outline22344 - American Academy of Optometry
advertisement
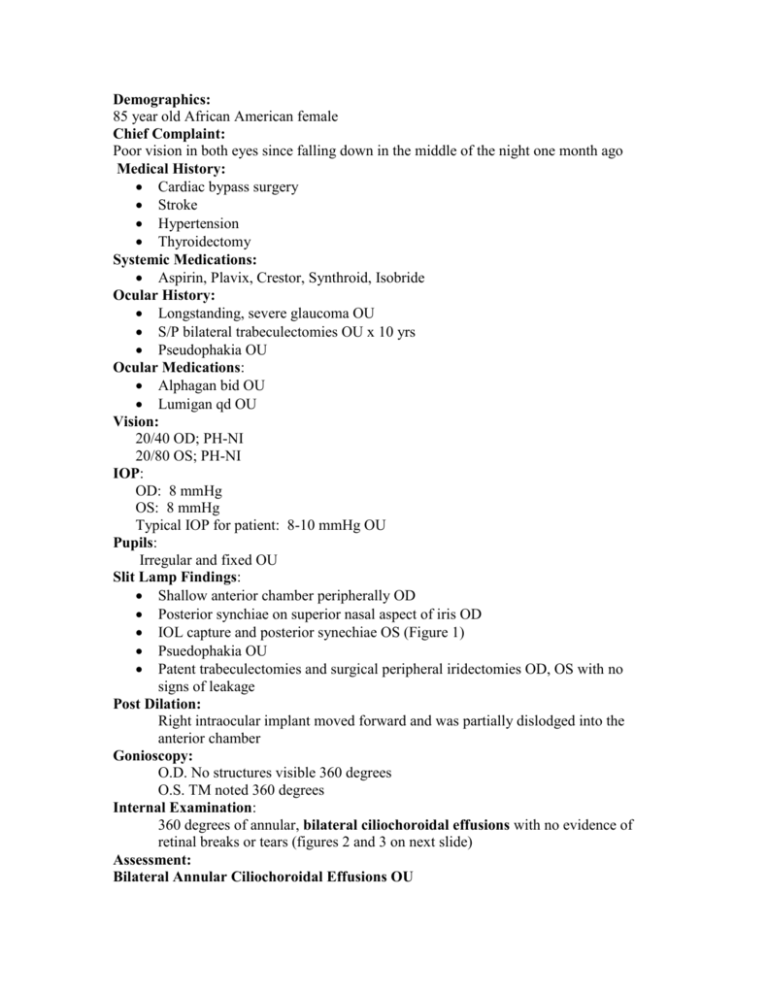
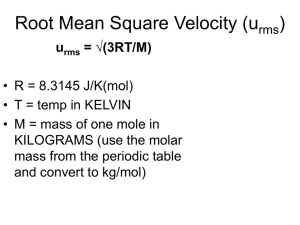
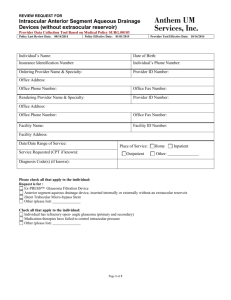
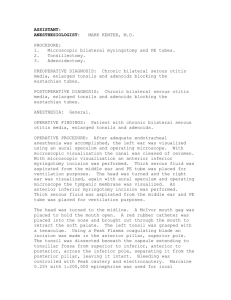
Demographics: 85 year old African American female Chief Complaint: Poor vision in both eyes since falling down in the middle of the night one month ago Medical History: Cardiac bypass surgery Stroke Hypertension Thyroidectomy Systemic Medications: Aspirin, Plavix, Crestor, Synthroid, Isobride Ocular History: Longstanding, severe glaucoma OU S/P bilateral trabeculectomies OU x 10 yrs Pseudophakia OU Ocular Medications: Alphagan bid OU Lumigan qd OU Vision: 20/40 OD; PH-NI 20/80 OS; PH-NI IOP: OD: 8 mmHg OS: 8 mmHg Typical IOP for patient: 8-10 mmHg OU Pupils: Irregular and fixed OU Slit Lamp Findings: Shallow anterior chamber peripherally OD Posterior synchiae on superior nasal aspect of iris OD IOL capture and posterior synechiae OS (Figure 1) Psuedophakia OU Patent trabeculectomies and surgical peripheral iridectomies OD, OS with no signs of leakage Post Dilation: Right intraocular implant moved forward and was partially dislodged into the anterior chamber Gonioscopy: O.D. No structures visible 360 degrees O.S. TM noted 360 degrees Internal Examination: 360 degrees of annular, bilateral ciliochoroidal effusions with no evidence of retinal breaks or tears (figures 2 and 3 on next slide) Assessment: Bilateral Annular Ciliochoroidal Effusions OU Our patient most likely developed annular choroidal detachments from a combination of having inflammation secondary to her trauma and a history of previous glaucoma filtering surgery Her effusions caused the anterior rotation of the ciliary body-iris diaphragm and the displacement of her right IOL into the anterior chamber Plan: D/C Lumigan Rx: Homatropine TID OU Rx: Lotemax qhs OU Referral to retinal specialist for possible surgical intervention Follow-Up After the dilating drops wore off, her right IOL implant did return completely to the posterior chamber Six months after her initial visit: The bilateral choroidal effusions have resolved Her glaucoma is managed only with Alphagan-P in the left eye and remains in 68mmHg range The right anterior chamber remains shallow and the angle is closed on gonioscopy Discussion Definition: Ciliochoroidal or uveal effusion is an abnormal accumulation of serous fluid from the choroiocapillaris into the potential space between the sclera and the choroid or ciliary body1,2 The word effusion, by definition, means an escape of fluid into a tissue. Clinically, the terms ciliochoroidal effusion and choroidal detachment are used interchangeably throughout the literature. Common Etiologies of Serous Detachments: Intraocular surgery Hypotony Inflammation Spontaneous-- typically occur in patients with unusually thick scleras or nanophthalmos3 Symptoms: No symptoms Complain of decreased visual acuity Photophobia Pain Reduced peripheral vision Clinical Characteristics of Ciliochoroidal Effusions Often times serous detachments are associated with hypotony and a flat anterior chamber Ciliochoroidal effusions may occur with or without other associated ocular abnormalities or systemic conditions Effusions can be flat, lobular, or annular in nature A smooth, solid appearance with no holes or tears will be noted on indirect ophthalmoscopy Typically appear yellowish-grey to orangish-brown in color The pattern of choroidal vessels will be visible on the elevation Visualization of the ora serrata and pars plana without scleral depression is usually possible Effusions almost always occur anterior to the vortex veins Serous fluid found within the effusion is biochemically consistent with blood serum Choroidal folds or linear streaks of RPE hypertrophy can occur after the effusion resolves4 Differential Diagnosis Diagnosis is usually confirmed with careful clinical observation and ultrasound. Fluorescein angiography can also help differentiate serous choroidal detachments from other suspicious lesions (table 1) Hemorrhagic Choroidal Detachment Malignant Melanoma Hemangioma Rhegmatogenous Retinal Detachment Non-rhegmatogenous Retinal Detachment Retinoschisis Treatment of Ciliochoroidal Effusions Treatment depends on the etiology Uncomplicated effusions can resolve spontaneously without treatment or sequelae Cycloplegics (atropine or scopolamine t.i.d.) can be used to decrease blood vessel permeability, retract the ciliary processes, and lessen ciliary spasm5 Topical steroids (prednisolone acetate 1%) can be added if inflammation is present or resolution doesn’t occur Systemic steroids (prednisone 20-80mg daily) may be necessary in severe or refractory cases Surgical drainage of the serous fluid should be considered if the detachment persists Immediate surgical intervention is indicated when there is lens-cornea touch or IOLcornea touch exists6 Conclusion Visual outcome is unpredictable and pre-existing eye conditions (e.g. advanced glaucoma) influence the final outcome7 In the case of our patient, her intraocular implant was displaced partially into her anterior chamber because the effusions caused her ciliary body to rotate around its attachment to the scleral spur, shifting the lens/iris diaphragm forward6 Her angle is closed on gonioscopy in the right eye but her intraocular pressure remains low because of a patent peripheral iridectomy References 1. Brockhurst RJ. Ciliochoroidal (uveal) effusion. ch. 112. In: Ryan SJ, editor. Retina. St. Louis: CV Mosby Year Book, 1994;2:1745-1752. 2.Torbit J. Ciliochoroidal Effusion. Clinical Vision and Vision Care. 1998; 10: 3-10. 3. Dunbar MT. Vision Loss Follows Hyperopia. Review of Optometry. 2006; 143:72-73. 4. Gass JDM. Stereoscopic atlas of macular diseases, diagnosis and treatment. 4th ed. St. Louis: CV Mosby, 1997: 200-205 5. Pavlin CJ, Easterbrook M, Harasiewicz K, Foster FS. An ultrasound biomicroscopic analysis of angle closure glaucoma secondary to ciliochoroidal effusion in IgA nephropathy. Am J Ophthalmol, 1993:116(3):341-5. 6. Dugel PU, Heurer DK. Annular peripheral choroidal detachment simulating aqueous misdirection after glaucoma surgery 7. Traverso CE. Choroidal Detachment. www.emedicine.com. 2005; 1-9