volume trying to dilute the contents) BP sympathetic reflex—baroreflex (↑ HR, force of contractility, sweating, causes orthostatic hypotenion due to BP; stuff sitting in duodenum causes nausea) – Prevent this by eating lots of small meals several time/day – Partial gastrectomy removes body of stomach, secretory cells—parietal cells and intrinsic factor—can’t absorb Vit B12 without it – acid (aids in iron absorption—changes it from Fe+3 to Fe+2) – intrinsic factor (necessary for B12 absorption) – pepsin (no real consequences; it’s the only enzyme that breaks down meat fibers)—stomach is expendable Small Intestine A. Movements of the Small Intestine 1. Mixing or Segmentation Contractions Distention (stretch) initiates Purpose: Breaks up chyme to increase surface area to make it easier for enzymes to digest Mixes chyme with secretions Rate related to electrical slow waves Myenteric plexus (myogenic) 2. Propulsive (Peristaltic) Contractions Distention (stretch) initiates Usually weak—die out after few cm, about 5cm Parasympathetic and myenteric nerves Influenced by nervous signals, hormonal factors 3. Law of the Intestine chyme moves analward B. What increases small intestinal motility? ACh (vagal, myenteric) Gastrin CCK—fat triggers its release; gastric motility Motilin—released during interdigestive period Distension (pressure)—open Ca2+ channels with a stretch Checked by Dr. Gwirtz GI #15 Wed, 02/19/03, 10am Dr. Gwirtz Jennifer Uxer for Michelle Steiner Page 6 of 7 Hyperthyroid— ↑ metabolism of all cells Fever Hyperglycemia Intense irritation—can be caused by bacteria, toxins, viruses An overabundance of intestinal motility causes diarrhea C. What decreases small intestinal motility? Norepi (sympathetic) Epinephrine VIP—inhibits smooth muscle GIP Secretin NO Glucagon—released in gut in response to different food substances Opioids Over-distension—blockage, build-up of gas Hypothyroid Hypoglycemia Malabsorption syndrome Trauma 1 big problem after surgery is the lack of peristaltic contractions which decrease gut motility (response to anesthesia). Patients complain of a bloated abdomen because gas builds up in the small intestine and colon causing discomfort. D. Peristaltic Rush Also called Power Propulsion Stimulus: intense irritation of intestinal mucosa e.g., severe infectious diarrhea, parasites, enterotoxins, ionizing radiation, application of vinegar to mucosa—anything irritating Initiated by extrinsic nervous reflexes to autonomic nervous system ganglia and to brainstem and back to the gut Enhanced by myenteric plexus reflexes Strong, long-lasting giant migrating contractions which travel long distances in small intestine Begins in duodenum, moves length of gut and Sweeps contents into colon → diarrhea E. Interdigestive Migrating Myoelectric Complex System Bursts of rhythmic contractions occur in cycles during the fasting state (2-4 hr after a meal), lasting 5-10 min followed by a quiet period. Recurs every 1.5 - 2 hrs and is related to the release of motilin. Occurs when the stomach is empty Active region slowly passes down length of the gut: starts in gastric antrum and progress to ileum (ileocecal valve) Related to hormone-like substance motilin Checked by Dr. Gwirtz GI #15 Wed, 02/19/03, 10am Dr. Gwirtz Jennifer Uxer for Michelle Steiner Page 7 of 7 Stops with feeding—with the 1st swallow Housekeeping function - keeps lumen cleared out during interdigestive period. Stops immediately with feeding.salivary glands secrete at basal rate to moisten oral cavity & keep it clean UES and LES constricted. Gastric juice produced at low level (stomach contains low volume of highly acidic fluid). There’s also a low rate of bicarbonate formation. F. Other Events Occurring During Interdigestive Phase of Digestion IMMC Pancreas produces low HCO3, low enzyme juice at minimal rate Concentration of bile salts in portal venous blood low Rate of hepatic bile salt synthesis is high Rate of hepatic salt secretion low