1 GI and Accessory System Alterations – PowerPoint Notes Slide 4
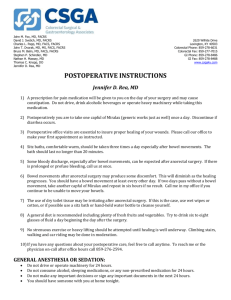
advertisement

1 GI and Accessory System Alterations – PowerPoint Notes Slide 4: >3 bm daily Increased liquidity Can be acute or chronic Acute usually associated with infection and may last 7-14 days Chronic often lasts 2-3 wks and returns sporadically May be caused by meds-stool softeners, laxatives, prokinetic agents, etc. We’ll cover problems that may cause diarrhea as we progress through this module. Intestinal rumbling (borborygmus) common w/ diarrhea. Consider c. diff if having unexplained diarrhea after recent antibiotics Disorder of small bowel=watery stools Disorder of large bowel=semisolid stools Malabsorption=greasy stools Blood, mucous, pus= inflammatory enteritis or colitis Diarrhea complications-f&E loss which can cause dysrhythmias (K+) loss, and will result in <30 ml/hr uop. Consider skin breakdown from chronic diarrhea. Slide 5: Your book only mentions anticholinergics. Slide 6: Many possible causes-consider dementia, laxative abuse, weakness of anal/rectal muscle tone w/age. Consider skin integrity-use barrier creams Bowel training-put on bedpan, etc. daily about 30 min. after breakfast. Dulcolax suppository/enema given 15-30 min. prior to usual evacuation time may help establish pattern. Drainage systems are available when continence cannot be achieved. Pic on p. 1073-think foley cath for rectum. Bowel training- put on bedpan, etc. daily about 30 min. after b’fast. Dulcolax suppository/enema given 15-30 min. prior to usual evacuation time may help establish a pattern. Slide 7: Causes-meds (ex. Pain meds/anticholinergics), hemorrhoids, tumors in bowel, certain diseases (we’ll cover), ignore urge to defecate, poor fiber/fluid intake several causes listed in ch. 38. As you practice, you’ll see frequent causes- Aunt Mae constipated d/t laxative abuse. <3 BM week People w/ spinal cord injuries often don’t recognize need to defecate, etc. Complications-hemorrhoids, fissures, megacolon(can lead to bowel perforation), straining resulting in valsalva maneuver (causes drop in arerial blood pressure-followed immediately by severe and quick rise in B/P-if pt has HTN, can rupture major artery in brain or elsewhere.) Test-when 1st realize pt is constipated, 1st thing you do is perform focused assessment to ID risk factors for constipation. Tenesmus-spasmotic contraction of anal sphincter w/pain & persistent desire to empty bowel. Hemorrhoids most common complication of chronic constipation 2 If fecal impaction results from constipation, perforation may occur-life threatening Slide 8: More comprehensive drug list for each category table 38-1 Bulk forming-absorbs water, stimulating peristalsis Stool softeners-softens feces-does NOT affect peristalsis Lubricants-lubricate intestinal tract Saline/osmotic solutions-cause retention of fluid in intestinal lumen caused by osmotic effect Stimulants-increase peristalsis by irritating colon wall and stimulating enteric nerves Selective chloride channel activator-increases intestinal fluid retention/motility Serotonin type 4 receptor partial agonist-triggers peristaltic activity in gut Teach Eat 25-30 g fiber daily-fruit/veg./beans/ bran cereal, etc. Drink 3 quarts fluid daily –unless contraindicated(avoid caffeine-diuretic) Exercise regularly Establish regular time to defecate Do not delay defecation Record bowel elimination pattern Avoid laxatives/enemas Slide 9: Cause unknown Results from disorder of intestinal motility-peristaltic waves affected at specific segments of intestine & in the intensity with which they propel fecal matter forward. No evidence of inflammation/tissue change Pain often precipitated by eating/relieved by defecation. s/s may be mild/infrequent to severe and frequent Test-any time pt presents w/ abd pain, 1st thing we need to do is have patient tell us about/describe pain Common symptoms Abd. Distention, Excessive flatulence/Bloating, Abd pain May be precipitated by stress, food intolerances (high fat, irritating foods, alcohol) Dx made when other conditions ruled out-colorectal CA, peptic ulcer disease, etc. do thorough hx/physical (recent stress?) Symptoms based criteria-AKA Rome II criteria Recurrent abd pain for at least 3 days month for past 3 months-including 2 or more of following: Relief w/ defecation Onset ass. w/ change in stool frequency Onset ass. w/change in stool appearance More men report diarrhea More women report constipation-women have 2-2.5x more often than men Slide 10: Restriction then gradual reintroduction of irritating foods Irritating foods-beans, caffeine, corn, wheat, dairy lactose, fried/spicy foods, alcohol, aspartame, etc) High fiber diet/exercise, stress reduction,antidepressants, immodium, metamucil, anticholinergics (propantheline-anticholinergic-works by slowing movement of food through stomach/intestines and 3 decreasing amount of acid made by stomach). or antispasmotics (bentyl-before meals)may be given to decrease smooth muscle spasm/cramping. Probiotics-bacteria (lactobacillus & bifidobacterium) helps decrease abd bloating & gas. Lewis discussed zelnorm & Lotronex for tx in women only, zelnorm stopped w/IBS b/c risk of MI and stroke. Lotronex can cause ischemic colitis (decreased blood flow to intestines) so used only in restricted access program when all else has failed. Slide 11: Appendicitis- inflammation of appendix-extends from inferior part of cecum. most common 10-30 yrs old Appendix fills w/food & empties into cecum-b/c empties inefficiently & lumen small, it’s prone to obstruction & vulnerable to infection. Obstruction results in distention, venous engorgement, accumulation of mucus & bacteria-can lead to gangrene/ perforation/abscess/peritonitis. Clinical Manifestations McBurney's point -halfway b/t umbilicus & right iliac crest usually prefers to lie still, often w/ right leg flexed. coughing aggravates pain Rovsing's sign-palpation of left lower quad, causing pain in right lower quad. Slide 12: Appendicitis- blood supply of appendix is impaired by inflammation and bacterial infection in wall of appendix. (May result in gangrene). Cecum-blind pouch that forms 1st portion of large intestine. Appendix at lower end. Slide 13: Physical-(particularly palpation of abd) WBC may be elevated w/ appendicitis. Urinalysis to r/o genitourinary conditions that mimic appendicitis. Gold standard is either ultrasound or CT scan. NeutroSpec imaging new technique to diagnose-advantage over current standard of care/diagnosis in less than 1 hr. (can read details in text) If dx/ tx are delayed, appendix can rupture- resulting peritonitis can be fatal. If appendix ruptured & evidence of peritonitis or abscess, tx w/ ABT/ parenteral fluids 6-8 hrs before appendectomy to prevent sepsis /dehydration. NURSING MANAGEMENT-preop Laxatives/enemas especially dangerous b/c resulting increased peristalsis may cause perforation of appendix. Until MD sees pt-keep NPO –possible surgery. ice bag to right lower quad to decrease blood flow & impede inflammatory process. Heat never used- may cause appendix to rupture. Surgery, generally laparoscopically, performed soon as dx made. Postop similar to postop care after laparotomy-wound care, ambulation, meds for n/v & pain, possible NG, advance diet, TC&DB,etc. General post-op care pp.383-386 if you need to review. Ambulation begin day of surgery/ 1st postop day. 4 diet advanced as tolerated. usually d/c 1st/2nd postop day-normal activities resumed 2-3 wks after surgery Slide 14: Peritonitis from localized or generalized inflammatory process of peritoneum. Caused by leakage of contents from abd. Organs into abd Cavity usually as result of infection, inflammation, ischemia, trauma, or perforation. Many causes. Paralytic ileus direct effect of infection. Primary peritonitis occurs when blood-borne organisms enter peritoneal cavity. Ex: ascites that occurs w/ cirrhosis of liver provides excellent liquid environment for bacteria to flourish. Secondary peritonitis much more common-occurs when abd organs perforate/rupture & release their contents (bile, enzymes, bacteria) into peritoneal cavity. Ex:ruptured appendix, perforated gastric/duodenal ulcer, severely inflamed gallbladder, trauma from gunshot/knife wounds. Intestinal contents/ bacteria irritate normally sterile peritoneum & produce immediate chemical peritonitis that’s followed few hrs later by bacterial peritonitis. No matter cause, resulting inflammatory response leads to massive fluid shifts (peritoneal edema) & adhesions as body attempts to wall off infection. Slide 15: Complications Hypovolemic shock, Sepsis, Intraabdominal abscess formation, Paralytic ileus/intestinal obstruction from adhesions Paracentesis (puncture of cavity w/removal of fluid) may be performed/ fluid analyzed for blood, bile, pus, bacteria, fungus, amylase (pancreatic enzyme that breaks down starch) content. x-ray of abd may show dilated loops of bowel consistent w/ paralytic ileus, free air if perforation has occurred, or air/fluid levels if obstruction present. Ultrasound/CT /MRImay ID presence of ascites/abscesses. Peritoneoscopy (placement of endoscope through stab wound in abd to inspect peritoneum)-helpful in pt without ascites. Diagnostic History / physical exam CBC-elevated WBC & hemoconcentration from fluid shifting into abdomen from vascular space. Serum electrolytes Management NPO status,IV fluid replacement-isotonic solution fluid from vascular space to peritoneal cavity, Antibiotics/antiemetics,NGT suction Analgesics (e.g., morphine), Oxygen prn-vent if septic, parenteral nutrition, blood transfusions, prn Surgery Remove infected material and correct cause. May come back w/drains, fecal diversion. Test-after any abd surgery, if pt. complains of gas pain/abd distention, best nursing action is to get up & walk. Slide 16: Autoimmune disease/genetic influence Crohn’s disease/Ulcerative colitis Commonly occur teens/early adult-2nd peak in 6th decade 5 Women/men equally affected Both forms of IBD chronic disorders w/ mild-severe acute exacerbations that occur at unpredictable intervals over many yrs Table 38-4 compares the two and would be good place to study Slide 17: Patho Chronic inflammation of gi tract wall that extends through all layers. Most common in distal ileum & sometimes ascending colon. Remission/exacerbation Edema/thickening of mucosa. Ulcers appear on inflamed mucosa, and separated by normal tissue causing cobblestone appearance. Manifestations Right lower quadrant pain & diarrhea unrelieved by defecation. Scar tissue interferes w/food digested in upper GI to pass causing crampy abd pain. B/c eating stimulates peristalsis, pains occur after meals. Pt eats less b/c of this causing wt loss, malnutrition, secondary anemia. Ulcers & inflammatory changes result in weeping, edematous intestine that empties irritating discharge into colon. Disrupted absorption causes diarrhea & nutritional deficits. Chronic symptoms-diarrhea, abd pain, steatorrhea (fatty stool), anorexia, wt. loss, nutritional deficiencies. Assessment/diagnostics Proctosigmoidoscopy initially performed Stool for occult blood & steatorrhea Most conclusive is barium study of upper gi (shows terminal ileum showing constriction of segment of intestine) Also, endoscopy, colonoscopy, intestinal biopsies, barium enema may show ulceration “cobblestone appearance”, CT shows wall thickening/fistulas. CBC for H&H (occult blood from ulcers) & WBC (consider peritonitis, etc.) ESR-erythrocyte sedimentation rate -may be elevated d/t inflammatory response albumin/protein may be decreased d/t malnutrition Complications Stricture/obstruction, perianal disease, F&E imbalance (diarrhea), malnutrition (from malabsorption), fistula/abscess formation. Slide 18: Crohn’s-mucosa demonstrates cobblestone appearance. Strictures at areas of inflammation may cause bowel obstruction. Since inflammation goes though entire wall, microscopic leaks can allow bowel contents to enter peritoneal cavity & cause perforation/ abscess/peritonitis/or fistulas b/t adjacent organs (bowel/bladder, bowel/vagina, etc) Which will in turn cause leukocytosis and fever Most common fistula b/t small bowel & skin (enterocutaneous fistula) UTIs usually 1st sign of bowel/bladder fistula, & feces sometimes seen in urine. Crohn’s pt at risk for colon CA 6 Slide 19: Patho Remission/exacerbation Recurrent ulcerative & inflammatory disease of mucosal/submucosal layers of colon/rectum. 5% dev colon CA Affects superficial mucosa of colon-characterized by multiple ulcerations, diffuse inflammation, &shedding of colonic epithelium. Ulcerations result in bleeding. Abscesses form & clumps of neutrophils in lumens of crypts that line intestinal mucosa. Usually begins in rectum & spreads proximally to involve entire colon. Bowel eventually narrows, shortens, & thickens. B/c inflammation only to inner lining mucosa, fissures/fistulas/obstruction uncommon. Manifestations Diarrhea w/mucous & pus. Left lower quad abd pain Intermittent tenesmus Rectal bleeding (mild-severe) resulting in pallor,anemia, fatigue. Anorexia, wt loss, fever, n/v, dehydration,. Cramping w/ urgent need to defecate, 10-20 liquid stools/day. Hypocalcemia & anemia frequently-increased risk for bone fx d/t decreased bone mineral density (steroid therapy may also cause diminished bone density.) May have rebound tenderness in right lower quad Assessment/diagnostic Tachycardia, hypotension, tachypnea, fever, pallor Assess hydration/nutrition, bowel sounds, distention, tenderness. Stool +for blood & used to r/o parasites, etc. that could cause s/s. CBC-H&H, WBC high (inflammation) Low albumin & electrolyte imbalances common Sigmoidoscopy/colonoscopy/barium enema to help diagnose. CT/MRI/US to ID abscesses,etc. Complications Toxic megacolon(read over this p. 1084), perforation, bleeding from ulceration, vascular engorgement, & highly vascular granulation tissue. Slide 20: Ulcerative colitis usually starts in rectum & moves in continual fashion up colon. Although there’s sometimes mild inflammation in terminal ileum, ulcerative colitis is a disease of colon & rectum. Unlike Crohn's, in which healthy tissue is interspersed w/ inflamed tissue, ulcerative colitis spreads in continuous pattern. Slide 21: Nutrition Oral/iv fluids (if hospitalized) Low residue/high protein/high calorie diet w/supplemental vitamins & iron Milk may need to be avoided if lactose intolerance-may contribute to diarrhea Cold food/smoking avoided b/c increase intestinal mobility 7 Parenteral nutrition prn Meds Sedatives, antidiarrheal, antiperistaltic-to minimize peristalsis & rest inflamed bowel Used until stool consistency/freq approach normal Aminosalicylates (ex. Azulfidine) for inflammation & used long-term to prevent/reduce recurrence. (mild-moderate disease) Corticosteroids (severe)-given orally (prednisone) or IV (solu-cortef) in hospital. Topical steroids in distal colon disease (rectal)(ex.)entocorec Immunomodulators (Imuran, methtrexate, etc.)may be used to alter immune response. Used in severe disease when haven’t responded to other therapy. Biologic therapy (Tysabri) & (remicade) Biologic therapy-agent modifies relationship b/t host & problem by altering response of host to problematic cells. Antimicrobials-used to tx inflammatory bowel disease, but no specific infectious agent has been discovered-(flagyl, cipro, biaxin) Surgery 75% crohn’s pt have surgery w/in 10 yrs diagnosis. 25-60% need more surgery in same time frame. Crohn’s Surgery Stricturplasty-widen areas of narrow bowel. Small bowel resection-resect & anastomose. Can tolerate 50% removal of sm bowel. If severe crohn’s & affects colon, total colectomy & iliostomy may be procedure of choice. New-intestinal transplant. Expensive. None of surgical procedures for crohn’s is curative-remission depends on medical therapy. Ulcerative colitis surgery At least 25% w/U. colitis have total colectomies (colon removed). Pt. considered cured b/c disease of colon. Proctocolectomy w/ileostomy (excision of colon, rectum, anus) when rectum severely diseased. If rectum preserved, proctocolectomy w/ ileal pouch anal anastomosis is procedure of choice. Ostomies discussed later in this module. See chart 38-3 for home care checklist. Slide 22: Mechanical-causes of mechanical Table 38-5 Figure 38-7 shows intussusception,volvulus (twisting), and hernia (inguinal) Detectable occlusion of intestinal lumen Surgical adhesion most common cause of small bowel obstruction Hernias/tumors next most common causes (small bowel) Carcinoma most common cause large bowel obstruction Functional Intestinal musculature cannot propel contents along bowel. *Paralytic Ileus Requires prompt tx Surgical adhesion can occur w/in days of surgery/several yrs later Other causes of mechanical bowel obstruction-volvulus (twisting of bowel on itself causing obstruction)/diverticular disease Functional Paralytic ileus (lack of intestinal peristalsis/no bowel sounds) most common form functional-occurs to some degree after any abd surgery. 8 Collagen vascular diseases/neurologic/endocrine disorders may cause functional obstruction-many times cause unknown. If blood flow inadequate, bowel tissue becomes ischemic, then necrotic, bowel may rupture. most dangerous obstruction is when bowel becomes strangulated/ blood supply cut off. If not corrected quickly, bowel will become necrotic/ rupture, leading to massive infection/death. Slide 23: Patho Intestinal contents, fluid, gass accumulate above obstruction causing edema, congestion, necrosis, & eventual rupture of intestinal wall resulting in peritonitis. May have reflux vomiting. Manifestations Colicky, wavelike, crampy pain. May pass blood/mucous, but no fecal matter or flatus. Vomiting-if obstruction complete, peristaltic waves extremely vigorous, then reverse, so contents go to mouth. If obstruction in ileum, fecal vomiting takes place. First stomach contents, then duodenum/jejunum contents, finally, fecal like contents of ileum. Dehydration occurs Abd distended/tender0lower the obstruction, the more marked the distention. Assess/diagnostic Diagnosed on s/s & imaging X-ray/CT Labs-dehydration, loss plasma volume, dehydration Management NGT-decompress If completely obstructed, may need surgery-IV fluids 1st to correct dehydration/F&E imbalances. Surgery for correction based on problem (hernia repair, dividing adhesions, etc.) Sometimes portions anastomosed. Nursing management p. 1098-read! Slide 24: Patho Accumulation of contents proximal to obstruction. If blood supply cut off, strangulation/necrosis can occur-life threatening! Colon can absorb fluid contents & can distend considerably beyond normal full capacity, so dehydration more slowly than if in sm intestine. Manifestations Constipation may be only s/s for months Shape of stool altered as it passes by obstruction. Blood loss may cause iron deficiency anemia. May have weakness, wt. loss, anorexia. Eventually becomes distended w/crampy lower abd pain. Finally, fecal vomiting develops Assess/diagnose s/s & imaging Barium studies contraindicated Management 9 NGT-decompress, IVF for dehydration & F&E imbalances. May do colonoscopy Rectal tube to decompress lower bowel Usual tx is surgical resection to remove obstructing lesion. Temporary/permanent colostomy may be necessary. Nursing mgmt p. 1098 Slide 25: Polyp-mass of tissue protruding into bowel lumen-can be anywhere in intestinal tract/rectum Neoplastic (adenomas/carcinomas) Adenomas-more common in men-higher after 50 yrs. Non-neoplastic (benign)-are most common in lg intestine. Must be followed closely, but most do not develop into neoplasms. In 80% poulation & frequency increases w/age. Manifestations Depends on size of polyp Most common s/s is rectal bleeding. May have lower abd pain. If large may have signs of obstruction Diagnosis Hx/digital rectal exam, barium enema, sigmoidoscopy/colonoscopy. Polyp should be removed & microscopic exam identifies type of polyp for further tx. Slide 26: Pendunculated (attached to intestinal wall by thin stalk) polyp in descending colon Slide 27: Patho 95% adenocarcinoma (from epithelial lining of intestine) May begin benign & become malignant Cancer cells may migrate from tumor to other areas (liver/peritoneum/lungs) Chart 38-9 discusses risk factors-read Manifestations Most common presenting symptom-change in bowel habit. Blood in stool 2nd most common. May also have anemia/anorexia/wt.loss/ fatigue. s/s w/right-sided lesions-dull abd pain/melena. s/s w/left-sided lesions-those ass. w/ obstruction & bright red blood in stool. s/s w/rectal lesions-tenesmus (ineffective straining w/stool), rectal pain, feeling of incomplete evacuation, altering constipation/diarrhea, & bloody stool Often no s/s until colorectal CA advanced Assess/dx Abd/rectal exam Fecal occult blood testing,barium enema, proctosigmoidoscopy, colonoscopy, (see ch 34 for review of tests) Usually detected w/ colonoscopy w/ biopsy or cytology smears. May check CEA (carcinoembryonic antigen) Complications 10 Bowel obstruction, tumor into blood vessels resulting in hemorrhage, perforation, abscess,peritonitis, sepsis, etc. Management Obstruction-NGT & IVF, blood prn Chart 38-10 has staging of colorectal CA read! From class A (contained) to class D (advanced w/mets) May receive chemo, radiation, immunotherapy, multimodality therapy, supportive therapy, surgical therapy (curative or palliative), etc. read all medical mgmt starting p.1100 Will cover ostomies coming up… Nursing care for pt w/ colorectal CA-very important reading p. 1102-covers assessment/nursing dx w/ potential complications/planning/interventions (surgery prep,emotional support, post-op care, nurtition,wound care, complications, ostomy care), home & community based care. Slide 28: Opening called stoma stoma created when intestine brought through abd wall & sutured to skin. intestinal contents empty through stoma rather than being eliminated through anus. If removal of anal sphincters, anus sutured shut/permanent ostomy created. The more distal an ostomy, the more intestinal content resembles feces Slide 29: End stoma Bowel divided & proximal end brought out as single stoma Distal portion removed or oversewn and left in abd cavity When oversewn rather than removed-known as Hartmann’s pouch If removed, stoma is permanent. If oversewn, potential to reanastomose bowel and close stoma Loop stoma Loop of bowel brought to abd surface and opening of anterior wall of bowel to provide fecal diversion. Result-1 stoma w/proximal & distal opening & intact posterior wall that separates the 2 openings. Loop of bowel held in place w/ plastic rod 7-10 days post op to prevent from slipping back into abd cavity. Usually temporary. Double-Barreled Stoma When bowel is divided, both proximal & distal ends brought through abd wall as 2 separate stomas. Proximal one is functioning stoma Distal-nonfunctioning stoma referred to as mucus fistula. Double-barreled stoma usually temporary. Kock Pouch Described p. 1085-a continent ileostomy-a variation from traditional ileostomy –pouch can hold feces & catheterize to empty every few hours. Trauma to intestines (gunshot wound, stab) may need a temp ostomy. CA involving rectum requires permanent b/c bowel distal to ostomy removed. 3 possibilities exist: 1.If distal bowel left in place, bowel walls can later be reconnected- ostomy temporary. 2.If distal bowel removed, but anal sphincters remain, ileal pouch anal anastomosis possible & ostomy temporary. 3.If distal bowel & sphincters removed, anus sewn shut and ostomy permanent. 11 Slide 30: Preop Care flat site on abd allows secure attachment of bag/avoid leakage. Select stoma site visible to pt taking care of it. Psychologic prep-body image, loss of control over elimination, odors-understand extent of surgery, type of stoma, & its care. Bowel prep-empty intestines preop to decrease chance of postop infection caused by bacteria in feces. neomycin & erythromycin given to decrease # of intracolonic bacteria. Postop Care Assess stoma/pouch/skin/drainage/odor. Stoma should be pink. Dusky blue stoma- ischemia Brown-black stoma- necrosis-Document stoma color q 8 hrs. Mild/moderate swelling of stoma first 2-3 wks after surgery Pouching system consists of skin barrier/ bag to collect feces. Skin barrier Skin barrier remains in place about 5-7 days. Length of adhesion depends on strength of seal/amt of drainage from stoma. If stoma site has creases,difficult to get good seal wt of drainage pulls wafer away from skin-empty when 1/3 full Pouch 1-piece system has skin barrier attached-2-piece system allows removal of pouch w/o removing skin barrier. skin washed w/ mild soap, rinse w/warm water, dried thoroughly before barrier applied. Skin Prep-applied before skin barrier to further protect skin/improve adherence size of stoma determined w/ stoma-measuring card-Colostomy functions when peristalsis restored. Volume, color, consistency of drainage recorded. Each time pouch changed-skin observed for irritation-Pouch never placed directly on irritated skin without skin barrier. D/C w/ written info about ostomy, instructions for pouch changes, list of supplies/where to buy, followup appointments, phone numbers. Slide 31: Semiliquid stools-use drainable pouch Semiformed/formed may be able to irrigate & not use pouch Nondrainable pouches need gas filter Most w/colostomies eat anything they choose-colonic bacteria act on certain carbs to form gas (cabbage, broccoli, etc.) Irrigations Used to achieve regular bowel pattern May only need pad/small pouch over stoma Regularity only possible w/stoma in distal colon/rectum irrigation-(think enema) Use stoma cone for irrigation-do not force tube Ileostomy susceptible to obstruction b/c lumen <1 in in diameter popcorn, coconut, mushrooms, olives, stringy veg, foods w/ skin, dried fruits, meats w/ casings must be chewed extremely well so very sm when swallowed. 12 Stoma bleed easily b/c high vascular supply-minimal oozing blood normal. If terminal ileum removed-may need cobalamin tx. P1089-1096 has several charts re:ostomy care- I suggest you read these. Slide 32: Grief-alteration body image-psychologic support needed. Cant do sports where direct trauma to stoma likely. Bath/swimming w/ or without pouch b/c water does not harm stoma. Sexual Dysfunction Pelvic surgery can disrupt nerve/vascular supply to genitals. Radiation , chemo, meds, fatigue can alter sexual function. Plan sexual activity around drug schedule/energy levels. Surgery that removes rectum has potential of damaging parasympathetic nerve plexus. Erection depends on parasympathetic nerves that control blood flow to pelvis & nerves that transmit sensory responses from genital area. Nerve-sparing surgery used when possible to preserve sexual function. Radiation to pelvis can reduce blood flow to pelvis by causing scarring in sm blood vessels. Radiation can affect vaginal expansion/ lubrication. Pelvic surgery does not affect woman's arousal unless part of or entire vagina removed. If sympathetic nerves in male's presacral area damaged, ejaculation may be disrupted. Concerns-ability to resume sex, altering clothing styles, effect on ADLs, sleeping w/ pouch, passing gas, odor, cleanliness, fear of rejection from partner. Pregnancy possible-MD may recommend limited pregnancies d/t physical condition. Slide 33: 1st pic-ascending colostomy 2nd pic-descending colostomy 3rd pic ileostomy 4th pic sigmoid colostomy-single barreled Last pic- transverse colostomy-double barreled Slide 34: Upper corner ileostomy Notice rod in place- Slide 35: Diverticulum -saclike herniation of lining of bowel that extends thru defect in muscle layer (most common in sigmoid colon 95%) Diverticulosis -multiple diverticula without inflammation/symptoms. Diverticulitis -food/bacteria retained in diverticulum produce infection/inflammation that can impede drainage & lead to perforation/abscess. Patho Diverticula form when mucous/submucosal layers of colon herniate thru muscle wall b/c of high intraluminal pressure, low volume in colon (low fiber diet), & decreased muscle strength in colon (muscle hypertrophy from hard fecal masses). Bowel contents accumulate & decompose in diverticulum causing inflammation/infection, and possible obstruction. 13 When diverticulitis has occurred, microperforation of colon has occurred. Abscesses may develop & eventually perforate causing peritonitis & erosion of arterial blood vessels, resulting in bleeding. Manifestations Diverticulosis Chronic constipation often precedes diverticulosis. Often no s/s, but if having s/s may see bowel irregularity w/intervals of diarrhea, nausea, anorexia, bloating. If repeated inflammation may see cramps, narrow stools, constipation/bowel obstruction. Diverticulitis Acute onset of mild/severe pain in LLQ, N/V, fever, chills, leukocytosis. If untreated may lead to peritonitis/septicemia. Assess/diagnose Colonoscopy w/biopsy Barium enema-but not w/peritoneal irritation b/c of potential for perforation. Complications Peritonitis, abscess, fistulas, bleeding (diverticula may erode areas adjacent to arterial branches, causing massive rectal bleed Manage Rest, analgesics, antispasmotics w/symptoms Clear liquid-then high fiber, low fat diet after s/s better Antibiotics 7-10 days & bulk forming laxative prescribed If severe-hospital, NPO, IV fluids, NG suction to rest bowel, ABT 7-10 days, demerol, (morphine contraindicated b/c increases intraluminal pressure of colon) Antispasmotics (Daricon)/fiber supplements (psyllium)/stool softeners (colace), may use suppository to help evacuate colon (bisacodyl). (Want to cleanse colon). Surgery Used for complications-perforation/peritonitis/hemorrhage/obstruction CT guided percutaneous drainage may be performed to drain abscess-give ABT May do 1 stage resection (remove inflamed piece & reanastomose) OR Multiple stage procedures if complications (obstruction/perforation) may need ostomy (fig. 38-4 gives visual) Nursing process care p. 1079 read! Slide 36: Diverticula-outpouchings of colon. When inflamed-condition is diverticulitis. Slide 37: Hernia- protrusion of organ or part of organ thru the wall of cavity that normally contains it. Hernias easily return to abd cavity called reducible. Can be reduced manually/may reduce spontaneously when pt lies down. If cannot be placed back in abd cavity- irreducible/incarcerated. Intestinal flow may be obstructed. When irreducible & intestinal flow & blood supply obstructed, hernia strangulated. Result-acute intestinal obstruction. Types 14 inguinal occurs at point of weakness in abd wall where spermatic cord in men/round ligament in women emerge. When protrusion escapes through inguinal ring & follows spermatic cord or round ligament-termed indirect hernia. When escapes through posterior inguinal wall- direct hernia. Inguinal more common in men. Femoral- protrusion through femoral ring into femoral canal. Occurs below inguinal (Poupart's) ligament as a bulge-becomes strangulated easily Occurs more in women. umbilical occurs when rectus muscle weak (as w/obesity) or umbilical opening fails to close after birth. Ventral/incisional d/t weakness of abd wall at site of previous incision. Occur most commonly in obese, had multiple surgeries in same area, or had poor wound healing b/c of poor nutrition/ infection. Hiatal Already covered hiatal hernia (opening in diaphragm thru which esophagus passes has part (upper stomach & part of gastroesophageal junction-AKA sliding or type 1) or all (entire stomach pushes up and beside esophagus-AKA paraesophageal) Paraesophageal classified as type II- IV depending on herniation severity Slide 38: Often readily visible Not testing on hiatal hernia- was discussed last semester-tx similar to GERD (Nissen fundoplication) If strangulated-severe pain-s/s bowel obstruction(vomiting, cramping abd pain, distention.) Dx based on history/ physical exam. Surgery prevents strangulation-usually laparoscopic/ outpatient Herniorrhaphy (surgical repair of hernia) Hernioplasty (reinforcement of weakened area w/wire fascia, mesh) Strangulated hernias treated immediately w/ resection of involved area or temporary colostomy so necrosis & gangrene do not occur. Some w/hernias wear truss (pad placed over hernia- held in place w/ belt.) Truss worn to keep hernia from protruding. Check for skin irritation caused by continual rubbing of truss against skin. Scrotal edema painful complication after inguinal hernia repair. Scrotal support w/ ice bag may help relieve pain/edema. Coughing not encouraged-deep breathing & turning should be done. If cough/sneeze, incision splinted and mouth open. After discharge-restricted from heavy lifting 6-8 wks. Slide 39: 1st-umbilical hernia 2nd –direct inguinal hernia 3rd-indirect inguinal hernia 4th –femoral hernia Live pic-indirect inguinal hernia 15 Slide 40: Malabsorption -inability of digestive system to absorb one or> of major vitamins (ex: A & B12) minerals (ex. Iron/calcium), nutrients (carbs/fats/proteins). Diseases of small intestine most common cause. Patho Mucosal disorders (celiac sprue)-causing generalized malabsorption. Postoperative malabsorption (short bowel syndrome) Table 38-2 lists malabsorptive disorders & characteristics of each-READ!!. Manifestations Diarrhea or freq, loose bulky, foul-smelling stools w/increased fat content that are often gray. Also, abd distention, pain, flatus, weakness, wt loss, Result of malabsorption is malnutrition (pt may present w/easy bruising (iron/b12), osteoporosis (calcium), anemia. May be weak/emaciated from malnutrition/dehydration Failure to absorb fat soluble vit ADEK cause problems. Assess/diagnose Stool for fat, hydrogen breath test to eval carb absorption (ch 34), d-xylose absorption test (good screen for carb absorption) Endoscopy w/biopsy best diagnostic tool. X-ray, US, CT can show tumors of pancreas/intestine that may be cause. CBC-anemia Management Supplement lost nutrients Fluids & antidiarrheals Some problems may require ABT & surgery, but handbook focuses specifically on short bowel syndrome/celiac disease Education about diet Monitor labs Pancreatic function test-to ID pancreatic causes I’ve already focused on short bowel syndrome w/gastric roux en y of upper GI Now, handbook specifically mentions celiac sprue (AKA gluten sensitive enteropathy) Celiac sprue 1st recognized in babies w/foul smelling diarrhea, abd distention, anorexia, wasting, failure to thrive – appeared about time started cereal. Causes-Gluten ingestion/genetic predisposition/autoimmune Gluten-free diet halts process (avoid wheat, barley oats, rye, flour, breads, pasta, pizza bagels, etc.) Lewis went so much more in depth, but we’re sticking w/text as much as possible. Slide 41: May be internal-(above internal sphincter) or external (outside external sphincter) Internal may be asymptomatic-If constricted will report pain- may bleed after defecation or prolapse when large.. External reddish blue-seldom bleed or cause pain unless vein ruptures. Blood clots in external cause pain/inflammation- hemorrhoids described as thrombosed. chronic, dull, aching discomfort, esp. when hemorrhoids prolapsed. Thought to develop as result of shearing forces during defecation. Force damages supporting muscles. 16 Precipitated by:Pregnancy, Prolonged constipation, Straining to defecate, Heavy lifting,Prolonged standing/sitting, etc. Amt of blood lost at 1 time may be small-over time may lead to iron deficiency anemia Diagnose Digital exam, anoscopy (speculum), sigmoidoscopy Manage High residue diet (fruit/bran), increase fluid, bulk forming agents (psyllium). Warm compresses, sitz bath, analgesic ointments (nupercainal)/suppositories, astringents (witch hazelshrink MM &relieve pain), bedrest to reduce engoegement. Short-term (< week) topical steroids may be used (hydrocortisone) to decrease swelling. Longer may cause mucosal atrophy/& contact dermatitis. Stool softeners may also be used. Bedrest to reduce engorgement. nonsurgical- several things done to affix mucosa to underlying muscle Sclerosing agents may be injected for small, bleeding hemorrhoids. Surgery Rubber band ligation, cryosurgical hemorrhoidectomy, laser (excisizing hemorrhoids), stapled hemorrhoidopexy (staples to treat prolapsing hemorrhoids). All else fails, may do hemorrhoidectomy. (gelfoam gauze may be placed over anal wounds.) Slide 42: Grade IV hemorrhoid disease Post op Slide 43: Sitz baths (15-20 min) 2-3x daily for 7-10 days to reduce pain/swelling w/hemorrhoids. Postop Pain d/t sphincter spasm common problem after hemorrhoidectomy. Procedure minor/pain severe. Opioids usually given initially-morphine/oxycodone Sitz baths start1-2 days after surgery-given 1-2 wks sponge ring in sitz bath helps relieve pressure. Packing may be inserted into rectum to absorb drainage-usually removed 1st or 2nd postop day. Assess for rectal bleeding. Usually dreads 1st BM-often resists urge to defecate. Colace usually ordered 1st few postop days-may also be sent home w/colace,etc. If no BM within 2-3 days, oil-retention enema given. Occasionally, anal strictures develop & dilation necessary T-binder may hold dressing in place. Pain med may be given before the BM to reduce discomfort. Slide 44: Most common causative organisms: E coli, staph, & strept. Clinical manifestations: local pain/swelling/tenderness-superficial Lower abd pain-deep foul-smelling drainage elevated temperature 17 Fistula can occur as complication. Palliative-sitz bath/analgesics If packing used, should be absorptive drsg (calcium alginate), & area should be allowed to Heal by granulation Avoid soiling drsg during urination/defecation. may leave hospital w/ wound still open. Teaching Wound care Sitz baths Thorough cleaning after bm Follow-up visits to MD Slide 45: Usually result of infection-can be from trauma/fissures May extend to outside of skin, vagina, or buttocks/often precedes an abscess. May be persistent, blood-stained, purulent discharge or stool leakage from fistula. May need to wear a pad to prevent staining clothes. Untreatreated fistula=syatemic infection & related problem tx Fistulectomy (recommended)- excision of entire fistulous tract-Gauze packing inserted Care same as after hemorrhoidectomy. Slide 46: Small tract under skin b/t buttocks in sacrococcygeal area. Visual figure 38-13 May have several openings/lined w/ epithelium & hair. Thought to be congenital or from trauma Hair frequently seen protruding from these openings Rarely symptoms until adolescence/early adult-perspiration/friction irritate Irritated skin becomes infected/forms pilonidal cyst or abscess. If infected, pt c/o pain/swelling at base of spine. Nursing care: Warm, moist heat when abscess present. Tell pt. to avoid contaminating drsg when urinating/ defecating ABT if caught early Surgery if abscess-I&D Probably pack wound after surgery. Slide 47: Bilirubin-Tabers 244 Conjugated/unconjugated Tabers 1153/1154 bilirubin level has to be approx 3x normal levels (2-3 mg/dl) for jaundice to occur. Hemolytic (prehepatic) jaundice d/t increased breakdown of (RBCs), which produces increased amt of unconjugated bilirubin in blood liver unable to handle increased load. Causes-blood transfusion reactions, sickle cell crisis, & hemolytic anemia. 18 Hepatocellular (hepatic) jaundice results from liver's altered ability to take up bilirubin from blood or to conjugate or excrete it. most common causes of hepatocellular jaundice are hepatitis, cirrhosis, hepatic carcinoma. Obstructive (posthepatic) jaundice d/t decreased/obstructed flow of bile through liver or biliary duct system. B/c bilirubin does not enter intestines, there’s decreased to no fecal/urinary urobilinogen. W/complete obstruction, stools clay colored. Slide 49: Note liver, GB, pancreas and how all connected-will have better pancreas picture Slide 50: Systemic viral infection w/necrosis & inflammation of liver cells. Easily transmitted Hep A 37% of all cases & Hep B18% all cases Rates slowly declining sine 1990-A & B vaccines 90% unreported d/t Mild cases/misdiagnosis Slide 51: found in feces 2 or more wks before onset of symptoms & up to 1 wk after onset of illness By time jaundice occurs, prob not infectious Hep A confers immunity against itself, but can still get other types present in blood only briefly-no carrier state exists No chronic hepatitis ass. w/this type Antigen in stool 7-10 days before illness appears & 2-3 wks after s/s appear. Anti-HAV (antibody to HAV) immunoglobulin M (IgM) appears in serum as stool becomes negative for virus. Detection of IgM anti-HAV indicates acute hepatitis IgG anti-HAV is indicator of past infection. presence of IgG antibody provides lifelong immunity. occurs more freq in underdeveloped countries. virus present in feces during incubation period, so it can be carried/transmitted by persons who have undetectable, subclinical infections. greatest risk of transmission occurs before clinical symptoms apparent. Incubation period 15-50 days (avg 30) Sex transmit possible (oral/anal) & multiple partners increases risk. preictiric phase-before jaundice Icteric phase-jaundice Slide 52: Transmission when infected fluids enter body of person not immune to virus. In pt w/HBV, hep B surface antigen (HBsAg) in vaginal secretions, menstrual fluids, semen, saliva, resp secretions, tears, gastric juice, synovial fluid, & cerebrospinal fluid. If (GI) bleeding, feces can be contaminated w/virus from blood. no evidence urine, feces (w/out bleed), breast milk, sweat infective-Organ/tissue transplant potential source of infection. Hep B is STD-Male homosexuals (esp unprotected anal intercourse) at risk. lower risk of transmission, kissing/sharing food may spread virus via saliva. 19 Also at risk- contacts w/ infected persons, hemodialysis pts, & health care/public safety workers. HBV can live on dry surface for at least 7 days-much more infectious than HIV. persistence of HBsAg in serum for 6-12 mo or > after infection w/virus indicates carrier state. Each antigen has corresponding antibody that may develop in response to acute viral hep B-These antibodies detected in serum of pt w/prior exposure to virus (Fig. 44-3). presence of hep B surface antibody (anti-HBs or HBsAB) indicates immunity from HBV vaccine/past HBV infection. HBsAg level remains detectable in chronic carriers (HBsAg + on at least 2 occasions at least 6 mo apart). Pts w/chronic HBV may have normal liver, low-grade disease, or severe liver disease. Incubation period 45-180 days Infective before/after symptoms appear-infectious 4-6 months-carriers infectious for life Approx 6% of those infected when >age 5 develop chronic HBV Slide 53: In US/Canada most common mode of HCV transmission is sharing of contaminated needles & paraphernalia among IV drug users. Transmission during blood transfusion has decreased proportion of cases attributed to high-risk sexual behavior (unprotected sex, multiple partners) has increased in recent yrs to 20%. sexual transmission among monogamous partners is rare. In US, 10% of all cases d/t occupational exposure, hemodialysis, & perinatal transmission. reliable antibody test for HCV not widely available until 1992-pts given blood/blood products before then at risk for chronic HCV infection & should be tested. Add. data needed re: risks of body piercings, tattooing, intranasal (cocaine) drug use in transmission of HCV. Incubation 14-180 days Infective 1-2 wks before symptoms appear-continues during clinical course, 75-85% go on to develop chronic hep Slide 54: (HDV), also called delta virus-a defective single-stranded RNA virus that cannot survive on its own. no vaccine for HDV; however, vaccination against HBV reduces risk of HDV co-infection. Incubation-2-26 weeks-HBV must precede Chronic carriers of HBV always at risk Slide 55: occurs primarily in developing countries-Asia, Africa, Mexico. Only few cases reported in US, and cases have been primarily in persons who recently traveled to HEVendemic areas. Currently, no serologic tests to dx HEV infection commercially available in US. Incubation 15-64 days Infectivity not known 20 Slide 56: poorly characterized parenterally & sexually transmitted virus. HGV coexists w/other viral infections, including HBV, HCV, & HIV, but does not appear to cause liver damage by itself. has been found in some blood donors & can be transmitted by blood transfusion. Slide 57: Liver-pathophysiologic changes in various types of viral hepatitis similar. Hep involves widespread inflammation of liver tissue. During acute infection, liver damage mediated by cytotoxic cytokines & natural killer cells that cause lysis of infected hepatocytes. Liver damage results from hepatic cell necrosis. Inflammation may interrupt bile flow (cholestasis). W/time, liver cells can regenerate in an orderly manner, & if no complications occur, they should resume normal appearance/function. Systemic Effects. antigen-antibody complexes b/t virus & its corresponding antibody form a circulating immune complex in early phases of hepatitis. circulating immune complexes activate complement system (Ch 13). clinical manifestations of this activation- rash, angioedema, arthritis, fever, malaise. Cryoglobulinemia (abnormal proteins in blood), glomerulonephritis, vasculitis also been found secondary to immune complex activation. Slide 58: Many asymptomatic-For pts who are asymptomatic during acute phase, infection may not be detected. acute phase usually lasts 1-4 mo. pt may find food repugnant-if smoker, may have distaste for cigarettes. Physical exam may revea lymphadenopathy acute phase may be icteric (symptomatic, including jaundice) or anicteric. Jaundice results when bilirubin diffuses into tissues. urine may darken because of excess bilirubin being excreted by kidneys. If conjugated bilirubin cannot flow out of liver b/c of obstruction/inflammation of bile ducts, stools will be light/clay colored. Pruritus sometimes accompanies jaundice pruritus occurs as result of accumulation of bile salts beneath skin. When jaundice occurs, fever usually subsides. convalescent phase following acute phase begins as jaundice disappearing & lasts for wks to mo, w/ avg of 2-4 mo. During this period pt's major complaint is malaise & easy fatigability. disappearance of jaundice does not mean pt has totally recovered. slight variation in manifestations b/t types of hep. In hep A onset more acute-symptoms usually mild/flu-like. In hep B onset more insidious-symptoms usually more severe. In hep C majority of cases asymptomatic/mild. HCV has high rate of persistence/often leads to chronic liver disease. 21 Slide 60: FIG. 44-4 Cirrhosis that developed secondary to alcoholism. characteristic diffuse nodularity of surface d/t combination of regeneration and scarring of liver. Slide 61: 4 types cirrhosis, in order of incidence: 1.Alcoholic cirrhosis, aka portal or nutritional cirrhosis, usually associated w/ alcohol abuse. 1st change in liver from excessive alcohol intake is accumulation of fat in liver cells. Uncomplicated fatty changes in liver potentially reversible if pt stops drinking alcohol. If alcohol abuse continues, widespread scar formation occurs throughout liver. 2.Postnecrotic cirrhosis -complication of viral, toxic, or idiopathic (autoimmune) hepatitis. Broad bands of scar tissue form within liver. 3.Biliary cirrhosis-ass. w/ chronic biliary obstruction & infection. diffuse fibrosis of liver w/ jaundice as main feature. 4.Cardiac cirrhosis-from long-standing, severe right-sided heart failure in pts w/cor pulmonale (enlargement of right ventricle r/t diseases of lung, thorax, or pulmonary circulation), constrictive pericarditis, & tricuspid insufficiency. Excessive alcohol ingestion single most common cause of cirrhosis b/c alcohol has direct hepatotoxic effect. some controversy as to whether cause is alcohol or malnutrition that frequently coexists w/chronic ingestion of alcohol. common problem in alcoholics is protein malnutrition. have been cases of nutritional cirrhosis resulting from extreme dieting/malnutrition. Some pt may have predisposition to cirrhosis, regardless of dietary/alcohol intake. Approx 20% of pts w/chronic hep C & 10-20% of those w/chronic hep B will develop cirrhosis. Slide 62: B/c structural changes in liver from cirrhosis, theres compression & destruction of portal & hepatic veins & sinusoids. changes cause obstruction to normal flow of blood through portal system, resulting in portal hypertension. Portal hypertension-characterized by increased venous pressure in portal circulation, splenomegaly, lg collateral veins, ascites, systemic hypertension, esophageal varices. Collateral circulation develops in attempt to reduce high portal pressure common area where collateral channels form are lower esophagus. Varicosities develop where collateral/systemic circulations communicate Gastric varices located in upper portion (cardia, fundus) of stomach-occur alone or in combo w/esophageal varies. collateral vessels contain little elastic tissue & quite fragile-tolerate high pressure poorly, & result is distended veins that bleed easily. Lg varices more likely to bleed. Esophageal varices responsible for approx 80% of variceal hemorrhageremaining 20% d/t gastric varicies varices rupture/bleed in response to ulceration & irritation. Factors producing ulceration/irritation-alcohol ingestion; swallowing poorly masticated food; ingestion of coarse food; acid regurg from stomach; & increased intraabdominal pressure caused by n/v, straining at stool, coughing, sneezing, lifting heavy objects. may have melena or hematemesis. 22 may be slow oozing or massive hemorrhage. Pt w/esophageal varices should avoid alcohol, ASA, irritating foods. Upper resp infections should be treated promptly-coughing controlled. Slide 63: Esophageal varices Slide 64: Pt who has not bled from varicies, prophylactic tx w/nonselective β-blockers (Inderal) shown to reduce risk of bleeding/bleeding-related deaths. Management w/combo of drug/endoscopic therapy more successful than either approach alone. When bleeding occurs, 1st step-stabilize pt/manage airway. IV started-may include admin. of blood products. Dx made by endoscopic exam ASAP. At time of endoscopy, sclerotherapy or banding of varices may be performed. main goal of drug therapy-stop bleeding so tx can be done. IV vasopressin produces vasoconstriction VP has many s/e, including decreased coronary blood flow & heart rate & increased BP. B/c of this, NTG often given in combo w/VP-NTG reduces detrimental effects of VP while enhancing its beneficial effect. Endoscopic sclerotherapy -sclerosing agent (Scleromate), introduced via endoscopy, thromboses & obliterates distended veins. Another procedure for acute bleeding is endoscopic ligation or banding of varices-sm rubber band slipped around base of varix. Balloon tamponade may be used in pts w/brisk esophageal or gastric hemorrhage that cant be controlled on initial endoscopy. controls hemorrhage by mechanical compression of varices. Minnesota or Sengstaken-Blakemore tube is used (Fig. 44-10). When inflated, balloons put mechanical compression on varices. Shunting Procedures Used to shunt blood away from varices Transjugular intrahepatic portosystemic shunt-fig 44-11 Portacaval shunt and Distal splenorenal shunt (Warren shunt) fig fig 44-12 Slide 66: Striae/distended abd wall veins may be present Signs of dehydration (dry tongue/skin, sunken eyeballs, muscle weakness). Hypokalemia d/t excessive loss of potassium caused by hyperaldosteronism-Low K+ levels can also result from diuretics. Sodium restriction based on degree of ascites-Initially 2g/day. severe ascites may need sodium to 250500 mg/day. usually not on restricted fluids unless severe ascites develops. Salt-poor albumin may be used to help maintain intravascular volume & adequate UOP by increasing plasma colloid osmotic pressure. Spironolactone-effective diuretic, even w/severe sodium retention-an antagonist of aldosterone & potassium sparing. loop diuretic-(Lasix), freq used in combo w/potassium-sparing drug. 23 Chlorothiazide or HCTZ may also be used, but thiazide diuretics not as potent as loop diuretics. paracentesis (needle puncture of abd cavity) done to remove ascitic fluid-reserved for pt w/impaired resp or abd pain from severe ascites. only temp measure b/c fluid tends to reaccumulate. Peritoneovenous shunt -surgical procedure provides continuous reinfusion of ascitic fluid into venous system. 1 type- LaVeen peritoneovenous shunt. tube runs from abd cavity through peritoneum, under SQ tissue, & into jugular vein or superior vena cava (Fig. 44-9). valve opens when pressure in peritoneal cavity is higher than in superior vena cava-allows ascitic fluid to flow to venous system. inspiration increases intraperitoneal pressure, causing valve to open-goal is to increase sodium & water excretion. not 1st-line therapy for ascites b/c of complications ass w/it, including thrombosis formation at venous tip of shunt, infection, fluid overload, DIC, variceal hemorrhage, & shunt occlusion. Also, do not improve survival rates. Transjugular intrahepatic portosystemic shunt- Slide 67: Grading system 0-insomnia to 4-not rousable Grading system considers LOC, intelectual function, neurologic findings considered terminal complication in liver disease. When liver unable to convert ammonia to urea, lg quantities of ammonia remain in systemic circulation. ammonia crosses blood-brain barrier & produces neurologic toxic manifestations. #factors may precipitate hepatic encephalopathy, primarily by increasing amt of circulating ammonia early (stages 0 & 1) euphoria, depression, apathy, irritability, memory loss, confusion, yawning, drowsiness, insomnia, agitation. Later (stages 2 & 3) slow/slurred speech, emotional lability, impaired judgment, hiccups, slow/deep resp, hyperactive reflexes, & + Babinski's reflex. manifestations of impending coma (stage 4) include disorientation as to time, place, or person. characteristic symptom- asterixis (flapping tremors)-may take several forms, most common involving arms/hands. When asked to hold arms stretched out, unable to hold position-series of rapid flexion & extension movements of hands. Impairments in writing-difficulty moving pen from left to right & apraxia (inability to construct simple figures). Other signs-hyperventilation, hypothermia, grimacing & grasping reflexes. Fetor hepaticus (musty, sweet breath)in some-odor from accumulation of digestive by-products liver unable to degrade Goal of tx-reduction of ammonia formation Antibiotics-to reduce bacteria in colon (neomycin sulfate,flagyl, vancomycin, etc) Lactulose-traps ammonia in gut-laxative effect expels from colon. (Give PO, enema, NG)-Constipation should be prevented Slide 69: Primary liver CA 4th most common CA in world. majority occur in males. About 80% w/primary liver CA have cirrhosis of liver-Cirrhosis risk factor regardless of cause of cirrhosis. Hepatocellular- cells of the liver. 24 Cholangiomas-tumor of a bile duct Metastatic carcinoma more common than primary carcinoma liver common site of metastatic growth b/c of its high rate of blood flow & extensive capillary network. CA cells in other parts of body commonly carried to liver via portal circulation. Cancer cells cause liver to be enlarged/misshapen. Hemorrhage/necrosis in liver common. Lesions may be singular or numerous & nodular or diffusely spread over entire liver. Some tumors infiltrate into other organs-gallbladder or into peritoneum or diaphragm. Slide 70: Want you to have a visual before I start talking about the pancreas. Slide 72: continuous, prolonged, inflammatory, & scarring process of pancreas. pancreas becomes progressively destroyed as its replaced w/fibrotic (scar) tissue. Strictures/calcifications may also occur in pancreas. Chronic pancreatitis may follow acute pancreatitis, but may also occur in absence of any hx of acute condition. CA of duodenum, or pancreas can also cause this type chronic pancreatitis. Chronic calcifying pancreatitis-inflammation & sclerosis, mainly in head of pancreas & around pancreatic duct. Increases in heavy social drinking have produced a higher incidence in countries in which the disease was previously considered rare. In US, chronic pancreatitis found almost exclusively in pt who abuse alcohol. Pseudocysts & abscesses commonly develop. Slide 73: risk increases w/age-peak incidence b/t 65-80 yrs of age s/s of pancreatic CA often similar to those of chronic pancreatitis. majority die w/in 5-12 mo of initial dx- 5-yr survival rate <5%. cause remains unknown. Pts w/DM & chronic pancreatitis at increased risk for pancreatic cancer. Risk factors-cigarette smoking 2x more likely to get pancreatic CA, family hx pancreatic CA, high-fat diet, & exposure to chemicals such as benzidine (carcinogen-formerly used to detect traces of blood in feces) & coke. Slide 74: Cholecystitis (inflammation of gallbladder) usually ass w/cholelithiasis. stones may be lodged in neck of gallbladder or in cystic duct. Cholecystitis may be acute or chronic. These conditions usually occur together. estimated 8-10% of adults in US have cholelithiasis-actual #not known b/c many asymptomatic w/stones. Cholecystectomy (removal of the gallbladder) ranks among most common surgical procedures performed in US. incidence of cholelithiasis higher in women, multiparous women, & persons over 40. Other factors-sedentary lifestyle, familial tendency, obesity. Female/fat/40 25 Slide 76: 1st –can have thousands of stones 2nd- cholesterol gallstones 3rd- x-ray with gallstones Slide 77: majority of GB carcinomas are adenocarcinomas (malignant tumor arising from glandular organ) seems to be relationship b/t CA of gallbladder & chronic cholecystitis/cholelithiasis. early symptoms insidious & similar to those of chronic cholecystitis/cholelithiasis Later symptoms usually those of biliary obstruction. When found early, surgery can be curative. Extended cholecystectomy w/lymph node dissection has improved outcomes for pts w/ GB CA. When surgery not option, endoscopic stenting of the biliary tree to reduce obstructive jaundice may be warranted. Adjuvant therapies, including radiation/chemo, may be used depending on disease state. Overall, poor prognosis. Nursing management involves supportive care w/special attention to nutrition, hydration, skin care, pain relief. Many nursing care measures used for pts w/cholecystitis/cholelithiasis freq applied, as well as nursing care for pt w/cancer Slide 78: Obstruction/ absence of extrahepatic bile ducts Atresia-congenital absence or closure of normal body opening. At birth, liver normal without inflammation-structural problem leads to cellular damage,eventual liver failure/death. cause unknown-b/c problem originates during prenatal period, viruses, toxins, chemicals cannot be ruled out. liver function (bilirubin, aminotransferases [ALT, AST]) clotting studies (prothrombin time [PT], partial thromboplastin time [PTT]) Any newborn w/conjugated hyperbilirubinemia should be evaluated completely. To r/o inborn errors of metabolism-galactosemia & alpha1-antitrypsin deficiency- produce similar initial findings, metabolic screens essential. Hepatitis & other viral titers necessary so neonatal hep can be eliminated as source of dysfunction. Urine/stool examined/urobilinogen (colorless derivative from biliruben) levels determined as indication of degree of obstruction. Percutaneous liver biopsy can provide definitive dx if bile plugs, edema, & fibrosis found in presence of normal hepatic lobular structure. Cholangiography-(radiograph of bile ducts/replace by US)used to determine extent of atresia. Slide 79: Obstruction of extrahepatic bile ducts causes obstruction of normal flow of bile out of liver & into gallbladder & sm intestine. As result, bile plugs form, causing bile to back up in liver. This process causes inflammation, edema, hepatic degeneration. Eventually liver becomes fibrotic (scarred), & cirrhosis & portal HTN develop, leading to liver failure. gradual degeneration of liver causes jaundice & hepatomegaly. 26 B/c bile not present in intestine, fat & fat-soluble vit cannot be absorbed. This condition leads to malnutrition, deficiencies in fat-soluble vitamins, & growth failure. Slide 80: During exploratory lap, size of lesion dentified & drainage attempted. If no correctable lesion found, (Kasai procedure) performed to allow bile to drain from liver. procedure allows bile to flow directly into intestine through anastomosis of jejunum Kasai procedure does provide some long-term benefits, but hepatic dysfunction will persist. main goal of procedure-allow growth /development of child until liver transplantation needs to be performed Medium-chain triglyceride (MCT) oil added to formula to increase calories or TPN provides essential nutrition. Vit malabsorption must be treated to prevent complication (A,D,E,K) Assess/tx of portal HTN w/its problems-ascites & variceal bleeding instituted. Control bleeding, restricting salt, using diuretics important in managing portal HTN Slide 81: During early disease, in 1st months of life, infant will appear jaundiced, w/mild hepatosplenomegaly & increased abd girth. As disease progresses-may appear thin, w/failure to thrive, marked jaundice, evidence of rickets caused by chronic vit D deficiency. Pruritus major problem-may develop skin infections or xanthomas (lipid deposits in skin) result of retention of cholesterol in skin. After Kasai procedure,assess for evidence of portal HTN, may include dev of ascites/GI bleeding. life-threatening, chronic problem that requires surgery, numerous health care people, repeat hospitalizations, & extended wait for transplant. Teach Calorie counts, daily wts, abd girths. NG fdg or TPN may become necessary at times. Supplement of vits A, D, E, K, & calcium, phosphate, zinc, essential for adequate nutrition. Protein may need to be limited to avoid development of hepatic encephalopathy. Bile acid binders (cholestyramine) aid in excretion of bile salts/decrease pruritus & development of xanthomas Aveeno baths can relieve severe itching. Prevent breakdown from severe scratching-gloves during sleep/apply lotions for dry skin may prevent infection Teach activities to provide developmental stimulation/use PT & OT. assessment for dev of portal HTN vital. Teach to watch for GI bleed/dev of severe edema/ascites. If these occur, sodium restriction, diuretics, IV albumin,hospitalization may be necessary. Provide info about daily care/focus parents' attention on future liver transplant & its long-term care/tx. transplantation usually occurs w/in 1st 2 years of life-should be prepared for eventual need for liver transplant & possible death of child. Teach all home care responsibilities-monitor growth & nutritional intake, mix special formulas, manage NG fdgs, provide skin care, give meds, assess for GI bleed, ascites, edema, skin infections. 27 Slide 82: During early disease, in 1st months of life, infant will appear jaundiced, w/mild hepatosplenomegaly & increased abd girth. As disease progresses-may appear thin, w/failure to thrive, marked jaundice, evidence of rickets caused by chronic vit D deficiency. Pruritus major problem-may develop skin infections or xanthomas (lipid deposits in skin) result of retention of cholesterol in skin. After Kasai procedure,assess for evidence of portal HTN, may include dev of ascites/GI bleeding. life-threatening, chronic problem that requires surgery, numerous health care people, repeat hospitalizations, & extended wait for transplant. Teach Calorie counts, daily wts, abd girths. NG fdg or TPN may become necessary at times. Supplement of vits A, D, E, K, & calcium, phosphate, zinc, essential for adequate nutrition. Protein may need to be limited to avoid development of hepatic encephalopathy. Bile acid binders (cholestyramine) aid in excretion of bile salts/decrease pruritus & development of xanthomas Aveeno baths can relieve severe itching. Prevent breakdown from severe scratching-gloves during sleep/apply lotions for dry skin may prevent infection Teach activities to provide developmental stimulation/use PT & OT. assessment for dev of portal HTN vital. Teach to watch for GI bleed/dev of severe edema/ascites. If these occur, sodium restriction, diuretics, IV albumin,hospitalization may be necessary. Provide info about daily care/focus parents' attention on future liver transplant & its long-term care/tx. transplantation usually occurs w/in 1st 2 years of life-should be prepared for eventual need for liver transplant & possible death of child. Teach all home care responsibilities-monitor growth & nutritional intake, mix special formulas, manage NG fdgs, provide skin care, give meds, assess for GI bleed, ascites, edema, skin infections. Slide 83: Necrotizing enterocolitis