1. Describe the both the conducting and
advertisement

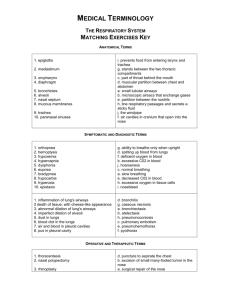
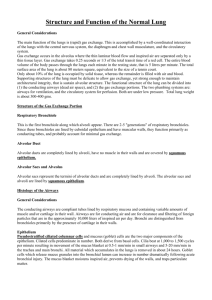
Pulmonary Week 2: Airways Disease Pulmonary Week 2 1. Describe the both the conducting and respiratory components of the respiratory tree including their histological appearance and explain the functional significance of each of these components. Conducting o Nasal cavities and sinuses Mucous controls inhaled debris and microorganisms Cavities and sinuses warms and humidifies inhaled air Olfactory bulb provides sense of smell o Nasopharynx Warms and humidifies inhaled air o Oropharynx Junction at which the esophagus meets the laryngeal orifice o Larynx Contains the vocal folds, an essential part of phonation Vocal folds (“vocal cords”) is the last barrier which prevents aspiration of foreign objects down into the trachea Momentary closure of vocal folds is important in completing the val salva maneuver o Trachea Anterior and lateral—12 to 20 hyaline cartilage “horseshoe” rings Posterior—a smooth muscle called “trachealis” that bridges the horseshoe ring gap, controls lumen size, and aids in coughing Lumen is lined by mucosa (respiratory epithelium, basement membrane, and richly vascular lamina propria), then submucosa (loose CT and seromucous glands that deliver secretions to mucosal surface), then finally adventitia (protective CT, i.e. cartilaginous rings) o Bronchi Right and left “mainstem” lobar segmental Walls of larger bronchi contain irregular rings of hyaline cartilage Walls of smaller bronchi contain plates and islands of cartilage Similar to the trachea, the lumen is lined by mucosa, then submucosa, and finally adventitia There is a gradual reduction in goblet cell propensity in the mucosa as we move away from the trachea, and an increase in Clara cells Lamina propria within the mucosa layer contains elastic fibers and lymphoid nodules Seromucous glands in the submucosa still connect to surface Smooth muscle completely encircles lumen o Bronchioles Diameter size ≤ 1 mm No cartilage or submucosal glands Cuboidal ciliated epithelium in place of simple columnar Goblet cells replaced by Clara cells (secretory & non-ciliated) Clara cells: dome-shaped, degrade toxins, reduce surface tension and serve as mitotic stem cells Smooth muscle arranged helically and complete encircles lumen 1 Pulmonary Week 2: Airways Disease Respiratory o Respiratory bronchioles Bronchioles which contain alveolar protusions Otherwise similar to bronchioles o Pulmonary alveoli (alveolar ducts, alveolar sacs, alveoli proper) Small air sacs (200 µm in diameter) Lined by simple epithelium called pneumocytes (two types) Inhabited by “Dust cells” of the immune system Thin walls separate a cluster of alveoli—they contain pulmonary capillaries and elastic fibers and they are called “interalveolar septae”) 2. Describe the embryological development of both components of the respiratory tree. 4 week old embryo o Tubular outgrowth emerge from primitive digestive tract o Tubular outgrowth form laryngo-tracheal diverticulum and lung buds o Foregut endoderm forms innermost layers of respiratory tree o Splanchnic mesoderm forms stroma, smooth muscle, and cartilage 3. Describe the composition and histological appearance of the respiratory mucosa and explain how it provides the muco-ciliary clearance mechanism. 30% Columnar Ciliated Cells o Cilia projections contains 9+2 microtubules, beats rhythmically o These structures move mucus and trapped matter towards nasopharynx 30% Goblet Cells o Secretes mucus to trap debris and microbials, protect the cells below 30% Basal Cells o Stel cells for renewal and regeneration 10% Other Cells o Mostly hormone producing APUD cells 4. In microscopic sections, differentiate between the trachea, bronchi, bronchioles and pulmonary alveoli. Trachea—large, muscular, cartilaginous, respiratory epithelium Bronchi—smaller, muscular, cartilaginous Bronchiole—microscopic, muscular, not cartilaginous Pulmonary alveoli—microscopic, not muscular or cartilaginous, RBCs 5. Describe the muco-ciliary clearance mechanism and factors that affect it in disease states. Goblet cells in conducting airway secrete mucous Mucus traps debris, toxins, and invading microorganisms Cilia on ciliated cells beat towards the nasopharynx to continually expel mucus Factoid! The debris tend to move upwards in a spiral pattern Chronic insult (i.e. smoking) lead to the dysfunction of this mechanism o Mucus no longer effectively moved up the respiratory tree 2 Pulmonary Week 2: Airways Disease 6. Describe the structure and ultra structure of the two types of pneumocytes and the alveolar macrophage cells and their roles in health and disease states. Type 1 Pneumocytes o Thin and flattened (80 nm wide) o Line 95% of the alveolar surface o Linked by tight junctions o Minimal thickness at 0.5 µm facilitates rapid gas exchange Type 2 Pneumocytes o More numerous but line only 5% of alveolar surface o Secrete surfactant to reduce surface tension and prevent alveolar collapse o Surfactant reduce surface tension at the alveoli and thus prevent the alveoli from completely collapsing on exhalation and allows them to be reopened with a lower amount of force o A lack of surfactant results in collapsed air spaces alongside hyperexpansion and vascular congestion Dust cells o Resident macrophages that absorb debris, attack invading microorganisms, and release inflammatory factors to initiate an immune response o Loss of Dust cell population makes the lung more prone to infection 7. Describe the key features of the blood-air barrier and indicate the functional significance of surfactant. <Histology Booklet p. 22, 53> The Blood-Air Barrier is minimal in thickness (0.5 u) which provides rapid gaseous exchange between pulmonary capillary and pulmonary alveoli 4 components: (1) Type 1 Pneumocyte with tight junction – attenuated cytoplasm (i.e. appears think & flattened), covering about 95% of surface area of a pulmonary alveoli - Covered by a thin layer of surfactant secreted by Type II pneumocyte (2) Basement membrane of Type 1 Pneumocyte May be fused together (3) Basement membrane of pulmonary capillary endothelial cells (4) Pulmonary capillary endothelial cell – enclosing capillary lumen - The tight junction prevents indiscriminate fluid leakage Type 2 Pneumocyte: produces surfactant that surface tension prevent alveolar collapse during expiration when air is being squeezed out of the alveoli 8. Specify the main components of total resistance offered to flow of air in and out of the lungs and describe the relationship between flow, driving pressure and resistance. Keys Mechanical factor contributing to air flow in & out of lungs: 1) Elastic recoil of lungs 2) Elastic recoil of chest wall 3) Total resistance to airflow Air molecules require energy to move forward to begin air flow, resistance (an opposing energy) must be overcome o Total resistance to airflow in & out of lungs have 3 components: (1) Inertia of the respiratory system (negligibly) (2) Tissue resistance of the lungs & chest wall (20%) Please see obj 10 for explanation (3) Airways resistance (80% - can tremendously in both health & disease 3 Pulmonary Week 2: Airways Disease In general, resistance R = P/ Flow, where R = resistance, & P= the pressure difference or driving pressure. ** R is only meaningful during airflow (unit = cm H20/L/sec) Total resistance is R = PA - PB / Flow, where PA is alveolar pressure, PB is barometric pressure or atmospheric pressure at the airway opening (typically the mouth) Resistance offered by healthy lungs during quiet inspiration (2 cm H20/L/sec) is very small compared to that of smoking pipe (500 cm H2O/L/sec) for a given flow rate o This small resistance is mainly due to the anatomic arrangement of the tracheobronchial tree o In a branched system of tubes (e.g. our airways), frictional resistance depends on: (a) individual resistance of each tube (b) the ways in which the tubes are connected o A branching system can be connected in two ways: 1) In series: Rtotal= R1 + R2 + R3 etc… (Total resistance of the system = the sum of each individual resistance). 2) In parallel: 1/Rtotal = 1/R1 + 1/R2 + 1/R3 etc... (Total resistance of the system << any individual single resistance. E.g. R1 = R2 = R3 = R4 = 2 1/Rtotal = 1/R1 + 1/R2 + 1/R3 + 1/R4 = 1/2 + 1/2+ 1/2 + 1/2= 4(1/2) = 2 Since 1/ Rtotal = 2 Rtotal = 1/2 *The general rule: if you have 4 identical R set up in parallel R total of the system = ¼ of a single R. Now, 20 identical R in parallel R total = 1/20 of a single R and 100 identical R in parallel R total = 1/100 of a single R 9. Describe the relationship between total cross sectional area, airways resistance and airflow velocity in the bronchial tree (A system of branching tubes) Resistance in a single tube is inversely related to the radius of the tube to the 4th power (R α 1/r4) o radius, diameter, or cross sectional area of the tube resistance. o Consider how our airways branch from the trachea to the alveoli: o At each new branch point, the daughter airways that arise from that same branch point belong to the same generation. o The airways of the same generation tend to be of the same size. o # of branches as we move from the trachea to the pulmonary alveoli o Also, the radius, diameter & cross section of the individual airway gets progressively smaller 4 Pulmonary Week 2: Airways Disease A small diameter usually causes a higher resistance, but the large number of parallel airways in that generation reduces the overall resistance. o Because the branching airways are arranged in parallel # of branches overall resistance o Remember, if you have 100 branches arranged in parallel having identical resistance (R) R total of system = 1/100 of R o As we move from trachea to alveoli, the total resistance become almost insignificant at the alveoli o Most of the overall airway resistance comes from the Upper Respiratory Tract & generations 0 through 6 where total cross sectional area of the generation is relatively small. o Enormous expansion of the sum of the cross sectional area of parallel airways from about 2.5 cm2 in the trachea to 180 cm2 at about generation 16, the end of the conducting zone o Affects airways resistance o ALSO impact on airflow velocity Velocity of air thru a series of branching tubes in parallel is similar to resistance Airflow velocity 1/total cross sectional area and R 1/total cross sectional area Airflow velocity & Resistance as the total cross sectional area as we move from trachea to alveoli Why airflow velocity? Check out: http://sprojects.mmi.mcgill.ca/resp/bernoulli_effect.htm **Important: As air moves from trachea to the distal airways, airflow velocity . In the respiratory zone of lung, convective flow stops & diffusion is the main mode of gas movement The parallel arrangement of the tracheobronchial tree optimizes the conflicting demands of the lung by having: 1) A small volume of airway that does NOT contribute to gas exchange (the conducting zone) 2) A small resistance to accommodate the flow of large amounts of air into respiratory zone As air moves from alveoli to trachea, airflow velocity allowing air to exit in reasonable time period through the relatively small airway volume of the conducting zone. o 5 Pulmonary Week 2: Airways Disease 10. Define tissue resistance of the lungs and explain why it is inversely related to lung volume. Lung tissue resistance = the resistance offered by lung tissue as it expands Lung tissue resistance varies w/ lung volume Lung tissue resistance as lung volume , 2 reasons for that: (1) The tethering effect of the alveoli o At high lung volumes, the alveoli are more distended and the elastic recoil tension in their walls is higher. o In our lungs, airways are surrounded by and attached to alveoli The airways are thus pulled open by the high tension in the distended alveolar walls of their neighboring airways o As lung volume , the tension in the alveolar attachments to the airways , pulling the airways open outwards o This airway diameter and resistance (R α 1/r4) o At lower lung volumes approaching RV, the elastic recoil tension in the alveolar wall is less o Thus, airways are narrower and contribute more to airway resistance o Some airways may even begin to close at such low volumes especially at the bottom of the lungs where the lungs are less expanded 6 Pulmonary Week 2: Airways Disease (2) The change in the parasympathetic tone o Airways are surrounded by a smooth muscle layer innervated by the PSN system o PSN smooth muscles to actively contract constricts the airways o Stretch receptors (mechanoreceptors) within this smooth muscle layer detect changes in lung volume o During inspiration when lung volume these mechanoreceptors neural firing rate PSN signals to the smooth muscles constriction of airways airflow resistance o During expiration, lung volume PSN signals smooth muscle constriction & air flow resistance 11. Distinguish between airflow and airflow velocity and describe the key features of laminar and turbulent airflow, where they typically appear in the airways and where they change in disease. Flow rate = amount of fluid (ml) moving per sec o [Flow rate = ml/sec]. Flow velocity = distance fluid travels in 1 sec o [Velocity = flow rate / cross-sectional area of the tube (cm2) =cm/sec]. Air is a fluid follows the principles of fluid dynamics as it moves in and out of the lungs. In the airways, flow will occur when a pressure difference exists between one point along the airway and another (driving pressure), from higher pressure to a lower pressure. Flow can exist in three patterns: Laminar Flow, Tubulent Flow, Disturbed Laminar Flow (1) Laminar Flow o This type of flow occurs in smooth tubes and at LOW flow rates. o Flow in small airways diameter < 2mm) is laminar, silent & slow o The flow is streamlined and there is no turbulence. The flow occurs in parallel layers, with minimal disruption between these layers. o The flow rate is greatest at the centre and diminishes towards the periphery laminar flow is described as having a bullet shaped or parabolic "velocity profile" o In Latin, laminae = layers o Laminar flow = circular layers of fluid movement w/ the fastest being in the center to the slowest at the walls of fluid movement o During laminar flow the relationship between driving pressure and flow is linear, ΔP α ΔV o driving pressure, flow will proportionally (2) Turbulent Flow o This type of flow occurs in rough tubes and at higher flow rates. o Flow in the large airways such as the trachea is turbulent, fast and noisy o The flow is not streamlined and there is lot of swirling (eddies) of the fluid. o The flow is not greatest at the centre "velocity profile" of turbulent flow is more flat (or more blunt) than that caused by laminar flow. o Fluid flow in both axial & radial direction o Fluid velocity is on average the same everywhere in tube 7 Pulmonary Week 2: Airways Disease o o The radial component of turbulent flow constantly impacts the walls of the tube and consumes energy, therefore, a higher pressure difference is needed to maintain a given flow rate. The relationship between driving pressure and flow in turbulent flow is alinear: ΔP α V2 o To double the flow under turbulent conditions the pressure difference must be > 2X. ** P greater laminar flow compared to turbulent flow because some of the P in turbulent flow is expended in generating radial flow (3) Disturbed Laminar Flow o A combination of laminar and localized turbulent fluid movements referred to as eddies. o Eddies occur where the tube either narrows, branches, or where there are irregularities in the tube surface. o This type of flow represents a mix between laminar and turbulent flow and is present in the majority of airways. 12. Explain how indices obtained from the expiratory force vital capacity help determine whether a patient has an obstructive ventilatory defect During expiration, the more effort healthy individuals put into contracting their expiratory muscles can force air out of their lungs at greater flow rates This efforts affects flow rate at high lung volumes This efforts DOES NOT affect flow rate at low lung volumes o Here flow rate is independent of effort due to air flow limitation In the clinical setting, patients are routinely asked to perform a forced expiratory vital capacity maneuver, emptying their lungs as rapidly and forcefully as possible from maximal inspiration to maximal expiration to determine the degree of air flow limitation. There are two important measurements obtained from the Pulmonary Function Test (PFT): FEV1 & FVC FEV1 = forced expiratory volume in 1 sec FVC = forced vital capacity used to estimate Vital Capacity (VC) FEV1/FVC ratio = % of VC is expired in 1st sec – used to differentiate between abnormal patterns of ventilator defect **Other measurements include FEF25-75% 8 Pulmonary Week 2: Airways Disease Pulmonary Function Test Results Obstructive Lung Disease Disproportionate FEV1 compared to FVC Low FEV1 Low FEV1/FVC ratio Asthma Episodic FEV1/FVC ratio improves with bronchodilator; worsens with bronchoprovocation Restrictive Lung Disease Low lung volumes & capacities Low FEV1 Normal or Above Normal FEV1/FVC ratio Normal or low DLCO COPD Chronic Bronchitis Sputum production Normal DLCO High RV & FRC 9 Emphysema Lung compliance curve shifted to left Low DLCO (alveoli wall destruction High TLC, RV, FRC (lung hyperinflation) Pulmonary Week 2: Airways Disease 13. Define dynamic compression of the airways using the equal pressure point hypothesis and specify the factors that affect airflow limitation in health and disease. Note: from www.sallyosborne.com “Airways Resistance and Airflow through the Tracheobronchial Tree” Equal Pressure Point Hypothesis: =points along the airways at which the intrapleural P is equivalent to airway P -as lungs empty, Equal Pressure Point moves from larger to smaller airways towards alveoli -increases dynamic compression of the airways ->results in airway collapse or closure Dynamic Compression of the airways: -develop close to the equal pressure point where intrapleural P EXCEEDS airway P AND -inadequate cartilaginous support or traction provided by neighbouring alveoli Factors that affect airflow limitation in health and disease: 1) Inertia of the respiratory system 2) Tissue resistance of the lungs and chest walls/ Lung Compliance 20% -↓ in elastic recoil of lungs ↓ its contribution to a greater P in the airway vs. intrapleural P -> Greater dynamic compression 1) Airways Resistance 80% -the greater the resistive drop in P along the airway from alveolus to Equal P Point -the sooner the development of an Equal P Point -the greater the dynamic compression 14. Compare and contrast the histological sections of the auditory tube, olfactory mucosa, epiglottis, and larynx. Auditory Tube Olfactory Mucosa Respiratory Epithelium 1) tall columnar cells w/ apical cilia 2) goblet shaped cells (palestaining) 3) small, rounded basal cells on bm underlying basement membrane Lamina Propria -loose CT -cellular + highly vascular modified, extra-thick pseudostratified epithelium 1) olfactory receptor cells -true bipolar neurons -nuclei in centermost layer -apical process w/ non-motile cilia receptive to odoriferous stimuli 2) supportive cells -mechanically support receptive cells 3) small basal cells -base of epithelium -stem cells for olfactory receptor cells lamina propria 1) unmyelinated axons from receptor cells Epiglottis lingual surface: stratified squamous nonkeratinizing epithelium undersurface: from the above to stratified columnar to pseudostratified ciliated columnar epithelium 10 Larynx False vocal cords True vocal cords Respiratory Stratified Mucosa Squamous NonKeratinizing Epithelium towards the laryngeal ventricle, epithelium changes to Pseudostratified type lamina propria -cellular + highly fibrous Pulmonary Week 2: Airways Disease =axons of cranial nerve I 1) many small blood vessels 2) serous glands of Bowman -watery surface secretion bony tissue of nasal concha sero-mucous glands central core of elastic cartilage sero-mucous glands central core of CT -mostly elastic fibers -some skeletal muscle (vocalis muscle) 15. Describe the histological features of the trachea with special reference to mucosa, submucosa and adventitia Mucosa epithelium basement membrane lamina propria (highly vascular) (30%) goblet cells: mucus Submucosa mostly loose CT Adventitia outer protective CT seromucous glands: secretions 12-20 hyaline cartilage horseshoe rings smooth muscle (Trachealis) -bridges gap -controls lumen size (30%) respiratory epithelium/ pseudostratified ciliated columnar epithelial cells (30%) basal cells - stem cells (10%) others -mostly hormone producing APUD (amine precursor uptake decarboxylation?) cells 16. Discuss the hilus of the lung with special reference to histological appearance of the main bronchi. Hilus of Lung The site where major blood vessels, bronchi, nerves and lymphatics enter or emerge from the lung. Main Bronchi: Structurally similar to the trachea with 2 exceptions: 1. the arrangement of cartilage into small plates 2. the circular arrangement of smooth muscle, which completely envelops the lumen and is submucosal in location. 11 Pulmonary Week 2: Airways Disease 17. Describe the essential histological features of the lung with special reference to intrapulmonary bronchi and bronchioles. 18. Contrast the main cell types in the respiratory epithelium of the bronchus with those of the bronchioles. Lung spongy, honeycomb-like network contains tubular structures of different sizes and at different levels of histologic organization consists of millions of alveoli Bronchi Bronchioles respiratory epithelium reduced in height gradual reduction in # of goblet cells Elastic fibers and lymphoid nodules in lamina propria Seromucous glands connect to surface Smooth muscle completely encircles lumen Irregular hyaline cartilage plates Simple columnar to simple cuboidal epithelium Goblet cells replaced by Clara cells Lamina propria rich in elastic fibers No submucosal glands Smooth muscle arranged helically and completely encircles lumen No cartilage 19. Discuss the causes and mechanisms of cough and chronic sputum production. Cough Can be voluntary or reflexive o afferent: stimulate irritant receptors in airway, travels up CN X (vagus) o efferent: activate inspiratory muscles and diaphragm, via phrenic nerve o activate expiratory muscles, larynx, CN X (vagus) – recurrent laryngeal nerve Phases of cough 1. Inhalation of gas (Not a critical component of cough) – inspire a LARGE volume of gas 2. Compressive - GLOTTIS is CLOSED; isometric contraction of the expiratory muscles increases intrathoracic pressure up to 300 mm Hg; expiratory effort against a closed glottis 3. Expiratory phase – GLOTTIS OPENED; high intrathoracic pressure causes a high expiratory flow rate Receptor location: most sensitive sites are larynx and tracheobronchial tree, especially the carina and sites of bronchial branching. Irritation on smaller airways and alveoli will not induce cough. Stimuli: cig smoke, ammonia, ether vapour, acid/alkaline solution, mucus, dust, etc. ACEi induced cough likely due to accumulation in the lungs of bradykinin, substance P, and/or prostaglandins. Stops within 4 days of d/c drug. Chronic Sputum Production Mucus contains: mucus glycoproteins (mucins), water, and peptides Mucus moves from lower airways, trapping particles and travelling up mucociliary ladder, coughed up and swallowed 12 Pulmonary Week 2: Airways Disease Mucus is ↑ in chronic bronchitis due to ↑ production of mucins and ↑ secretion from goblet cells. Stimuli include neutrophil elastase, LPS, cigarette smoke, oxidative stress leading to goblet cell metaplasia and mucus hypersecretion (also caused by smoking) Chronic inflammation can lead to formation of pus and contribute to purulent sputum 20. Discuss the pathogenesis (mechanism of which disease is caused) of COPD, asthma, bronchiolitis obliterans, and bronchiectasis COPD Is essentially due to the inhalation of noxious particles and gases, especially smoking and occupational hazards Along with host factors (ie. Alpha 1 antitrypsin deficiency/genetic factors), lead to lung inflammation oxidative stress and proteinases affect the lung Squamous metaplasia results in response to smoke exposure Lung parenchymal damage decreases diffusive capacity (↓ DLco) Glandular enlargement and goblet cell hyperplasia excess mucus production Asthma Inflammatory condition associated with allergies, genetics, viral infections; often precipitated by stress or exercise Exposure to an antigen/irritant results in the release of histamine/leukotrienes/growth factors leading to airway smooth muscle constriction Can be accompanied with pulmonary vascular dilation and leakage, ↑ mucus secretion, and airway remodelling if chronic Largely a reversible condition with drugs or spontaneously Lung parenchyma is often not affected Smooth muscle hypertrophy leads to hyperreactive airways Goblet cell hyperplasia ↑ mucus production, may form plugs Bronchiolitis Obliterans Chronic inflammation of bronchioles that can obstruct the lumen Caused by inhalation of noxious substances, infection, connective tissue disease, chronic rejection, adverse drug reactions, or idiopathic Inflammation results in edema and movement of cell substances to obstruct airway lumen Smooth muscle hyperplasia, bronchiolectasis, fibrosis due to inflammation Bronchiectasis Irreversible ilation of the bronchial tree Due to infection, obstruction, congenital defects, immunodeficiency, connective tissue and immune disorders (common in cystic fibrosis) Neutrophils release mediators that cause inflammatory reactions and destroy the structure of bronchial walls ↑ susceptibility of infection Often will find fluid filled dilated bronchi, ↑ sputum production, hemoptysis 13 Pulmonary Week 2: Airways Disease 21. Correlate the patho-physiological process in the obstructive lung diseases with the changes observed in physiological measurements ALL obstructive disease have a) low FEV1/FVC1 b) low PEF o This is because there is an object/buildup/remodeling that decreases the ability of the lungs to expire air rapidly i) Asthma ○ Why Low FEV1/FVC1? Asthma is condition involving airways – chronic inflammation, remodeling (including a) increased smooth muscle around bronchioles which spasm, b) increased ECM/basement membrane) – ultimately leading to airway wall thickening ii) COPD a) Chronic Bronchitis ○ Why normal DLCO? Parenchyma not affected ○ Why high RV, FRC? Excess mucous (hypertrophy of mucous glands & goblet cell metaplasia), airway inflammation difficulty expiring air lung hyperinflation with air trapped at end of expiration b) Emphysema ○ Why low DLCO? Parenchyma affected ○ Why high TLC, RV, FRC? Inflammation proteinases (e.g., elastase) mucous plugging, narrowing, decreased elasticity/increased compliance, damage parenchyma decreased “tethering” to keep airways open when intrapulmonary pressure increases to expire, airways collapse 22. Describe the role of smoking on the pathogenesis of COPD. Smoking Tobacco smoke in airway hypertrophy of mucous glands & goblet cell metaplasia (to remove irritant) excessive mucus in bronchial tree + cough chronic bronchitis ↑ [free radicals] in tobacco smoke oxidative stress and damage to lungs Tobacco smoke (irritant particles) in airway body response = cytokine release + chronic airway inflammation remodelling + thickening small airway disease (chronic bronchiolitis) Tobacco smoke & free radicals ↓ activity of antiprotease enzymes (i.e. alpha 1antitrypsin) protease damage lung destruction to alveolar wall ↓ lung recoil emphysema Emphysema & small airway disease ↓ expiratory flow; hyperinflation; gas exchange abnormalities cough, sputum, dyspnea, wheeze 23. Understand the importance of the immune system in the pathogenesis of asthma “Allergic asthma”: type I hypersensitivity reactions cytokines from Th2 Cd4+ cells such as IL-4, IL-5, IL-3 IgE created stick to inflammatory cells (e.g., mast cells) histamines, and leukotrienes etc released w/ exposure to allergen airway narrowing o (Smooth muscle contraction, airway wall edema, increased mucus, recruitment of additional inflammatory cells). 14 Pulmonary Week 2: Airways Disease 24. List the major drug classes used in the management of asthma/COPD Class – Prototype SABA (Short acting β2 agonist) salbutamol MOA SE/safety Pharmacokinetics Binds β2 receptor, activates adenylate cyclise to ↑ cAMP ↑ bronchodilation - Well tolerated - tachycardia - palpitations (↓ β2 selectivity-↑ dose) - tremor Onset in ≤5 minutes, used acutely LABA (Long acting β2 agonist) – salmeterol, formoterol Same as SABA, with ↑ β2 selectivity - same as SABA Inhaled corticosteroids – budesonide, fluticasone @ nucleus to inhibit expression of proinflammatory cytokines (COX2) - oral thrush (candidiasis) - dysphonia (hoarseness) - long term SE, osteoporosis Diskus, DPI salmeterol is slow acting formoterol is fast acting, can use as rescue tx MDI, DPI, diskus Systemic corticosteroids – prednisone Same as ICS Anticholinergics – iptratropium, tiotropium Antagonizes muscarinic receptors M1 bronchodilation M3 ↓ bronchial secretions Phosphodiesterase (PDE) Inhibitor, slows breakdown of cAMP ↑ bronchodilation - osteoporosis - fat redistribution “moon face” - obesity “buffalo hump” - hyperglycemia - and many more! - dry mouth Slower onset of action Dissociates from receptor more slowly than SABA lasts 12 hours not for rescue/acute - Treats inflammatory component of asthma, needs to be used regularly (twice a day dosing) - Immunosuppressant - significant metabolic effects - less bronchodilation, more SE, slower onset of action compared to ICS - slower onset of action than SABA - tiotropium is longer acting (once a day dosing) MDI, DPI, nebules Methylxanthines - theophylline - narrow therapeutic range - nausea, vomiting - stimulatory; insomnia, tremor, restlessness - cardiac arrhythmias - lots of drug interactions! 15 Mode of Delivery/Other MDI, diskus, nebules, DPI If used >3 times/week, need ICS therapy oral oral Pulmonary Week 2: Airways Disease Leukotriene receptor antagonists (LTRA) – montelukast Monoclonal antibodies – omalizumab Blocks lipoxygenase pathway, leading to ↑ bronchodilation Binds to allergen/antigen to stop interaction with IgE = no allergic response - headache oral - possible immune/injection site reactions (45%) - viral infections (24%) - URTI (19%) - headache (15) - subcutaneous injection every 2-4 weeks - expensive Combination therapy ICS + LABA – chronic B2 agonist use can lead to receptor downregulation, so use ICS to upregulate β2 receptors in the lung; also, β2 agonist dilates airways, ↑ ICS deposition fluticasone + salmeterol (Advair) budesonide + formoterol (Symbicort) MDI- Metered dose DPI – dry powder Diskus Nebulizer inhaler inhaler - ≤10% of dose reaches alveoli (depends on particle size; smaller = ↑ drug to target) - needs coordination - can use aerochamber for young or elderly - patient controlled - coordination not as demanding - fine powder; not obvious the dose has been delivered - patient controlled - coordination not as demanding - fine powder; not obvious the dose has been delivered - inconvenient - not portable - used for young patients 25. Describe mechanism of action of drug classes used in asthma/COPD 26. Describe major side effects and safety issues with these agents 27. Describe pharmacokinetic issues, modes of delivery MOA Bronchodilator: β agonists activate - epi: α&β agonist adenylate cyclase - isoproterenol: β1&β2 increase cAMP agonist bronchodilation - salbutamol Pharmacokinetics salbutamol: short acting (SABA) - onset minutes - acute use 16 Side Effects - Well-tolerated - Tachycardia/ palpitation with high dose - tremor Pulmonary Week 2: Airways Disease - salmeterol - ipratropium tiotropium - theophylline Corticosteroids - not anabolic - prednisone budesonide fluticasone ciclesonide salmeterol: long acting (LABA), 12h - high selectivity for β2 - not for acute use, slow onset Ipratropium (Atrovent) Local: dry mouth due to - minimize systemic decreased Ach absorption, nonselective for muscarinic receptor - M1 & M3 R: bronchoconstriction - M2 R: autoreceptor, feedback inhibition of Ach release Anticholinergic Tiotropium: - selective to M1&M3 R - long-lasting, better acting Theophylline: - strong coffee - Phosphodiesterase inhibitor: inhibit breaking down of cAMP Methylxanthine: Systemic (oral): - Prednisone - Act in nucleus - inhibit expression of pro-inflammatory cytokines & COX2 - immunosuppressant (beneficial) Inhaled: - budesonide, fluticasone (localized delivery, minimize systemic side effects - ciclesonide: prodrug activated by esterase in airway, minimize systemic&local side effects 17 - narrow margin of safety - nausea, vomiting, “stimulatory” (tremor, insomnia, restlessness) - cardiac arrhythmia - common & frequent drug interaction Prednisone: - Metabolic effects - osteoporosis - fat redistribution (moon face) - obesity - hyperglycemia Budesonide - oral thrush (candida) - dysphonia (hoarse voice) - systemic effects can still occur with long term use, osteoporosis Pulmonary Week 2: Airways Disease Leukotriene antagonists Leukotriene receptor allow oral dosing not as efficacious antagonist: Montelukast LT2 (leukotriene) - montelukast receptor : - mediates airway smooth muscle proliferation asthma Monoclonal Ab Omalizumab - subcutaneous injection - immune reaction - omalizumab - prevents interaction of every few weeks - high cost allergen with IgE Combination Therapy: Bronchodilator “opens up” - oral, injection, Chronic use of β2 - corticosteroid airways, facilitating inhalation (local effect) agonists may lead to (inhaled) + long-acting inhaled corticosteroid - size of particle receptor beta agonist: deposition (which matters: increase size, downregulation - Advair: fluticasone + increased β2 receptor) decrease ability to reach salmeterol target - Symbicort: budesonide - Nebulizer: vaporized + formoterol liquid, mask inhaled - Pressurized metered dose inhaler: aerosolized particles, needs coordination drug ends up at back of throat - Dry powder inhaler: not obvious that the dose has delivered Targets: bronchoconstriction, airway inflammation, mucous plugs, remodeling 28. COPD, asthma, bronchiectasis, bronchiolitis obliterans: definition, etiology, pathology, pathogenesis (risk factors), natural history 29. Compare and contrast asthma and COPD in adults 30. Clinical presentation, pulmonary function test, radiological finding Asthma Definition - Reversible airflow obstruction - bronchial hyperresponsiveness - chronic airway inflammation - airway remodeling COPD Chronic Bronchitis emphysema - largely caused by smoking, progressive, partially reversible airway obstruction & lung hyperinflation - Chronic Bronchitis: cough productive of 18 Bronchiectasis - Permanent dilation of bronchi with inflam changes in their walls and lung parenchyma - chronic airflow limitation Bronchiolitis obliterans - bronchiolitis obliterans: not COPD, occlusion of airway lumen by polyps rich in ECM - small airway (<2mm) disease (a Pulmonary Week 2: Airways Disease - airway, spare parenchyma sputum form of COPD) - emphysema: permanent enlargement of alveoli with wall destruction Etiology - 1-15% of pop. - smoking (pulmonary - infection - toxic inhalation - hygiene hypothesis inflammation) only 15- - bronchial obstruction - connective tissue (CD4+ T cell-medicated 20% heavy smoker - immune deficiency disease Th1/Th2 cytokine develop COPD - CF - chronic rejection balance shift to Th2 - occupation -Non-obstructive (allergic-type) response - α1-antitrypsin (infection or - familial extrinsic/ deficiency congenital): CF, allergic asthma onset - chronic infection by Kartageners’s (ciliary before age 30: allergy, virus or atypical dysfunction), immune increased IgE, + skin bacteria deficiency, necrotizing test pneumonia (TB, staph) - non-allergic/ intrinsic - obstructive: foreign asthma onset middle body, neoplasm, mucus age: environmental irritants (smoke, exercise, T) - viral exacerbation pathology - Fragile epithelium - squamous metaplasia - transmural -Cellular infiltrate - thickened basement - parenchymal inflammation - smooth muscle membrane damage - permanent dilatation hyperplasia - goblet cell hyperplasia - glandular enlargement - neo-vascularization - bronchiolectasis - smooth muscle - goblet cell - mucopurulent - fibrosis hypertrophy hyperplasia material - obliterative scarring - mucus cast - lymphoid follicle - airway smooth muscle - eosinophil, mast cell hypertrophy Pathogenesis - acute narrowing of - imbalance of - Recurrent - chronic fibrosis/ airway cough, proteolytic and antiinflammation of inflammation dyspnea, wheezing proteolytics bronchial walls & (neutrophil, - reverse spontaneously - neutrophils (release fibrosis of surrounding macrophage) with anti-inflam/ elastase) & macrophage parenchyma bronchodilator damage lung - weakened walls - inflam cytokine parenchyma during irreversible dilation secreted by Th2 inflammation airway smooth muscle - α1-antitrypsin (AAT) contraction, airway wall synthesized in liver, edema, increased bind irreversibly to mucus production, proteolytic enzyme and 19 Pulmonary Week 2: Airways Disease recruitment of inflam inactivate them cell to airway - Emphysema - stimulation of classification: parasympathetics centriacinar (smoking, - damaged airway epi upper lobes), panacinar decrease production of (AAT deficiency, lower bronchial relaxing lobes), paraseptal factors (distal acinar, tall thin young adults, bullae rupture spontaneous pneumothorax), paracicatricial (irregular, most common) Natural Cough, wheeze, dyspnea -progressive dyspnea - progressive dyspnea history - Paroxysmal - chronic bronchitis - daily mucopurulent - provoked - increasing frequency sputum - worse at night of exacerbation - infective exacerbation - weight loss - recurrent pleurisy - hemoptysis Clinical - wheeze - hyperinflation - often related to Presentation - hyperinflation during - wheezes infection: productive attacks - R heart failure cough, fever, - allergy - weight loss hemoptysis (erosion - hyper-resonance - CB (chronic through weakened - use accessory muscle bronchitis): daily cough bronchial walls into - sputum production productive of sputum vessels) - tachypnea for several months over - clubbing - tachycardia min 2 consecutive yrs - localized coarse - acute distress/ crackles confusion - wheezes Pulmonary - reversible airflow - partially reversible - Airflow obstruction Function obstruction airflow obstruction - restrictive Test - hyperresponsive - reduced diffusing - normal or reduced - normal DLCO capacity DLCO - increase TLC, FRC, RV - decrease elastic recoil - decrease VC decreased FEV1, - decrease FEV1, FEV1:FVC ratio, increase FEV1:FVC ratio TLC, FRC, RV - decrease flow rate Radiological - Normal CXR - hyperinflation - dilated bronchi Finding - bronchial thickening - emphysema bullae - fluid filled bronchi 20 - progressive dyspnea - unproductive cough - symptoms develop rapidly over months - wheezes - inspiratory squeaks - hyperinflation - fine crackles - irreversible airflow obstruction - reduced DLCO - gas trapping - mosaic perfusion Pulmonary Week 2: Airways Disease - mucoid impaction Treatment - incidental carcinoma - regional volume loss - corticosteroid (main - bronchodilator - bronchial hygiene Tx, takes time) - inhaled corticosteroid - Antibiotics - β2 agonist - Anti-inflammatories - methylxanthine - anticholinergic/ sympathomimetics - leukotriene antagonist - mAb - centrilobular nodules - bronchiectasis - bronchodilator - erythromycin - corticosteroids 31. Describe and explain how it is possible that the distinct clinical and pathological features of these conditions may overlap, and share features in common, particularly chronic airflow obstruction and chronic inflammation. These 4 clinical conditions overlap in terms of airflow obstruction and inflammation. INFLAMMATION COPD includes a chronic inflammation of the lung parenchyma, and can present as emphysema or obstructive bronchitis or bronchioitis Asthma is inflammation of the airways as well, leading to remodeling B ronchiectasis is chronic inflammation and/or infection resulting in permanent dilation and destruction of the bronchi Bronchiolitis, as described by its name, is the recurrent inflammation of the respiratory and membranous bronchioles OBSTRUCTION COPD presents with progressive and/or partially reversible airflow limitation, presenting as persistent dyspnea and exercise limitation Asthma presents as variable airflow limitation but with bronchodilator reversibility, with exacerbations triggered by the environment Bronchiectasis can present as either obstructive or restrictive airflow limitation, along with cough, sputum and/or hemoptysis Bronchiolitis, which can present together with bronchiectasis, involves irreversible airflow obstruction and presents similar to COPD 32. Compare and contrast the rationale for the differing approaches to treating asthma and COPD. COPD Involves a number of non-pharmacological and pharmacological approaches o Because it is well-known that there are many different triggers for COPD exacerbations. Vaccination (for both influenza and pneumococcal) for COPD infections may play role in causing exacerbations Pharmacological treatment is also common in COPD to reduce the frequency of exacerbations. ASTHMA: Goal of asthma management is to maintain control symptoms using the lowest dose of medication Need to identify and eliminate environmental triggers for asthma Come up with an action plan to dictate how the patient should deal with exacerbations 21 Pulmonary Week 2: Airways Disease 33. Explain why both pharmacological and non-pharmacological treatments are important in the management of patients with obstructive lung disease. Often, pharmacological treatments are not sufficient in the management of patients with obstructive lung disease because there are a lot of environmental factors can exacerbate COPD Therefore non-pharmacological treatments such as smoking cessation and vaccinations are important in the management of patients with obstructive lung disease Pharmacological treatments are also important as well primarily for the symptomatic treatment of COPD, and are also useful in the management of exarcerbations. 34. Compare and contrast the pathophysiology and response to therapy for persons with asthma and COPD. COPD Pharmacological treatment in COPD: short acting bronchodilators or long acting bronchodilators o β 2-agonists and anticholinergics o Evidence : combination of β2-agonists together with anti-cholinergics are more effective. o Inhaled corticosteroids can be used by COPD patients to reduce the frequency of exacerbations, but oral corticosteroids and antibiotics are primarily used only in the case of exacerbations o Oxygen is also used only when COPD patients become hypoxemic ASTHMA: Primarily: inhaled corticosteroids as an anti-inflammatory + fast acting bronchodilator (short acting β2-agonist) for the acute relief of symptoms Evidence for combined inhaled corticosteroids + long acting β2-agonists for long-term treatment 35. Describe the indications, contraindications, benefits and side-effects of influenza and pneumococcal vaccine in COPD Influenza vaccines should be given annually to COPD patients o Reduce exacerbations o No evidence for reduced mortality or hospitalizations. Pneumococcal vaccinations should be given every 5 to 10 years no RCT evidence of benefit Contraindications: hypersensitivity to any component, acute febrile or neurological illness 36. Differentiate the gross and microscopic findings in COPD, asthma, bronchiolitis and bronchiectasis. COPD – chronic inflammation of airways and lung parenchyma, leading to progressive airflow limitation and loss of elastic recoil, and hyperinflation during exertion o Microscopically: squamous metaplasia, parenchymal damage, glandular enlargement, goblet cell hyperplasia, lymphoid follicles ASTHMA – inflammation in airways leading remodeling, variable airflow limitation and hyperresponsiveness o Microscopically: fragile epithelium, thickened basement membrane, goblet cell hyperplasia, smooth muscle hypertrophy BRONCHIOLITIS– inflammation to small airways (respiratory and membranous bronchioles) resulting in irreversible airflow obstruction and reduced diffusing capacity 22 Pulmonary Week 2: Airways Disease Microscopically: cellular infiltrates, smooth muscle hyperplasia, bronchiolectasis, fibrosis, obliterative scarring BRONCHIECTASIS – permanent abnormal dilation and destruction of bronchi and bronchioles due to chronic inflammation and recurrent infection, can be obstructive or restrictive o Microscopically: transmural inflammation, permanent dilation, neovascularization o 37. Correlate the pathological findings with the physiological findings in patients with chronic airflow obstruction. Chronic airflow obstruction Pathological Hyperplasia and hypertrophy of both goblet cells and bronchial mucus gland Airway smooth muscle contraction, luminal occlusion, thickening wall, decreased lung elasticity, obliteration Inflammatory cells recruited to airway inflammation Loss of elastic recoil hyperinflation Hyperinflation flattened diaphragm Damaged airway epithelium Bullae (air sacs with thin wall) Physiological Increased mucus production, sputum, cough Increased resistance in airways dyspnea Narrowed airway wheezing; ventilation-perfusion abnormalities hypoxemia dyspnea ↑ residual volume; ↑ functional residual capacity; ↑ total lung capacity; ↓ vital capacity ↓ inspiratory capacity dyspnea ↓ bronchial relaxing factors; ↓ neutral endopeptidase (inactivates inflammatory mediators) Obstruct function of host lung; put pressure on other lung and interfere with its proper function; reduce efficiency of surrounding tissues 38. Discuss the rationale for the use of oxygen therapy in patients with chronic hypoxia, including mechanisms of delivery and the outcomes of therapy. (Case) Long term O2 therapy can: Prevent tissue hypoxia Reverse secondary polycythemia Improve body weight Ameliorate cor pulmonale Enhance neuropsychiatric function, exercise tolerance and activities of daily living Stabilize pulmonary hemodynamics survival benefit * Supplemental oxygen does not greatly improve shortness of breath O2 most frequently delivered through a nasal cannula or oxygen mask at rates of 2-5 L/min. Transtracheal administration (requires humidifier) provides O2 sparing benefits (scrupulous attention to catheter maintenance and hygiene – not suitable for all patients) 23 Pulmonary Week 2: Airways Disease 39. Describe the modalities available for chest imaging, and the advantages and disadvantages of each (All answers from radiology lectures and powerpoints) Chest X-Ray Pros o fast/available, cost-effective, good for confirmation of line placement, post surgical imaging, low radiation, bone detail Cons o only 2D, not as good resolution as other techniques (e.g., CT) Fluoroscopy Pros o real time, bone detail, inexpensive, available Cons o often require contrast media (has risks), poor tissue contrast, many layers are superimposed, continuous low-dose radiation (radiation exposure) Angiography/Catheterization Pros o good for arteries, easy to access blood for O2 saturation, intracardiac pressures, cardiac/valcular abnormalities Cons o invasive, <1% risk of MI, dysrhythmia, CHF, renal failure, pseudoaneurysm from groin puncture Computed Tomography Pros o high resolution, fast, non-invasive, excellent for detecting Ca2+, 3D images, excellent for bone and lung parenchyma Cons o high radiation exposure Magnetic Resonance Imaging Pros o soft-tissue contrast (e.g., b/w vessels and cardiac chambers), great for cardiac motion studies, not invasive, no radiation Cons o availability/cost, procedure time/claustrophobia, bone detail, weight<450lb (200kg), no metal (e.g., pacemaker), rare serious contrast reactions Ultrasound Pros o low cost, availability, portability, real-time imaging (e.g., useful for guiding a needle), sensitivity to flow, lack of ionizing radiation Cons o confined to processes in contact with chest wall (e.g., pleural effusions & superficial soft tissue lesions), not good for deep structures, obstructed by air in lungs, bone, high calcified materials Nuclear Medicine Pros o PHYSIOLOGICAL imaging (vs anatomical), good for ventilation-perfusion scanning (e.g., in pulmonary embolism), simpler than echocardiography, non-invasive, used for “myocardial perfusion scintigraphy (MIBI) to see coronary artery disease, risk post MI, angina, and preoperatively, used for “radionuclide angiocardiography”which labels RBCs with technetium-99m to image the blood pool (to calc ejection fraction, wall motion analysis) Cons o radiation 24