Histology
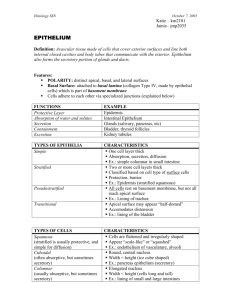
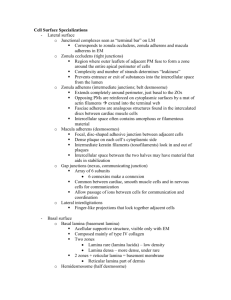
advertisement

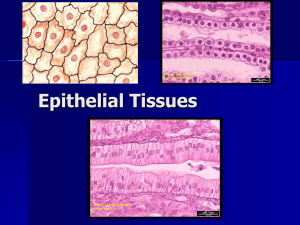
***************************************************** Lab 1-11-99 ************************************************************* From inside the jejunum to outside the layers are: Mucosa is in contact with the lumen. Fingerlike projections from the mucosa into the lumen are called villi. The core of the villus is called the lamina propria ( made of CT) Submucosa extends into the plicae Plicae contain mucosa and submucosa The next layer is the muscularis: 2 regions The outermost layer is the serosa Stains Hematoxolyn – purple nuclei Eosin – pink cytoplasm, muscle fibers, and collagen; pale pink nerve fibers Connective tissue stains: Azan ( esp for pancreas and pituitary ) Masson’s trichrome Mallory’s triple stain: blue CT Red muscle Orange-red RBCs Periodic acid Schiff (PAS) reaction: id’s carbos, rose or purplish red Weigert’s elastic blood stain – dark blue elastic fibers Wright’s stain - blood **************************************************** Lecture 1-13-99 ************************************************** There are 4 basic tissues, all of which are composed of functionally related cells: 1. Epithelial tissue 2. Connective tissue 3. Nervous tissue 4. Muscle tissue Epithelial – means upon. There are 3 types of epithelial tissues 1. Surface epithelium – is arranged in sheets, covers all body surfaces and body cavities, and and organs with free surface. EXCEPTION: there is no surface epithelium in the synovial joints 2. Glandular epithelium – is made of cells that have specific secretory function. It is found in the ducts that carry the secretion 3. Special epithelium – germinal epithelium in the male testes Epithelial origins 1. Endoderm – GI tract lining 2. Mesoderm – muscle tissues, blood vessels 3. Ectoderm – skin General characteristics of epithelial tissues 1. Avascular – nutrients come in from underlying connective tissues by diffusion 2. Contiguous – all cells are attached, all touch 3. Polarized – externally – apical, basal, and lateral Internally – nuclear region 4. Regeneration – constant renewal of cells 5. Metaplasia – if irritated, epithelium can change from one type of epithelium to another. EXAMPLE: in the respiratory tract of a smoker, the epithelium has changed into stratified squamous epithelium ( premalignant condition?) 6. Basement membrane – or basal lamina – all cells rest on one the attaches it to the underlying connective tissue. Functions of epithelial tissues 1. Semipermeable membrane or selective barrier – things have to go through epithelial cells. This can be complete or incomplete. EXAMPLE of complete: brain-blood barrier. 2. Protection – skin 3. Absorption – GI tract Marie Paas Page 1 533579581 03/08/16 4. Secretion – glands – ( useful products ) 5. Excretion – ( waste products ) 6. Transportation – internal mechanism – nutrients ( active function ) External mechanism – respiratory tract moves debris out 7. Conduit – epithelial cells act like a hose ( passive function ) 8. Lubrication – mesothelial cells secrete watery fluid for easy sliding 9. Extension – bladder – transitional 10. Sensation – incoming sensations to taste buds, olefactory 11. ( Contractility – myoepithelial cells ) Usually there is one primary function, but there can be more than one. Classification of epithelial tissues Epithelial cells are arranged in sheets that can be classified by 3 factors: 1. By number of layers a. simple – one layer b. stratified – more than one layer c. pseudostratified 2. According to the shape of the superficial layer of cells. The nucleus often corresponds roughly with cell shape a. squamous – flat, wide, but not tall, fried egg appearance in surface view. Nucleus: flat b. cuboidal – square Nucleus: round c. columnar – rectangular Nucleus: elongated d. transitional We will be asked to identify a vertical section most likely, except for simple squamous. 3. By types Simple squamous epithelium 1. regular 2. endothelial 3. mesothelial Location – Bowman’s capsule, parietal layer, nothing gets through. Loop of Henle. Lungs: alveolar lining Function - selective barrier Location endothelia – entire vascular system: heart, blood vessels, lymphatic vessels Function – selective barrier Location Mesothelia – lining of major body cavities: pleural, pericardial, and peritoneal cavities. Lines the free surface of organs within those cavities. These are membranes that are continually moist. Simple cuboidal tissue Square cells with round, central nuclei Location thyroid follicles salivary gland ducts kidney tubules: proximal, distal, and collecting ovarian surface: outer lining = germinal epithelium ( misnomer ) ducts of exocrine glands Function secretion conduit, absorption, secretion absorption and secretion burial and protection conduit Simple columnar epithelium Basally located, elongated nucleus. Location GI tract: stomach through rectum Gall bladder ( best developed SCE in body!) Kidney- papillary ducts ( final pathway of urine in the kidneys) Fallopian tubes Lining of the uterus Marie Paas Function absorption, some secretion absorption conduit conduit, secretion secretion Page 2 533579581 03/08/16 Pseudostratified Considered a simple epithelium, all cells rest on the basement membrane, but not all cells stretch to the top. It only looks stratified. Contains goblet cells. Usually this tissue is ciliated, but not always. Location Function PCCE: in most of the respiratory tree. Ciliated conduit, secretion, transport Epidydimus – sterocilia – these are not cilia, but long, branching forms of villi absorption Male urogenital tract – vas deferens Stratified squamous epithelium (always identify tissue in lab as keratinized or non-keratinized ) Polygonal – look at the outer cells Keratinized – dead cells are outermost – like in skin – waterproof, upper cells are filled with the protein keratin. Non-keratinized – oral cavity, esophagus, vagina, anal canal, true vocal cords. These are part of a mucus membrane that is continually moist. Stratified cuboidal epithelium Is not very common. Usually 2 layers of cuboidal cells. Lines the ducts of sweat glands, functions in absorption and secretion. In the large salivary ducts it also functions as conduit. Stratified columnar epithelium Usually 2 layers, a basal layer that consists of cuboidal cells and a superficial layer made up of columnar cells. Located in large exocrine glands, palpebral conjunctiva, male and female reproductive tract, tansitional epithelium. Transitional epithelium This is a variety of stratified epithelium with large, dome shaped cells in outermost layer. Some of them are bi-nucleate ( only ones in the body ). This type of tissue can alter its shape. Cells in the bladder are often times 6-8 layers thick, but can thin out to only 3 layers when stretched. Found only in the urinary tract, major and minor calyces, renal pelvis, and the ureters. Surfaces and Surface Specializations of Epithelial Cells Structural specializations reflect specific activities at the various cell surfaces and are an important part of cell polarity. 1. Apical surface -faces lumen (below) 2. Basal surface - attaches to basal lamina 3. Lateral surfaces - intercellular junctions 4. Apical surface specializations ( 1-3 below ) 5. Basal surface specializations 6. Lateral surface specializations ( below ) Apical surface specialization Cilia – are membrane bound. Their function is to beat rhythmically to move substances across surfaces. There are about 250 cilia on each cell, arranged in parallel rows. Cilia are arranged in what is called 9+2 arrangement: (page 44) 1. Cilia a. motile b. most found on pseudostratified variety c. inner structure: 1. microtubules, composed of tubulin 2. 9 pairs of microtubules - 9 cilia doublets (a) microtubule A-with dynein arms (b) microtubule B 3. central pair of microtubules 4. 9+2 arrangement or axoneme d. attached to a basal body e. basal bodies have 9 microtubule triplets f. cilia move to and fro in order to move substances across their surface 2. Microvilli are extensions of plasmalemma on most cells. There are many or few, depending on the absorptive properties of the particular tissue. Each microvillus is part of the cell itself and is covered with plasmalemma. Due to the resulting increase in surface area this also increases absorptive capacity of the cell. Microvilli are shorter than cilia, and they lack the inner structure of cilia. The core of an microvillus consists of actin microfilaments. The basal ends of these microfilaments mix with the microfilaments of the terminal web just underneath the microvilli, so these actin filaments are extensions of the terminal web. The terminal web consists of several types of filaments and is thought to provide the Marie Paas Page 3 533579581 03/08/16 apex of the cell with rigidity. Microvilli can be found in the GI tract as (striated border) or in the PCT of the kidney ( brush border ) – these are light microscopy terms because these structures give a double red line. Microvilli have mostly absorptive function. The glycocalyx is a filamentous coat covering the microvillus. It contains glycoproteins ( PAS +). The complex of microvilli and glycocalyx is easily seen with the light microscope and is called brush border ( or striated border ) More on apical surface than anywhere else. Carbohydrates attach to lipids or proteins of the membrane. The function of this glycocalyx is cellular recognition, it determines what “self” is. EXAMPLE: blood type. Another function is cellular adhesion. 3. Stereocilia These are long, branched microvilli that are found in the epididymis and sensory hair cells of the ear Basal surface specializations 1. basement membrane - basal lamina and reticular lamina, made of type IV and type VII reticular fibers 2. basal lamina a. attachment site of epithelial cells to connective tissue b. lamina densa – always 1 c. lamina rare or lamina lucida – sometimes more than 1 d. components of the basal lamina (1) type of IV collagen (2) heparin sulfate – glycoseaminoglycans/proteoglycans –negatively charged, impedes particles (3) chondroitin sulfate - glycoseaminoglycans –negatively charged, impedes particles (4) laminin – basal protein, acts as glue, adhesive molecules (5) fibronectin – basal protein, acts as glue, adhesive molecules (6) entactin – basal protein, acts as glue, adhesive molecules (7) anchoring filaments – type VII collagen connects the basal lamina to reticular lamina All these components are produced by the epithelial cells. 3. reticular lamina a. not always present b. type III collagen 4. stains for basement membrane a. PAS - stains carbohydrates in proteoglycans b. silver stain - stains type III collagen ( reticular fibers ) and is therefore called argyrophilic Hematoxolyn and Eosin do not show the basement membrane 5. hemidesmosomes – a site of adhesion between 2 epithelial cells 6. basal infoldings can be found in the kidney and in the striated ducts of the salivary ducts. They have elongated mitochondria. Therefore these infoldings indicate the active transport of ions. Lateral surface specializations These are also called intercellular junctions, which serve as sites of adhesion as well as sealing the cell, but they also allow for intercellular communication. The various junctions are usually present in a distinctive order from the apex to the base of the cell. Terminal bar is another light microscope term. The terminal bar can be seen at the apical portion as a dark dot. It represents the junctional complex consisting of the following items (Junctional complex is an electron microscope term) (1) zonula occludens (2) zonula adherens (3) Desomosome or macula adherens 1. Zonula occludens a. most apical point of the cell and also most apical component of the junctional complex b. forms a complete ring around cell c. a pentalaminar structure e. functions as a barrier preventing anything from entering the space between cells, but is not very resistant to stress f. The number of fusion sites has a high correlation with the leakiness of the epithelium. (book page 64) g. gaps are ca. 2nm 2. Zonula adherens a. just below zonula occludens b. forms a complete ring – belt desmosome c. binding proteins in the intercellular space that attaches cells together d. intracellular and extracellular components Marie Paas Page 4 533579581 03/08/16 e. intracellular area contains dense plaques of the following proteins: myosin, tropomyosin, actinin, vinculin f. actin microfilaments from the terminal web enter these plaques g. calcium dependent junction that deteriorates in the absence of Calcium h. provides a firm attachment site for adjacent cells i. gaps are ca. 15-20nm 3. Desmosomes or Macula adherens a. a "spot weld" – spot desmosome b. exceptionally strong attachment site c. lower most and most numerous of the intercellular connections, scattered all over the surface of the cell d. intercellular space contains a dense material - intermediate line (1) desmocollins - linker proteins e. intracellular region contains attachment plaques f. intermediate filaments enter the plaque, these consist of condensation from glycocalyces (1) may from hairpin loops and re-enter the cytoplasm, forming very, very tight connections g. calcium dependent h. gaps are ca. 30nm i. desmosomes are the only type of junction found in the StSE of the skin Gap junctions a. aka nexus b. not part of the junctional complex c. connexons – made of 6 integral membrane proteins in dumbbell structure d. connexons of adjacent cells are in register e. allows communication between cells of molecules less than 1500 Molecular Weight due to pearcing of membranes through hydrophilic channels f. cells are about 2 nm apart Summary of junctions Adhering junctions a. zonula adherens b. desmosomes = macula adherens c. hemidesmosomes Impermeable junctions a. zonula occludens Communicating junctions a. gap junctions GLANDULAR EPITHELIUM Glandular epithelial cells are specialized to perform a secretory function Classification of glandular epithelia 1. Exocrine glands usually release their secretions to a surface usually through a duct system. These external secretions act locally, close to where they were produced. 2. Endocrine glands pass their secretions directly into the blood or lymph. These internal secretions are usually hormones whose targets can be quite a way away. The effects are far-reaching or systemic. Glandular epithelia can be unicellular or multicellular: 1. Unicellular exocrine gland - goblet cell, in the GIT, respiratory tract (PCCE). The mucin they produce protects the linings or traps debris. 2. Unicellular endocrine gland – entero-endocrine cells of the GI tract 3. Mlticellular exocrine gland - salivary glands, pancreas 4. Multicellular endocrine gland – endocrine organs: pituitary, thyroid… Multicellular exocrine gland classification Classification is based on A. Presence or absence of branching in the ducts 1. Simple multicellular exocrine gland - unbranched 2. Compound multicellular exocrine gland - branched B. Based on cellular arrangement of the secretory unit 1. alveolar or acinar - round Marie Paas Page 5 533579581 03/08/16 2. tubular- tube shaped, long and slender 3. tubuloalveolar - mixed Examples: 1. simple tubular - crypts of Lieberkuhn in the colon 2. simple coiled tubular - sweat glands 3. simple branched tubular - fundic glands of the stomach – branching is in the secretory unit and not in duct! 4. simple alveolar - none in humans, poisonous amphibians 5. simple branched alveolar - sebaceous glands in hair follicles in the skin 6. compound tubular - cardiac glands of the stomach 7. compound alveolar - exocrine pancreas 8. tubuloalveolar - salivary glands Types of secretions A. serous – thin secretion, glands secreting this have round nuclei, small lumens B. mucous – thick secretion, glands secreting it have flat nuclei and a larger lumen C. seromucous Methods of secretion ( Compound acinar ) A. holocrine - results in cell death, whole cell is secreted, duct can get clogged causes acne 1. sebaceous and tarsal glands B. apocrine - results in loss of some cytoplasm, point – only top of cell pinches off and secretes 1. mammary gland (lipid) C. merocrine - exocytosis - most glands, no part of the cell is lost Classification: 1. Exocrine 2. Endocrine 3. Unicellular – One cell makes up the substance a. unicellular endocrine – goblet cells – reverse tear drop shaped mucin b. unicellular exocrine – enteroendocrine or cardiac cells of GI tract 4. Multicellular exocrine glands – salivary glands, pancreas a. unbranched ducts – simple b. branched ducts – compound c. rounded or grapelike secretory units – acinar or alveolar d. tube shaped - tubular e. mixed – tubuloalveolar or tubuloacinar EXAMPLES simple tubular – Crypts of Lieberkühn in the colon simple coiled tubular – sweat glands simple branched tubular – fundic glands of stomach - branching not in duct, but secretory unit simple alveolar – none in humans simple branched alveolar – sebaceous glands compound tubular – cardiac glands of the stomach compound alveolar – exocrine pancreas tubuloalveolar – salivary glands 5. Multicellular endocrine glands – thyroid and pituitary Connective tissue Mesenchyme – the mother of all connective tissues, an early embryonic tissue that migrates into developing organs Marie Paas Page 6 533579581 03/08/16 Questions: Zona occludens functions as a barrier preventing anything from entering the space between cells, but is not very resistant to stress PER BOOK: The number of fusion sites has a high correlation with the leakiness of the epithelium. (p 64) From the notes I thought the terminal bar is made up of the junctional complex which in turn is made up of both zonulas and the macula. In the book (p 64) it comes across that the terminal bar is made up of only the zonula occludens and the zonula adherens Marie Paas Page 7 533579581 03/08/16 Mononuclear phagocyte system( MPS ),a widely distributed collection of both free and fixed macrophages derived from bone marrow precursor cells by way of monocytes; their substantial phagocytic activity is mediated by immunoglobulin and the serum complement system. In both connective and lymphoid tissue, they may occur as free and fixed macrophages; in the sinusoids of the liver, as Kupffer cells; in the lung, as alveolar macrophages; and in the nervous system, as microglia. Marie Paas Page 8 533579581 03/08/16