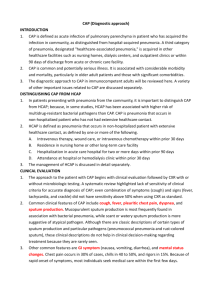
Pneumonia - aaronsworld.com
advertisement

PNEUMONIA Definition Acute infection of lung parenchyma including alveolar spaces and/or interstitial tissue. Causative agent may be bacterial, viral, mycoplasmal, or fungal. Symptoms Pneumococcal: often preceded by URI, onset sudden with single shaking shill, followed by fever, pain with breathing on affected side, cough, dyspnea, and sputum production. Pain mb referred. Temp rises rapidly to 100.4-105 F, pulse 100-140/min, respirations 20 to 45/min. Also common are nausea, vomiting, malaise, myalgias. Cough dry mb initially, but usually becomes productive with purulent, blood streaked or "rusty" sputum. In patients at age extremes, symptoms may not be as obvious. Pneumocystis: progressive dyspnea, tachypnea, cyanosis; dry, nonproductive cough evolving in subacute fashion over several weeks or acutely over several days. Nearly all patients have immunologic deficiencies. Viral: Headache, low fever, myalgia, cough producing mucopurulent sputum Mycoplasmal: initially resembles influenza, with malaise, sore throat and dry cough. Sx increase in severity, mb paroxysm of coughing with production of sputum that is mucoid, mucopurulent, or blood-streaked. Progression gradual (unlike pneumococcal). Acute sx persist 1-2 wks followed by gradual recovery. Maculopapular rashes (erythema multiforme) occur in 10-20%. Coccidiomycosis (San Joaquin Valley Fever): ssx mild to severe- moderate fever, cough, pleural pain, headache, weakness, erythema nodosum or multiforme. Secondary forms can occur weeks or months after primary infx and can lead to abscess, meningitis, or bone infection Histoplasmosis: as in Coccidiomycosis, or may present like influenza. A progressive form can be chronic and look like TB. Mb hepatomegaly, splenomegaly, lymphadenopathy, uveitis, retinitis. DDx Etiology/Epidemiology Pneumococcus (Strep pneumoniae) causes 60-80% of bacterial pneumonias, others caused by Hemophilus influenza, Klebsiella, group A beta Strep, Legionella, Pneumocystis carinii Predisposing factors: respiratory viral infection, alcoholism, age extremes, debility, immunosuppressive disorders and therapy, compromised consciousness, dysphagia, exposure to transmissible agents. Mechanism: inhalation of droplets small enough to reach alveoli, aspiration of secretions from upper airways, hematogenous dissemination via lympatics, directly from contiguous infections Pathophysiology (RF) mycoplasma pneumoniae is a frequent cause of atypical pneumonia; it behaves as a extracellular human parasite and incites epithelial damage of the airways -interstitial inflammation resembling viral inflammation of intra cellular septa -no severe exudate as in bronchial bacterial pneumonia -Pneumonia Infections Klebsiella & Enterobacteria -Klebsiella produces severe pneumonia -more resistant to antibiotics than E. Coli -bronchiopneumonia ,in chronic alcoholics without homes, which produces pus and exudate that plugs airway and prevents air escape PNEUMONIA Pneumocystis carinii (Protozoa) -no life cyle outside human -lives as a commensal grazing on epith. lining of the alveolar cells (I &II) -fairly common, only appears: long term corticosteriods, immune suppressed, children in Somalia(protein and calorie def.) -principal reasons for activation: not held at bay by macrophages because no T cell support; AAlso long term malignancies: ie. Hodgkins-pneumocytis secondary to it. Pneumococcus (Strep pneumoniae) -classified under strep as s. pneumoniae -present in 60 % of individuals in the winter time in nasal secretions; sensitive to pencillin -a gram positive diplococcus; 80 serotypes based on different cell capsules; normally colonize the pharynx -carbohydrate capsule around cell wall is slippery, so neutrophils have difficulty phagocytotizing it. -damage of mucociliary escalator can predispose to pathogenesis -most common cause of lobar pneumonia but can also produce bronchopneumonia, upper respiratory infections, sinusitis, middle ear infections(major cause of infection in children), and mastoid infections -severe consequences are meninigitis or brain abscess when it spreads through the blood -pneumococcal pneumonia has a high mortality if untreated; seen among the aged, debilitated, and immunosuppressed -disseminate to pneumococcemia, a serious consequence which can lead to meningitis (40% mortality rate even when treated) Key PE EXAM Pneumococcal: mb pleural rub, increased fremitus, local fine crackles, dullness, bronchial breath sounds, pectoriloquy, egophony Pneumocystis: minimal auscultatory signs except perhaps diffuse crackles Viral: diffuse fine crackles and wheezes or WNL Mycoplasma: as in bacterial or WNL Fungal: physical signs mb absent, or occasional rales and areas of dullness to percussion mb present X-RAY Pneumococcal: dense consolidation usually unilateral, confined to single lobe Pneumocystis: diffuse bilateral interstitial infiltrates Viral: interstitial pneumonia or peribronchial thickening, or WNL Mycoplasmal: variable, but most commonly show patchy bronchopneumonia in lower lobes Key Lab CBC, sputum gram stain/culture Pneumococcal: leukocytosis w/ shift to left, gram stain shows gram + lancet-shaped diplococci in short chains, >=10 typical morphotypes per oil immersion Pneumocystis: organism identified on stained slide of lung material derived from bronchial brushing, open lung biopsy; aspirates of tracheobronchial mucous mb positive as well Viral: peripheral WBC count often low, but mb normal or moderately elevated Mycoplasmal: Gram stain shows sparse bacteria, mixture of PMNs and macrophages, and clumps of desquamated respiratory epithelial cells. Fungal: skin test 10-20 days after infection; organism found in sputum; eos mb high Strategy Evaluate carefully: fulminant cases in the compromised patient must receive aggressive therapy in hospital setting. Skilled Dx based on history, palpation and auscultation obviates the need for X-Ray (RB) Very responsive to drugless therapy in appropriately selected cases (2) PNEUMONIA TX PROTOCOLS Nutrient Considerations Vit A 25,000-100,000 IU/day (2,10); dose varies w/ viscosity of mucous (BB) Vit C 500-1000 mg/hr (2,10) Vit E, B-complex, Zn & Se(2,10); Bioflavonoids (EM,10) Adequate protein (10) and water (2) Glandulars: Thymus, lymph, spleen (2) Eliminate dairy and known allergens (2) Calcium: 1000 mg qd (viral/mycoplasma) Magnesium: 500 mg qd Zinc: 50 mg qd B complex Vit D 4000 qd Dietary Considerations Pneumococcal pneumonia: papaya, pineapple, sprouts Botanicals Tnct: Phytolacca(4)-Glycyrrhiza fl.ext.(4)-Echinacea(4)-Grindelia(2)-Lobelia(2) sig: 30 gtt qid (RB) Glycyrrhiza powdered extract (EM) Anti-inflammatory. Eucalyptus oil: Steam inhalation (EM, 5) Anti-bacterial. Bryonia alba tnct: 1-5 bid. (11,5) With sharp chest pain. Allium sativa (12) Aconite tnct: 1/2-2 minim (5) Ipecac, Turpentine, or Strophanthus (5) Symphytum, Veratrum, Quebracho, or Asclepias (6) Sanguinaria Viral pneumonia: Lomatium isolate, Thymic fractions (SSL) Pneumococcal pneumonia: Valerian fluid ext: 10 gtt qid, Echinacea tinct: 30 gtt 5x/day Hydrastis tinct: 20 gtt qid, Leptandra tinct: 10 gtt tid, Bee propolis Homeopathy Prescribe constitutionally Physical Medicine Diathermy to chest (BB,RB) Postural drainage, rest (2) Mustard plaster to chest (BB,5) Color therapy: green light, potentized oil to chest (13) Hydrotherapy: Cold compresses (RC), Revulsive poultices: hot moist to back, cold to front Castor oil poultice Sine wave to spleen, liver, thymus Thoracic adjustment (T9) Colonic--lung reflex Oriental Medicine Acupuncture: LU7, K3,24-27, ST 13-16, BL 42-44, 36-37, LI 3-4, SP21, LV14 (14) Other Bed rest important Postural drainage and percussion -- AM and at bedtime (4)