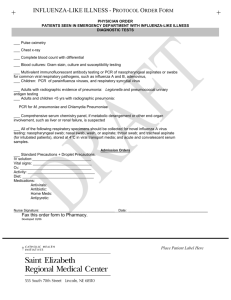
CAP_01 (Diagnostic approach)
advertisement

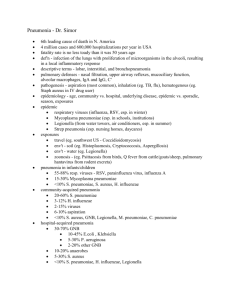
CAP (Diagnostic approach) INTRODUCTION 1. 2. 3. CAP is defined as acute infection of pulmonary parenchyma in patient who has acquired the infection in community, as distinguished from hospital-acquired pneumonia. A third category of pneumonia, designated "healthcare-associated pneumonia," is acquired in other healthcare facilities such as nursing homes, dialysis centers, and outpatient clinics or within 90 days of discharge from acute or chronic care facility. CAP is common and potentially serious illness. It is associated with considerable morbidity and mortality, particularly in older adult patients and those with significant comorbidities. The diagnostic approach to CAP in immunocompetent adults will be reviewed here. A variety of other important issues related to CAP are discussed separately. DISTINGUISHING CAP FROM HCAP 1. In patients presenting with pneumonia from the community, it is important to distinguish CAP from HCAP; because, in some studies, HCAP has been associated with higher risk of multidrug-resistant bacterial pathogens than CAP. CAP is pneumonia that occurs in non-hospitalized patient who has not had extensive healthcare contact. 2. HCAP is defined as pneumonia that occurs in non-hospitalized patient with extensive healthcare contact, as defined by one or more of the following. A. Intravenous therapy, wound care, or intravenous chemotherapy within prior 30 days B. Residence in nursing home or other long-term care facility C. Hospitalization in acute care hospital for two or more days within prior 90 days D. Attendance at hospital or hemodialysis clinic within prior 30 days 3. The management of HCAP is discussed in detail separately. CLINICAL EVALUATION 1. The approach to the patient with CAP begins with clinical evaluation followed by CXR with or without microbiologic testing. A systematic review highlighted lack of sensitivity of clinical criteria for accurate diagnosis of CAP; even combination of symptoms (cough) and signs (fever, tachycardia, and crackle) did not have sensitivity above 50% when using CXR as standard. 2. Common clinical features of CAP include cough, fever, pleuritic chest pain, dyspnea, and sputum production. Mucopurulent sputum production is most frequently found in association with bacterial pneumonia, while scant or watery sputum production is more 3. suggestive of atypical pathogen. Although there are classic descriptions of certain types of sputum production and particular pathogens (pneumococcal pneumonia and rust-colored sputum), these clinical descriptions do not help in clinical decision-making regarding treatment because they are rarely seen. Other common features are GI symptom (nausea, vomiting, diarrhea), and mental status changes. Chest pain occurs in 30% of cases, chills in 40 to 50%, and rigors in 15%. Because of rapid onset of symptoms, most individuals seek medical care within the first few days. 4. On physical examination, approximately 80% are febrile, although this finding is frequently absent in older patients and temperature may be deceptively low in the morning. RR > 24 is noted in 45 to 70% of patients and may be the most sensitive sign in older adult patients; tachycardia is also common. Chest examination reveals audible crackles in most patients, while approximately 33% have evidence of consolidation. However, no clear constellation of symptoms and signs has been found to accurately predict whether or not patient has pneumonia. 5. The major blood test abnormality is leukocytosis (typically between 15,000 and 30,000 per mm3) with leftward shift. Leukopenia can occur and generally connotes poor prognosis. RADIOLOGIC EVALUATION 1. The presence of infiltrate on CXR is considered gold standard for diagnosing pneumonia when 2. 3. 4. clinical and microbiologic features are supportive. CXR should be obtained in patients with suspected pneumonia when possible; demonstrable infiltrate by CXR or other imaging technique is required for diagnosis of pneumonia, according to 2007 consensus guidelines from IDSA/ATS. Recommendations are less clear in patient with what appears to be viral infection with nasal congestion and cough; one approach in these cases is to obtain CXR when there is abnormal vital sign with particular emphasis on RR > 20 or fever. This recommendation is relatively insensitive in older adult patients. The radiographic appearance of CAP may include lobar consolidation (image 1 and image 2), interstitial infiltrate (image 3 and image 4 and image 5), and/or cavitation (image 6). It has been taught that lobar consolidation is due to "typical" bacteria, and interstitial infiltrates are due to Pneumocystis jirovecii (formerly P. carinii) and viruses. However, radiologists cannot reliably differentiate bacterial from nonbacterial pneumonia on basis of radiographic appearance. There is also substantial inter-observer variation in interpretation of CXR in patients with possible pneumonia between different radiologists and between emergency room physicians and radiologists. It is also clear that HRCT is superior to CXR in detecting lesions and defining anatomical changes. Nevertheless, CXR is generally adequate for clinical care of most patients with CAP. If clinical evaluation does not support pneumonia in patient with abnormal CXR, other causes for radiographic abnormalities must be considered, such as malignancy, hemorrhage, pulmonary edema, pulmonary embolism, and inflammation secondary to noninfectious causes. On the other hand, if clinical syndrome favors pneumonia but radiograph is negative, radiograph may represent false-negative result. In some cases, this can be clarified with CT scan, which, as noted above, has higher sensitivity and accuracy than CXR for detecting CAP. There are case reports and animal experiments favoring hypothesis that volume depletion may produce initially negative radiograph, which "blossoms" into infiltrates following rehydration. In support of this hypothesis, one population-based cohort study of suspected CAP found that 7% of patients with negative initial CXR developed changes consistent with CAP on repeat CXR. 5. 6. For hospitalized patients with suspected pneumonia and negative CXR, 2007 IDSA/ATS consensus guidelines consider it reasonable to initiate empiric presumptive antibiotic and repeat CXR in 24 to 48 hours. The basis for this recommendation is from classic studies of pneumococcal pneumonia, which found that absence of infiltrate at 24 hours after onset of symptoms indicated diagnosis needed to be questioned. Alternatively, CT could be performed in patients with negative CXR when there is high clinical suspicion for pneumonia. HRCT is more sensitive than plain films for evaluation of interstitial disease, bilateral disease, cavitation, empyema, and hilar adenopathy. CT is not generally recommended for routine use because data for its use in CAP are limited, the cost is high, and there is no evidence that it improves outcome. Thus, CXR is the preferred method for initial imaging, with CT or MRI reserved for further anatomical definition (detecting cavitation, adenopathy, or mass lesions). DIAGNOSTIC TESTING FOR PATHOGEN 1. There is agreement that treatment is best when it is pathogen directed, but there is little consensus on practicality of achieving this goal due to controversies in value of diagnostic tests. 2. 2007 IDSA/ATS consensus guidelines recommend diagnostic testing for specific organism when, based on clinical or epidemiologic data, pathogens that would not respond to usual empiric antibiotic regimens are suspected. These guidelines otherwise support following testing strategy, based on patient characteristics and severity of illness. A. For outpatients with CAP, routine diagnostic tests are optional. B. C. D. 3. 4. Hospitalized patients with specific indications should have blood cultures and sputum Gram stain and culture and/or other tests as outlined in the following Table (table 1); some experts consider diagnostic tests to be optional for hospitalized patients without severe CAP. Patients with severe CAP requiring ICU admission should have blood cultures, Legionella and pneumococcus urinary antigen tests, and sputum culture (either expectorated or endotracheal aspirate). Newer tests that have been approved by FDA include PCR for detecting C. pneumoniae and M. pneumoniae as well as 14 respiratory tract viruses. These tests are rapid (one to two hours), sensitive, and specific. A guide to utilization of microbiology laboratory for diagnosis of infectious diseases was published in 2013 by IDSA and ASM. This guide includes tables summarizing available tests for the diagnosis of CAP; it can be found at the IDSA website. Critical microbes A. Some microbes are critical to detect because they represent important epidemiologic challenges and/or serious conditions that require treatment different from standard empiric regimens. i. ii. 5. 6. Legionella species Influenza A and B, including avian influenza A H5N1 and avian influenza A H7N9 iii. Middle East respiratory syndrome coronavirus (MERS-CoV) iv. Community-associated methicillin-resistant Staphylococcus aureus (CA-MRSA) v. Agents of bioterrorism vi. Other emerging pathogens Outpatient A. Testing for microbial diagnosis is usually not performed in outpatients because empiric treatment is almost always successful. In one study of over 700 ambulatory patients treated for CAP, empiric antibiotics (macrolide or fluoroquinolone in > 95%) were almost universally effective; only 1% required hospitalization due to failure of outpatient regimen. B. The 2007 IDSA/ATS consensus guidelines suggest that routine tests to identify etiology for CAP are optional for patients who do not require hospitalization. An exception is in clinical or epidemiologic settings suggesting critical microbe is etiologic agent, in which tests for microbial diagnosis are important. Hospitalized patient A. Most hospitalized patients with CAP in the US are treated empirically with no etiologic diagnosis. A review of experience of Medicare for 17,340 patients hospitalized for CAP in 2009 showed microbial diagnosis was made in only 7.6% of cases. Several reasons for this include distancing of laboratory from the site of care; CLIA, ruling that rid hospitals of housestaff labs in 1988; perception that quality of microbiology as applied to sputum Gram stain and culture was variable but generally poor; Medicare Performance Indicator policy that required administration of antibiotics within 6 hours of registration in emergency rooms (requirement that has been discontinued); and RCT showing that medical care outcomes were as good with empiric decisions based on guidelines as they were with pathogen-directed antibiotics. Despite these observations and realities, there is interest in increasing diagnostic microbiologic studies in CAP patients along with increased emphasis on better quality in the traditional tests and use of newer molecular techniques. The emphasis on pathogen-directed treatment is motivated by desire to reduce unnecessary complications (including Clostridium difficile infection), to limit B. antibiotic overuse, to reduce resistance, and to improve care. A prospective study published in 2005 evaluated diagnostic yield of traditional microbiologic tests in 262 hospitalized patients with CAP. Clinical samples included sputum for Gram staining, culture, and detection of pneumococcal antigen; blood for culture and serologic tests; urine for Legionella and pneumococcal antigens; and specimens obtained by bronchoscopy. i. A pathogen was identified in 158 (60%) patients, with Streptococcus pneumoniae identified most commonly, accounting for 97 of 158 (61%) identified pathogens. ii. Adequate sputum samples were obtained in only 44 patients (17%); Gram stain was diagnostic and confirmed by positive sputum culture in 36 of 44 patients (82%). iii. Urinary pneumococcal antigen test was positive in 52 of the 97 (54%) patients with pneumococcal pneumonia. iv. Blood cultures were positive in 40 of 254 (16%) patients. v. Bronchoscopy provided additive diagnostic value in 18 of 37 patients (49%) who did not expectorate sputum and in 14 of 27 patients (52%) who failed treatment within 72 hours after admission. C. There is substantial interest and progress in development of molecular methods to detect multiple pathogens. Potential advantages are speed and enhanced sensitivity and specificity. This technology is now available for detecting 16 viral pathogens, M. pneumoniae, C. pneumoniae, and L. pneumophila. In prospective study of 184 adults with CAP, investigators used comprehensive battery of tests using blood cultures, urinary antigen tests, and respiratory tract specimens for conventional culture plus PCR for respiratory viruses and atypical agents. For S. pneumoniae and H. influenzae, they used quantitative PCR to avoid detection of colonizing flora. A likely pathogen was detected in 78% of cases and in 89% among patients with complete sampling. S. pneumoniae was the most common pathogen (38%), and PCR provided the highest yield for its detection. Respiratory viruses were found in 29% of cases, and many had bacterial superinfection. D. Blood culture i. Pretreatment blood cultures are positive for pathogen in 7 to 16% of hospitalized ii. iii. iv. patients. S. pneumoniae accounts for 66% of positive blood cultures. Blood cultures are commonly advocated in hospitalized patients with CAP. 1. When positive for likely pathogen, microbial diagnosis is established. 2. This is only diagnostic test done, in most cases, and is major source of microbiologic data for CAP for many hospitals. 3. The isolates identified serve as important resource for tracking resistance patterns of S. pneumoniae (CDC surveillance network is highly dependent on blood culture data). These are data used for evaluating efficacy of current S. pneumoniae vaccines and serotypes needed for inclusion in future vaccines. Counter arguments for not obtaining these tests. 1. The blood culture positivity rate is relatively low. 2. There is high rate of false-positive blood cultures (10% in one study). Contaminants may actually prolong hospital stays due to perceived need for vancomycin to treat S. aureus, when laboratory calls to report GPC, which are actually coagulase-negative staphylococci that are not yet identified. 3. Positive cultures rarely lead to modification or narrowing of antibiotic therapy. In one study, variables associated with bacteremia included absence of prior antibiotic, chronic liver disease, pleuritic pain, tachycardia (> 125 bpm), tachypnea (> 30 bpm), and systolic hypotension (< 90 mmHg). v. Some studies have suggested that sicker patients (as judged by PSI) are more likely to have positive blood cultures, although this has not been observed in other reports. 2007 IDSA/ATS consensus guidelines recommend blood cultures for hospitalized patients with specific indications, including all patients who require admission to ICU for CAP, and consider them optional for other patients. E. Sputum i. Expectorated sputum can be submitted for Gram stain and culture, but utility of these tests is subject to substantial controversy due in part to variations in quality of service and distance of clinical microbiology laboratory, apparent success of empiric treatment, and need to initiate antibiotic while in ED or clinic. Thus, rate of pathogen detection varies in studies, some with pathogen detection rate of < 10% and others with yields of 54 to 86%, particularly in patients with bacteremic pneumococcal pneumonia or when invasive procedures were used to obtain samples. A review of Medicare data from 33,000 patients hospitalized for CAP in the US showed that only 7.6% had pathogen detected. ii. 2007 IDSA/ATS consensus guidelines recognize limitations of sputum Gram stain and culture. The guidelines recommend that pretreatment sputum Gram stain and culture of expectorated sputum be performed only if good quality sputum can be obtained, with appropriate measures in place for collection, transport, and processing to assure quality performance. Under these circumstances, expectorated sputum specimens are recommended for hospitalized patients with any of the following criteria. 1. Intensive care unit admission 2. Failure of antibiotic (either outpatients or hospitalized patients), although clinician must be aware that post-treatment specimens are notorious for colonization by resistant bacteria 3. 4. 5. 6. 7. 8. 9. iii. Cavitary lesions, although anaerobic bacteria, the usual cause of primary lung abscess, would require an uncontaminated sputum sample for detection; this requires culture of empyema fluid, a transtracheal aspirate, transthoracic aspirate or (possibly) quantitative bronchoscopic aspirate. Active alcohol abuse Severe obstructive or structural lung disease Immunocompromised host Pleural effusion Epidemic pneumonia Epidemiologic or clinical data suggesting pathogen likely to be resistant to standard therapy, such as GNB or MRSA 10. Epidemiologic or clinical data suggesting pathogen of clinical or epidemiologic interest, such as Legionella, MERS-CoV, SARS, avian influenza A H7N9, or agents of bioterrorism Standards of quality control for sputum culture for bacterial pathogens have been proposed. 1. The specimen should be deep cough specimen obtained prior to antibiotics. 2. Cultures should be performed rapidly after collection, preferably within 2 hours; alternative for rapid plating of sample is to retain specimen at 4ºC if delay is more than two hours. 3. A "good" sputum sample is one with PMN but few (or no) SEC on Gram stain. Several guidelines have been proposed to evaluate quality of sputum samples. These guidelines have proposed different combinations and cutoffs of the minimum number of SEC and/or PMN per LPF, but none of these parameters can be considered to be clearly superior. An example of one approach is to reject all specimens with > 10 SECs/LPF, without considering number of PMNs. It should be noted that these criteria do not apply to cultures for Legionella or mycobacteria. iv. v. vi. vii. viii. ix. The sensitivity and specificity of sputum Gram stain vary substantially in different settings. A meta-analysis evaluated 12 studies of sensitivity and specificity of sputum Gram stain in CAP. The sensitivity of Gram stain compared with culture ranged from 15 to 100% and specificity ranged from 11 to 100%. Culture results should be interpreted based upon the following findings. 1. Quantitation of growth (heavy, moderate, or light) 2. Clinical correlation 3. Correlation with Gram stain True pathogens should be present in moderate or heavy amounts by Gram stain and culture. However, some agents are regarded as significant regardless of concentration, including Legionella spp, Bacillus anthracis, M. tuberculosis, M. pneumoniae, C. pneumoniae, and C. psittaci; these respiratory pathogens are virtually never colonizers but always represent disease. Antibiotics may alter yield of any subsequent culture of respiratory secretions. Specimens collected after antibiotics are given are more likely to grow S. aureus or GNB, which usually represent early airway contaminants. When S. pneumoniae and H. influenzae is etiologic agent, false-negative cultures are common because of their fastidious growth requirements and lack of selective media. By contrast, S. aureus and GNB are relatively rare pulmonary pathogens that are easily grown in respiratory secretions because they are hardy and easily recognized by growth on selective media. The failure to grow these organisms is strong evidence against their presence and, when grown, they often represent contaminants. The preferred tests for Legionella are culture on selective media and urinary antigen assay. A travel history should be obtained in patients presenting with CAP and Legionella testing ordered for patients who have traveled in 2 weeks before symptom onset. The risk of Legionella infection is especially associated with contaminated water in hotels, although outbreaks have occurred in diverse settings including hospitals, cruise ships, and industrial plant. F. Urinary antigen i. Alternative or complementary methods to detect S. pneumoniae and Legionella are ii. urinary antigen assays. There are several advantages and disadvantages to urine antigen testing compared with culture. Advantages 1. Most studies show these urinary antigen tests are more sensitive and specific than Gram stain and culture of sputum as commonly done by most labs. 2. Urine specimens are usually available in 30 to 40% of patients who cannot supply expectorated sputum. 3. Results of urine antigen testing are immediately available. 4. The test retains validity even after initiation of antibiotic therapy. 5. iii. iv. v. vi. The test has high sensitivity compared with blood cultures and sputum studies and high specificity. 6. The urinary antigen tests for Legionella and S. pneumoniae are FDA cleared and provide results in minutes; reagents are commercially available, and they require no equipment. They are not CLIA waived, meaning they must be done by laboratory technician. Disadvantages 1. The sensitivity and specificity may be less in patients without bacteremia. 2. There is no microbial pathogen available for antibiotic sensitivity testing. 3. These tests require licensed technician and cannot be done by provider despite their simplicity. A disadvantage of the urine antigen assay for diagnosis of Legionella is that it is only useful for diagnosis of L. pneumophila group 1 infection. Nevertheless, this serogroup accounts for 80% of Legionnaires' disease acquired in community and in hotels. Nosocomial Legionella infections often involve other serotypes, so sensitivity is decreased. A prospective trial evaluated sensitivity and specificity of pneumococcal urinary antigen test in 107 patients with bacteremic pneumococcal infection compared with 106 patients with septicemia caused by other organisms. Antigen was detected in 88 of 107 pneumococcal bacteremic patients (82%) compared with 3 of 106 patients with bacteremia due to other pathogens (3%), for sensitivity and specificity of 82 and 97%. It is important to note that these findings were in patients with bacteremic pneumococcal pneumonia and may not reflect what occurs in patients without bacteremia. In subsequent prospective study that included 171 adults hospitalized with CAP caused by S. pneumoniae, majority of whom did not have S. pneumoniae isolated from blood cultures, sensitivity of pneumococcal urinary antigen was 71% and specificity was 96%. vii. Among patients with definite diagnosis of pneumococcal CAP, sensitivity of urinary antigen testing was 78% compared with 57% in those with probable diagnosis. A definite diagnosis was defined as S. pneumoniae isolated from blood culture or pleural fluid culture or detected by PCR from pleural fluid, whereas probable diagnosis required S. pneumoniae to be the predominant organism in good quality sputum sample with accompanying positive Gram stain. Pneumococcal CAP was diagnosed exclusively by urinary antigen test in 75 cases (44%). The results of urinary antigen test led clinicians to reduce spectrum of antibiotics in 41 of 474 patients with CAP (9%). This study suggests that, although sensitivity of pneumococcal urinary antigen test is lower in patients who are not bacteremic, the presence of positive urinary antigen test in non-bacteremic patient can be helpful viii. ix. for tailoring therapy. According to 2007 IDSA/ATS consensus guidelines on CAP, pneumococcal urinary antigen assay may augment standard diagnostic methods of blood culture and sputum Gram stain and culture, with potential advantage of rapid results similar to those for sputum Gram stain. It is of particular value when antibiotic has already been initiated, prior to obtaining sputum sample; specimens may remain positive 3 days after antibiotic initiation. A disadvantage compared with culture is inability to test antibiotic sensitivity. The standard tests to diagnose Legionella spp infection in most clinical laboratories are culture on selective media and urinary antigen assay (table 2). G. Polymerase chain reaction i. Like urinary antigen assay, PCR improves accuracy of microbiologic diagnosis for patients with CAP with rapid turnaround time. One limitation of PCR when used on respiratory specimens, including bronchoscopic samples, is that specimens are contaminated by upper airway flora. Thus, quantitative or semiquantitative PCR assay is necessary, and results must be interpreted with understanding that some of pathogens isolated may be colonizers of upper respiratory tract. Another limitation is that these are not point-of-care tests, meaning they require laboratory and laboratory technician. This may present logistical problems in facilities that have outsourced microbiology or have limited coverage H. Viral infection i. Viral pathogens that cause CAP include influenza, adenovirus, parainfluenza, RSV, and human metapneumovirus. The diagnosis can be made by culture, serology, or through rapid diagnostic testing EIA, immunofluorescence, or PCR. PCR-based diagnostic panels have been developed that can detect multiple respiratory viruses simultaneously and can be performed in 2 to 3 hours in hospital laboratories. Using such panel can aid in rapid diagnosis of viral pneumonia, which might reduce unnecessary use of antibacterial agents. Caution is necessary in interpretation since up to 15% of healthy persons harbor respiratory tract virus at any point of time. PROCALCITONIN AND CRP 1. Biologic markers are sometimes used to try to distinguish between bacterial and nonbacterial 2. 3. 4. 5. 6. 7. causes of pneumonia. The two most promising are PCT and CRP. PCT is peptide precursor of calcitonin that is released by parenchymal cells in response to bacterial toxins, leading to elevated serum levels in patients with bacterial infections; in contrast, procalcitonin is down-regulated in patients with viral infections. Procalcitonin is measured by two commercially available tests, Kryptor assay and LUMI assay; the former is preferred due to higher sensitivity. PCT has been studied prospectively to facilitate decision of whether to use antibacterial agents in patients with pneumonia and when antibiotics can be safely stopped. In two trials, clinicians were strongly recommended not to prescribe anti-bacterials in patients with PCT < 0.1 mcg/L but were encouraged to use anti-bacterials in patients with PCT > 0.25 mcg/L. The analysis suggested the correct decision in 83%. Several trials have shown that using PCT results to help determine whether antibiotics are necessary results in lower rates of antibiotic exposure. In Cochrane meta-analysis that used individual patient data from 14 trials of 4221 patients with acute respiratory infections (half of whom had CAP), PCT guidance for antibiotic use was associated with reduction in antibiotic exposure (from median of 8 days to 4 days) without increase in mortality or treatment failure in any clinical setting (outpatient clinic, ED) or in patients with any type of acute respiratory infection, including CAP. Most patients with diagnosis of CAP supported by imaging showing pulmonary infiltrate will be treated with antibiotic, but low PCT may support impression of viral or other nonbacterial cause. PCT may also facilitate decision to stop antibiotics since levels reflect bacterial replication. We consider PCT useful adjunct to antibiotic decisions in CAP, but other observations and clinical judgment are also important. Other studies have shown that PCT correlate with severity of pneumonia. In one small study, PCT increased over time in non-survivors but decreased in survivors. PCT also predict bacteremia. These studies show that PCT help to distinguish between bacterial and viral pneumonia, reduce antibacterial use, predict severity based on magnitude of result, and may predict survival. The use of PCT for distinguishing between bacterial and viral bronchitis is discussed in detail separately. CRP has shown more limited utility, due in part to paucity of studies. One study showed CRP > 40 mg/L had sensitivity and specificity for bacterial pneumonia of 70 and 90%. Another study that included 364 patients with respiratory infection showed sensitivity of 73% and specificity of 65%. Another report indicated particularly high CRP in patients with pneumococcal pneumonia (mean 178 mg/L). CRP appears to be less sensitive than PCT for detection of bacterial pneumonia. Both of these tests need to be interpreted in context of clinical observations. SPECIAL INTEREST 1. The most common etiologic agents of CAP or those that are less common but require more 2. specific therapy are discussed below. The microbial etiology of CAP in studies from different countries is reviewed in Table (table 3) and is discussed in greater detail separately. Streptococcus pneumoniae A. S. pneumoniae historically has accounted for about 65% of bacteremic pneumonia cases, and it continues to be the most common identified pathogen in nearly all studies. B. Nevertheless, clinical studies from the US show infrequent detection of any pathogen in majority of CAP cases, and yield of S. pneumoniae is < 20% of all cases of CAP even with assiduous attempts to detect pathogen. One of the highest yields of S. pneumoniae in recent years was from study from Sweden that used semiquantitative PCR; 70 of 184 C. D. 3. cases of CAP among inpatients (38%) were found to be caused by S. pneumoniae. Note that care must be exercised in cross-country comparisons of rate of detection of S. pneumoniae due to differences in pneumococcal vaccine strategies as well as diagnostic methods. The yield with sputum Gram stain and culture is variable and dependent on quality of sputum processing, experience of the reader, and population studied. Among patients with bacteremic pneumococcal pneumonia, yield with expectorated sputum ranges from ≤ 50 to ≥ 80% in labs with good quality control. Diagnostic ability may be enhanced with the addition of urine antigen test to sputum culture. It is expected that PCR assay for detection of S. pneumoniae from respiratory specimens will be available in near future, but this will probably require quantitation when using specimens contaminated by the oral flora due to the sensitivity of these methods and the frequency of carriage of pneumococci in upper airway. Staphylococcus aureus A. S. aureus is infrequent pulmonary pathogen, but it is important to detect since it is associated with severe disease and is usually resistant to standard antibiotics for CAP. Prior studies emphasized importance of MRSA that are most common in association with influenza. S. aureus continues to be uncommon, but often highly lethal, cause of CAP in patients with influenza. B. S. aureus should be suspected in patients with influenza and bacterial superinfection, especially those with clinical characteristics of staphylococcal toxic shock syndrome. S. aureus should also be suspected in previously healthy young adult or child with rapidly progressive lung infection that is often accompanied by pulmonary necrosis, shock, and neutropenia; these features have been associated with USA 300 strain of S. aureus that causes community-acquired MRSA infection. 4. Influenza A. Influenza is important to recognize because of need for appropriate infection control in B. C. D. 5. 6. hospitalized patients, for public health reporting purposes, and for rapid treatment with antiviral agents. During influenza outbreaks, most patients can be diagnosed on clinical grounds alone. Rapid point-of-care diagnostic tests can be done in ED or office without laboratory technician; these tests show sensitivity of only about 50 to 60%, but specificity is > 95%, so negative result does not rule out influenza. Real-time reverse-transcriptase PCR is the test of choice to diagnose influenza but requires laboratory and laboratory technician. The need to know influenza type depends partly on whether multiple influenza strains with different resistance patterns are circulating. For example, majority of seasonal influenza H1N1 during 2008 to 2009 season were resistant to oseltamivir, but almost all isolates of pandemic H1N1 influenza in 2009 to 2012 were susceptible to Oseltamivir. For severe and sporadic cases of influenza-like illness, there is more urgency to make specific diagnosis due to concern for avian influenza A H5N1, avian influenza A H7N9, or other emerging strains. In such situations, PCR for influenza is appropriate. Reagents to test for novel influenza strains when they first emerge may be available only in public health laboratories; local hospital laboratory supervisors will know specimen referral process. Viral culture takes approximately 2 to 5 days to yield result, is less sensitive than PCR, and is mainly used to track which viruses are circulating during given season. There needs to be caution in attributing pneumonia to respiratory viruses, since about 15% of healthy adults harbor a virus without symptoms. An exception is influenza, which is rarely detected in absence of clinical illness. Middle East respiratory syndrome coronavirus A. MERS-CoV emerged in 2012 to cause severe pneumonia in patients in Saudi Arabia. It has also caused disease in other countries among individuals who traveled to Middle East or who were close contacts of individuals with MERS-CoV infection. Patients with acute respiratory syndrome who have epidemiologic risk factor for MERS-CoV infection should be tested for MERS-CoV infection using real-time reverse-transcriptase PCR of respiratory specimens and other assays (serology). The approach to diagnosis of MERS-CoV is discussed in greater detail separately. Legionella spp A. Legionella is implicated in approximately 2 to 9% of CAP cases, depending on site of care (severity). B. Legionella is important to identify because of potential to cause epidemics (usually in hospitals and hotels). Outbreaks usually reflect contaminated water sources. This pathogen is resistant to all β-lactams and Legionella spp infection has relatively high mortality rate, even with proper treatment. 7. 8. 9. Chlamydia pneumoniae A. The incidence of C. pneumoniae in adults with CAP has varied in different studies from 0 to 20%, although the validity of these data is in question due to problems with diagnostic testing. One problem is use of serologic test in many studies, which lacks both sensitivity and specificity for C. pneumoniae. In addition, positive serologic results may represent either current or past infection. Some authorities feel disease is rarely diagnosed because its occurrence is largely limited to infrequent outbreaks and some consider the only valid tests to be tissue culture or PCR. In 2012, multiplex PCR assay was cleared by FDA for diagnosis of C. pneumoniae using nasopharyngeal sample. Mycoplasma pneumoniae A. Mycoplasma pneumoniae has historically been considered pathogen primarily of children and adolescents, but there are reports of increasingly high rates of infection in adults, especially older adults. Diagnostic methods to detect M. pneumoniae infection include culture (which is rarely available), PCR, and serology with IgM and IgG (the most commonly performed assay). In 2012, multiplex PCR assay was cleared by FDA for diagnosis of M. pneumoniae using nasopharyngeal samples. The difficulty of using serology for diagnosis is serologic response is often delayed so that results may not be available at time of selection of antimicrobial therapy. The other concerns are the difficulty in showing correlation between positive results of standard tests and response to therapy in adults and poor correlation when comparing PCR, serology, and culture. Anaerobic bacteria A. Anaerobic bacteria were well-recognized agents of aspiration pneumonia and lung abscess during period 1970 to 1980 when transtracheal aspiration was common method to obtain uncontaminated specimens that were valid for anaerobic culture. Transtracheal aspiration is no longer performed due to safety concerns. Subsequently, there has been interest in use of quantitative cultures of bronchoscopic aspirates using bronchoalveolar lavage or protected brush catheter. Although this procedure can be done, there is only one published study documenting validity of this approach, and strict quality assurance is critical including the admonition to exclude patients who have received antibiotics, avoid lidocaine with preservative, and expedite processing of cultures due to fastidious nature of these organisms. Anaerobes should be suspected on clinical grounds when there is aspiration, pulmonary cavity in aspiration-prone patient, putrid discharge (sputum or empyema fluid), and/or no likely aerobic pathogen. 10. Bioterrorism agent A. Agents that may be used for bioterrorism and can cause pneumonic syndrome include Bacillus anthracis (inhalational anthrax), Yersinia pestis (pneumonic plague), Francisella tularensis (tularemia), Coxiella burnetii (Q fever), Legionella spp, influenza virus, hantavirus, and ricin (table 4). 11. Emerging infections and zoonoses A. Several pathogens have emerged from animal sources to cause outbreaks of respiratory disease in humans (H1N1 pandemic influenza, H5N1 avian influenza, H7N9 avian influenza, severe acute respiratory syndrome coronavirus, MERS-CoV). Other zoonotic pathogens that can cause respiratory disease in humans include hantaviruses (Sin Nombre virus) and Yersinia pestis; such pathogens should be considered in patients with relevant travel or exposure history. SUMMARY AND RECOMMENDATIONS 1. Clinical features and radiographic changes are usually not helpful in identifying the etiologic pathogen of CAP. 2. The presence of an infiltrate on plain chest radiograph is considered the "gold standard" for 3. 4. 5. 6. 7. diagnosing pneumonia when clinical and microbiologic features are supportive. False-negative chest radiographs are occasionally attributed to an infection very early in the course (< 24 hours), neutropenia, dehydration, and Pneumocystis carinii pneumonia (PCP, but officially renamed Pneumocystis jirovecii pneumonia). The only common cause of a false-negative radiograph is infection with PCP. For PCP, spiral CT are more sensitive. Radiologists cannot reliably differentiate bacterial from nonbacterial pneumonia on the basis of the radiographic appearance. Tests for a microbial diagnosis in outpatients with suspected CAP are optional. Not testing is appropriate in most patients since empiric treatment is usually successful. Indications for performing specific tests in hospitalized patients with CAP are shown in the following Table (table 1). The combination of good sputum specimen for Gram stain and culture plus urinary antigen testing is likely to be most useful for rapid diagnosis of CAP, although diagnostic testing is optional for patients without specific indications. Patients hospitalized in ICU should have pretreatment blood cultures, sputum culture and Gram stain, and urine antigen tests. Multiplex polymerase chain reaction tests are now available for detection of Chlamydia pneumoniae, Mycoplasma pneumoniae, and 14 respiratory viral pathogens. These are rapid, sensitive, specific, and the preferred tests for most of these pathogens. The blood culture positivity rate is relatively low but, when positive for likely pulmonary pathogen, this establishes the microbial diagnosis. There are some pulmonary pathogens that are particularly important to recognize due to their epidemiologic significance and/or their need for treatment strategies that differ from the regimens commonly used by empiric selection. These pathogens include Legionella spp, CA-MRSA, influenza, emerging respiratory viral pathogens such as Middle East respiratory syndrome coronavirus, and agents of bioterrorism.