Pneumonia Case Study: Group Activity
advertisement
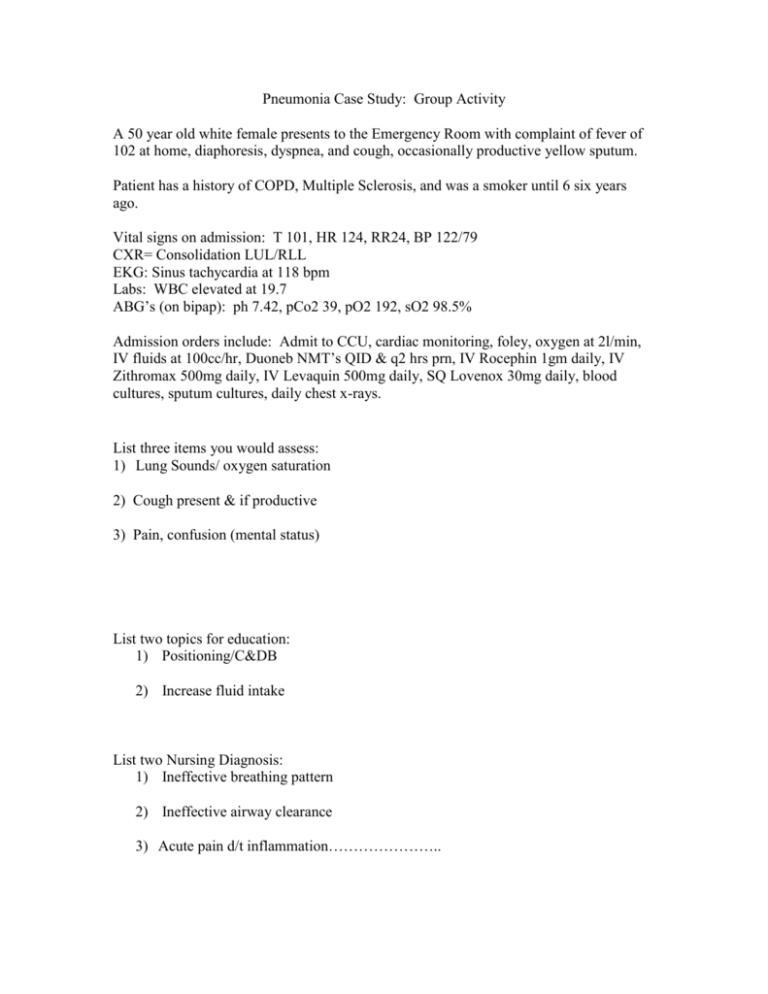
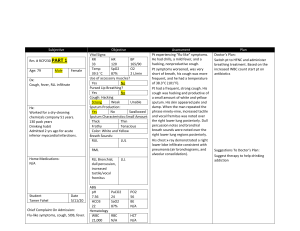
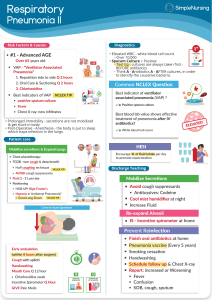
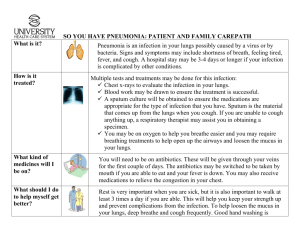
Pneumonia Case Study: Group Activity A 50 year old white female presents to the Emergency Room with complaint of fever of 102 at home, diaphoresis, dyspnea, and cough, occasionally productive yellow sputum. Patient has a history of COPD, Multiple Sclerosis, and was a smoker until 6 six years ago. Vital signs on admission: T 101, HR 124, RR24, BP 122/79 CXR= Consolidation LUL/RLL EKG: Sinus tachycardia at 118 bpm Labs: WBC elevated at 19.7 ABG’s (on bipap): ph 7.42, pCo2 39, pO2 192, sO2 98.5% Admission orders include: Admit to CCU, cardiac monitoring, foley, oxygen at 2l/min, IV fluids at 100cc/hr, Duoneb NMT’s QID & q2 hrs prn, IV Rocephin 1gm daily, IV Zithromax 500mg daily, IV Levaquin 500mg daily, SQ Lovenox 30mg daily, blood cultures, sputum cultures, daily chest x-rays. List three items you would assess: 1) Lung Sounds/ oxygen saturation 2) Cough present & if productive 3) Pain, confusion (mental status) List two topics for education: 1) Positioning/C&DB 2) Increase fluid intake List two Nursing Diagnosis: 1) Ineffective breathing pattern 2) Ineffective airway clearance 3) Acute pain d/t inflammation…………………..