034_MLP_ENG
advertisement

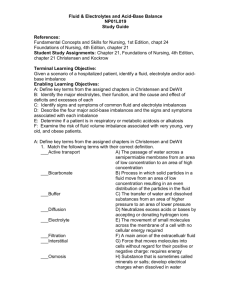
AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance Instructor Serial/Semester Location Start/Finish Time Date LESSON OBJECTIVE Performance: To gain an understanding of fluid and electrolytes and acid-base balance. Conditions: The student will be presented a powerpoint presentation by the instructor and will have all necessary references made available to him/her. Standard: 1. Given the five elements of the nursing care process and a scenario of a hospitalized patient by correctly responding to written, oral, and experiential assessment measures. TEACHING POINTS 1. Define key terms 6. 2. 7. 3. 4. 5. Identify the major electrolytes, their function, and the cause and effect of deficits and excesses of each Identify signs and symptoms of common fluid and electrolyte imbalances Describe the four major acid-base imbalances and the signs and symptoms associated with each imbalance Determine if a patient is in respiratory or metabolic acidosis or alkalosis Examine the risk of fluid volume imbalance associated with very young, very old, and obese patients. 8 9. 10. INSTRUCTIONAL STRATEGY Interactive Lecture Method: Instructor Media: Classroom Environment: OTHER LESSON SPECIFICATIONS Knowledge Lesson Type of Lesson: 1/50 Ratio: Resources: . LESSON PLAN APPROVAL End of Lesson Test: None Minutes Instructional Time: 195 Reference(s): DEWIT, S. C. (2) Fundamental Concepts and Skills for Nursing, 1st Edition, W B Saunders (ISBN: 0721669239) 01 Jan 2001 ISBN 0-323-01727-4 Foundations of Nursing, 4th Edition 01 Jan 2003 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance Signature of Standards Officer 1 Date AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance INTRODUCTION Allocated Time: Review: 5 Minutes You have had previous anatomy and physiology lectures in your combat medic training, this lecture will build upon prior instruction. Objective: To discuss/describe topics related to the nursing process. Importance: Nurses work in various health care settings so it is important to gain an understanding of this subject as it will apply to your clinical practice. Fit: The process of maintaining homeostasis is complex and ever changing. When a client is ill, this balance is easily upset. As a practical nurse, it is your responsibility to provide health care personnel with accurate information regarding your clients fluid, electrolyte and acid-base status. Approach: You will be presented the subject in lecture format and will be tested using a written exam at a later date. Control Statement: If you have any questions during the lesson please feel free to ask. BODY 1. Teaching Point: Define key terms Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Skill Lesson Learning Support: a. Adenosine Triphosphate (ATP): (1) Produced in the mitochondria from nutrients (2) It is capable of releasing energy that enables cells to work b. Active transport: (1) Force that moves molecules into cells without regard for their positive and negative charge and against concentration gradients (2) Requires energy (3) Moves fluid and electrolytes from an area of lower concentration to an area of higher concentration (4) Examples of substances actively transported: (a) Sodium 2 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (b) Potassium (c) Calcium (d) Iron (e) Hydrogen (f) Amino acids (g) Insulin provides transport for glucose c. Passive transport: movement of substances through the cell membrane. Does not require energy (1) Diffusion: (a) Movement of particles in all directions through a solution (b) Solutes move from an area of higher concentration to an area of lower concentration, which eventually results in an equal distribution of solutes within the two areas (2) Osmosis: (a) Movement of water from an area of lower concentration to an area of higher concentration (b) Equalizes the concentration of ions or molecules on each side of the membrane (c) Flow of water will continue until the number of ions or molecules on both sides of the membrane is equal (3) Filtration: (a) Transfer of water and dissolved substances from an area of higher pressure to an area of lower pressure (b) Force behind filtration is hydrostatic pressure. (c) Hydrostatic pressure: the force of fluid pressing outward on a vessel wall. The pumping action of the heart determines the amount of pressure. d. Solution classifications: (1) Isotonic: (a) A solution of same osmotic pressure as that of blood (b) Solution with the same amount of solutes as blood (2) Hypertonic: 3 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (a) A solution of higher osmotic pressure than extravascular fluids (b) Contain more solutes than blood (3) Hypotonic: (a) A solution of lower osmotic pressure (b) Solutions that contain less solutes than extravascular fluids e. Homeostasis: balance f. Fluid compartments: (1) Intracellular: (a) Larger of the two compartments (b) Fluid inside the cells within the body (2) Extracellular: any fluid outside the cells (a) Interstitial: fluid between the cells or in the tissues (b) Intravascular: fluid within the vessels. Plasma g. Bicarbonate (HCO3): (1) Main anion of the extracellular fluid (2) Alkaline electrolyte whose major function is the regulation of acid base balance (3) Acts as a buffer to neutralize acids in the body (4) Kidneys regulate amount of bicarbonate by selectively retaining or secreting it h. Buffer: (1) Blood buffers are one of the three systems that work to keep the body's pH within the narrow range of normal (2) Chemical sponges: circulate through the body in pairs and neutralize excessive acids or bases by contributing or accepting hydrogen ions i. Composition of body fluids: (1) Water: (a) Major percentage of body weight is water 4 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance 1) Newborn water content: 70 to 80% 2) Adult water content: 50 to 60% 3) Older adult water content: 45 to 50% (b) Body fat and water content: 1) Fat contains very little water 2) Females have more body fat than males; thus females have less water content 3) Obese and older adults have less body water content than average adults. (c) Functions of water: 1) Vehicle for the transportation of substances to and from the cells 2) Aids in heat regulation by providing perspiration that evaporates 3) Maintenance of acid-base balance 4) Serves as a medium for the enzymatic/chemical actions 5) Acts as a lubricant for tissues (d) Body fluid distribution: 1) Extracellular fluid: a) Approximately 1/3 of total body water b) Transports water, nutrients, oxygen, waste and other substances to and from the cells c) Infants have more extracellular fluid than adults (approximately 1/2 of TBW) 2) Intracellular fluid: a) Contains 2/3 of body fluids b) Fluid contained within the cell walls (2) Electrolytes: substances that develop electrical charges when they dissolve in water (a) Ion: particles that electrolytes break up into when dissolved in water (b) Anion: ions with a negative charge (c) Cation: ion that is positively charged 5 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (d) For each positively charged cation in a fluid compartment, there must be a negatively charged anion so that balance is maintained (e) Milliequivalent (mEq): measure of chemical activity or chemical combining power of an ion (3) Non-electrolytes: substances that remain bound together when dissolved in body fluids (4) Blood: (a) 4 to 6 liters of circulating blood volume depending on body size and sex (b) Any condition that alters body fluid volume also alters the plasma volume of the blood Knowledge Lesson: Question: Answer: Check on Learning In a knowledge lesson, pose questions to the class. What does mEq/L stand for? The measure of chemical activity or chemical combing power of an Ion. Skill Lesson: In a skill lesson, provide practice and watch students perform a skill. 2. Teaching Point: Identify the major electrolytes, their function, and the cause and effect of deficits and excesses of each Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Skill Lesson Learning Support: a. Sodium (NA): (1) The major extracellular electrolyte (cation) (2) Normal range: 134-142 mEq/L (3) Functions of sodium: (a) Principle role is the regulation and distribution of fluid volume in the body (b) Regulates osmotic pressure because water follows sodium in the body (c) Stimulates condition of nerve impulses and helps maintain neuromuscular irritability (d) Important in controlling contractility of muscles, especially the heart (4) Hyponatremia: 6 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (a) A less than normal concentration of sodium in the blood (b) Occurs when there is a sodium loss or a water excess 1) Sodium loss: The body compensates by decreasing water excretion 2) Water excess: dilutes all blood components 3) As sodium levels decrease in the extracellular fluid, water is pulled into the cells. This causes them to swell (c) Causes: 1) Loss of GI fluids, vomiting, diarrhea 2) GI or biliary drainage via nasogastric tube 3) Fistulas, small bowel obstructions 4) Loss through skin, diaphoresis 5) Large open lesions, burns 6) Massive edema, shifting of body fluids, ascites (5) Hypernatremia: (a) Greater than normal concentration of sodium (b) Occurs when there is an excess of sodium or a decrease in body water 1) The body attempts to correct the imbalance by conserving water through renal reabsorption 2) Causes fluid to shift from the cells to the interstitial spaces, resulting in cellular dehydration (c) Causes: 1) More water than sodium is lost from the body 2) Abnormally large intake of sodium a) Taking too many salt tablets b) Overuse of tablet salt c) IV saline infused too quickly d) Prepared foods; frozen, canned, smoked 7 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance e) Dairy products in large amounts f) Consumption of antacids containing sodium b. Potassium (k): (1) Dominant intracellular cation (2) Normal range: 3.5 to 5 mEq/L (3) Functions: (a) Main function of potassium is regulation of water and electrolyte content within the cell (b) Promotes transmission of nerve impulses (c) Promotes the function of skeletal muscles (d) Regulation of acid-base balance (4) Hypokalemia: (a) Decrease in the body's potassium level (b) Occurs when kidneys do not conserve potassium or large amounts of potassium is lost through GI system (c) Hypokalemia can affect skeletal and cardiac function. The resulting weakness causes lifethreatening cardiac conduction abnormalities (d) Causes: 1) Decreased potassium intake: poor diet 2) Increased potassium loss a) Increased aldosterone activity b) GI Losses: Vomiting, diarrhea, GI suctioning c) Potassium losing diuretics: Lasix d) Loss from cell damage: trauma, burns, fistulas e) Excessive sweating 3) Conditions that cause very large urine output (5) Hyperkalemia: 8 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (a) An increase in body's serum potassium level (b) Occurs most often in renal disease when the kidneys can not properly excrete potassium (c) Hyperkalemia is very dangerous because of cardiac arrest, which is caused by potassium's over stimulation of the cardiac muscle (d) Causes: 1) Potassium intake in excess of kidney's ability to excrete a) Oral: Excessive consumption of foods high in potassium b) Parenteral: IV solutions containing potassium. Potassium should not be infused at more than 10 mEq/hour 2) Excessive use of salt substitution 3) Renal failure 4) Adrenal insufficiency: Addison's disease 5) Excessive trauma to cells: burns, crush injuries and chemotherapy 6) Medications: potassium sparing diuretics, beta blockers, ACE inhibitors, NSAIDS, Aminoglycosides c. Chloride: (1) Extracellular anion (2) Normal range: 96 to 105 mEq/L (3) Functions: (a) Necessary for the formation of hydrochloric acid in gastric juices (b) Assists in regulation of osmotic pressure between the compartments (c) Assists in the regulation of acid-base balance (4) Hypochloremia: decreased chloride in the body (a) Usually occurs when sodium is lost because sodium and chloride are frequently paired (b) Most common causes are vomiting and prolonged nasogastric or fistula drainage (5) Hyperchloremia: increased chloride in the body (a) Rarely occurs but can be seen when bicarbonate levels fall 9 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (b) Chloride anions attempt to compensate to maintain equal number of cations in the body fluid d. Calcium: (1) Positively charged ion. 99% is concentrated in the bones and teeth (2) Normal range: 9 to 11 mg/dl (3) Calcium is deposited into the bones and mobilized as needed to keep the blood level constant during periods of insufficient intake (4) Vitamin D, calcitonin and parathyroid hormone are needed for the absorption and utilization of calcium (5) Functions: (a) Required for the formation and maintenance of strong bones and teeth (b) Necessary for normal clotting (c) Has a depressing or sedating effect on neuromuscular irritability and thus promotes normal transmission of nerve impulses. It helps regulate normal muscle contraction and relaxation (d) Establishes the thickness and strength of cell membranes (e) Acts as an enzyme activator for chemical reactions in the body (6) Hypocalcemia: decreased calcium levels in the blood (a) Causes: 1) Infusion of excess amounts of citrated blood. (citrates bind to calcium ions) 2) GI: a) Excessive loss through diarrhea b) Inadequate dietary intake of calcium or vitamin D c) Disease of the small bowel 3) Parathyroid function: a) Surgical removal of parathyroid gland b) Decrease function of parathyroid 4) Pancreatic disease 10 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance 5) Medications: anticonvulsants, diuretics 6) Severe burns (b) Causes muscle irritability (7) Hypercalcemia: increased levels of calcium (a) Causes: 1) Calcium stores from bone enters circulation a) Immobilization b) Bone loss c) Metastatic bone cancer 2) Increased dietary intake of calcium or vitamin D 3) Antacids containing calcium 4) Increased parathyroid hormone (b) Neuromuscular activity is depressed and renal calculi may develop e. Phosphorus: (1) Intracellular anion (2) Normal range: 2.7 to 4.5 mg/dl (3) Phosphorus and calcium have an inverse relationship; an increase in one causes a decrease in the other (4) Majority of phosphorus is found in the bones and teeth combined with calcium (5) Functions: (a) Supports the maintenance of bones and teeth (b) Acts as a buffer to regulate the body's acid-base balance (c) Promotes the effectiveness of many of the B vitamins (d) Assist in normal nerve and muscle activity (e) Participates in carbohydrate metabolism (6) Hypophosphatemia: decreased levels of phosphorus in the blood 11 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (a) Causes: 1) Dietary insufficiencies 2) Impaired kidney function (b) Muscle weakness, especially the respiratory muscles, and muscle spasms can be caused by hypophosphatemia (7) Hyperphosphatemia: increased levels of phosphorus (a) Causes: 1) Renal insufficiency 2) Increased intake of phosphate or vitamin D (b) Tetany and muscle spasms may occur f. Magnesium: (1) Intracellular cation (2) Normal range: 1.5 to 2.4 mEq/L (3) 60% is found in the bone, 39% in muscle and soft tissue, 1% in extracellular fluids (4) Function: (a) Cofactor in the activation of many enzymes (b) Promoted regulation of serum calcium, phosphate and potassium levels (c) Essential for integrity of nervous tissue, skeletal muscle and cardiac functioning (5) Hypomagnesemia: decreased level of magnesium in the blood (a) Causes: 1) Decreased intake: a) Prolonged malnutrition b) Starvation 2) Impaired absorption from GI tract: a) Alcoholism 12 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance b) Diarrhea c) Draining intestinal fistulas 3) Conditions that cause large losses of urine (b) A decrease in magnesium often parallels decreased potassium, because if the magnesium level is low, the kidneys tend to excrete more potassium (6) Hypermagnesemia: increased levels of magnesium in blood (a) Causes: 1) Impaired renal function 2) Excessive magnesium administration 3) Severe water loss associated with diabetic ketoacidosis (b) Rarely occurs when kidney function is normal g. Bicarbonate: (1) Extracellular anion (2) Normal range: 22 to 24 mEq/L (3) Functions: (a) Regulation of acid-base balance (b) Acts as a buffer to neutralize acids in the body and maintain homeostasis Knowledge Lesson: Question: Answer: Check on Learning In a knowledge lesson, pose questions to the class. What is the chief intracellular ion? Potassium. Skill Lesson: In a skill lesson, provide practice and watch students perform a skill. 3. Teaching Point: Identify signs and symptoms of common fluid and electrolyte imbalances Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Skill Lesson 13 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance Learning Support: a. Fluid volume: (1) Normal fluid intake: (a) Water loss replenishment: 1) Ingestion of liquids and food 2) Metabolism of food and in body tissues (b) Average daily intake: 2500 mls (2) Fluid loss: (a) Sensible fluid loss: fluid loss that can be measured 1) Kidneys 2) GI tract (bowel) (b) Insensible fluid loss: fluid loss that cannot be measured 1) Skin 2) Lungs (c) Average daily fluid loss: 2500 mls (3) Kidneys play an important role in fluid balance. If not functioning properly, the body has great difficulty regulating fluid balance (a) Must excrete a minimum of 30 ml/hr of urine to eliminate waste products from the body (b) Kidney must respond to fluid changes by increasing, decreasing, concentrating or diluting urine output (4) Water balance can be determined by weighing a client (a) Client must be weighed under the exact same conditions each time 1) Same time of day 2) Same clothing 3) Same equipment attachments (b) One liter of fluid equals 1 kg (2.2 lbs): A change of 1 kg will reflect a loss or gain of 1 liter of body fluid 14 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance b. Fluid volume deficit (hypovolemia): (1) When a fluid deficit occurs, it causes loss of water from the cells (dehydration) (2) Causes: (a) Inadequate fluid intake (b) Severe diarrhea or vomiting (c) Severe burns (d) Hemorrhage (e) Profuse perspiration or urination (3) Signs and symptoms: (a) Thirst (b) Weakness (c) Postural hypotension, complaints of dizziness (d) Decrease urine production: dark, concentrated urine (e) Dry, cracked lips, tongue and mucous membranes; thick saliva (f) Dry, scaly skin; poor skin turgor 1) Skin turgor: degree of elasticity 2) The client that is dehydrated will have tenting. (Tenting: When loose skin is pinched, it remains elevated for several seconds afterwards) (g) Flat neck veins when lying down (h) Increased pulse rate; weak, thready pulse (i) Elevated temperature (j) Weight loss (4) Nursing care: (a) Evaluate intake & output records (b) Monitor urine concentration: 15 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance 1) Specific gravity: Concentration of urine is compared to concentration of distilled water 2) When urine becomes more concentrated related to decreased fluid volume, specific gravity will be high (c) Daily weights: Weigh client at the same time each day (d) Assess skin turgor (e) Monitor vital signs: orthostatic hypotension (f) Offer oral fluids at frequent intervals if able to take PO (g) Monitor hematocrit: 1) Usually increased related to hemoconcentration 2) Hematocrit: percentage of formed elements of the blood related to the fluid part of the blood 3) When fluid volume decreases while formed elements stay the same, the hematocrit increases c. Fluid volume excess (hypervolemia): (1) An excess or increase in the body's fluid volume. High volume of fluid in the intravascular compartments (2) Causes: (a) Take in more fluid than can excrete: 1) Rapid infusion of IV fluids 2) Tap water enemas 3) Excessive drinking of water (b) Excessive salt intake: Water follows sodium in the body (c) Disease processes that cause fluid retention: 1) Renal failure 2) Congestive heart failure 3) Cushing's syndrome (d) Corticosteroid therapy (3) Signs and symptoms: 16 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (a) Weight gain (b) Crackles in lungs; pulmonary edema and ascites (c) Slow, bounding pulse (d) Elevated blood pressure (e) Distended neck veins (f) Diluted urine (g) Edema: 1) Excessive accumulation of interstitial fluid 2) Fluid tends to accumulate in dependent areas a) Ambulatory clients: accumulates in the lower extremities b) Bed ridden clients: accumulates in sacral area 3) Generalized edema: occurs when excessive fluid is spread throughout the body. Most visible in the hands and face (4) Nursing care: (a) Monitor urine concentration: 1) Decreased specific gravity 2) Pale colorless urine (b) Monitor edema: 1) Puffy eyelids 2) Swollen hands 3) Pitting: a) A depression in the skin that occurs when a fingertip is pressed into the tissue over a bony prominence and held for 5 secs b) After the finger is removed, the pit slowly disappears 4) Measure circumference of the affected extremity (c) Monitor vital signs 17 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (d) Monitor client weight (e) Monitor client lung sounds (f) If on fluid restriction, offer fluids at regular intervals throughout the waking hours (g) Monitor skin for breakdown, reposition client q 2 hrs (h) Monitor hematocrit for hemodilution: hematocrit will decrease d. Sodium imbalances: (1) Hypernatremia: (a) Signs and symptoms: 1) Headache; apathy 2) Muscle weakness; fatigue 3) Postural hypotension 4) Abdominal cramps; nausea/vomiting 5) Severe or prolong deficit: a) Shock b) Mental confusion c) Coma (b) Nursing care: 1) Monitor input and output 2) Observe for abnormal GI, renal or skin losses 3) Replace fluid loss with fluids containing sodium not plain water (2) Hypernatremia: (a) Signs and symptoms: 1) Dry, tenacious membranes 2) Low urinary output 3) Firm, rubbery tissue turgor 18 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance 4) Severe or prolonged excess: a) Manic excitement b) Tachycardia c) Death (b) Nursing interventions: 1) Monitor I&Os. Encourage increased fluid intake 2) Decreased sodium in the diet. Foods high in sodium: a) Canned foods: meats, fish, vegetables, soups b) Cheeses, lunchmeats, ham, hot dogs, processed foods c) Salted snacks: nuts, popcorn, snack foods d) Tomatoes and vegetable juices e) Packaged mixes: gravy mixes, casserole & pasta mixes 3) Monitor water loss from fever, infection and increased respirations e. Potassium imbalances: (1) Hypokalemia: (a) Signs & symptoms: 1) Skeletal muscle weakness, leg cramps 2) Decreased bowel sounds, constipation, anorexia, nausea, vomiting 3) Diminished deep tendon reflexes, lethargy, paralysis involving the respiratory muscles 4) Cardiac dysrhythmias, ECG changes 5) Severe or prolonged deficit: a) Flaccid paralysis b) Kidney damage c) Paralytic ileus d) Cardiac or respiratory arrest 19 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (b) Nursing interventions: 1) Instruct clients on foods high in potassium; especially those client taking diuretics. Encourage intake a) Fruits: raisins, bananas, oranges, dates, apricots, cantaloupe b) Vegetables: avocado, potatoes, broccoli, carrots c) Meats, salmon, tuna, cod fish d) Milk, nuts and peanut butter 2) Instruct client taking on signs of digitalis toxicity 3) Administer replacements as ordered. IV potassium should not be given faster than 10 mEq/hour 4) Monitor bowel sounds and EKG 5) Monitor I&Os (2) Hyperkalemia: (a) Signs and symptoms: 1) Irritability 2) Nausea/vomiting, diarrhea, colic 3) Cardiac dysrhythmias, EKG changes 4) Numbness, tingling, paresthesia 5) Skeletal muscle weakness 6) Severe or prolonged excess: a) Flaccid paralysis b) Cardiac arrest c) Anuria (b) Nursing interventions: 1) Decrease intake of foods high in potassium and salt substitutes 2) Administer Kayexalate as ordered (cation-exchange resin) 3) Monitor telemetry, I&Os, serum level 20 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance 4) Monitor bowel sounds and number of stools. f. Chloride imbalances: Because chloride imbalances rarely occur independently of other electrolyte imbalances, there are no specific signs and symptoms to identify a chloride imbalance g. Calcium imbalances: (1) Hypocalcemia: (a) Signs and symptoms: 1) Osteoporosis, pathological fractures 2) Tingling around nose, mouth, ear, fingers, toes 3) Muscle spasms of feet and hands 4) Tetany 5) Laryngeal spasms 6) Nausea/vomiting, diarrhea 7) Hyperactive deep tendon reflexes 8) Cardiac dysrhythmia, cardiac arrest 9) Tests for hypocalcemia: a) Chvostek's sign: contraction of facial muscles in response to a light tap over the facial nerve in front of the ear b) Trousseau's sign: carpal spasm induced by inflating a blood pressure cuff above the systolic pressure for a few minutes (b) Nursing interventions: 1) Monitor vital signs 2) Encourage diet high in calcium rich foods, vitamin D and protein 3) Administer replacement as ordered 4) Monitor respiratory status; be alert for stridor, dyspnea 5) Acute hypocalcemia: Keep tracheotomy tray and resuscitation equipment at bedside in case of laryngeal spasms 6) Monitor telemetry, serum levels and I&Os 21 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance 7) Falls precautions (2) Hypercalcemia: (a) Signs and symptoms: 1) Thirst, polyuria 2) Renal stones 3) Decreased deep tendon reflexes 4) Lethargy, confusion, coma 5) Decreased muscle tone 6) Decreased GI motility and abdominal pain 7) Cardiac dysrhythmias, cardiac arrest (b) Nursing interventions: 1) Administer diuretics as prescribed 2) Encourage increased PO fluids 3) Monitor I&Os h. Phosphorus imbalances: (1) Hypophosphatemia: (a) Signs and symptoms: 1) Muscle weakness; especially the respiratory muscles 2) Confusion, seizures, coma 3) Numbness (b) Nursing interventions: 1) Assess for vitamin D deficiency or hyperparathyroidism 2) Educate client on hazardous overuse of aluminum containing antacids (2) Hyperphosphatemia: (a) Signs and symptoms: 22 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance 1) Tetany 2) Numbness, tingling around the mouth 3) Deep muscle spasms 4) Anorexia, nausea, vomiting (b) Nursing interventions: 1) Monitor muscle spasms 2) Monitor electrolyte levels i. Magnesium imbalances: (1) Hypomagnesemia: (a) Signs and symptoms: 1) Anorexia, nausea, vomiting, dysphagia 2) Mental status changes, agitation, depression, confusion, seizures 3) Hyperactive deep reflexes, leg and foot cramping 4) Paresthesia, twitching, tremors 5) Positive Chvostek and Trousseau signs 6) Vertigo (b) Nursing interventions: 1) Monitor vital signs, I&Os, telemetry, respiratory status 2) Assess neuromuscular status and dysphagia 3) Administer replacements per orders 4) Encourage increase in magnesium containing foods: a)Chocolate b) Nuts c) Soybeans d) Green, leafy vegetables 23 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance e)Whole grains 5) Institute seizure precautions (2) Hypermagnesemia: (a) Signs and symptoms: 1) Hypotension 2) Sweating and flushing, thirst 3) Nausea/vomiting 4) Loss of deep tendon reflexes, muscle weakness, paralysis 5) Respiratory depression 6) Prolonged or severe excess: a) Coma b) Cardiac arrest (b)Nursing interventions: 1) Promote urine excretion through increased fluid intake and/or diuretics as prescribed 2) Teach clients to avoid overuse of laxatives and antacids containing magnesium 3) Monitor I&Os 4) Monitor vital signs Knowledge Lesson: Question: Answer: Check on Learning In a knowledge lesson, pose questions to the class. In what electrolyte imbalances are Chvostek and Trousseau signs positive? Hypocalcemia and Hypomagnemia Skill Lesson: In a skill lesson, provide practice and watch students perform a skill. 4. Teaching Point: Describe the four major acid-base imbalances and the signs and symptoms associated with each imbalance Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson 24 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance Skill Lesson Learning Support: a. Acid-base balance: (1) Definition - homeostasis of the hydrogen ion concentration in the body fluids (2) Hydrogen ion concentration is determined by the ratio of carbonic acid to bicarbonate in the extracellular fluids (1:20) (3) pH - hydrogen ion concentration in the body. Measure of the degree to which a solution is acid or alkaline (a) Alkaline (base) - fewer hydrogen ions in a solution. Causes the pH to increase greater than 7.45 (b) Acid - increase in hydrogen ions in a solution. Causes the pH to decrease less than 7.35 (c) Normal pH - 7.35 to 7.45 b. Acid-base imbalances: (1) Two types of disturbances that cause a pH imbalance: (a) Addition or subtraction of acid substances - carbonic acid (b) Addition or subtraction of base substances - bicarbonate (2) Body effects on acid-base balances: (a) Body's metabolism affects the base side of balance. Bicarbonate imbalances cause metabolic acidosis or alkalosis (b) Body's respiratory system affects the acid side of balance. Carbonic imbalances cause respiratory acidosis or alkalosis (3) Three systems that work to keep the pH in the normal range: (a) Blood buffers: 1) Chemical sponges 2) Circulate in pairs of weak acids and weak basis and neutralize the body fluids 3) Immediate response - fraction of a second (b) Respiratory system: 1) Second line of defense 2) Speeding up or slowing down of respiratory rate, the lungs can increase or decrease the amount of carbon dioxide in lungs 25 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance a) Carbon dioxide removed from the blood, carbonic acid level is lowered b) Respiratory system regulates pH by removing carbon dioxide from the blood by decreasing or increasing the removal rate 3) Quick response: within minutes (c) Kidneys: 1) Third line of defense 2) Excrete varying amounts of acids or bases based on the pH level of the blood 3) Normal urine is acid because the body produces excess acids in the metabolic processes 4) Show response: may take hours to days; but more precise c. Types of imbalances: (1) Respiratory acidosis: (a) A retention of carbon dioxide occurs with resultant increase in carbonic acid in the blood. pH decreases (b) Shallow respirations result because of the retained carbon dioxide (c) Depression of central nervous system activities occurs (d) Cause: any condition that impairs normal ventilation 1) Compromise in ventilation, perfusion or diffusion 2) Pneumonia 3) Respiratory failure, paralysis of respiratory muscles 4) Atelectasis 5) Traumatic injuries to the thorax, head injuries 6) Obesity 7) Airway obstructions: COPD, asthma (e) Signs and symptoms: 1) Central nervous system: a) Lethargy, disorientation 26 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance b) Occipital headache, dizziness c) Decreased level of consciousness, coma 2) Cardiopulmonary system: a) Dyspnea b) Tachycardia, cardiac dysrhythmias c)Hypertension 3) Musculoskeletal system: tremors, weakness (f) Mode of compensation: Kidneys will retain increased amounts of bases. (2) Respiratory alkalosis: (a) Loss of excessive amounts of carbon dioxide with a resultant lowering of the carbonic acid level in the blood (b) pH rises because of the decrease in carbonic acid being blown off with each exhalation (c) Causes: hyperventilation, respirations that increase in rate, depth or both 1) Anxiety, fear 2) Anemia 3) Head injuries or infections 4) Aspirin overdose 5) Asthma, pneumonia 6) Inappropriate mechanical ventilator settings (d) Signs and symptoms: 1) Anxious, irritable appearance 2) Tingling of extremities 3) Fainting, dizziness 4) Tachypnea, cardiac dysrhythmia 5) Tetany, muscle weakness 27 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (e) Mode of compensation: Kidneys will excrete increased amounts of base to lower pH (3) Metabolic acidosis: (a) Gain of hydrogen ions or loss of bicarbonate (b) Causes: 1) Starvation 2) Dehydration, diarrhea 3) Diabetic ketoacidosis, shock 4) Renal failure, renal tubular acidosis 5) Drugs: methanol, ethanol, aspirin (c) Signs and symptoms: 1) Lethargy, headache, decreased level of consciousness 2) Kussmaul respirations, cardiac dysrhythmias 3) Anorexia, nausea/vomiting, diarrhea 4) Weakness (d) Mode of compensation: Lungs blow off CO2 to raise pH (hyperventilation) (4) Metabolic alkalosis: (a) Significant amount of acid is lost from the body or an increase in the bicarbonate level occurs (b) Depresses the central nervous system (c) Causes: 1) Excessive vomiting: most common cause 2) Prolong gastric suctioning 3) Electrolyte disturbances 4) Cushing's disease, hyperaldosteronism 5) Drugs: steroids, sodium bicarbonate, diuretics, overdose of baking soda, excessive use of antacids such as Mylanta (d) Signs and symptoms: 28 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance 1) Headache, irritability, lethargy, decreased level of consciousness 2) Atrial tachycardia, slow shallow respirations with periods of apnea, bradycardia 3) Nausea, vomiting 4) mbness and tingling of extremities, hypertonicity of muscles, tetany (e) Mode of compensation: Lungs retain CO2 to lower pH Knowledge Lesson: Question: Answer: Check on Learning In a knowledge lesson, pose questions to the class. What is the most common cause of metabolic alkalosis? Vomiting. Skill Lesson: In a skill lesson, provide practice and watch students perform a skill. 5. Teaching Point: Determine if a patient is in respiratory or metabolic acidosis or alkalosis Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Skill Lesson Learning Support: a. Normal Arterial Blood Gas (ABG) values: (1) pH: 7.35-7.45 (2) PaCO2: 35-45 mm Hg (3) P02: 80-100 mm Hg (4) O2 saturation: 95-100% (5) HCO3: 22-26 mEq/L b. Respiratory acidosis: (1) pH: less than 7.35 (2) PaCO2: greater than 45 mm Hg (3) PaO2: normal or below 80 mm Hg (4) O2 Sat: normal or below 95% 29 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance (5) HCO3: normal in early stages c. Respiratory alkalosis: (1) pH: greater than 7.45 (2) PaCO2: less than 35 mm Hg (3) PaO2: normal (4) O2 sat: normal (5) HCO3: normal d. Metabolic acidosis: (1) pH: less than 7.35 (2) PaCO2: normal or less than 35 mm Hg (3) PaO2: normal or decreased (4) O2 sat: normal (5) HCO3: below 22 mEq/L e. Metabolic alkalosis: (1) pH: greater than 7.45 (2) PaCO2: normal or greater than 45 mm Hg (3) PaO2: normal (4) O2 sat: normal (5) HCO3: above 26 mEq/L Knowledge Lesson: Question: Answer: Skill Lesson: 30 Check on Learning In a knowledge lesson, pose questions to the class. The client has the following ABG values. What acid-base disturbance might he be experiencing? pH: 7.3, PaCO2 25mm Hg, PaO2: 75, O2 Sat: 98%, HCO3: 20mm Hg Metabolic acidosis. In a skill lesson, provide practice and watch students perform a skill. AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance 6. Teaching Point: Examine the risk of fluid volume imbalance associated with very young, very old, and obese patients. Minutes Allocated Time: Introduction: Learner Participation: Knowledge Lesson Skill Lesson Learning Support: a. Very young clients: (1) Babies have the highest percentage of water content: 50-60% (2) Over ½ of an infant’s fluid is extracellular fluid. Extracellular fluid is lost from the body more rapidly than intracellular fluids, thus infants are at a greater risk for dehydration (3) In infants, a loss of 5% of body fluid is significant. 15% is fatal (4) Signs of severe fluid volume deficit in the infant include sunken eyeballs and depression of the anterior fontanel b. Obese client: (1) Fat cells contain very little water. Therefore, the more obese an individual the smaller percentage of body water (2) Because they have less of a reserve, they are at a greater risk for complications related to dehydration (3) A loss of 10% body fluid is serious. 20% is fatal c. Older adults: Older adults are at an increased risk for dehydration because of: (1) Fat replaces lean muscle mass with aging, leading to decrease in total body fluid (2) The aging kidney is less able to concentrate urine, leading to increased fluid loss (3) Decreased mobility and diminished sense of thirst often result in decreased fluid intake (4) Incontinent older adults may restrict fluid to reduce the frequency of urination (5) To compensate for changes in taste, older adults may over-salt their food, resulting in electrolyte and fluid imbalances (6) Physiological changes in the skin and mucous membrane make them less reliable indicators of dehydration (7) Dehydration may first manifest as mild disorientation and be misdiagnosed 31 AFAMS Master Lesson Plan (MLP) Nursing Program Fluid & Electrolytes and Acid-Base Balance Knowledge Lesson: Question: Answer: Check on Learning In a knowledge lesson, pose questions to the class. What are signs of severe dehydration in the infant? Sunken eyeballs and depression of the anterior fontanel. Skill Lesson: In a skill lesson, provide practice and watch students perform a skill. END OF LESSON TEST Allocated Time: Instructions: Test Questions or Performance Expected: Test Key: 0 Minutes CONCLUSION Allocated Time: Summary: 5 Minutes Review and re-emphasize the difficult Teaching Points below. 1. 2. 3. 4. 5. 6. Define key terms Identify the major electrolytes, their function, and the cause and effect of deficits and excesses of each Identify signs and symptoms of common fluid and electrolyte imbalances Describe the four major acid-base imbalances and the signs and symptoms associated with each imbalance Determine if a patient is in respiratory or metabolic acidosis or alkalosis Examine the risk of fluid volume imbalance associated with very young, very old, and obese patients. 7. 8 9. 10. Closing Statement: Nurses work in various health care settings so it is important to gain an understanding of this subject as it will apply to your clinical practice. Re-motivating Statement: The process of maintaining homeostasis is complex and ever changing. When a client is ill, this balance is easily upset. As a practical nurse, it is your responsibility to provide health care personnel with accurate information regarding your clients fluid, electrolyte and acid-base status. 32