CASE 1:
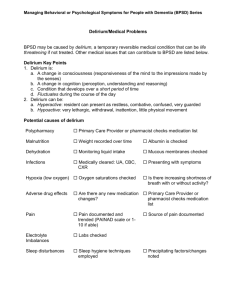
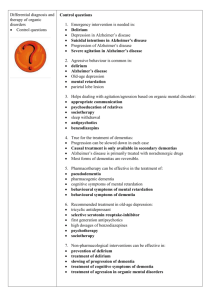
advertisement

Objectives: i. ii. iii. iv. v. vi. vii. viii. Discuss the Differential diagnoses for the patient who presents with confusion Discuss the difference between delirium and dementia List the causes of delirium in the elderly Discuss the Mini-Mental status exam Name 2 other clinical tests that can be done in the office to assess for dementia Describe the symptoms of Alzheimer’s Disease Discuss laboratory evaluation of a patient who presents with confusion. Describe the role of sleep apnea in confusion USC Case # 12: Acute Confusion PART 1 Backgound, You are in a rural primary care practice in an office adjacent to the hospital. You have access to outpatient laboratory and xray. Your patient is Mr. John Galimore age 77 accompanied by his wife Pearl. The following is the soap note you have prepared from your interview with the patient and your exam: s) CC: Pearl Galimore brings John to the office today complaining that he has been “out of it” all morning. Pearl noted that John had taken two doses of his medicines that morning, due to his confusion. She is not certain however which came first the confusion or his taking of the medication. Past Medical History: Hypertension, arthritis, cholecystectomy in 1999, hyperlipidemia, hypercholesterolemia, and a fracture of his R. arm as a young man. Medications: Lopressor 50 mg. 1 daily Motrin 600 mg. 1 daily in am Lipitor 40 mg. 1 daily. Allergy: NKDA Family history: Father deceased at age 80 with M.I. and Diabetes. Patient’s mother became "very confused" in the years prior to her death, but she did not have any known heart or cerebrovascular disease. He has one daughter who is married and has two grandchildren, all in good health. He had one brother who was killed at a young age in the military. Social history: Smoked one pack of cigarettes a day for 54 years until age 70, He and his wife deny alcohol or drug use. He does wood working for a hobby and sells it in local fairs. He plays the fiddle in a local town bluegrass band and practices at least once per week. Review of Systems: Mr. Galimore does NOT complain of any headache, visual disturbances, chest pain, dizziness, fatigue, syncope, shortness of breath, palpitations, and no numbness or tingling of extremeties, and no muscular weakness. The rest of the review of systems did not contribute any new symptoms.Patient denies any fevers or unintended weight loss, denies recent head trauma or headaches, denies any cough, or SOB. No diarrhea, constipation, nausea, or vomiting. Patient also denies urinary frequency, urgency, or dysuria. Physical Exam: T. 98 p. 52 R. 20 Bp. 110/60 Wt. 230 height 5 ft 8 inches HEENT: Pupils were equal and reactive. Fundoscopic exam was normal for age with some mild AV nicking. Carotids were equal without bruits, Thyroid was not enlarged, and ears, nose and throat were unremarkable with the exception of a cerumen occlusion in the patient’s right ear. Heart exam revealed regular rhythm and rate, except a mild bradycardia at 52/min. No Murmurs or gallups heard. Lungs were clear in all fields Abdomen exam was unremarkable except that there was difficulty in palpation due to obesity Extremeties revealed no edema, pulses were intact, no cyanosis, no skin lesions Neurological exam: Cerebellar exam was intact. There were good reflexes bilaterally and a normal motor and sensory exam. Cranial nerves were intact. There was no speech impairment and no abnormalities in facial expression. “There is no generally accepted consensus regarding the distinction between delirium and confusional states. The terms "acute confusional state" and "encephalopathy" are often used synonymously with delirium. The more general term "confusion" is used to indicate a problem with coherent thinking. Confused patients are unable to think with normal speed, clarity, or coherence [3]. Confusion is typically associated with a depressed sensorium and a reduced attention span, and it is an essential component of delirium.” Up To Date QUESTION What is your differential diagnosis prior to performing any further tests or exams: Please list prior to going to the next page: CASE 1, PART 1. 1. ANSWERS AND DISCUSSION Confusion Confusion can be related to many reasons in this age group. The following is a list of possible etiologies a. Secondary to Medication b. Dementia c. Delirium d. Transient Ischemic Attack e. Hypoxic Event f. Metabolic Disorder g. Unwitnessed head trauma h. Infection i. Brain Tumor j. Atypical seizure Discussion of each differential: a. Secondary to Medication Pearl does not know if the confusion occurred prior to or after the medication error occurred. Note the patient is bradycardic. Could this occur secondary to taking his medication twice? Is confusion a side effect of taking larger than the recommended dose of medication in the elderly? Could his two doses of him blood pressure medication causing the bradycardia and the blood pressure to be much lower than usual result in less cerebral flow? b. Dementia/delirium In a patient age 77 one must consider both dementia and delirium with changes in behavior. Other alternatives can include depression or suicidal behavior. You further question for depression and suicidal behavior and they are not a factor. What exams could you perform to evaluate the patient for dementia and or delirium? Physical exam, Mental status exam, Lab work to r/o infection, hypoxemia, CHF, CVA, metabolic causes (electrolyte imbalance) What are some causes of delirium in the elderly? Dementia, Underlying metabolic disorder, Medications, CVA, Intoxication, Sleep deprivation, Fecal impaction, urinary retention, hypoxia, head trauma, change in residence – almost anything c. Transient Ischemic Attack. A transient Ischemic Attack may be caused by atherosclerotic disease. John has dyslipidemia and is a candidate for atherosclerotic disease. Other possibilities for TIA include sudden lowering of his blood pressure resulting in decreased perfusion, or an emboli. What tests might you order to rule these out? d. Hypoxic Event A hypoxic event can result in confusion. Note John’s height and weight. Calculate his BMI. Sleep apnea may occur in obese individuals and may be the cause of morning confusion upon waking in elderly patients. e. Metabolic Disorder With the obesity and the history of dyslipidemia you must consider the metabolic causes of confusion especially those associated with diabetes. You should rule our an adult onset diabetes in an elderly obese patient who becomes ill. Thyroid disorders are a cause of acute confusion or dementia that must be considered in the elderly. Electrolyte disorders must be considered due to use of NSAID and renal function. You should rule out renal abnormalities. f. Infection Infection, especially if the patient is septic, is a frequent reason for acute confusion in the elderly. John does not show any sign of respiratory or other infection, however some infections are not readily evident in the elderly such as a U.T.I. g. Unwitnessed head trauma Elderly patients often fall and recover. They may or may not mention the injury to a family member. If a slow subdural bleed occurs, the first signs might be confusion. h. Tumor Brain tumors may present as acute confusion. Common causes of delirium and confusional states Drugs and toxins Prescription medications (eg, opioids, sedative-hypnotics, antipsychotics, lithium, skeletal muscle relaxers, polypharmacy) Non-prescription medications (eg, antihistamines) Drugs of abuse (eg, ethanol, heroin, hallucinogens, nonmedicinal use of prescription medications) Withdrawal states (eg, ethanol, benzodiazepines) Medication side effects (eg, hyperammonemia from valproic acid, confusion from quinolones, serotonin syndrome) Poisons: Atypical alcohols (ethylene glycol, methanol) Inhaled toxins (carbon monoxide, cyanide, hydrogen sulfide) Plant-derived (eg, Jimson weed, Salvia) Infections Sepsis Systemic infections; fever-related delirium Metabolic derangements Electrolyte disturbance (elevated or depressed): sodium, calcium, magnesium, phosphate Endocrine disturbance (depressed or increased): thyroid, parathyroid, pancreas, pituitary, adrenal Hypercarbia Hyperglycemia and hypoglycemia Hyperosmolar and hypoosmolar states Hypoxemia Inborn errors of metabolism: porphyria, Wilson's disease, etc. Nutritional: Wernicke's encephalopathy, vitamin B12 deficiency, possibly folate and niacin deficiencies Brain disorders CNS infections: encephalitis, meningitis, brain or epidural abscess Epileptic seizures, especially nonconvulsive status epilepticus* Head injury* Hypertensive encephalopathy Psychiatric disorders* Systemic organ failure Cardiac failure Hematologic: thrombocytosis, hypereosinophilia, leukemic blast cell crisis, polycythemia Liver failure: acute, chronic Pulmonary disease, including hypercarbia and hypoxemia Renal failure: acute, chronic Physical disorders Burns Electrocution Hyperthermia Hypothermia Trauma: with systemic inflammatory response syndrome, *head injury, fat embolism * Disorders that, while not truly systemic or "medical", may produce the clinical picture of Questions 2 and 3 1. What other physical exams do you want to do BEFORE you order any further laboratory tests? Mini-Mental State Examination — The Mini-Mental State Exam (MMSE) has been the most widely used cognitive test for dementia in US clinical practice [27,28], although patent protection has led to increased use of other bedside exams. The MMSE takes approximately seven minutes to complete. It tests a broad range of cognitive functions including orientation, recall, attention, calculation, language manipulation, and constructional praxis. While not designed specifically to assess late life neurodegenerative dementias, it has become a common language for clinicians until a better, simpler or shorter test is developed. The MMSE includes the following tasks [27]: ●What is the date: (year)(season)(date)(day)(month) - 5 points ●Where are we: (state)(county)(town)(hospital)(floor) - 5 points *Name three objects: Ask the patient all three after you have said them. Give one point for each correct answer. Then repeat them until he/she learns all three. Count trials and record. The first repetition determines the score, but if the patient cannot learn the words after six trials then recall cannot be meaningfully tested. Maximum score - 3 points. ●Serial 7s, beginning with 100 and counting backward: one point for each correct; stop after five answers. Alternatively, spell WORLD backwards: one point for each letter in correct order. Maximum score - 5 points. ●Ask for the three objects repeated above: one point for each correct. Maximum score - 3 points. ●Show and ask patient to name a pencil and wrist watch - 2 points. ●Repeat the following, "No ifs, ands, or buts." Allow only one trial - 1 point. ●Follow a three stage command, "Take a paper in your right hand, fold it in half, and put it on the floor." Score one point for each task executed. Maximum score - 3 points. ●On a blank piece of paper write "close your eyes;" ask the patient to read and do what it says - 1 point. ●Give the patient a blank piece of paper and ask him/her to write a sentence. The sentence must contain a noun and verb and be sensible - 1 point. ●Ask the patient to copy a design (eg, intersecting pentagons). All 10 angles must be present and two must intersect - 1 point. The maximum score on the MMSE is 30 points. A score of less than 24 points is suggestive of dementia or delirium. Using a cutoff of 24 points, the MMSE had a sensitivity of 87 percent and a specificity of 82 percent in a large population based sample. However, the test is not sensitive for mild dementia, and scores may be influenced by age and education, as well as language, motor, and visual impairments. In one study, for example, the median MMSE score was 29 for individuals with at least nine years of schooling, 26 for those with five to eight years of schooling, and 22 for those with four years of schooling or less [29]. The pattern of missed questions can be as important as the overall score; if the clinical deficit is memory loss, a person may miss all three objects on delayed recall and score 27, which for that individual would be a false-negative result if a cutoff of 24 is being used. The use of higher cutoff scores on the MMSE improves sensitivity but lowers specificity. For research purposes, some investigators use a cutoff score of 26 or 27 in symptomatic populations in order to not miss many true cases, while lower cutoffs would be necessary in populations where the expected prevalence is low [31]. Agespecific norms also have been established [29]; some groups have developed tools that incorporate age, gender, and education level. The MMSE also has utility in assessing competency in decision making. Studies suggest that high scores, ≥23, and low scores, <19, can be highly predictive in discriminating competency from incompetency. Intermediate scores warrant more detailed competency evaluation. The MMSE has limitations for assessing progressive cognitive decline in individual patients over time. Changes of two points or less are of uncertain clinical significance as they may represent measurement error, regression to the mean, or a practice effect. Other brief cognitive assessments — Ideal tests for mental status screening should be brief and have good performance in populations with different cultural, linguistic, and educational backgrounds. 2. Mini-Cog — The "Mini-Cog" test consists of a clock drawing task (CDT) and an uncued recall of three unrelated words [40]. The CDT is considered normal if all numbers are present in the correct sequence and the hands display the correct time in a readable way. Scoring is based on a simple decision tree with the following three rules: ●Subjects recalling none of the words are classified as demented ●Subjects recalling all three words are classified as non-demented ●Subjects with intermediate (one to two) word recall are classified based on the CDT (abnormal = demented; normal = non-demented) The advantages of the Mini-Cog include high sensitivity for predicting dementia status, short testing time relative to the MMSE, ease of administration, and diagnostic value not limited by the subject's education or language [40]. In a retrospective analysis of data from a random sample of 1119 older adults, the MiniCog was compared with the MMSE (at a cut point of 25); the Mini-Cog had similar sensitivity (76 versus 79 percent) and specificity (89 versus 88 percent) for dementia [41]. Although promising, the Mini-Cog requires further validation with prospective data. These tests are not appropriate for assessing patients with aphasic or anomic disorders. 3. Informant interview — A brief, eight-item questionnaire for informants appears to be sensitive for detecting dementia and cognitive impairment [42]. Informants are asked whether the patient has exhibited any increase in the following deficits or behaviors: ●Problems with judgment ●Reduced interest in hobbies/activities ●Repeats questions, stories, or statements ●Trouble learning how to use a tool or appliance ●Forgetting the correct month or year ●Difficulty handling financial affairs (bill-paying, taxes) ●Difficulty remembering appointments ●Consistent problems with thinking and/or memory A positive response to two or more questions had a sensitivity of 93 percent and a specificity of 46 percent. Increasing the cutoff score to three positive responses decreased the sensitivity to 90 percent and increased the specificity to 68 percent. 3. What preliminary tests do you want to order, prior to ordering further more expensive exams? To better learn/remember what will follow, Answer these questions prior to preceding. EXAM and TESTING CONSIDERATIONS: First consider the Dementia or Delirium diagnosis. Dementia is characterized by multiple cognitive deficits and impairment in memory. It usually develops slowly and insidiously, and is essentially a disease of older people. On the other hand, delirium is a condition marked by alterations in level of consciousness, and its onset can be quite sudden and the symptoms may come and go. Importantly, delirium is often reversible while dementia is generally a progressive and irreversible disorder. The mental status examination is an important exam the family physician must use to assess a patient’s cognitive function including: 1. 2. 3. 4. 5. Patient’s orientation to person place and time, Alertness to surroundings and conversation and thought patterns Mood Speech Specific cognitive functions. A Mini-mental status exam was performed and found the following: The Mini-Mental Status Exam is used by practitioners to screen for certain cognitive difficulties. The maximum score is 30 points, with scoring as follows: Orientation: 10 points maximum The patient was able to answer the year, season, date, and day of the week and month. The patient was also able to answer that town he lived in, what state, what country, and where he was currently. Registration: 3 points maximum The patient was told of three objects, a pencil, a notebook, and a tissue box. He was able to repeat all three in the correct order. Attention and Calculation: 5 points maximum The patient was asked to count backward from 100 by 7 (up to 65). He could not perform this task after the 80s. Recall: 3 points maximum You ask the patient to recall the items you told him during registration earlier. The patient was only able to answer the pencil and the tissue box. Language: 9 points maximum You ask the patient to identify your watch and your tie as you point to them. He correctly identifies both for two points. You ask the patient to repeat “No ifs ands or buts.” He repeats it accurately and completely for one point.. You hand the patient a paper towel and ask him to fold it in half twice and place it on the stool. He fold it in half twice and hands it to you. He receives 2 of the 3 points. You write on a paper “tap your toe three times”, he taps his toe three times for one point. You ask the patient to write any sentence on the paper. He performs this with a legible sentence for one point. You draw interlocking pentagons on a piece of paper and ask him to copy it, he does so correctly. The patient receives a 24 on this exam. You do not believe the patient is demented. The Alzheimer’s Association has developed a list of warning signs that include common symptoms of Alzheimer’s disease: 1. Memory loss that affects job skills--frequent forgetfulness or inexplicable confusion at home or in the workplace. 2. Difficulty performing familiar tasks - e.g. prepare a meal and not only forget to serve it, but also forget they made it. 3. Problems with language--forgetting simple words or substitute inappropriate words, making his or her sentences difficult to understand. 4. Disorientation to time and place -getting lost on their own street, not knowing where they are, how they got there or how to get back home. 5. Poor or decreased judgment-- dressing inappropriately in noticeable ways, wearing a bathrobe to the store or several blouses on a hot day. 6. Problems with abstract thinking-- trouble recognizing numbers or performing basic calculations. 7. Misplacing things-- putting items in inappropriate places - such as an iron in the freezer or a wristwatch in the sugar bowl - then not recall how they got there. 8. Memory loss that affects job skills--frequent forgetfulness or inexplicable confusion at home or in the workplace. 9. Difficulty performing familiar tasks - e.g. prepare a meal and not only forget to serve it, but also forget they made it. 10. Problems with language--forgetting simple words or substitute inappropriate words, making his or her sentences difficult to understand. 11. Disorientation to time and place -getting lost on their own street, not knowing where they are, how they got there or how to get back home. 12. Poor or decreased judgment-- dressing inappropriately in noticeable ways, wearing a bathrobe to the store or several blouses on a hot day. 13. Problems with abstract thinking-- trouble recognizing numbers or performing basic calculations. 14. Misplacing things-- putting items in inappropriate places - such as an iron in the freezer or a wristwatch in the sugar bowl - then not recall how they got there. 15. Changes in mood or behavior-- exhibit rapid mood swings for no apparent reason. 16. Changes in personality-- personalities may change dramatically, either suddenly or over a period of time. Someone who is generally easygoing may become angry, suspicious or fearful. 17. Loss of initiative - becomes uninterested and uninvolved in many or all of his usual pursuits. The pathology of Alzheimers Disease: On histological examination, one can find granulovesicular degeneration, neurofibrillary tangles, senile neuritic plaques, and microvascular amyloid. On gross examination of the brain, diffuse cortical atrophy is apparent. The Genetics of Alzheimer Disease The apoE-e4 allele, which provides an important susceptibility factor for late-life Alzheimer’s, three gene abnormalities have been identified as responsible for early-onset familial clusters of the disease. Testing for the apolipoprotein E (APOE) gene, when used in conjunction with other tests, may be useful in diagnosing Alzheimer’s disease in people displaying symptoms of dementia. Consensus statements developed at a Conference on Apolipoprotein E Genotyping in Alzheimer’s Disease in October 1995: "The usefulness of APOE genotyping for predicting risk of [Alzheimer’s disease] in asymptomatic individuals has not been established in longitudinal population-based studies and as such is not recommended...at this time." There are several reasons the APOE test should not be used as a predictive test. People who carry the APOE-e4 gene, considered a risk factor for Alzheimer’s, may not develop the disease. Furthermore, people who do not carry APOE-e4 may still develop Alzheimer’s, so not having APOE-e4 does not mean that individuals are risk-free. Since the APOE test cannot be used for prediction, sharing test results may be unduly alarming or comforting to the individuals being tested. The consensus statements recommend that "adequate pre-test and post-test counseling, education and psychosocial support" be provided with all applications of APOE testing. Counseling should include a full discussion of the implications of the test for patients and their families and provide people with all the information they need ABOUT JOHN GALIMORE It is unlikely the patient has dementia with a 24 on his mental status exam. In addition the patient is quite active and continues to play a musical instrument, socialize, and perform work. His orientation has improved slightly, but you are concerned that it is still lower than what you would expect, you are concerned about other causes of mental status impairment. CONSIDER DEPRESSION AND SUICIDAL BEHAVIORS. You inquire about the patient’s mood and if he has been depressed. The patient’s history does not indicate depression or suicidal behaviors in the recent or distant past. Again the patient has hobbies, plays a musical instrument and socializes frequently. His wife states there are no marital difficulties or difficulties in the family. A helpful pneumonic for the signs and symptoms of depression is SIG E CAPS. Sleep – may be an increase or a decrease in amount/quality of sleep Interest – less interest in doing things they used to enjoy Guilt – feelings of guilt or worthlessness Energy – decreased energy Concentration – decreased ability to concentrate Appetite – may be increased or decreased Psychomotor retardation – individual talks/thinks much slower than normal Suicidality – patient entertains thought of hurting themselves A positive finding of 4 of these signs/symptoms, in the presence of a depressed mood, is diagnostic for clinical depression. After careful history you do not believe this patient to be depressed. NEXT CONSIDER DELIRIUM. Delirium is a condition marked by alterations in level of consciousness, and its onset can be quite sudden and the symptoms may come and go. Importantly, delirium is often reversible while dementia is generally a progressive and irreversible disorder DELERIUM CAUSED BY DECREASED PERFUSION Delirium in this case may be caused by decreased perfusion or a TIA, by hypoxia, or by embolic event. This may also be caused by the medication. What are some inexpensive tests and exams that you should perform to evaluate the above? Multi-infarct dementia is the second-most common form (15 to 30% of all dementia cases) and occurs as a result of cerebral infarcts secondary to atherosclerosis. Hypertension predisposes a person to this disease. Deterioration is stepwise with periods of clinical plateaus. The most important here is the history. You must determine from Pearl, and from John if there has ever been any difficulty with confusion in the past. Have these events ever occurred before? She states he is confused at times in the morning. IF he did not have these symptoms before, it may well have been an effect of the medication and decreased perfusion secondary to the decreased heart rate and low blood pressure. You should evaluate the patient’s routine blood pressure (138 /80 at his last visit) and pulse (78 at his last visit) This may very well be a cause of his continued symptoms, however you must evaluate further as he has had these symptoms in the morning before. The patient has no bruits, relates no numbness weakness or tingling of his extremities, and no speech alteration. It does not give a history of a typical TIA. You may wish to order a CBC to rule our infection/sepsis or an anemia that might affect perfusion. This is a simple inexpensive test. You may wish to perform an urinalysis to screen for renal problems. UA was normal. CONSIDER THE METABOLIC CAUSES. Delirium from metabolic imbalances include hypoxia, hypoglycemia, hyperglycemia with ketosis, and hepatic or renal disease. A simple laboratory Chemistry usually identifies the 6 (to 12) most common test for an inexpensive panel. (Glucose-electrolytes, bun, creat, liver enzymes, calcium) The glucose was normal, the electrolytes were normal, and the bun and creatinine were normal. You will want to do a thyroid panel and it is sent to the laboratory. You will not have immediate results from this test. CONSIDER HYPOXIA The patient could have hypoxia from more than one reason. He has a history of smoking and likely has a degree of COPD. In addition the patient is obese and may have sleep apnea which can result the morning confusion she describes. A simple test you might perform would be a pulse oximetry. This however will only tell you the patient’s current condition. If you are suspicious of sleep apnea, you should order a sleep study to evaluate for this condition. You order this test, it will be performed later this week. CONSIDER HEAD INJURY OR TUMOR The patient and Pearl both give a negative history for injury. You cannot find any evidence of injury. The fundascopic exam was normal. The remainder of the neurological exam was normal. There is not headache or other accompanying symptoms. Should you not find an answer from the hypoxia study, or if symptoms of confusion were to persist, you might want to get a MRI of the brain to rule out a cerebral bleed or tumor. Because John has no evidence of a focal neurological lesion and no history of trauma, you decide not to pursue a CT or MRI at this stage. FINAL DIAGNOSIS AND DISPOSITION The sleep study you performed was abnormal. The patient had several episodes of hypoxia during the night with occasional spells of apnea. You ordered for night-time oxygen with Bi-PAP. John was placed on a diet to improve his BMI as his body habitus was an important factor. John was also to watch his lipid and cholesterol intake and to begin a walking program. The patients post studies were normal. Your follow-up exam with the patient and his wife was negative for any further episodes of confusion. The patient reported increased energy and had lost weight and was following his diet more appropriately. SUMMARY AND RECOMMENDATIONS Delirium is a clinical syndrome caused by a medical condition, substance intoxication or withdrawal, or medication side effect that is characterized by a disturbance of consciousness with reduced ability to focus, sustain, or shift attention. Nearly 30 percent of older medical patients experience delirium at some time during hospitalization. The incidence is higher in those with advanced age and pre-existing brain disease A disturbance of consciousness and altered cognition are essential components of delirium. Some patients are drowsy and lethargic, others are agitated and confused. Visual hallucinations, tremulousness, and myoclonus/asterixis are variably present Focal or lateralized neurologic findings are not characteristic of delirium. A careful neurologic examination can also distinguish between focal syndromes that can mimic delirium. The past medical history, a review of medications, and a physical examination may provide clues as to the underlying etiology Laboratory evaluation in patients with delirium should include serum electrolytes, creatinine, glucose, calcium, complete blood count, and urinalysis and urine culture. Drug levels, toxicology screen, liver function testing, and arterial blood gas should follow if the cause remains obscure. Neuroimaging, lumbar puncture, and electroencephalogram are not required in most patients with delirium, but are recommended in specific clinical scenarios, including in those whose cause remains obscure after routine testing. Uptodate.com Readings: Rakel’s Textbook of Family Medicine pp 2010 - 2013