State Health Business Continuity Plan Version 5
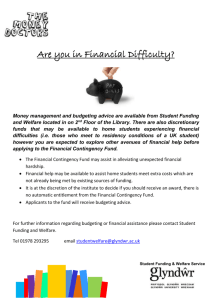
advertisement

State Health Business Continuity Plan Version 5 December 2012 Endorsed by: Date endorsed: Health Services Subcommittee 11 February 2013 State Health Business Continuity Plan Authorisation The State Health Business Continuity Plan has been revised to provide governance arrangements, strategies, operating procedures and key contacts for maintenance of critical business functions. This plan is a supporting document to the individual hospital emergency and disaster plans and is a sub plan to WESTPLAN-Health. This document has been endorsed formally by the following personnel as the standard operating procedure to be followed in the event of such a resource failure or external incident/disaster. Recommended Mr John Heslop Acting Chair Hospital Health Coordinators Group Dated: 19 December 2012 Approved Dr Revle Bangor-Jones Acting Chair Health Services Subcommittee Dated: 11 February 2013 2 State Health Business Continuity Plan Foreword The State Health Business Continuity Plan (formerly the Metropolitan Business Continuity and Disaster Plan) outlines the State response required to ensure that the health emergency management response is coordinated and local resources can be supplemented where necessary. Activation of this plan will occur at the State level by the State Health Coordinator in response to any major failure or disaster that threatens life or health and requires resources beyond local capabilities. This plan is supplemented by local and State level health disaster response plans. These plans all form part of a coordinated health disaster management response under the direction of the State Health Coordinator. The plan highlights the responsibilities and obligations of local health services to provide the initial health response to failures or disasters within their areas and the overall arrangements required to provide the health response in the event of a major failure or disaster. It is important for all health institutions to have plans in place to meet these challenges in recognition of the emergency management principles of prevention, preparedness, response and recovery. Dr Revle Bangor-Jones Acting Director Disaster Management, Regulation and Planning Public Health and Clinical Services Division Department of Health (WA) 3 State Health Business Continuity Plan Amendment Certificate Suggested amendments or additions to the contents of these plans are to be forwarded in writing to: Senior Policy Officer Disaster Preparedness and Management Unit Disaster Management, Regulation and Planning Directorate Public Health and Clinical Services Division Department of Health (WA), 189 Royal Street East Perth, WA 6004 dpmu@health.wa.gov.au All proposed changes to these plans will be subject to recommendation and approval as detailed on page 2 of this plan. Version No. 1.1 Amendment Number Date Entered Signature Date Pages 8, 9 and 12 26 November 1999 26 November 1999 13 December 1999 13 December 1999 1.3 Pages 8, 9, 10, 13, 14, 50, 51 and 54 Page 10 2 Annual Update 15 August 2001 15 August 2001 3 Annual Update 18 October 2002 18 October 2002 4 Complete revision 16 September 2004 16 September 2004 5 Complete revision 19 December 2012 13 February 2013 1.2 22 December 1999 4 State Health Business Continuity Plan Table of Contents Glossary of terms .............................................................................................................................................................. 7 Abbreviations .................................................................................................................................................................... 11 PART ONE - INTRODUCTION ..................................................................................................................................... 13 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 1.10 1.11 1.12 PREAMBLE ............................................................................................................................................................ 13 AIM ....................................................................................................................................................................... 13 PURPOSE OF THE PLAN .......................................................................................................................................... 13 SCOPE .................................................................................................................................................................. 13 OUT OF SCOPE ...................................................................................................................................................... 14 ASSUMPTIONS ....................................................................................................................................................... 14 LEGISLATION AND OTHER STANDARDS ..................................................................................................................... 15 WESTPLAN - HEALTH .......................................................................................................................................... 16 GOVERNANCE ARRANGEMENTS............................................................................................................................... 16 TITLE .................................................................................................................................................................... 16 RELATED PLANS..................................................................................................................................................... 17 AUTHORITY AND PLANNING RESPONSIBILITY ............................................................................................................. 17 PART TWO - Operational Management .................................................................................................................. 18 2.1 2.2 2.3 INTRODUCTION ...................................................................................................................................................... 18 ROLES, RESPONSIBILITIES AND AUTHORITIES ........................................................................................................... 18 MANAGEMENT STRUCTURE ..................................................................................................................................... 21 PART THREE – Business Continuity Management .......................................................................................... 23 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 3.10 3.10.1 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 INTRODUCTION ...................................................................................................................................................... 23 BLOOD AND BLOOD PRODUCTS ............................................................................................................................... 25 CATERING SERVICES ............................................................................................................................................. 28 COMMUNICATION SYSTEMS..................................................................................................................................... 32 ELECTRICITY SUPPLY ............................................................................................................................................. 36 GAS SUPPLY .......................................................................................................................................................... 38 HUMAN RESOURCES .............................................................................................................................................. 40 INFORMATION AND COMMUNICATION TECHNOLOGY ................................................................................................... 42 LINEN SUPPLY ....................................................................................................................................................... 43 MEDICAL GAS SUPPLY ........................................................................................................................................... 46 DESCRIPTION ........................................................................................................................................................ 46 PHARMACEUTICAL SUPPLY AND SERVICES .............................................................................................................. 49 SECURITY SERVICES .............................................................................................................................................. 52 SPECIALIST SERVICES ............................................................................................................................................ 55 SPECIALIST BIOMEDICAL EQUIPMENT ....................................................................................................................... 57 SUPPLY AND LOGISTICAL SERVICES ........................................................................................................................ 61 TRANSPORT SERVICES........................................................................................................................................... 66 WASTE SERVICES .................................................................................................................................................. 70 WATER SERVICES (INCLUDING SEWERAGE) ............................................................................................................. 73 Appendices ......................................................................................................................................................................... 76 APPENDIX 1: PROTOCOLS FOR MANAGING BLOOD AND BLOOD PRODUCTS IN A SURGE OR MASS CASUALTY INCIDENT IN WA. ......... 77 APPENDIX 2: CATERING SERVICES – DEMAND MANAGEMENT STRATEGIES ................................................................................. 78 APPENDIX 3: ELECTRICITY SUPPLY DEMAND MANAGEMENT STRATEGIES..................................................................................... 79 APPENDIX 4: GAS SUPPLY – DEMAND MANAGEMENT STRATEGIES .............................................................................................. 80 APPENDIX 5: LINEN SUPPLY – DEMAND MANAGEMENT STRATEGIES ........................................................................................... 84 APPENDIX 6: WATER SERVICES DEMAND MANAGEMENT STRATEGIES ....................................................................................... 85 APPENDIX 7: CONTAMINATED WATER – DEMAND MANAGEMENT STRATEGIES ............................................................................ 86 5 State Health Business Continuity Plan Distribution List Health Services Subcommittee Secretary Members Hospital Health Coordinators Group Members Advisors Department of Health Director General Disaster Preparedness and Management Unit Library Executive Director, Public Health and Clinical Services Division Director, Disaster Management, Regulation and Planning State Health Incident Coordination Centre Department of Health, On Call Clinical Officers Department of Health, On Call Duty Officers Department of Health, State Health Coordinators All Regional Emergency Operations Centres WA Hospitals All WA Hospitals All Public Hospital Emergency Operation Centres All Private Hospital Emergency Operation Centres Other Health Agencies Royal Flying Doctor Service St John Ambulance Australian Red Cross Blood Service 6 State Health Business Continuity Plan Glossary of terms Business continuity management Business Continuity Management (BCM) is a discipline that prepares an organisation for the unexpected. It is a management process that provides the framework for building resilience to business and service interruption risks, responding in a timely and effective manner to ensure continuity of critical business activities, and ensuring the long tem viability of the organisation following a disruptive event. Business continuity plan A Business Continuity Plan (BCP) is, in effect, a treatment plan for certain risks, the consequences of which could disrupt core functions. The plan outlines the actions to be taken and resources to be used before, during and after a disruptive event to ensure the timely resumption of critical business activities and long term recovery of the organisation. Critical business activity Although there are a wide range of business activities that are provided to internal and external customers, identification of critical business activities allows organisations to identify what businesses are essential. This allows prioritisation of services in the event of a service-level disruption to the organisation’s daily operations. Contingency maximum operating length of time The contingency maximum operating length of time determines how long the contingency or intervention can continue for. In some circumstances, the time may be finite, whereas in other circumstances, the contingency can continue indefinitely. Contingency plans For the purposes of this document, contingency plans refer to plans developed by the nominated person responsible for each of the critical function areas which include actions to be taken in the event of a resource/s failure due to any cause. These plans are developed across the metropolitan area. Demand management strategies Demand management strategies are graduated and phased reductions in service or resource sparing strategies, which are implemented in response to a decrease in supply or surge in demand of available logistical resources. Disaster An event, actual or imminent, which endangers or threatens to endanger life, property or the environment, and which is beyond the resources of a single organisation to manage or which requires the coordination of a number of significant emergency management activities. 7 State Health Business Continuity Plan NOTE: The terms "emergency" and "disaster" are used nationally and internationally to describe events which require special arrangements to manage the situation. "Emergencies" or "disasters" are characterised by the need to deal with the hazard and its impact on the community. The term "emergency" is used on the understanding that it also includes any meaning of the word "disaster". Disaster plans For the purposes of this document, disaster plans refer to plans developed by the nominated person responsible for maintaining up to date plans, which include actions to be taken in the event of a major failure or disaster. Every hospital and health service should have such a plan. Expert / lead advisors Expert advisors are technical experts who are members of the expert panel that has assisted in the compilation of a sub-category of the State Health Business Continuity Plan (SHBCP). They are also key contacts who can be consulted in the event of an impact event or business disruption. Lead advisors are the principle experts in the panel. Health Services Subcommittee The Health Services Subcommittee (HSS) may be convened by the SHC to assist in the provision of a coordinated health response to, and recovery from, the emergency. It is the operational arm of WA Health’s disaster response and includes representation from the different health care providers whom would need to be involved in the response and recovery for the emergency. Hospital health coordinator A Hospital Health Coordinator (HHC) is a person designated by the hospital executive to be the hospital coordinator for the purposes of coordinating the hospital response in an emergency. Each hospital will provide a rostered HHC who is available 24 hours per day for: being the contact position to receive/give the initial notification that the hospital is involved in a major incident/disaster. commencing a notification process to alert other key hospital disaster stakeholders monitoring the overall hospital response to the situation assuming overall command and control of the hospital's general resources and management of its responses during the time the hospital disaster plan is activated, be it for an internal disaster or as a response to an external disaster. Each hospital will have an appropriate system to enable this notification process to be conducted in a timely manner, as per Operational Directive 0164/08. Impact The impact defines what the effect will be if the critical business activity is lost or not available. In strategic terms, many impacts may be defined ambiguously, such as loss of 8 State Health Business Continuity Plan assets or denial of access. The SHBCP will focus upon clinical and business related impacts. Interdependencies Interdependencies are internal and external, processes, resources, functions or organisations that are, directly or indirectly, critical to the continuity of business within an organisation. Maximum Acceptable Outage Maximum Acceptable Outage (MAO) is a measurement concept that enables stakeholders to make an informed decision on how long a particular critical business activity can be disrupted before the consequences become unacceptable. Normal operating mode criteria Normal operating mode criteria are pre-set conditions that must be met before a business can return to normal work practices. In most circumstances, this involves the removal of the trigger or risk. In other circumstances, it may be that certain interventions are enacted in order to allow for the return of normal business activities, such as relocation or restoration of basic utilities. On-Call Clinical Officer The On-Call Clinical Officer (OCCO) (formerly the Hospital Emergency Operations Centre Coordinator [HEOC Coordinator]) is an officer with a clinical background who, on the authority of the State Health Coordinator (SHC), oversees the coordinated use of hospital resources in WA Health. On-Call Duty Officer The On-Call Duty Officer (OCDO) is the single point of entry into WA Health for notifications of all incidents or issues, including communicable diseases, environmental health, hospital service continuity and incident notification. Regional Health Disaster Coordinator A Regional Health Disaster Coordinator (RHDC) is a person designated by the CEO of the WA Country Health Service (WACHS), on recommendation by the Regional Director, to be the Regional Health Coordinator of a designated regional health service in accordance with Operational Circular 1976/05, for the purposes of coordinating the regional health response in a major incident emergency. Relevant stakeholders Relevant Stakeholders are the key contacts or key stakeholders that must be considered in the event that State-level interventions and contingencies are implemented. Relevant stakeholders are critical to the success of the employed contingency. 9 State Health Business Continuity Plan State level strategies State level strategies are high-level plans or interventions that can be implemented in support of local and district level plans in order to minimise the impact of the disruption, and to accelerate the recovery process. State Health Coordinator The State Health Coordinator (SHC) has the authority to command the coordinated use of all health resources within WA Health for response to and recovery from, the impacts and effects of a major emergency or disaster situation. The SHC is responsible for identifying the requirement for Commonwealth and interstate assistance and requesting this through the State Emergency Coordination Group. State Health Incident Coordination Centre This is the State-level health incident control centre that addresses strategic management of an incident/disaster as well as facilitating management of State-wide events. Support organisation This is an organisation whose response in an emergency is either to restore essential services (e.g. Western Power, Water Corporation of WA, Main Roads WA etc) or to provide such support functions as welfare, transport, communications, engineering, etc. Trigger to invoke contingency Triggers to invoke contingency are risks or triggers that have the potential to impact and disrupt critical business activities are identified. 10 State Health Business Continuity Plan Abbreviations ADF AHP AHPC AKHS AMTCG BCM BCP CAHS CEO COO CSSD CUA DEMC DFES DOHA NIR DON DPMU DRP EMWA EOC FESA FHHS FSH HCN HIN HHC HHCG HMA HRT HSS ICT JBC LEMC LOS LTI MAO MCI MERN MOU MRWA NBA NBSCP NMHS NMO - Australian Defence Force Approved Health Providers Australian Health Protection Committee Armadale Kelmscott Health Service Australian Medical Transport Coordination Group Business Continuity Management Business Continuity Plan Child and Adolescent Health Service Chief Executive Officer Chief Operating Officer Central Sterile Supply Department Common Use Agreements District Emergency Management Committee Department of Fire and Emergency Services Department of Health and Ageing – National Incident Room Director of Nursing Disaster Preparedness and Management Unit Disaster Recovery Plans Emergency Management Western Australia Emergency Operations Centre See DFES Fremantle Hospital and Health Service Fiona Stanley Hospital Health Corporate Network Health Information Network Hospital Health Coordinator Hospital Health Coordinators Group Hazard Management Agency Hospital Response Team Health Services Subcommittee Information Communication Technology Jurisdictional Blood Committee Local Emergency Management Committee Length of Stay Lost-time Injury Maximum Acceptable Outage Mass Casualty Incident Metropolitan Emergency Radio Network Memorandum of Understanding Main Roads Western Australia National Blood Authority National Blood Supply Contingency Plan North Metropolitan Health Service Nursing and Midwifery Office 11 State Health Business Continuity Plan OCCO OCDO OCMO OD PABX PMH PSS PSTN PTA RFDS RGH RHDC RPH SCGH SECG SEMC SHBCP SHC SHEF SHICC SJA SKHS SLA SMHS SOP TMU VoIP WA WACHS WATAG WNHS WWC - On-Call Clinical Officer On-Call Duty Officer Office of the Chief Medical Officer Operational Directive Private Automatic Branch eXchange Princess Margaret Hospital Patient Support Services Public Switched Telephone Network Public Transport Authority Royal Flying Doctor Service Rockingham General Hospital Regional Health Disaster Coordinator Royal Perth Hospital Sir Charles Gairdner Hospital State Emergency Coordination Group State Emergency Management Committee State Health Business Continuity Plan State Health Coordinator State Health Executive Forum State Health Incident Coordination Centre St John Ambulance Swan Kalamunda Health Service Service Level Agreement South Metropolitan Health Service Standard Operating Procedure Transfusion Medicine Unit Voice over Internet Protocol Western Australia Western Australian Country Health Service Western Australian Therapeutic Advisory Group Women and Newborn Health Service Working With Children 12 State Health Business Continuity Plan PART ONE - INTRODUCTION 1.1 Preamble The Public Sector Commissioner’s Circular 2009-19 states “all public sector bodies must practice risk management, regularly undertake a structured risk assessment process to identify the risks facing their organisations, be able to demonstrate the management of risks and where appropriate be able to have continuity plans to ensure that they can respond to and recover from any business disruption.” The Western Australian Department of Health (WA Health) requires all hospitals and support services to have in place Business Continuity Plans (BCPs) to ensure continuity of critical business functions in the event of failure or disruption. However, should critical business functions fail and escalate beyond the management capabilities of any individual hospital or support service, or affect multiple hospitals or support services, the State Health Business Continuity Plan (SHBCP) is activated. 1.2 Aim The aim of this SHBCP is to provide governance arrangements, strategies, operating procedures and key contacts for maintenance of critical business functions for WA Health in the event of a major disruption of any cause. 1.3 Purpose of the plan a) To provide the basis for the provision and coordination of the State health response in the event of a denial of access, denial of activities and/or denial of assets, resulting in the critical disruption of health business functions. b) To provide the basis for the provision and coordination of the State health response in the event of a major external disaster causing a disruption to or elevated demand on critical health business functions. c) To provide the State Health Coordinator (SHC) with agreed strategies, operational procedures and contacts based on the expert advice of key stakeholders. d) To provide plans for a number of health service categories. 1.4 Scope Encompasses all of WA Health. Integrates the capabilities of non-public sector services. Is enacted for any health service failure that cannot be managed by local or districtlevel BCPs. Is enacted when a coordinated response is required to manage an external disaster. Identifies thresholds for engagement of Federal resources, but does not outline the 13 State Health Business Continuity Plan nature of that engagement or support of Federal resources. 1.5 Does not identify all potential disruptions or strategies for their resolution. Accordingly, the governance processes outlined are not limited to the categories defined. Out of scope The SHBCP does not supersede WESTPLAN - Health or its sub-plan arrangements, WA Health Operational Directives or existing local health care facility and hospital BCPs. 1.6 Assumptions 1.6.1 Assumptions applying to the State Health Business Continuity Plan The following assumptions have been made in regards to activating the SHBCP: Any major loss of hospital and/or health service global resources (e.g. power, fuel, gas, water, communications, etc), which cannot be dealt with at a local or district (regional) level, will be addressed by the SHBCP. The plan can be activated in response to an incident that affects single and multiple sites. Information technology recovery plans are addressed separately as a part of the Health Information Network (HIN) BCP and Disaster Recovery Plans. The event is specific to the critical infrastructure operations of State-wide health services. The contingencies detailed in this SHBCP must be cost-justified to be considered for inclusion. For the contingency maximum operating time to be accurate, the relevant plans are fully effective. The SHBCP has been developed as a supporting document to individual hospital BCPs, emergency and disaster plans and as a sub plan to WESTPLAN - Health. 1.6.2 Assumptions applying to hospitals and health care services All hospitals shall develop and document a service continuity plan. The plan shall be tested and reviewed at the appropriate intervals The plan shall include intended actions for all foreseeable disruptions to the continuity of services provided by the hospital: For which planning is possible. Prioritised first by the impact of the disruption on service delivery (most severe being the highest priority). 14 State Health Business Continuity Plan The plan integrates with the plans of other health service plans and with the SHBCP, the result being a whole of health service continuity initiative. The plan shall identify the extent of the hospital’s intended actions for each foreseeable disruption. The extent of the hospital’s intended actions is to be determined in consultation with the Disaster Preparedness and Management Unit (DPMU) prior to finalisation of the plan. Where the hospital’s service continuity capabilities are insufficient to manage the disruption, the hospital shall contact the DPMU or SHICC with a request for assistance. Granting of a request for assistance results in the activation of the SHBCP by the DPMU or SHICC. Responsibility for management of the response to the disruption at the site remains with the hospital (and health service). The role of the DPMU is to assist with the response as requested. A high level of resilience is expected of the hospital. All evacuations resulting in internal transfer only shall be managed by the hospital. All evacuations resulting in inter-hospital transfer shall be facilitated by the SHICC. The OCDO shall be immediately notified of all disruptions that could foreseeably require the activation of the SHBCP. All health services are responsible for ensuring that their staff are familiar with these plans. It is acknowledged that not all problems can have contingencies or plans developed and that the management of any incident will be situation specific at the time it occurs. The SHICC shall coordinate application of the SHBCP across multiple hospitals as required. The DPMU shall develop Memorandums of Understanding (MOU) with agencies and service providers for major critical services (e.g. water and power). In the event of a major incident, the principles of WESTPLAN – Health will apply. 1.7 Legislation and other standards Public sector bodies must submit details of their risk management policy assessment processes and continuity plans to Risk Cover in accordance with a schedule that will be provided by the Public Sector Commissioner’s Circular 2009-19 Risk management and Business Continuity Planning. 15 State Health Business Continuity Plan Other standards and guidelines apply to business continuity planning, including: Business Continuity Management Guidelines, 2nd Edition (2009) RiskCover, Western Australian Government. Australian / New Zealand Business Continuity Management HB 221-2004. International Risk Management Standard ISO 31000: 2009. Australian Council on Health Standards EQuIP 5 Standards and Guidelines, Support Function Standard 2.1 & Corporate Function Standard 3.2 Standards Australia, AS/NZS HB 292-2006, A Practitioners Guide to Business Continuity Management. Standards Australia, AS/NZS HB 221-2004, Business Continuity Management Standards Australia, AS/NZS HB 293-2006, Executive Guide to Business Continuity Management. Standards Australia, AS/NZS 5050: 2010, Business continuity – Managing disruption-related risk. Standard Australia AS/NZS 31000: 2009 Risk Management Principles and Guidelines. WA Health, Redundancy and Disaster Planning in Health’s Capital Works Programs (2nd Ed) – January 2012. 1.8 WESTPLAN - Health In the event of a major incident, the principles of WESTPLAN - Health will apply. This is to ensure the greatest good is done for the greatest number and management of the incident is graduated from local to district to State level as required. 1.9 Governance arrangements WA Health is the single agency responsible for coordination of the State-wide health emergency management response. The activation of the SHBCP can only be authorised by the SHC. Activation of this plan is facilitated by the OCCO in the DPMU. Individual hospitals, health services are responsible for maintaining their individual disaster plans and ensuring that they are congruent with the SHBCP. They are also responsible for ensuring that there is a contact person (i.e. a HHC) available 24 hours per day should the SHC require their assistance. 1.10 Title The plan shall be titled the ‘State Health Business Continuity Plan’. 16 State Health Business Continuity Plan 1.11 Related plans This plan may be activated in support of existing WESTPLANs and related agency and health plans. Related plans include: WESTPLAN – Epidemic WESTPLAN – Heatwave WESTPLAN – Gas Supply Disruption WESTPLAN – Liquid Fuel Supply Disruption WA Disaster Hospital Response Team subplan (2012) Western Australia Burns Disaster subplan WA Health Metropolitan Surge Plan (2010) Metropolitan Business Continuity Plan for Blood and Blood Products (SOP-180) National Blood Supply Contingency Plan Health Information Network (HIN) BCP and Disaster Recovery Plans Regional / district health disaster plans (however titled) Individual hospital disaster plans (however titled) NurseWest Business Continuity Plan (2011) Overseas Mass Casualty Plan (OSMASCASPLAN) Western Australia Disaster Hospital Response Team Sub-plan Domestic Response Plan for Mass Casualty Incident of National Consequence (AUSTRAUMAPLAN) and Annex A - Australian Mass Casualty Burn Disaster (AUSBURNPLAN) (2011). Hospital and Health Facility Surge Sub-plans Local hospital and health facility BCPs. 1.12 Authority and planning responsibility The development, implementation and revision of the SHBCP are the responsibility of the SHC in consultation with WA Health and the Hospital Health Coordinators Subcommittee (HHCG). 17 State Health Business Continuity Plan PART TWO - Operational Management 2.1 Introduction Emergency management requires a structure to coordinate all actions required to manage incidents or disasters. This section outlines the roles and responsibilities of those persons implementing the SHBCP All utility failures or service outages will, in the first instance, be managed within the individual hospital as per the hospital disaster plans (however titled). This is in accordance with the principle of gradual escalation from local to district to State level as required at the time. Escalation of response to the SHBCP may occur: If the utility, systems failure or number of casualties is beyond the capabilities of the local hospital management. If there are two or more hospitals disaster plans (however titled) activated at any one time. In the development of a worsening situation. When it is necessary to coordinate resources across hospitals. When WESTPLAN-Health is activated. Escalation of response to State level will occur if the systems failure or number of casualties is deemed beyond the capabilities of the metropolitan or regional management effort. 2.2 Roles, responsibilities and authorities Emergency management requires a structure to coordinate all actions needed to deal with incidents or disasters. This section outlines the roles and responsibilities of those persons implementing the SHBCP. 2.2.1. State Health Coordinator The SHC is the Director General of the WA Health. This responsibility has been formally delegated to the Director, Disaster Management, Regulation and Planning, who will undertake the role of the SHC in a major event or disaster. He/she has the authority to command the coordinated use of all health resources within Western Australia for response to, and recovery from, the impact and effects of a major emergency. The responsibilities of the SHC are to: Authorise the activation of the SHBCP, if required. Authorise the activation of expert advisers as appropriate. Determine when normal operations may be resumed and to manage the recovery phase. 18 State Health Business Continuity Plan 2.2.2. State Health Incident Coordination Centre This is the State-level health operations and coordination centre that addresses strategic management of an incident/disaster as well as facilitating management of State-wide events. The responsibilities of the SHICC are to: Monitor potential or developing emergencies in Western Australia and other states and territories. Advise stakeholders of changes to readiness phase of WA health emergency management plans. Provide appropriate information to other State and Commonwealth departments/authorities/agencies on emergency situations and SHICC operations. Process requests for State health physical and/or technical assistance. Coordinate provision of that assistance. Develop intelligence and strategic planning capability. Provide information on SHICC operations to the SHC and Public Relations representative as required. Maintain records of all SHICC operations and activities. 2.2.3. On-Call Duty Officer The OCDO is the single point of entry for any event affecting WA Health. In the event of an actual or potential incident, the OCDO is responsible for: Receiving the initial notification of an actual or potential incident. Notifying the OCCO of any actual or potential incident affecting hospitals, including those that require clinical input. Assisting the OCCO and SHC with the activation of the SHBCP. The OCDO can be paged on (08) 9328 0553. 2.2.4. On-Call Clinical Officer The OCCO works under the direction of the SHC and is responsible for activating and managing the SHBCP once activation is authorised by the SHC. The responsibilities of the OCCO, under the SHC’s direction are: Planning and coordinating the operational control of all resources required to resolve resource and equipment failures detailed in the SHBCP. Activation of the SHBCP. Activation of expert advisors. Providing regular update reports to the SHC. 19 State Health Business Continuity Plan Liaison with the SHC, expert advisers and OCDO. Maintenance of the SHBCP. 2.2.5. Regional Health Disaster Coordinators The RHDC has an operational role in rural/remote areas and is responsible to the SHC. The RHDC(s) responsibilities are to: Notify the SHC, Regional Director, Chief Operating Officer (COO) and Chief Executive Officer (CEO) of the Western Australian Country Health Services (WACHS) of emergency management and/or business continuity plan activation. Represent the health district at District Emergency Management Committees (DEMC). 2.2.6. State Health BCP expert advisors The State Health BCP Expert Advisors are responsible for; The development and maintenance of the individual contingency or disaster response plans in their area of expertise, such as catering or treatment of multiple chemical casualties. Providing advice and support to the SHC and OCCO in times of the SHBCP activation. Representing the State in their area of specialty at relevant contingency or disaster meetings. Other duties, as requested. 2.2.7. Hospital Health Coordinators HHCs are responsible to the SHC (metropolitan area) or RHDCs (regional areas) during a MCI for: Provision of the hospital’s available resources. Assuming overall command and control of the hospitals' general resources and management of its responses. Determining when it is appropriate to return to normal operations within the hospital and managing the recovery phase. Representing the hospital at Local Emergency Management Committee (LEMC) meetings. Maintenance of the hospital disaster plan (however titled). Other duties, as requested. 20 State Health Business Continuity Plan 2.3 Management structure 2.3.1. Control, coordination and communication WA Health is the single agency responsible for coordination of the State-wide health emergency management response. The SHBCP activation will be authorised by the SHC. Individual hospitals and/or health services are responsible for maintaining their individual disaster plans and ensuring that they are congruent with the SHBCP. They are also responsible for ensuring that there is a contact person available 24 hours per day should the SHC require their assistance. 2.3.2. State activation procedures The activation procedures detailed hereunder relate to the State arrangements. The first indication that the SHBCP may need to be activated may come from a number of sources as follows: One of the HHCs may identify the need to activate this plan to help manage a local emergency. The SHC may identify the need to activate this plan based on information provided from other sources, such as the trauma advice 1800 631 798 number, the State Burn Service Director, State Director of Trauma, Royal Flying Doctor Service (RFDS) or St John Ambulance. The SHC may activate this plan to respond to a regional, national or international emergency. Regardless of who first identifies the need, the SHC shall confer and agree that the SHBCP should be activated. Once this decision is made, the SHC and OCCO shall activate and manage the SHBCP accordingly. 2.3.3. Stages of activation The SHBCP will normally be activated in stages. In an impact event, these stages may be condensed with stages being activated concurrently. Stage 1 – Alert - The alert stage is activated when advice of an impending emergency or failure is received or, when following the occurrence of an event, it is unclear as to whether a State response is required. During this stage, the situation is monitored to determine the likelihood and nature of WA Health’s response. Stage 2 – Standby – The standby stage is activated when information received is sufficient to warrant preparatory activities in readiness for a response. Stage 3 – Response - The response stage is activated when a WA Health emergency response is required and resources are deployed accordingly. Stage 4 – Stand Down - The stand down stage is activated when a response is no longer required. Recovery activities are undertaken. 21 State Health Business Continuity Plan 2.3.4. Operational Debriefing The SHC will ensure the operational debriefing of all participating agencies within a reasonable time frame following stand down and will participate in any general debrief conducted by the Hazard Management Agency (HMA), if separate from WA Health. 2.3.5. Reports The SHICC Coordinator will arrange for the provision of a report relating to the utility, system failure or disaster response to the SHC, the HMA, and the HHCG sub-committee. The report is to identify any problems or shortfalls relating to the provision of health emergency management support and any amendment that may be required to the SHBCP. 2.3.6. Contact details A listing of key positions and their contact details are given in PART 3. 2.3.7. State coordination procedures The overall coordination of the WA Health emergency response to a major disaster will be through the activation of WESTPLAN - Health, which will be managed from the SHICC. 2.3.8. Hospital management Hospital management, from an emergency management context, relates to hospitals being prepared for the impact of emergencies. Hospitals are required to plan for internal and external emergencies on an individual basis. They are also required to ensure that their local plans integrate with the regional and State plans in order that a cohesive response can be mounted should activation of the SHBCP be required. These plans should make provision for: Contingency plans in the event of an internal system or utility failure. Acting as a receiving hospital for casualties transferred from a disaster site. Receiving patients transferred from other hospitals where bed space is required or when a hospital is unable to maintain their business operations. 2.3.9. Health Assistance to or from Interstate, Federal or Overseas Agencies Where the WA health emergency management services are unable to cope with the magnitude and nature of health services required, the SHC may request, through the Executive Officer, SEMC, for Federal, interstate or overseas assistance from Australian Emergency Management. 22 State Health Business Continuity Plan PART THREE – Business Continuity Management 3.1 Introduction Under the current reiteration of the SHBCP, 17 identified sub-categories of core business activities have been identified, including: 1. Blood and blood product services 2. Catering services 3. Communication systems 4. Electricity supply 5. Gas supply 6. Human resources 7. Information and communication technology 8. Linen supply 9. Medical gas supply 10. Pharmaceutical services and supply 11. Security services 12. Specialist services 13. Specialist biomedical equipment 14. Supply and logistics services 15. Transport services 16. Waste services 17. Water services (including sewerage) 23 State Health Business Continuity Plan Impact rating definitions Impact ratings have been included to describe the severity of the service disruption based on both business and clinical outcomes. The identification of the disruption impact rating allows for the prioritisation of contingency to occur. Disruption Impact Table Indeterminate prolonged suspension of work. Impact non Business 5 manageable. Non-performance. Other providers appointed. Catastrophic Clinical Probable death, permanent disability Prolonged suspension of work. Additional resources, Business budget, management assistance required. Performance criteria compromised 4 Major Probable increased level of care / extended length of stay Clinical (> 7 days). Significant complication and/or significant permanent disability Medium-term temporary suspension of work. Backlog Business 3 requires extended work or overtime or additional resources to clear. Manageable impact. Moderate Probable increased level of care / length of stay (3-7 Clinical days). Significant complication / permanent disability. Loss Time Injury 1 week – 1 month. Business 2 Short-term temporary suspension of work. Backlog cleared in a day. No public impact. Minor Minimal increased level of care with increased length of Clinical stay up to 72 hours. Loss Time Injury < 1 week. No disability. Business 1 No measureable impact to the business. No material disruption to work. Insignificant Clinical No increased level of care or length of stay. First Aid only required. (This table has been adapted from Office of Safety and Quality, 2009, ‘Integrated Clinical and Corporate Risk Analysis Tables and Evaluation Criteria (2009)’, Department of Health, Government of Western Australia.) 24 State Health Business Continuity Plan 3.2 Blood and blood products 3.2.1 Description The supply and distribution of blood and blood products is contracted to suppliers and coordinated nationally by the National Blood Authority (NBA), in collaboration with the Jurisdictional Blood Committee (JBC). Extensive risk assessment and business continuity planning has occurred at the national level that has identified three main risks to the supply of demand of blood and blood products: 1. Supply failure, due to decreased stock levels, distribution issue or manufacturing error. 2. Demand surge, due to unforeseen incident or disaster. 3. Public health risk, arising from the product itself, which leads to transfusion related illness (es). 3.2.2 Prevention and mitigation strategies Local hospital emergency blood management plans 3.2.3 Existing Plans The NBA National Blood Supply Contingency Plan (NBSCP) coordinates the supply and redistribution of blood and blood products in a supply crisis. This plan outlines local, State and national strategies in coordinating existing blood stock and redistributing to affected areas. The Metropolitan Business Continuity Plan for Blood and Blood Products (SOP-180) details arrangements in response to a supply or stock issue in Metropolitan Perth. This controlled document is owned and maintained by the PathWest Laboratory Medicine Transfusion Medicine Laboratory Group. 3.2.4 Key stakeholders The NBA is the Australian Government statutory agency legislated to improve and enhance the management of blood and blood products at the national level. The NBA is responsible for maintaining and activating the NBSCP. The JBC is the lynch-pin between governments and the NBA pertaining to issues surrounding national blood supplies. The JBC representative for WA Health is from the Office of the Chief Medical Officer (OCMO). The JBC representative also liaises with clinical stakeholders to ensure congruency in clinical policy with State and national guidelines. 3.2.5 Ordering of blood and blood products by health providers in a surge or mass casualty incident in Western Australia. In the event of a Mass Casualty Incident (MCI) in WA, where there is an increase in the demand for blood out side of normal operational requirements, centralised coordination of available blood and blood products is necessary. Central coordination allows available blood resources to be directed to the most appropriate Transfusion Medicine Units (TMU) based on the allocation of casualties and minimises the likelihood of wastage or misallocation. 25 State Health Business Continuity Plan Protocols for the management of blood in a MCI have been developed in consultation with the Australian Red Cross Blood Service (Blood Service) (see Appendix 1). Note: Where there are issues with the ability of the Blood Service to supply the demand, the Blood Service’s National Executive will liaise directly with the National Blood Authority only. The Blood Service is unable to direct transfer of product between Health Providers due to regulatory restrictions. 3.2.6 Key contacts and expert advisors Title Organisation Position Landline Senior Medical Advisor OCMO Expert Advisor (08) 9222 2066 Senior Policy Officer - Blood OCMO Expert Advisor (08) 9222 2342 Transfusion Medicine Specialist Blood Service Expert Advisor (08) 9421 2301 Medical Scientist in Charge, Transfusion Medicine PathWest - RPH Expert Advisor (08) 9224 2044 Medical Scientist in Charge, Transfusion Medicine PathWest- KEMH Expert Advisor (08) 9340 2761 Acting Operations Manager PathWest -FHHS Expert Advisor (08) 9431 2460 Clinical Nurse Consultant - Patient Blood Management FHHS Expert Advisor (08) 9431 2211 Medical Scientist In Charge Transfusion Medicine Pathwest - QEII Expert Advisor (08) 9346 2783 Production and Laboratory Services Manager Blood Service Expert Advisor (08) 9421 2322 Medical Scientist In Charge Haematology PathWest - PMH Expert Advisor (08) 9340 8801 Director Regional & Support Services PathWest Expert Advisor (08) 9346 7230 Clinical Director, Haematology PathWest Expert Advisor (08) 9346 2554 Consultant Haematologist KEMH Expert Advisor (08) 9340 2222 26 State Health Business Continuity Plan 3.2.7 Blood and Blood Products Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Liaise with Blood Service about priority restoration of supply. 3.2.7.1 Clinical utilisation of available blood and blood product stocks from local inventory Indeterminate Loss of local bulk supply of blood and blood product stocks or MCI Inability to supply sufficient blood and blood products based on clinical demand. 4 Dependant upon blood product involved and nature of disruption. Liaise with PathWest Laboratory Medicine Transfusion Medicine Laboratory Group regarding activation of SOP 180 metropolitan BCP for blood and blood products. Consult with JBC delegate regarding the appropriate liaison with National Blood Authority Blood Service PathWest Laboratory Medicine Transfusion Medicine Laboratory Group Local Jurisdictional Blood Committee Delegate Reestablishment of local bulk supply of blood and blood products Indeterminate Dependant upon blood product involved and nature of disruption. On Call Clinical Officer or SHICC Operations Cell Coordinator 27 and / or Activation of National Blood Supply Contingency Plan State Health Business Continuity Plan 3.3 3.3.1 Catering Services Introduction This plan covers to loss of catering services or arrangements and is enacted when local BCPs fail, due to problems with the facility providers and/or when State-level intervention is required. In metropolitan Perth, catering is predominantly prepared by contractors off-site and transported to sites where meals are heated or cooled in kitchens prior to serving. In regional areas, meals are predominantly prepared on-site from fresh produce. Catering managers are responsible for staffing and rostering, bulk ordering of food stuffs, groceries and clinical nutrition supplies, and ensuring that food safety standards are maintained. 3.3.2 Critical business activities 1. The delivery of catering services through: a. Provision of meals to persons in care, staff members, emergency services, visitors, volunteers, hostels and/or lodge staff. b. Procurement, supply and warehousing of catering supplies. c. Maintenance of food safety standards. d. Ordering and storage of clinical nutrition supplies. 3.3.3 Prevention and mitigation strategies Local site BCPs Adequate forecasting and food redundancy 3.3.4 3.3.5 Interdependencies Power Supply Water Supply Gas Supply Warehousing Contractual fulfilment by obligated service providers Human resources and credentialing Key contacts and expert advisors Name Organisation Position Landline Manager, Patient Support Services FHHS Co-lead Advisor 08 9431 2857 Manager, Patient Support Services SCGH Co-lead Advisor 08 9346 3180 Manager, Catering (Retail) SCGH Expert Advisor 08 9346 4521 Catering Manager FHHS Expert Advisor 08 9431 2909 Manager, Patient Support Services RGH Expert Advisor 08 9599 4600 Manager, Support Services PMH Expert Advisor 08 9340 8532 Catering Manager (Patient Meals) SCGH Expert Advisor 08 9346 4521 Manager, General Services RPH Expert Advisor 08 9224 3033 Catering Manager (Patient Meals) RPH Expert Advisor 08 9224 2015 Scientific Officer (Food Unit) Environmental Health Expert Advisor 08 9388 4923 28 State Health Business Continuity Plan 3.3.6 Catering Services BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or Resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices 1 week Restoration of power to affected health care facilities Indefinitely Access restored to health care facilities 1 week Staffing issues resolved or minimal staffing requirement achieved Local health asset contingency plans 3.3.6.1 Provision of food to patients, staff members and visitors and the storage of clinical nutrition supplies Organise portable refrigeration units Ability to process, store, cook and reheat food. Power Failure Inability to maintain food safety through cold storage and heating. 4 4 hours 6 Liaise with Environmental Health to ensure food safety 1,2 Liaise with volunteer organisations to assist in delivery of meals via stairwells 3 Inability to locally transport meals (lifts) BCP Expert Advisors Portable refrigeration unit suppliers Volunteer organisations Environmental Health Director WA Health Organise portable generator sets to power refrigeration units 3.3.6.2 Provision of food to patients, staff members and visitors Inability to access hospital site (e.g.: industrial action, road block, transportation issues) Unable to deliver meals or bulk food stuffs 5 24 hours - 1 week (depending on use and stock of bulk foods) Liaise with WA Police / DFES to ensure passage of food stuffs WA Police / DFES Food suppliers Utilise alternative transport arrangements Enlist volunteers / agency staff to assist with the production and delivery of meals 3, 7 HCN Nursing Agencies EMWA 3.3.6.3 Provision of food and clinical nutritional supplies to patients, staff members and visitors Staff shortage (kitchen and delivery) Unable to resource food production and delivery 4 24 hours Liaise with HCN and workforce to enlist or employ supplementary staff HCN Volunteer organisations Liaise with Environmental Health Directorate to ensure that all enlisted volunteers have undertaken the necessary food safety training Environmental Health Director WA Health 29 State Health Business Continuity Plan 3.3.6 Catering Services BCP Number 3.3.6.4 CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Identify and Coordinate Alternative Bulk Food Suppliers 4 BCP Expert Advisors Indefinitely Supply of bulk food supplies restored 5 - 7 days Alternative kitchen facility commissioned or restoration of existing kitchen facility Procurement, supply, and provision of food and clinical nutritional supplies to patients, staff members and visitors 1 - 5 days Food Supply Shortages Unable to procure food supplies 3 (dependant upon site's food storage capacity) Implement graduated demand management strategies (see appendix 2) Organise portable/alternative refrigeration and ovens 3.3.6.5 Provision, preparation and storage of food and clinical nutritional supplies to patients, staff members and visitors Utilise alternative kitchen facility Loss of individual kitchen facility due to infrastructure damage (e.g.: fire, flood) Inability to store and heat food stores and maintain food safety 6 4 Organise alternative menus HCN HHCs BCP Expert Advisors Contractors for hiring of bulk Refrigeration and ovens. Immediately Utilise disposable cutlery and crockery Seek Environmental Health to assist and advise on alternative kitchen arrangements Bulk food suppliers Environmental Health Director WA Health Liaise with Environmental Health Directorate 3.3.6.6 Provision, preparation and storage of food and clinical nutritional supplies to patients, staff members and visitors Loss of health facility potable water supply through infrastructure failure or contamination Inability to prepare food, maintain food safety, and infection control standards 5. Inability to dish wash tray ware 3 Immediately Advise health assets to boil water before consumption Advise health assets to utilise processed food only Indeterminate Environmental Health Director WA Health Depends upon location of health facility and nature of incident Restoration of clean potable water supply to health care asset Utilise disposable cutlery 30 State Health Business Continuity Plan 3.3.7 Notes 1. Environmental Health liaison is required to ensure safety of food stuffs is maintained. The Environmental Health Directorate plays both an advisory and watchdog role in ensuring that catering arrangements meet legislative requirements. 2. Environmental Health is only concerned about food delivery to patients. Retail catering in hospitals is regulated by local government environmental health agencies. 3. All volunteers and supplementary staff involved in food handling are required to undergo mandatory training for production and delivery of food. 4. WA Health would still need to comply with government policy and current CUAs 5. In extraordinary circumstances, the SHC may suspend adherence to some aspects of the Food Act (2008). Advice must be sort from the Environmental Health Directorate before this action is implemented. 6. After 4 hours, food cannot be used and alternative sources would be required. This may increase the impact to 5 (catastrophic). 7. Refer to Human Resources section. 31 State Health Business Continuity Plan 3.4 Communication systems 3.4.1 Description Communication is vital to the conduct of business at health care facilities. It is used for both routine and emergency correspondence and can be utilised through various platforms. Communication systems have many interdependencies, such as power supply, and information technology infrastructure. This plan covers the loss of communication platforms that cannot be managed at the local level. 3.4.2 Critical business activities 1. Continuity of communication systems through: a. Internal and external telephone communication systems (e.g. PABX, VoIP). b. Internal and external paging systems. c. Mobile telephone networks. a. Metropolitan Emergency Radio Network (MERN). b. Health voice network (DOHnet / tie lines). 3.4.3 Prevention and mitigation strategies Local site BCPs Memorandum of Understanding (MOU) with different service providers Communication systems compliant with Redundancy and Disaster Planning in Health's Capital Works Programs (2nd Ed) 2010. 3.4.4 Interdependencies Electricity supply Human resourcing Contractual fulfilment by obligated service provider and carriers 3.4.5 Key contacts and expert advisors Name Organisation Position Landline Telecommunications Infrastructure Manager HIN Lead Advisor 08 6213 5499 Manager, Telecommunications FHHS Expert Advisor 08 9431 2895 Telecommunications Service Coordinator RPH Expert Advisor 08 9224 7000 Manager, Service Delivery HIN (Royal St) Expert Advisor 08 9222 2338 32 State Health Business Continuity Plan 3.4.6 Communication systems BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or Resource What could cause the loss of the Activity or Resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See Impact Table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indefinitely Restoration of internal telephone communication system Indefinitely Restoration of external telephone communication system Indefinitely Restoration of internal paging network Liaise with carrier to ensure priority restoration of services 3.4.6.1 Continuity of internal telephone communication systems. Multi-site or widespread telephone network failure (PABX or VoIP failure) Inability to communicate with onsite or off-site health care staff, emergency services and between health care assets. Assist health service in setting up alternative switchboard 5 Immediate Liaise with media to inform public of communication issues. Notify WA Health assets through sitrep notification and broadcasting Liaise with external telephone provider to ensure priority restoration of services 3.4.6.2 Continuity of external telephone communication systems. Multi-site or widespread telephone network failure (PSTN or VoIP failure) Inability to communicate with onsite or off-site health care staff, emergency services and between health care assets. Liaise with media to inform public of communication issues. 3 Immediate Notify WA Health assets through sitrep notification and broadcasting Assist hospital to set up alternate telephone exchange / switchboard Assist health care sites to liaise with contractor to ensure early restoration of paging services 3.4.6.3 Continuity of internal paging communication systems. Single or multi-site failure of internal paging network. 1 Inability to page on-site health care staff members or on-call emergency staff. 4 Immediate Liaise with media to inform public of communication issues. Notify WA Health assets through sitrep notification and broadcasting Carrier and local sites Public Relations Manager DPMU – OCDO/OCCO State Health Coordinator External telephone provider Public Relations Manager Department of Health DPMU – OCDO/OCCO State Health Coordinator Hospital Health Coordinators and individual site Telecommunication Managers Public Relations Manager Department of Health DPMU – OCDO/OCCO State Health Coordinator 33 State Health Business Continuity Plan 3.4.6 Number 3.4.6.4 3.4.6.5 Communication systems BCP CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? Continuity of external paging communication systems. Continuity of mobile telephone communications systems. Failure of external paging network. Intentional or unplanned mobile telephone network failure Inability to page on-site health care staff members or on-call emergency staff. Unable to contact transplant candidates awaiting organ donation. Inability to contact on-site or offsite key stakeholders, health care staff or emergency personnel. IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Assist health care sites to liaise with contractor to ensure early restoration of paging services 2 HHCs and individual site telecommunication managers Liaise with media to inform public of communication issues. Public Relations Manager Department of Health Indefinitely Restoration of internal paging network Notify WA Health assets through sitrep notification and broadcasting DPMU – OCDO/OCCO State Health Coordinator Liaise with mobile telephone providers to ensure priority restoration of mobile telephone networks affiliated with health care assets. 3 Hospital Health Coordinators and individual site Telecommunication Managers Liaise with media to inform public of communication issues. Public Relations Manager Department of Health Indefinitely Restoration of mobile telephone network. Notify WA Health assets through sitrep notification and broadcasting DPMU – OCDO/OCCO Indefinitely Restoration of MERN Radio Network or establishment of alternative radio network/communication platform. 4 4 Immediate Immediate Failure of health care staff's personal mobile telephones Assist HIN in the repair of the MERN radio network 3.4.6.6 Continuity of Metropolitan Emergency Radio Network (MERN) Technical Problem or electromagnetic interference leading to MERN failure Failure to communicate between health care facilities through MERN radio network. Failure to communicate with deployed health care teams in the field. Liaise with media to inform public of communication issues. 3 Immediate Notify WA Health assets through sitrep notification and broadcasting. Assist in the procurement of alternative communication platforms to deployed health care teams State Health Coordinator Chief Information Officer (HIN) Public Relations Manager Department of Health SHICC Logistics Cell Coordinator; or DPMU – OCDO/OCCO SHC 34 State Health Business Continuity Plan 3.4.6 Communication systems BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? Continuity of Metropolitan Health Voice Network (DOHnet / Tie lines) 3.4.6.7 Technical Problem or electromagnetic interference leading to DOHnet failure IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Chief Information Officer (HIN) Indefinitely Restoration of DOHnet network Indefinitely Re-establishment of essential communication platforms. Communicate through alternative methods (pager, email, facsimile, mobile telephone, radio, MERN, runners) Failure to communicate between health care facilities through DOHnet network. 4 1 Indefinite outage time Liaise with media to inform public of communication issues. Notify WA Health assets through sitrep notification and broadcasting Prioritise the restoration of at least 2 communication platforms. Continuity of all communication platforms 3.4.6.9 Catastrophic and simultaneous failure of multiple communication platforms at multiple sites. Failure to communicate between health care facilities, health care workers, emergency staff 5 Immediate Re-establish telecommunication services to health care facilities SHICC Operations Cell Coordinator (Hospital Service Continuity) Utilise the media to relay information Public Relations Manager Department of Health 3.4.7 Notes 1. Health care assets operate stand alone paging systems that are not interconnected with other health care facilities. Includes the SHC use of emergency purchasing powers. 2. External paging services are being utilised less due to the reliance on mobile telephone and Smartphone technology. Many companies are now scaling down external paging services. 3. In major incidents, telephone companies may allow special access to telephone networks only for emergency services. 4. DOHnet outage would result in a significant increase in cost associated with the loss of free telephone connections between health care facilities. 35 State Health Business Continuity Plan 3.5 Electricity Supply 3.5.1 Description This plan covers for failure of the supply of electricity from the network supplier on a medium to long-term basis. Health assets may be without electricity for a considerable time, or experience fluctuating or low quantity supplies. Failure could be due to one of many causes (industrial action, storm damage, earthquake, bomb, tsunami, terrorist attack, etc). 3.5.2 Critical business activities 1. Provision of electricity supplies to state wide health care assets and hospitals. 3.5.3 Prevention and mitigation strategies Local site BCPs MOUs and customer relationship plans with utility provider(s) Ensure that capital infrastructure development is in accordance with Redundancy and Disaster Planning in Health Capital Works Programs 2nd Ed. (2010) and AS/NZS 3009 Regular testing schedule for emergency diesel generators Regular cleaning of sump sludge in diesel generators to prevent generator failure. Adequate diesel fuel storage based on requirements Local site MOUs for emergency diesel resupply for emergency generators 3.5.4 Interdependencies Contractual fulfilment by obligated utility provider(s) Gas Supply Note: As of 2012, approximately 60% of electricity is generated through natural gas turbines. With many new health capital works projects including the installation of gas-powered tri-generation systems to provide electricity to hospitals, health care assets may be particularly vulnerable to a disruption in gas supply. 3.5.5 Key contacts and expert advisors Title Area Director, Infrastructure and Facilities Management Organisation Position Landline SMHS Lead Advisor 08 6466 7822 Executive Director, Facilities Management NMHS Expert Advisor 08 9346 3865 Manager, Infrastructure Support CAHS/WNHS Expert Advisor 08 9340 1407 Manager, Capital and Infrastructure WACHS Expert Advisor 08 9223 8555 Manager, Engineering Services FHHS Expert Advisor 08 9431 2467 36 State Health Business Continuity Plan 3.5.6 Electricity Supply BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indefinite - dependant upon fuel supply Restoration of reliable power supply to health care assets Implement demand management strategies (see Appendix 3) Power cogeneration HHCs Organise/coordinate re-supply of fuel for emergency back-up generators 1 3.5.6.1 Supply of state wide electricity to health care facilities and hospitals Local or remote loss of electricity supply. Cessation of operational health care capabilities (limited capability for emergency surgery) 5 Coordinate hospital resource sharing (CSSD) where practicable Immediate State Health Coordinator Coordinate reduction in elective surgery. Seek alternative sources of linen, or utilise disposable linen supplies Liaise with supplier to ensure priority restoration Utility Provider (Western Power / Horizon Energy). Coordinate the supply of alternative power sources 3.5.7 Notes 1. State government coordination of fuel resupply if during a fuel shortage crisis in line with WESTPLAN – Liquid Fuel Supply Disruption. 37 State Health Business Continuity Plan 3.6 Gas supply 3.6.1 Description This plan covers for failure of the mains gas supply on a widespread or long term basis. Health assets may be without gas for a considerable time, or experience irregular supply. Loss of supply could manifest through remote external supply interruption (damage, plant failure) or through on-site plant failure or malpractice. 3.6.2 Critical business activities 1. Provision of gas supply to State wide hospitals and health care facilities 3.6.3 Prevention and mitigation strategies Local site BCPs MOUs and customer relationship plans with facility providers Ensure that capital infrastructure development is in accordance with Redundancy and Disaster Planning in Health Capital Works Programs 2nd Ed. (2010) Ability to interchange fuel for boilers Ensure minimum of at least 7 days storage capacity 3.6.4 Interdependencies Contractual fulfilment by obligated utility provider(s) 3.6.5 Key contacts and expert advisors Title Area Director, Infrastructure and Facilities Management Organisation Position Landline SMHS Lead Advisor 08 6466 7822 Executive Director, Facilities Management NMHS Expert Advisor 08 9346 3865 Manager, Infrastructure Support CAHS/WNHS Expert Advisor 08 9340 1407 Manager, Capital and Infrastructure WACHS Expert Advisor 08 9223 8555 Manager, Engineering Services FHHS Expert Advisor 08 9431 2467 38 State Health Business Continuity Plan 3.6.6 Gas Supply BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Implement demand management strategies (see Appendix 4) HHCs Indefinitely Bulk gas supply is restored Loss of hot water, steam, sterilisation capability, kitchen, air-conditioning and laundry services. 3.6.6.1 Supply of State-wide gas Local or remote loss of gas supply. Decreased external power availability Decreased ability to produce CO2, O2 and dry ice. Indirect consequences due to loss of service (medico-legal, research, capital works, waste processing) Liaise with supplier about priority restoration of gas supply 1. 5 Immediate Liaise with electricity facility provider about priority power supply to health care assets Liaise with health contractors about implementing contingencies Gas utility provider (Alinta Gas) Electricity facility providers (Western Power Horizon Power) Health contractors (Waste, Medical Gases, Catering) 3.6.7 Notes 1. Refer to WESTPLAN - Gas Supply Disruption (2011) 39 State Health Business Continuity Plan 3.7 Human Resources 3.7.1 Description This plan covers arrangements for human resource management for specialist clinical staff and non-specialist general staff members. Human resourcing issues may be due to a surge in demand or staffing shortage, and can present significant organisational issues to WA Health, with potentially direct impacts on the safe provision of patient care. 3.7.2 Prevention and mitigation strategies Local site BCPs Local and area-wide volunteer management policies 3.7.3 Managing surge For management of human resources in a surge event, please refer to the Master Action Card 7 of the Surge Management Plan (2010) and section 2.2.1.7 of the WAHMPPI (2009). 3.7.4 Interdependencies Transportation and parking – Refer to Transport Services Section Security Services – Refer to Security Services Section 3.7.5 Volunteer Management WA Health has a volunteer policy that outlines the recruitment and management of voluntary staff. The use of volunteers is primarily to support health care delivery rather than replace work traditionally undertaken by paid health service staff. In the event of disaster or service disruption, WA Health may either be overwhelmed by spontaneous volunteers and donations of support, or experience a shortage of willing volunteers. Volunteering WA is the peak body for volunteer management in WA. Volunteering WA can be utilised to register and manage spontaneous volunteers, as well as a central contact to mobilise volunteers who have had criminal record screening. Volunteering WA can be contacted on (08) 9482 4333. 3.7.6 Key contacts and expert advisors Title Principal Nursing Advisor Organisation Nursing and Midwifery Office Position Landline Expert Advisor 08 9222 0288 Director, Workforce WA Health Expert Advisor 08 9222 4193 Manager NurseWest Expert Advisor 08 6444 5308 Senior Manager, Services Volunteering WA Expert Advisor 08 9482 4333 40 State Health Business Continuity Plan 3.7.7 Number Human Resources BCP CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or Resource What could cause the loss of the Activity or Resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See Impact Table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Identify / prioritise core services (e.g. cancellation of elective surgery) Redeploy staff from unaffected hospitals.1 Shortage of clinical staff Provision of specialist human resources 3.7.7.1 (e.g.: Medical, Nursing, Allied Health, etc) Multiple Causes (e.g.: Industrial action, surge event, absenteeism due to epidemic illness) Restriction or cessation of clinical service provision 4 Dependant upon nature of trigger and affected positions Inability to provide adequate staffing for clinical care Temporary or permanent recruitment of additional clinical staff Resolution of human resourcing issues HR Directors HHCs Dependant upon nature of trigger and affected positions Surge in activity subsides Staffing returns to minimum safe levels NurseWest Use of casual or locum health care professionals.2 Core services restored Overseas or interstate temporary recruitment of specialist staff 3 Identify / prioritise core services Provision of generic human resources 3.7.7.2 (e.g.: patient support staff, administration, clerical, etc) Shortage of non-clinical staff Multiple Causes (e.g.: Industrial action, surge event, absenteeism due to epidemic illness) Restriction or cessation of clinical service provision 3 Inability to provide adequate staffing for clinical support Dependant upon nature of trigger and affected positions Redeploy staff from unaffected hospitals.1 Temporary or permanent recruitment of additional nonclinical staff Resolution of human resourcing issues HR Directors HHCs Dependant upon nature of trigger and affected positions Surge in activity subsides Staffing returns to minimum safe levels Volunteering WA Core services restored Utilise volunteer staff 4 3.7.8 Notes: 1. The SHC has the authority to redistribute staff throughout WA Health to backfill urgent staffing deficits or to relocate staff to alternative facilities in response to a critical service disruption. 2. Refer to Master Action Card 7 of the Surge Management Plan 2010; NurseWest Business Continuity and Recovery Plan 2011; WAHMPPI, 2009. 3. Refer to OD 0338/11 Registration of interstate health practitioners in a disaster. 4. Refer to WA Health Volunteer Policy. 41 State Health Business Continuity Plan 3.8 3.8.1 Information and communication technology Description Information and Communication Technology (ICT) is an essential tool utilised by WA Health for both clinical and non-clinical business activities. A disruption in ICT services can seriously impact on the core business functions of WA Health, including patient care delivery. ICT failure can be a result of infrastructure failure, application error or both. The Health Information Network (HIN) is the State-level agency responsible for supporting and maintaining ICT infrastructure and applications, including BCM for WA Health. 3.8.2 BCM Arrangements HIN has developed their own specific BCPs and Disaster Recovery Plans that cover ICT failures, or outages, in both enterprise applications and enterprise infrastructure. Detailed failover and recovery plans are also available that cover central data centres, which house core systems. Enterprise applications are covered by Service Level Agreements (SLAs) which outline predetermined response and recovery times for application outages. 3.8.3 Interdependencies Electricity Gas Human resources Contractual fulfilment by obligated service provider(s) 3.8.4 Incident Management In the event of an ICT outage, HIN is to be contacted on 1300 170 089 (business hours) or 1300 302 536 (after hours) to log a service call. For any application problems, infrastructure failure, or service disruption that directly affects critical business activities, including patient care, the OCDO is to be paged on (08) 9328 0553. The OCDO will hand the incident over to the OCCO, who will liaise with HIN stakeholders and hospitals to ensure information pertaining to the ICT disruption is disseminated to all relevant stakeholders. 42 State Health Business Continuity Plan 3.9 Linen Supply 3.9.1 Description and scope of this plan This plan covers the loss of linen supply to hospitals and health care facilities and is enacted when local BCPs fail, or due to problems with the service contractor. This plan is activated when a State-level response is required. Linen is supplied and used in two major areas of hospitals; general services, such as wards; and specialised linen in operating rooms and other procedural areas. In metropolitan Perth, linen is laundered by contractors off-site and transported to health care sites and hospitals. In regional areas, linen is predominantly laundered on-site. In the event of a linen shortage, WA Health must also compete for available linen resources with private and public accommodation providers, such as hotels. 3.9.2 Critical business activities 1. The provision and delivery of linen to State wide health care assets. 3.9.3 3.9.4 3.9.5 Prevention and mitigation strategies Local site BCPs MOUs with utility providers about priority customers in a shortage (e.g.: gas or electricity supply) Interdependencies Gas supply Power supply Water supply Transport Contractual fulfilment by obligated service providers Key contacts and expert advisors Name Organisation Position Landline Manager, Patient Support Services FHHS Co-lead Advisor 08 9431 2857 Manager, Patient Support Services SCGH Co-lead Advisor 08 9346 3180 SMHS Expert Advisor 08 6466 7816 Manager, General Services RPH Expert Advisor 08 9224 3033 Manager, Patient Support Services RGH Expert Advisor 08 9599 4600 Manager, Support Services PMH Expert Advisor 08 9340 8532 Contract Manager, Finances SKHS Expert Advisor 08 3947 5295 Senior Contracts Officer, Corporate & Clinical Contracting 43 State Health Business Continuity Plan 3.9.6 Number Linen Services BCP CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Dependant upon size of storage area Normal linen collection service is restored Organise alternate collectors Store soiled linen in temporary storage area 3.9.6.1 Supply of linen to health care assets Soiled linen not collected Build-up of soiled linen supplies4 3 1 day Seek alternative sources of linen, or utilise disposable linen supplies Local site linen managers through HHCs HCN Liaise with supplier to ensure priority restoration of linen provision Implement demand management strategies (see Appendix 5) 3.9.6.2 Supply of linen to health care assets Critical service failure of contracted linen supplier (E.g. Gas Supply Disruption) State wide linen shortages or incomplete linen orders 4 1 day Seek alternative sources of linen through: (i) Other linen stockholders (e.g.: Brightwater) HHCs (ii) Interstate agencies (e.g. South Australia) HCN 1 - 3 days (dependant upon disposable linen redundancy and nature of service disruption) Restoration of critical services by contracted linen supplier or Alternative supplier(s) of linen is utilised 1,2 Utilise disposable linen supplies Liaise with supplier to ensure priority restoration of linen provision Nursing Agencies 3.9.6.3 Supply of linen to health care assets Staff shortages Inability to deliver clean linen and remove soiled linen 4 4 1 day Enlist volunteers / agency staff to collect and deliver linen 3 EMWA 1 week HCN Staffing issues resolved or minimal staffing requirement achieved Volunteer organisations 44 State Health Business Continuity Plan 3.9.7 Notes 1. The current contractor is the only company that is able to supply linen in the quantities required by WA Health. There is therefore limited redundancy in the event of a service disruption affecting linen services. Therefore WA Health would be required to negotiate with multiple smaller suppliers and urgently procure alternative linen stocks should the current contractor be subjected to a major service disruption. 2. In the event of a linen shortage, WA Health must also compete for available linen resources with private and public accommodation providers, such as hotels and hostels. 3. Refer to Human Resources Section. 4. Build-up for soiled linen poses an increased risk of infection and vermin infestation. 45 State Health Business Continuity Plan 3.10 Medical Gas Supply 3.10.1 Description This plan covers for the loss of bulk medical gas supplies to hospitals and health care facilities, and is enacted when local BCPs fail, or due to problems with the facility provider. 3.10.2 Critical business activities 1. Provision of medical gases to health care facilities through the supply of: a. Bulk medical gases. b. Specialist medical gases. 3.10.3 Prevention and mitigation strategies Local site BCPs MOUs and customer relationship plans with utility provider(s) and alternate suppliers Ensure that capital infrastructure development is in accordance with Redundancy and Disaster Planning in Health Capital Works Programs 2nd Ed. (2010) and AS/NZS 3009 3.10.4 Interdependencies Contractual fulfilment by obligated medical gas provider(s) Home oxygen patients 3.10.5 Key contacts and expert advisors Title Area Director, Infrastructure and Facilities Management Organisation Position Landline SMHS Lead Advisor 08 6466 7822 Executive Director, Facilities Management NMHS Expert Advisor 08 9346 3865 Manager, Infrastructure Support CAHS/WNHS Expert Advisor 08 9340 1407 Manager, Capital and Infrastructure WACHS Expert Advisor 08 9223 8555 Manager, Engineering Services FHHS Expert Advisor 08 9431 2467 3.10.6 Medical Gas Suppliers Company Phone (Business) Phone (Emergency) Website Email BOC 1800 363 109 1800 653 572 www.boc.com hospital.care@boc.com Air Liquide 08 6389 1199 www.airliquidehealthcare.com.au 46 State Health Business Continuity Plan 3.10.7 Medical Gas Supply BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indefinitely Bulk gas supply is restored Indefinitely Resumption in the delivery of bulk gases Organise alternate supply of medical gases from interstate. 1 Coordinate supply of bottled gas stores 3.10.7.1 Supply of Bulk Medical Gases Disruption in local production of medical gases (Kwinana) Loss of bulk gas replenishment to State-wide health infrastructure 5 Immediate HHCs Enact BOC MOU Consolidate patients requiring O2 into one centralised hospital BOC Coordinate the supply of medical gases for home oxygen services Vacate affected regional hospitals 3.10.7.2 Supply of Bulk Medical Gases Inability to deliver bulk supply Inability to supply regional health assets with bulk medical gas supplies 5 Immediate Liaise to deliver gas supplies through alternative means of transport. Oversee air-freighting in of bulk medical gas supply to regional health centres HHCs BOC 47 State Health Business Continuity Plan 3.10.7 Medical Gas Supply BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indefinitely Supply of specialist gases is resumed Inability to provide certain specialist clinical capabilities Carbon Dioxide (CO2) Storage of donor tissues, Operating Theatre instruments (lasers), Angiography Heliox 2 Used in critical care for treatment of asthma and airway obstruction 3.10.7.3 Supply of specialist medical gases (e.g., CO2, He2+, N2O, NO, etc) Disruption in supply of specialist medical gases Nitrous Oxide (N2O) Anaesthesia and pain relief Nitric Oxide (NO) Used in critical care for treatment of pulmonary hypertension and ARDS Implement demand management strategies 4 Dependant upon gas Source specialist gases from alternative supplier HHCs BOC Utilise alternative anaesthetics and analgesia Nitrogen (N) Used to power medical instruments and in packaging Argon (Ar) Used in cryosurgical procedures 3.10.8 Notes 1. Most hospitals should have 3 - 4 days contingency before requiring replenishment of bulk medical gas stores 2. Helium in MRI units are self-contained and do not require replenishment. Problems would arise only if Helium overheated and was released into atmosphere. In these situations an emergency quench would occur. 48 State Health Business Continuity Plan 3.11 Pharmaceutical Supply and Services 3.11.1 Description and scope of this plan This plan seeks to ensure the continuity of pharmaceutical supplies and services for hospitals in the state of Western Australia. This will essentially involve ensuring the provision of necessary drugs to maintain the functioning of a health care facility but may also include services such as preparation of sterile and cytotoxic drugs, dispensing, manufacture of special products and provision of clinical services and drug information. 3.11.2 Critical business activities 1. Continuation of pharmaceutical services through: a. The procurement of pharmaceutical items. b. The storage of pharmaceutical items. c. The supply and dispensing of pharmaceutical items. d. In-house manufacturing of specialist pharmaceutical items. e. Extraordinary circumstances (stock-piling, rationing, pandemic/epidemic planning). 3.11.3 Prevention and mitigation strategies Contractual requirements for redundancy on CUA agreement Local site BCPs Maintenance of relevant pharmaceutical stockpiles Power supply to warehouse and storage 3.11.4 Interdependencies Power supply Transport Warehousing and storage Water Supply Gas Supply Contractual fulfilment by obligated service providers 3.11.5 Key contacts and expert advisors Name Organisation Position Landline Head of Department, Pharmacy SCGH Lead Advisor 08 9346 2334 Coordinator Pharmacy Manufacturing Services RPH Expert Advisor 08 9224 2081 Chief Pharmacist PMH Expert Advisor 08 9340 8224 Director, Pharmacy Services FHHS Expert Advisor 08 9431 2967 Senior Pharmacist SKHS Expert Advisor 08 9391 2046 Public Health Expert Advisor 08 9222 6883 Chief Pharmacist WACHS Expert Advisor 08 9174 1336 Principal Pharmacist AKHS Expert Advisor 08 9391 2043 Chief Pharmacist, Disaster Management, Planning and Regulation 49 State Health Business Continuity Plan 3.11.6 Pharmaceutical Supply and Services BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Communicate with stockpile holders regarding release of medication Initiate State control for collation and distribution of State pharmaceutical stockpile 3.11.6.1 Supply and dispensing of pharmaceutical stock and extraordinary circumstances Surge in demand due to Epidemic, Pandemic or Major Incident that overwhelms current supplies Decreased or unavailable pharmaceutical stock 4 Immediate Implement planning groups and clinical stakeholders meeting Provide assistance in procurement of additional supply or procurement of alternative drug. 1 State Health Chief Pharmacist to coordinate in conjunction with Hospital Chief Pharmacists and WATAG Procurement and stockpiling of adequate quantities of pharmaceuticals to meet requirement Indeterminate depends upon nature of surge. or Surge in demand subsides Assist in the sourcing of alternative warehouse and storage equipment (e.g. fridges) Communicate with stockpile holders regarding release of medication 3.11.6.2 Procurement, Supply and dispensing of pharmaceutical stock Stock Quarantine, Product Recall or manufacturing delay on specialist item or critical item without clinical substitute. Decreased or unavailable pharmaceutical stock 4 Initiate State control for collation and distribution of State pharmaceutical stockpile Immediate Implement planning groups and clinical stakeholders meeting State Health Chief Pharmacist to coordinate in conjunction with Hospital Chief Pharmacists and WATAG Specialist item becomes available Indeterminate or depends upon item involved. Clinical substitute becomes available Provide assistance in procurement of additional supply or procurement of alternative drug. 50 State Health Business Continuity Plan 3.11.6 Pharmaceutical Supply and Services BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Coordinate sourcing and distribution of new stock from manufacturers or sourcing from alternate manufacturer 3 3.11.6.3 Supply and dispensing of pharmaceutical stock Warehouse or storage disruption (fire, flood, power disruption) 2 Decreased or unavailability of multiple items of pharmaceutical stock 5 Initiate State control for collation and distribution of remaining State pharmaceutical stockpile Immediate State Health Chief Pharmacist to coordinate Indeterminate Depends upon type and quantity of affected items 4 Availability of necessary minimum stock levels. Implement planning groups and clinical stakeholders meeting at health service level Implement planning groups and clinical stakeholders meeting 3.11.6.4 Procurement of pharmaceutical stock Delivery disruption or delays (e.g. ash cloud, industrial action) Provide assistance in expediting delivery of pharmaceutical supplies from alternative origin or supplier. Decreased or unavailable pharmaceutical stock 5 Immediate State Health Chief Pharmacist to coordinate ● Liaising with ADF to assist in delivery of items Alternative delivery arrangements organised Depends upon type and quantity of affected items, nature of industrial action or if alternative transport arrangements can be utilised Utilise alternative transport methods by: ● Seeking WA Police assistance to ensure safe delivery of stock Indeterminate or Resumption of normal delivery arrangements WA Police ADF through SECG 3.11.7 Notes 1. WA Health may also be contractually bound by CUAs and government policy. 2. Redundancy: 3 warehouses available (2 for public hospitals, 1 for commercial pharmacies) 3. The SHC may use emergency purchasing powers to lease alternative warehouse and storage equipment 4. Current IV fluid supplier has a monopoly on the supply of IV fluids in Australia. Any incident involving this company could have national ramifications and require international sourcing of products. 51 State Health Business Continuity Plan 3.12 Security services 3.12.1 Description and scope of this plan This BCP covers the provision of security services to health care facilities, and is enacted when hospitals and health care facilities are overwhelmed and local arrangements and BCPs have failed. 3.12.2 Critical business activities 1. Continuation of security services through the provision of: a. General security services. b. Security services in extraordinary circumstances. 3.12.3 Prevention and mitigation strategies Local site BCPs State level MOUs with Department of Corrective Services and WA Police and security contractors. CUAs 3.12.4 Interdependencies Electricity Communications, including surveillance and monitoring technologies WA Police Contractually obligated service provider Human resources 3.12.5 Key contacts and expert advisors Name Organisation Position Telephone Manager, Area Security NMHS Lead Advisor 0417 095 870 Security Supervisor RPH Expert Advisor 08 9224 3800 Security Supervisor FHHS Expert Advisor 08 9431 2600 52 State Health Business Continuity Plan 3.12.6 Security services BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Dependant upon nature of incident and availability of resources Surge in patients subsides or provision of adequate security personnel to secure health care facilities Liaise with WA Police as required 3.12.6.1 Provision and continuation of security services in normal and extraordinary circumstances. Inundation of people to health care facilities due to a surge in attendances at a hospital of health care facility Assist in the sourcing of extra security staff from private security firms. Inability to maintain security services 4 Immediate WA Police Private Security Firms Redistribute security personnel from other health care assets. Consult with mental health facilities regarding security requirements HHCs Mental Health Advisors Liaise with WA Police to assist in securement of health care facilities. Redistribute security personnel from other health care assets. 3.12.6.2 Provision and continuation of security services in normal and extraordinary circumstances. Large scale acts of violence in community, impacting upon hospital services Inability to provide adequate security services 5 Immediate Assist in the sourcing of extra security staff from private security firms. Liaise with MRWA, PTA and WA Police about establishing secure transport corridor for staff members to and from health care facilities HHCs WA Police Violence is controlled MRWA indefinite Security is strengthened to health care assets PTA SECG Mental Health Advisors Consult with mental health facilities regarding security requirements 53 State Health Business Continuity Plan 3.12.6 Security services BCP Number 3.12.6.3 CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See Impact Table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Provision and continuation of security services in normal and extraordinary circumstances. Large inundation of high risk prisoners into hospital setting (E.g. prison riot, evacuation or fire) Liaise with WA Police & Department of Corrective Services to assist in securement of health care facilities Inability to provide or maintain adequate security services 4 Immediate Liaise with Department of Corrective Services regarding the distribution of prisoners to hospitals or the requirement to either cohort or separate high risk prisoners. 1 HHCs Department of Corrective Services or relevant contractor Bulk of prisoners are sent back to prisons. Dependant upon nature of incident and availability of resources WA Police 3.12.7 Notes 1. The securement, transport and welfare of prisoners are the sole responsibility of the Department of Corrective Services or authorised contractor. 54 Hospitals are secured by Dept of Corrective Services or approved contractor State Health Business Continuity Plan 3.13 Specialist services 3.13.1 Description and scope of this plan This BCP covers the provision and continuity of designated State specialist services, such as burns, adult trauma and paediatric trauma. These services are essential services that are not duplicated elsewhere within the State. 3.13.2 Scope of this plan This plan covers the loss of specialist services that are unable to be accommodated within the originating health service’s existing infrastructure or business continuity plans and whereby State-level intervention is required to assist in the relocation of the service. Where an entire hospital evacuation is required, this section of the plan may be activated in conjunction with the Surge Management Plan. 3.13.3 Out of scope for this plan Specialist staff is covered by the human resources section of this BCP. Loss of specialist consumables is covered under the supply and logistics section of this BCP. 3.13.4 Critical business activities 1. Provision of specialist State Adult Trauma Service. 2. Provision of specialist State Paediatric Trauma Service. 3. Provision of specialist State Burns Service. 3.13.5 Prevention and mitigation strategies Local site BCPs MOUs with private hospitals 3.13.6 Interdependencies Human Resources Supply of specialist consumables Medical Gas supply Electricity supply Water supply Specialist biomedical equipment Pharmaceutical services Other specialist clinical services (e.g.: ICU, Theatres, ED) 3.13.7 Key contacts and expert advisors Name Organisation Position Telephone Director, State Trauma Service RPH Lead Advisor (08) 9224 2244 Trauma Program Manager RPH Expert Advisor (08) 9224 8076 Senior Project Officer – Trauma Services RPH Expert Advisor (08) 9224 2487 Director State Burns Service RPH Expert Advisor (08) 9224 3558 Clinical Nurse Consultant – Burns Service RPH Expert Advisor (08) 9224 3578 Executive Director – Medical Services PMH Expert Advisor (08) 9340 8245 55 State Health Business Continuity Plan 3.13.8 Specialist Services BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or Resource What could cause the loss of the Activity or Resource? What will the impact be if that activity / resource is not available? See Impact Table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Provision of specialist adult State Trauma Services 3.13.8.1 Loss of assets (Building loss) Inability to provide specialist Adult Trauma Service 5 Relocate trauma service to alternative facility1 Immediately Move Trauma Service staff to alternative facility2 SHC HHCs Director of State Trauma Services Indeterminate, depends upon nature of incident and ability of temporary facility to provide specialist support Co-locate State Paediatric Trauma Service with State Adult Trauma Service SHC Provision of specialist Paediatric State Trauma Services 3.13.8.2 or Loss of assets (Building loss) Inability to provide specialist Paediatric Trauma Service 4 Immediately HHCs Relocate trauma service to alternative facility1 Director of State Trauma Services Indeterminate, depends upon nature of incident and ability of temporary facility to provide specialist support Move Trauma Service staff to alternative facility (Allied Health, Medical and Nursing Staff) 2 Provision of specialist State Burns Services 3.13.8.3 Loss of assets (Building loss) Inability to provide specialist Burns Service 5 Relocate burns service to alternative facility1 Immediately Move Burns Unit staff to alternative facility2 SHC HHCs Director of State Burns Services Indeterminate, depends upon nature of incident and ability of temporary facility to provide specialist support Reestablishment of State Adult Trauma Services at alternative site or existing site. Reestablishment of minimum operational requirements Reestablishment of State Paediatric Trauma Services at alternative site or existing site. Reestablishment of minimum operational requirements Reestablishment of State Burns Services at alternative site or existing site. Reestablishment of minimum operational requirements 3.13.9 Notes 1. Ideally, the alternative State Trauma and Burns Centres should have access to: Helicopter Landing Site; 24 hour Radiology Services (including USS, CT Scanner); Intensive Care Unit; Angiography; Transfusion Medicine laboratory; Emergency Department , Operating Theatres and positive pressure isolation rooms with air particle filtering. 2. Receiving health services are responsible for the credentialing of redeployed staff members. 56 State Health Business Continuity Plan 3.14 Specialist biomedical equipment 3.14.1 Description This plan covers the biomedical specialist equipment that is required to maintain essential life support for patients. It is the responsibility for each health site to have plans in place to cover the redundancy of their specialist biomedical equipment; however, in the event of a mass influx of patients the existing equipment may be insufficient to cater for the extra numbers. Alternatively, an incident may occur, such as a fluctuation in power from a lightning strike which renders a number of machines incapable, which could exceed the normal redundancy coverage of the health site. Such problems are to be resolved by the biomedical engineering staff. 3.14.2 Critical business activities 1. Utilisation of available specialist biomedical equipment. 2. Continuity of specialist biomedical equipment availability and functionality through: c. Procurement of new clinical equipment. d. Servicing, refurbishment and maintenance of current clinical equipment. e. Transferring of clinical equipment between health care assets. 3.14.3 Prevention and mitigation strategies Local Site BCPs Maintenance of the State medical equipment stockpile 3.14.4 Interdependencies Contractual fulfilment by obligated service providers Power supply Gas supply Medical gases supply Water supply Human resources and credentialing Supply of specialist items and consumables 3.14.5 Key contacts and expert advisors Title Organisation Head of Department, Medical Engineering and Physics RPH Lead Advisor 08 9224 3224 Senior Clinical Engineer (Biomedical Systems) RPH Expert Advisor 08 9224 2702 Manager, Biomedical Services FHHS Expert Advisor 08 9431 2094 Manager, Medical Technology Management CAHS Expert Advisor 08 9340 7081 Head of Department, Medical Technology and Physics SCGH Expert Advisor 08 9346 4288 WACHS Expert Advisor 08 9318 6888 SCGH Expert Advisor 08 9346 1347 Coordinator, Biomedical Engineering Services Product Liaison Officer, Hospital Equipment Services Position Landline 57 State Health Business Continuity Plan 3.14.6 Specialist biomedical equipment BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indeterminate, depends upon size and nature of incident Clinical equipment becomes serviceable or new clinical equipment is procured and commissioned. Indefinite Surge in patients subsides, or additional specialist equipment is procured or commissioned Coordinate and distribute additional resources from the State Medical Stockpile1 Disabled specialist equipment Multiple reasons Utilisation of available specialist biomedical equipment 3.14.6.1 Servicing, refurbishment and maintenance of current clinical equipment EG: Power Failure, Brownout, Equipment recall, loss of specialist consumables, medical gas failure, loss of suction, loss of water supply, gas or water contamination Inability to provide patient treatment, monitoring or interventions Inability to service, repair or refurbish available clinical equipment Coordinate in the mobilisation of biomedical expertise.4 4 Prioritise the delivery of health care services Immediate Loss of ability to communicate Damage to equipment Manage implications of major reductions in service delivery and relocations Borrow, procure or purchase additional equipment from private hospitals.2,3,4,5,6 Inability to provide sufficient clinical equipment resources based on demand. Coordinate in the mobilisation of biomedical expertise.4 3.14.6.2 A surge of patients to one or more health care sites as a result of an impact or pandemic event. Prioritise the delivery of health care services Inability to provide sufficient specialist equipment resources based on demand. Equipment procurement Biomedical Engineers to coordinate procurement of additional specialist equipment. Mobilisation of DPMU resources SHICC Logistics Cell Coordinator or On-Call Duty Officer Procure alternative specialist consumables items 6 Coordinate and distribute additional resources from the State medical stockpile1 Utilisation of available specialist biomedical equipment Health care delivery HHCs to manage local health asset implications 4 Immediate Manage implications of major reductions in service delivery and relocations Borrow, procure or purchase additional equipment from private hospitals.2,3,4,5,6 Procure alternative specialist consumables items 6 Health care delivery HHCs to manage local health asset implications Equipment procurement Biomedical Engineers to coordinate procurement of additional specialist equipment. Mobilisation of DPMU Resources SHICC Logistics Cell Coordinator or On-Call Duty Officer Refer to Metro Surge Plan 2010 58 State Health Business Continuity Plan 3.14.6 Specialist biomedical equipment BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indeterminate, depends upon size and nature of incident Decontamination of clinical equipment or procurement and commissioning of replacement clinical equipment Indeterminate, depends upon size and nature of incident Repair of existing specialist clinical equipment or replacement of disabled clinical equipment Coordinate and distribute additional resources from the State Medical Stockpile1 Coordinate in the mobilisation of biomedical expertise.4 3.14.6.3 Utilisation of available clinical equipment Contamination of reticulated water or medical gas lines at multiple health sites. Contamination of clinical equipment Inability to provide sufficient clinical equipment resources based on demand 4 Prioritise the delivery of health care services Immediate Manage implications of major reductions in service delivery and relocations Borrow, procure or purchase additional equipment from private hospitals.2,3,4,5,6 Health Care Delivery HHCs to manage local health asset implications Equipment Procurement Biomedical Engineers to coordinate procurement of additional specialist equipment. Mobilisation of DPMU Resources SHICC Logistics Cell Coordinator or On-Call Duty Officer Procure alternative specialist consumables items 6 Coordinate and distribute additional resources from the State Medical Stockpile1 Coordinate in the mobilisation of biomedical expertise.4 Disabled clinical equipment 3.14.6.4 Utilisation of available clinical equipment Rapid and escalating malfunction of particular specialist equipment Inability to provide patient treatment, monitoring or interventions 4 Prioritise the delivery of health care services Immediate Manage implications of major reductions in service delivery and relocations Borrow, procure or purchase additional equipment from private hospitals.2,3,4,5,6 Health Care Delivery HHCs to manage local health asset implications Equipment Procurement Biomedical Engineers to coordinate procurement of additional specialist equipment. Mobilisation of DPMU Resources SHICC Logistics Cell Coordinator or On-Call Duty Officer Procure alternative specialist consumables items 6 59 State Health Business Continuity Plan 3.14.6 Specialist biomedical equipment BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indefinite Additional clinical equipment is procured and commissioned Coordinate and distribute additional resources from the State medical stockpile1 Coordinate in the mobilisation of biomedical expertise.4 3.14.6.3 Utilisation of available clinical equipment Deficiency in clinical equipment or specialist consumables due to shortage or delay in clinical equipment procurement Inability to provide sufficient clinical equipment resources based on demand. 3 Prioritise the delivery of health care services Immediate Manage implications of major reductions in service delivery and relocations Borrow, procure or purchase additional equipment from private hospitals.2,3,4,5,6 Procure alternative specialist consumables items 6 Health Care Delivery HHCs to manage local health asset implications Clinical Equipment Procurement Biomedical Engineers to coordinate procurement of additional specialist equipment. Mobilisation of DPMU Resources SHICC Logistics Cell Coordinator or On-Call Duty Officer 3.14.7 Notes 1. The State Medical Stockpile includes specialist medical equipment and specialist consumables 2. Includes the SHC use of Emergency Purchasing Powers 3. Procurement of new equipment in a prolonged international incident could take up to 8 weeks or longer. 4. Purchasing of specialist equipment must be coordinated through Biomedical Engineers. 5. Procurement processes are still bound by State Government Policies, such as Common Use Agreements (CUA), delegation, etc 6. Stakeholders must ensure that staff are competent with redundancy equipment. 60 State Health Business Continuity Plan 3.15 Supply and Logistical Services 3.15.1 Description and scope of this plan This BCP covers the logistical supply of goods and consumables to hospitals linked to WA Health, key support agencies and interdependent agencies (such as private hospitals). 3.15.2 Current supply and logistical arrangements Under current arrangements, metropolitan hospitals are supplied through Health Corporate Network (HCN) Supply Services. WACHS services and hospitals purchase their supplies directly from the suppliers. 3.15.3 Critical business activities Procure and distribute goods and services for WA Health, including: 1. Requisition - receiving requests from hospitals: a. Held stock – from HCN warehouse b. Non held stock – requested via iprocurement. 2. Warehousing: a. Storage b. Inventory management c. Receipting of goods from vendor d. Binning. 3. Procurement: a. Contracts b. Placing orders with vendors c. Payment d. Following up on items not delivered (expediting). 4. Distribution: a. Picking b. Imprest c. Packing d. Courier service. 3.15.4 Prevention and mitigation strategies Local Site BCPs Adequate stock holding by HCN Warehouse and suppliers Review contractual requirements for redundancy to >48hrs Pre-identification of alternate suppliers 3.15.5 Interdependencies Power Transportation Warehousing Contractual fulfilment by obligated service providers Human resources Oracle 61 State Health Business Continuity Plan 3.15.6 Common use agreements and health contracts WA Health facilities are required to procure select items from designated suppliers as stipulated by WA State Government Common User Agreements (CUAs) and WA Health Contracts. In any urgent procurement process, WA Health must ensure that existing CUAs and health contracts are honoured. 3.15.7 Dawn Project Existing HCN warehouses located at RPH and FHHS are at capacity and cannot continue to effectively meet increasing demand. Under the proposed Dawn Project, the existing HCN warehouses will be closed and a single, centrally located distribution and warehouse facility will be established. The new facility will have the capacity to warehouse and distribute essential medical supplies more cost effectively and efficiently. The target date for the closure and re-location is October 2013. Despite the risk presented from warehousing all supplies in one location, this risk has been mitigated by “just-in-time” contracts and bulk storage of stock by suppliers. In the event of losing the Central HCN warehouse, the SHC can seek authorisation to lease an alternative warehouse under existing leasehold processes. This risk can be further mitigated by drawing on other health agencies, such as WACHS and private hospitals, for immediate replacement of stock, and utilising the strategic medical stockpile at the DPMU Warehouse. 3.15.8 Key contacts and expert advisors Title Organisation Position Landline Title Manager Procurement Services HCN Lead Advisor 08 6444 5182 0430317719 Coordinator Payment Management HCN Expert Advisor 08 6444 5144 0407480353 Coordinator iProcurement HCN Expert Advisor 08 6444 5174 0421344667 Coordinator Business Management HCN Expert Advisor 08 6444 5172 Coordinator Health Contract Procurement HCN Expert Advisor 08 6444 5137 0414481784 Coordinator Operational Procurement HCN Expert Advisor 08 6444 5106 0404890230 Manager Distribution HCN Lead Advisor 08 6444 5911 0413321052 Coordinator SDC Operations HCN Expert Advisor 08 6444 5179 0450959413 Coordinator Site Operations HCN Expert Advisor tba tba Director HCN Supply HCN Expert Advisor 08 6444 5951 0430991574 General Manager HCN HCN Expert Advisor 08 6444 5004 0404890183 62 State Health Business Continuity Plan 3.15.9 Supply and Logistics BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Implement planning groups with clinical stakeholders at health service level to coordinate the reduction in the use of available resources. Utilise private sector resources if and where available. 3.15.9.1 Request, store and procure goods and services Damage or loss of warehouse due to fire, flooding, access, etc. Decreased or unavailability of stock Inability to receipt, store or distribute goods and products Coordinate distribution of remaining stock and sourcing of new stock from supplier 4 2 days Assist with restoring access to warehouse (if applicable) OCMO to liaise with Clinical Stakeholders Director - HCN Supply Alternative warehousing site established Dependant upon access issues / Indefinitely HHCs or Access restored to warehouse and supplies Provide assistance by communicating with hospitals about the incident, and ensure system wide awareness of workarounds. Identify alternative warehouse Liaise with bulk suppliers in order to provide bulk replenishment Provide assistance by communicating with hospitals about the incident ICT Failure 3.15.9.2 Request, store and procure goods and services Oracle service failing – software / hardware / network issue (activity). Unable to perform requisition and procurement. 4 2 days Director - HCN Supply Ensure system wide awareness of workarounds. HHCs to implement demand management strategies Liaise with HIN about priority restoration of services Director Operations - HIN Indefinitely, but would require increased HCN and health resourcing Resolution of IT issues 63 State Health Business Continuity Plan 3.15.9 Supply and logistics BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Dependant upon supply issues and stock item Resolution of supply shortage or Dependant upon supply issues Resolution of supply shortage Provide assistance in procurement of substitute consumable through alternative supplier 3.15.9.3 Request, store and procure goods and services Shortage of general medical consumables in Western Australia Inability to perform general medical / surgical procedures 4 2 days If necessary; implement planning groups with clinical stakeholders at health service level to coordinate the reduction in the use of available resources. OCMO to liaise with clinical stakeholders Director - HCN Supply HHCs to implement demand management strategies Provide assistance by communicating with hospitals about the incident Coordinate the supply of existing available stock 3.15.9.4 Request, store and procure goods and services Shortage of specialist consumables Inability to perform specialist services 4 Dependant upon priority of consumables If necessary; implement planning groups with clinical stakeholders at health service level to coordinate the reduction in the use of available resources. Provide assistance by communicating with hospitals about the incident OCMO to liaise with clinical stakeholders Director - HCN Supply HHCs to implement demand management strategies Provide assistance in procurement of substitute specialist item through alternative supplier 64 State Health Business Continuity Plan 3.15.9 Supply and logistics BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Dependant upon supply issues and stock item Resolution of supply shortage or Coordinate the supply of existing available stock If necessary; implement planning groups with clinical stakeholders at health service level to coordinate the reduction in the use of available resources. 3.15.9.5 Request, store and procure goods and services International or national shortage of general or specialist medical or surgical consumables OCMO to liaise with clinical stakeholders Director - HCN Supply Inability to perform general medical / surgical procedures 4 Dependant upon priority of consumables Provide assistance by communicating with hospitals about the incident Provide assistance in procurement of substitute specialist item through alternative supplier HHCs to implement demand management strategies SHC Liaise with AHPC about prioritisation of care. 3.15.10 Notes 1. Please note: WACHS are supplied from different supply means and can be used as contingency supply in the event that a warehouse is destroyed or unavailable. 65 State Health Business Continuity Plan 3.16 Transport Services 3.16.1 Description and scope of this plan This plan covers the loss of transport services that affects the safe passage of patients, staff members and visitors through internal and externally-contracted transport services. This plan is activated when local BCPs fail and State-level intervention is required. This plan includes the loss of areomedical transport capabilities. 3.16.2 Out of scope This plan does not cover loss of St John Ambulance (SJA) assets and services. Please refer to the relevant SJA surge and business continuity plans. 3.16.3 Critical business activities 1. Transportation of medical products and samples, patients, escorts and visitors: a. From health care facility to health care facility. b. From health care facility to home or other destination. c. From home / other destination to health care facility. d. In a prehospital setting (including emergency and routine). 3.16.4 Prevention and mitigation strategies Local site and agency BCPs MOUs with transport and private ambulance / air ambulance providers 3.16.5 Relevant plans Ambulance Emergency Management Plan (AMBPLAN) WA 2010 Western Australian Mass Casualty Areomedical Transport Plan (2012) 3.16.6 Interdependencies Supply of liquid fuel Human resources and credentialing Access and egress to ports and health care facilities Supply and maintenance of suitable vehicles and airframes Contractual fulfilment by obligated service providers 3.16.7 Key contacts and expert advisors Name Organisation Position Landline Area Fleet Manager FHHS Lead Advisor 08 9431 2409 Manager, Patient Support Services SCGH Expert Advisor 08 9346 3180 Manager, Patient Support Services FHHS Expert Advisor 08 9431 2857 SMHS Expert Advisor 08 6466 7816 Manager, Patient Support Services RGH Expert Advisor 08 9599 4547 Manager, Support Services PMH Expert Advisor 08 9340 8532 Manager, Emergency Management SJA Expert Advisor 08 9334 1455 Senior Contracts Officer, Corporate & Clinical Contracting 66 State Health Business Continuity Plan 3.16.8 Transport Services BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indefinitely Resolution of industrial action or surge in demand subsides 1 Indefinitely Fuel availability restored 2 Indefinitely Health Fleet restored State level liaison with Public Transport Authority (PTA) and Taxi Council 3.16.8.1 Transportation of patients and patient escorts to outpatient appointments SJA, Taxi or Public Transport Industrial Action Higher demand and workload on internal transport services 2 1 day Cancellation of non-elective appointments Redistribute health vehicle fleet PTA / Taxi Council State Health Vehicle Fleet Department Liaise with St John Ambulance Patient Transport Services Oversee the utilisation of transport resources at State level 3.16.8.2 Transportation of patients, visitors and staff members Inability to utilise fleet vehicles or transport patients Fuel shortage Staff and patients unable to selftransport to and from hospital 4 Immediate Liaise with the PTA regarding organised transport of staff to hospital Secure fuel supply through State Emergency Coordination Group (SECG) and oversee utilisation of fleet vehicles at State level Commence contractual negotiations for renewed fleet lease agreement 3.16.8.3 Transportation of patients, visitors and staff members Loss of health fleet (due to damage, vehicle recall) Inability to utilise fleet vehicles or transport patients 3 Immediate Redistribute remaining health vehicle fleet State Vehicle Fleet Manager PTA SECG State Vehicle Fleet Manager St John Ambulance Liaise with St John Ambulance for transferring of patients 67 State Health Business Continuity Plan 3.16.8 Transport services BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Prioritise St John Ambulance transfers Liaise with hospitals regarding the utilisation of own transport services 3 3.16.8.4 Transportation of patients, visitors and staff members St John Ambulance patient transport demand surge Major Disaster or High Impact Event Delays and cancellations in the transport of patients Increased demand on SJA resources at scene. 4 Immediate Increased demand on transport services by hospitals to evacuate, decant and discharge patients. St John Ambulance Oversee the utilisation of transport resources at State level Hospital Transport Coordinators through HHCs Liaise with other private ambulance service providers to assist with transport requirements Private Ambulance Providers Liaise with Public Transport Authority for buses to transport discharged or decanted patients away from hospital. St John Ambulance demand subsides or Indefinitely Surge in demand of transport services subsides and recovery plans activated. Public Transport Authority WA Police Liaise with WAPOL regarding safe passage of fleet vehicle and health care workers through roadblocks and access issues. 3.16.8.5 Transportation of staff members to and from health care facilities Public Transport disruption Staff members unable to attend work 3 Assist hospitals in coordinating the charter of bus services from central hubs HHCs 1 day Indefinitely Utilise cab charge vouchers Transport Stakeholders Restoration of Public Transport Services Encourage car pooling 68 State Health Business Continuity Plan 3.16.8 Transport services BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indefinitely Areomedical transportation restored to minimum acceptable service levels Seek Federal assistance through SECG 4 3.16.8.6 Areomedical transportation of patients and patient escorts to outpatient appointments Multiple causes (loss of fleet, fuel shortage, weather, fleet grounding, surge or impact event) Delay / inability to transport patients in between regional areas and Perth 5 SECG Prioritise fuel provision to critical services through SECG Immediate Utilise private areomedical evacuation contractors Transport patients by alternative methods (road) RFDS to coordinate St John Ambulance 3.16.9 Notes 1. St John Ambulance will not utilise volunteer drivers for ambulances as volunteers lack emergency driver accreditation. As a last resort, they may utilise DFES or WA Police drivers. 2. Refer to WESTPLAN Liquid Fuel Supply Disruption (2011). 3. Transporting of clinical specimens is covered under the PathWest BCP. 4. Liaise with SECG to seek Federal assistance through Australian Emergency Management to activate Australian Medical Transport Coordination Group (AMTCG) via the Federal Department of Health and Ageing - National Incident Room, in order to provide a nationally coordinated aero-medical response. 69 State Health Business Continuity Plan 3.17 Waste services 3.17.1 Description This BCP covers the provision and continuity of waste services to hospitals and health care facilities and is enacted when local BCPs fail, or due to problems with the service contractor. This plan is activated when a State-level response is required. 3.17.2 Critical business activities 1. Removal of waste products from the hospital (excluding sewerage) including: a. Medical waste. b. General waste. 3.17.3 Prevention and mitigation strategies Local site BCPs Contractual negotiations and common use agreements (CUAs) ensuring continuance of service 3.17.4 Interdependencies Electricity supply Gas supply to contractor’s incinerator Transportation availability, including access to liquid fuel supply Contractual fulfilment by obligated service providers Human resources 3.17.5 Key contacts and expert advisors Name Organisation Position Telephone Operations Manager, Facilities Management RPH Lead Advisor 08 9224 2700 Facilities Manager CAHS Expert Advisor 0408 757 269 Manager, Patient Support Services FHHS Expert Advisor 08 9431 2857 Manager, Support Services CAHS Expert Advisor 08 9340 8532 70 State Health Business Continuity Plan 3.17.6 Waste services BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Provide direction and assistance in fast-tracking or resolving human resourcing issues. Utilise alternative contractor 3.17.6.1 Removal of general waste products from health care assets (includes recycled, confidential and food waste) Multiple causes (EG: transport problems, human resource deficit dispute with contractor, damage or loss of waste processing plant) Accumulation of general waste products in health care settings 7. Waste storage problems at health care facilities 1 - 3 days 2 Depends if individual sites have compactors Organise for contractor to collect waste after hours. Seek alternative contractor to facilitate the removal or processing of waste products. Utilise warehouse or secure area to temporarily store waste products. 1 SHEF HHCs Current contractor Alternative Waste Contractors Indeterminate Removal and disposal activities are restored to normal business operations (dependant upon effectiveness of contingencies) Local Governments Liaise with local governments for assistance Provide direction and assistance in fast-tracking or resolving human resourcing issues SHEF After-hours waste removal HHCs Utilise alternative contractor 2 Current contractor (SITA Medicollect) Multiple causes 3.17.6.2 Removal and disposal of medical waste products from health care assets (EG: transport problems, human resource deficit, dispute with contractor, damage or loss of waste processing plant, gas supply failure to incinerator) Accumulation of medical waste products in health care settings 7. Potential increased infection risk and infectious waste storage issues. 3 12 - 24 hours Alternative disposal methods including alkaline degradation and autoclaving 3,4 Supervised burials under environmental health direction in consultation with local government. Director - Environmental Health (WA Health) Local Governments Metropolitan Cemeteries Board Incinerator downtime contractor (SITA) have approximately 30 days contingency through storage in refrigeration containers Removal and disposal activities are restored to normal business operations Indeterminate if alternatives methods of disposal utilised in consultation with stakeholders Use of alternative incinerators (Interstate or crematoriums) 5,6 71 State Health Business Continuity Plan 3.17.7 Notes 1. Confidential waste to be managed at local level by purchasing of shredders 2. There is currently only one medical waste incinerator in metropolitan Perth. In the event of an outage involving the incinerator, the contractor has refrigeration units with 30 days of storage capacity. 3. Alkaline degradation and autoclaving methods require waste segregation and cannot be used to destroy pharmaceuticals, cytotoxic substances and body parts. 4. Alkaline degradation is situated adjacent to incinerator and may pose problem if access issue associated with incinerator. 5. Most old on-site incinerators cannot be recommissioned due to asbestos-related issues. 6. Funeral home crematoriums lack suitable volume capacity to effectively act as a redundancy for the medical waste incinerator. 7. Waste accumulation presents a higher risk of vermin activity. 72 State Health Business Continuity Plan 3.18 Water Services (including sewerage) 3.18.1 Introduction The BCP covers the provision of water, sewer and storm water services to health care facilities and hospitals, and is enacted when local BCPs fail, or due to problems with the facility provider. 3.18.2 Critical business activities 1. Supply of water and sewerage service to health care facilities through the supply to: a. Fire hydrants and boosters. b. Clean water supply. c. Sewerage services. d. Stormwater drainage. 3.18.3 Prevention and mitigation strategies Local site BCPs MOUs and customer relationship plans with utility provider(s) and alternate suppliers Ensure that capital infrastructure development is in accordance with Redundancy and Disaster Planning in Health Capital Works Programs 2nd Ed. (2010) and AS/NZS 3009 3.18.4 Interdependencies Contractual fulfilment by obligated utility provider(s) Electricity supply to water pumps and boosters 3.18.5 Key contacts and expert advisors Title Area Director, Infrastructure and Facilities Management Organisation Position Landline SMHS Lead Advisor 08 6466 7822 Executive Director, Facilities Management NMHS Expert Advisor 08 9346 3865 Manager, Infrastructure Support CAHS/WNHS Expert Advisor 08 9340 1407 Manager, Capital and Infrastructure WACHS Expert Advisor 08 9223 8555 Manager, Engineering Services FHHS Expert Advisor 08 9431 2467 73 State Health Business Continuity Plan 3.18.6 Water Services (including sewerage) BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA Activity or resource What could cause the loss of the activity or resource? What will the impact be if that activity / resource is not available? See impact table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indefinitely Restoration of reliable potable water supply to hospitals and fire hydrants. Loss of domestic and fresh water supply to multiple health care sites Implement demand management strategies for water (See Appendix 6) Diminished / Lost Renal Dialysis capability 1 Implement demand management strategies for contaminated water (See Appendix 7) Diminished / Lost Laboratory capability Consider hospital evacuation if outage is not restored within 24 hours Diminished / Lost Operating Theatre capability Supply of clean water 3.18.6.1 Fire Hydrants and Booster Supply Catastrophic loss of mains water supply through multiple triggers Contamination of Water Supply Diminished / lost ability to sterilise equipment Hospital Health Coordinators Water Corporation Organise alternate supply of water/liaise with Water Corporation e.g. Water Tankers. DPMU Loss of laundering services Coordinate supply of bottled water. Catering and Linen Contractors Inability to perform infection control procedures Liaise with DFES regarding supply of fire tanks. Relevant Renal Dialysis Stakeholders Inability to maintain patient hygiene standards Truck in/out catering and linen supplies Hire Company Loss of Air-conditioning, loss of steam Organise for haemodialysis to be conducted at alternative venue(s).1 Inability to prepare onsite meals/catering Loss of fire-fighting water supply 5 Immediately DFES Organise portable toilets Inability to perform on-site laundering of linen 74 State Health Business Continuity Plan 3.18.6 Water Services (including sewerage) BCP Number CRITICAL BUSINESS ACTIVITIES TRIGGER TO INVOKE CONTINGENCY IMPACT/ CONSEQUENCE Activity or Resource What could cause the loss of the Activity or Resource? What will the impact be if that activity / resource is not available? IMPACT RATING MAXIMUM ACCEPTABLE OUTAGE STATE-WIDE RESPONSE STRATEGIES RELEVANT STAKEHOLDERS CONTINGENCY OPERATING MAX LENGTH OF TIME NORMAL OPERATING MODE CRITERIA See Impact Table on page 23 Time before an outage threatens achievement of organisational objectives Strategic plans utilised by the State Health Coordinator in response to situation Who to contact in order to facilitate the contingency Once plan is implemented, how long can contingency plan continue for? Criteria that must be met before a business can return to normal work practices Indefinitely Restoration of reliable sewerage network Indefinitely Functional storm water draining network Increased infection risk 3.18.6.2 Sewerage Services Failure of sewerage System from multiple causes Decreased ability to provide catering services Secure chemical toilets, if required. 4 Immediately Reduced ability to sterilise equipment Notification of Environmental Health Directorate. 3.18.6.3 Storm Water Drainage Inability to clear storm water from multiple sites Water Corporation Secure supply of pump trucks, if required. Contact Water Corporation Failure of Storm Water Drainage network Environmental Health Directorate 3 Immediately Coordinate the sourcing of alternative means to clearing water (pumps, channels, drains) Water Corporation SHICC 3.18.7 Notes 1. Refer to the Western Australia Renal Dialysis Business Continuity Plan (2010). 75 State Health Business Continuity Plan Appendices Appendix 1 Protocols for managing blood and blood products in a surge or mass casualty incident in Western Australia Appendix 2 Catering services demand management strategies Appendix 3 Electricity supply demand management strategies Appendix 4 Gas supply demand management strategies Appendix 5 Linen services demand management strategies Appendix 6 Water supply demand management strategies Appendix 7 Contaminated water demand management strategies 76 State Health Business Continuity Plan Appendix 1: Protocols for managing blood and blood products in a surge or mass casualty incident in Western Australia. 1. In a surge or Mass Casualty Incident (MCI), blood and blood products will be prioritised for allocation based on the number of patients and nature of their injuries. 2. When notified of a MCI, Transfusion Medicine Units (TMU) will assess their inventory levels of red cells, clinical fresh frozen plasma, cryoprecipitate, platelets and albumin. 3. Once casualty allocation has commenced, hospitals will be able to assess the number of casualties and the nature of their injuries they are receiving. TMUs of hospitals receiving patients will then be able to commence placing orders with the Blood Service. 4. Orders placed specifically to deal with the MCI casualties are to be highlighted as such on the order forms by the requesting TMUs (i.e. “This request is in response to the XXXX Incident”). 5. The Blood Service Transfusion Medical Specialist will liaise directly with hospital TMUs to determine the type of blood product required based on the nature of patient injuries. 6. In the period between the occurrence of a MCI and the commencement of casualties to hospitals, TMUs will place orders with the Blood Service via the normal BloodNet ordering system. 7. The timing of provision of product will be determined by the location of the incident, the time required for casualties to arrive at the relevant hospitals and for the determination of type of product to be aligned to the patients needs at the receiving hospital (s). 8. In ordering blood, TMUs must consider that the Blood Service will need to: a. Have sufficient time to allow orders to arrive from all the involved hospitals as authorised via SHICC. b. Assess local Blood Services and Approved Health Providers (AHP) inventory and begin the process of importing more from the Blood Service’s national Inventory if required. c. Ensure that there is fair and equitable alignment of blood and blood products to the hospitals concerned based on the information the Blood Service has been given by the SHICC. This will be dependant upon the number of casualties allocated to each hospital and the nature of their injuries. d. The Blood Service’s Medical Services or Transfusion Medicine Specialist on call will be required to consider other requests received for urgent/life threatening blood provision not associated with the Incident. 9. Each TMU are to have this instruction readily accessible. 77 State Health Business Continuity Plan Appendix 2: Catering Services – Demand management strategies Phase Trigger Food Shortages Phase 0 Normal bulk food demand Environmentally friendly practices Business as usual and supply Phase 1 Restriction in menus to meet supply status 25% decrease in bulk food WA Health Recommendations supplies Critical diets (clinical) can still be maintained Phase 2 No-choice menu, Cold meals (Sandwiches) 50% decrease in bulk food WA Health Directives supplies Critical diets (Clinical) can only be fulfilled Phase 3 State Mandated Actions Individual meal packs and shelf stable meals 1 to be provided. 75% decrease in bulk food supplies Prioritisation of critical diets (clinical) Source bulk ration packs from supplier. Phase 4 Commonwealth Interventions Bulk food supplies decrease by more than No fresh meals provided 75% Seek interstate/Federal assistance to fulfil critical diets (clinical) Appendix 2 Notes 1. Shelf stable meals require water for reconstitution 78 State Health Business Continuity Plan Appendix 3: Electricity supply demand management strategies Phase Trigger Phase 0 Environmentally friendly practices General Measures Responsible usage of resources Normal demand and supply Raise staff awareness of environmentally and encourage implementation Continue Phase 0 Recommendations Phase 1 WA Health Recommendations 25% decrease in supply Raise staff awareness of current situation with gas supplies and government initiatives to address the gas supply disruption. EG: regular updates Implement environmentally friendly practices throughout the hospital. Continue preparatory work should phase 2 directives be implemented. Demand management strategies for electricity supply Utilise public affairs to encourage staff to turn off unnecessary lighting and electrical equipment. Utilise thermal blankets to conserve heat overnight in hydrotherapy and swimming pools Utilise power safe modes on all equipment, Utilise one printer/photocopier per area. Turn off non-essential computer and other electrical equipment after hours (printers & photocopiers) Modify air-conditioning arrangements within buildings e.g.: alter static pressure set points to reduce air flow. Reduce airconditioning set points in clinical areas and administrative areas. Switch of unnecessary lighting e.g.: empty meeting rooms and offices, main lighting in wards during the day. Review all power generation infrastructure and diesel fuel levels for readiness. Commence preparatory activities for phase 2 activation Review alternative fuel options for generators Reduce heating in swimming pools to 25°C. Phase 0 and 1 recommendations become directives and must be implemented. Phase 2 WA Health Directives 50% decrease in supply Provide directives to staff on actions to be implemented Continue preparatory work should phase 3 mandates be implemented. De lamp i.e.: remove fluorescent tubes in areas where there is sufficient light without them (corridors, larger offices). Turn off all non-essential lights after hours. Modify air-conditioning arrangements within buildings e.g.: alter static pressure set points to further reduce air flow. Reduce air-conditioning set points further in clinical areas and administrative areas. Turn off all equipment when not in use. Supplement hospital power through co-generation with emergency diesel generators. Restrict showers to second daily and utilise bed bath bags with 1 towel only to conserve energy. Close all non-essential services Phase 3 State Mandated Actions 75% decrease in supply Phase 0, 1 & 2 measures are mandatory Implement and monitor mandatory directives Reduce water temperature settings to minimum level that will maintain flow and return rates above 50°C Cut heating to non-essential swimming pools. Supplement hospital power through co-generation with emergency diesel generators Phase 4 Commonwealth Interventions Greater that 75% decrease in supply Commonwealth Assistance is required Diesel generation of power for essential services only 79 State Health Business Continuity Plan Appendix 4: Gas supply – Demand management strategies Phase Phase 0 Environmentally friendly practices Trigger Normal demand and supply General Measures Responsible usage of resources Raise staff awareness of environmentally friendly practices and encourage implementation Continue Phase 0 Recommendations Phase 1 WA Health 25% decrease in supply Recommendations Raise staff awareness of current situation with gas supplies and government initiatives to address the gas supply disruption. EG: regular updates Implement environmentally friendly practices throughout the hospital. Continue preparatory work should phase 2 directives be implemented. Linen Dry Ice Awareness raising eg: place posters in linen store outlining costs per item to launder and impact of soaps on environment Recycle dry ice as able Conserve linen wherever possible e.g.: change only when soiled, curtains changed only on discharge from isolation wards, one towel per patient, paper towels for examination benches in clinics. Staff to hot wash and iron own uniforms Encourage patients to use their own pyjamas Utilise disposable linen in clinic areas e.g.: paper towel for examination tables Ensure wards and departments are not hoarding linen Recycle dry ice as able Import dry ice from South Australia and Victoria to supplement existing supplies and secure supply to meet medical demand. Review necessity for dry ice and determine priority list for ongoing supply i.e.: clinical use versus research. Consider alternative mediums for transport of specimens. Increase HCN stock levels of disposable linen and attire Phase 0 and 1 recommendations become directives and must be implemented. Phase 2 WA Health Directives 50% decrease in supply Patients supply own nightgowns / pyjamas Reduce amount of linen supplied to areas Provide directives to staff on actions to be implemented Use disposable linen and attire Continue preparatory work should phase 3 mandates be implemented. Restrict the number of blankets per patient (consider using space blankets in addition to 1 blanket) Limit supply of dry ice to clinical areas only Continue sourcing of dry ice from interstate. Use regional hospital laundries for metropolitan linen Phase 3 State Mandated Actions 75% decrease in supply Phase 0, 1 & 2 measures are mandatory Utilise disposable linen and attire Implement and monitor mandatory directives Utilise bed bath bags to reduce linen usage Continue sourcing of dry ice from interstate. Supply priority areas only. Patients to supply own blankets / Doona's Phase 4 Commonwealth Interventions Greater that 75% decrease in supply Commonwealth Assistance is required Metro non-infection linen to be cold washed in the regional hospital laundries Priority areas only to be supplied Metro infectious linen to be transported interstate to be hot-laundered. 80 State Health Business Continuity Plan Appendix 4: Gas supply – Demand management strategies (continued) Phase Trigger Carbon Dioxide Normal demand and supply Minimise Wastage Phase 0 Environmentally friendly practices BOC is procuring additional CO2 from South Australia and Victoria. WA Health Recommendations 25% decrease in supply Review CO2 clinical usage versus research usage to determine priority list for supply of CO2. Monitor impact on bone and tissue banks CO2 supplies restricted to clinical usage only Phase 2 WA Health Directives 50% decrease in supply Utilise public to highlight lighting costs to encourage staff to turn off unnecessary lighting and electrical equipment. Oxygen Business as usual Utilise thermal blankets to conserve heat overnight in hydrotherapy and swimming pools Monitor consumption and supplies. Phase 1 Power Supply of CO2 to Bone and Tissue Banks is to be restricted to WA usage. Interstate transfers of bone and tissue will need to be reviewed. Utilise power safe modes on all equipment, Utilise one printer/photocopier per area. Turn off nonessential computer and other electrical equipment after hours (printers & photocopiers) Modify air-conditioning arrangements within buildings e.g.: alter static pressure set points to reduce air flow. Reduce air-conditioning set points in clinical areas and administrative areas. Switch of unnecessary lighting e.g.: empty meeting rooms and offices, main lighting in wards during the day. Review all power generation infrastructure and diesel fuel levels for readiness. Commence preparatory activities for phase 2 activation Review alternative fuel options for generators BOC gases reclassified as tier 2 supplier by Office of Energy to secure supply of O2 Hospitals to monitor supplies. HCN to review alternative suppliers from interstate. Identify O2 usage in clinical versus research. Reduce heating in swimming pools to 25°C. De lamp i.e.: remove fluorescent tubes in areas where there is sufficient light without them (corridors, larger offices). Turn off all non-essential lights after hours. Modify air-conditioning arrangements within buildings e.g.: alter static pressure set points to further reduce air flow. Reduce air-conditioning set points further clinical areas and administrative areas. Continue phase 1 implementations. Turn off all equipment when not in use. Procure O2 from Interstate. Supplement hospital power through co-generation with emergency diesel generators. Restrict showers to second daily and utilise bed bath bags with 1 towel only to conserve energy. Phase 3 State Mandated Actions 75% decrease in supply Supply of priority clinical areas only. Review and prioritise bone and tissue graft surgery within WA. Close all non-essential services Reduce water temperature settings to minimum level that will maintain flow and return rates above 50°C Cut heating to non-essential swimming pools. Supplement hospital power through co-generation with emergency diesel generators Phase 4 Commonwealth Interventions Greater that 75% decrease in supply Cease elective surgical procedures requiring CO2. Continue phase 1 & 2 implementations. Procure O2 from Interstate. Implement usage of O2 concentrators in clinical areas. Procure O2 from interstate. Diesel generation of power for essential services only Continue use of O2 concentrators 81 State Health Business Continuity Plan Appendix 4: Gas supply – Demand management strategies (continued) Phase Trigger Boilers Clinical Service Delivery Food Supply Normal demand and supply Business as usual Business as usual Business as usual Phase 0 Environmentally friendly practices Identify boiler usage i.e. sterilising, steam production, heating, hot water supply, kitchen usage. Phase 1 WA Health Recommendations 25% decrease in supply Reduce water temperature settings. Ensure reduced setting does not allow flow and return temperatures to fall below 55°C. Educate patients to reduce showering times to 4 minutes maximum. Commence preparatory work on prioritising elective surgery procedures to be continued if gas supply is further disrupted Review impact of Gas disruption on hospital food supplier. Advise WA Health of any supply disruption issues. Turn off continuous hot water supplies in non-essential areas overnight. Restriction of patient showers to 4 minutes second daily to conserve energy. Phase 2 WA Health Directives 50% decrease in supply Implement reductions in elective surgical procedures Reduce water temperature settings. Ensure reduced setting does not allow flow and return temperatures to fall below 53°C. Phase 3 State Mandated Actions Prioritisation of equipment for sterilisation. Review perishable goods usage and change food availability accordingly No-choice menu, Cold meals (Sandwiches) Further reduction in sterilising related to surgery. 75% decrease in supply Reduce water temperature settings to minimum level that will maintain flow and return temperatures above 50°C. Emergency Surgery Only Cold food, Individual meal packs and shelf stable meals to be provided. Cease all surgery unless equipment is chemically sterilised. Utilise Ration Packs Phase 4 Commonwealth Interventions Greater that 75% decrease in supply Surgery with chemical sterilisation of instruments only. 82 State Health Business Continuity Plan Appendix 4: Gas supply – Demand management strategies (continued) Phase Trigger Research Capital Works Medico-Legal Normal demand and supply Business as usual Business as usual Business as usual Review all research being undertaken to determine necessity to continue Monitor impact of gas disruption on capital works program Monitor and report clinical indicators e.g.: infection control, patient complaints, standards of care. Phase 0 Environmentally friendly practices Phase 1 WA Health Recommendations Up to 25% decrease in gas supply Identify measures to minimise impact on research if gas supply is further disrupted Report any delays to DPMU Monitor and report clinical indicators e.g.: infection control, patient complaints, and standards of care. Phase 2 WA Health Directives Up to 50% decrease in gas supply Clinical trials only to be continued Phase 3 State Mandated Actions Phase 4 Commonwealth Interventions DPMU to advise medico-legal department of potential issues Review necessity to continue capital works Capital Works Ceased Up to 75% decrease in gas supply Cease all research Greater that 75% decrease in gas supply Maintain cessation of all research until full power has been restored Maintenance functions only continue Cease all capital works until full power has been restored 5% increase in any clinical indicator to be reported to DPMU Monitor and report clinical indicators eg: infection control, patient complaints, and standards of care. 10% increase in any clinical indicator to be reported to DPMU Monitor and report clinical indicators e.g.: infection control, patient complaints, and standards of care. Clinical indicators to be reported to DPMU 83 State Health Business Continuity Plan Appendix 5: Linen Supply – Demand management strategies Phase Phase 0 Trigger Environmentally friendly practices Normal Demand and Supply Linen Awareness raising e.g.: place posters in linen store outlining costs per item to launder and impact of soaps on environment Conserve linen wherever possible e.g.: change only when soiled, curtains changed only on discharge from isolation wards, one towel per patient, paper towels for examination benches in clinics. Staff to hot wash and iron own uniforms Phase 1 Up to 25% increase in demand or WA Health Recommendations supply Encourage patients to use their own pyjamas Utilise disposable linen in clinic areas e.g.: paper towel for examination tables Ensure wards and departments are not hoarding linen Increase HCN stock levels of disposable linen and attire Patients supply own nightgowns / pyjamas Phase 2 Up to 50% increase in demand or WA Health Directives supply Reduce amount of linen supplied to areas Use disposable linen and attire Restrict the numbers of blankets per patient (consider using space blankets in addition to 1 blanket) Use regional hospital laundries for metropolitan linen Phase 3 Up to 75% increase in demand or State Mandated Actions supply Utilise disposable linen and attire Utilise bed bath bags to reduce linen usage Patients to supply own blankets / Doona's Phase 4 Demand levels increase by more Commonwealth Interventions than 75% Metro non-infection linen to be cold washed in the regional hospital laundries Metro infectious linen to be transported interstate to be hot-laundered. 84 State Health Business Continuity Plan Appendix 6: Water Services Demand Management Strategies Phase Water Trigger Phase 0 Environmentally friendly practices Normal demand and supply Business as usual Dialysis ● Prioritise patients who requiring dialysis ● Medically manage patients requiring non-urgent dialysis ● Refer renal dialysis patients to alternative renal dialysis units Theatres: ● Cancel all non-elective surgery ● Sterilise equipment at alternative site or through external contractor Phase 1 WA Health Recommendations 24 – 72 hours of water remaining Hygiene: ● No shower, baths or hair washing ● Bed Bath with sanitary wipes only ● Use washing bowl with water for soiled patients only ● Organise portable toilet facilities through external contractors Linen: ● Change only soiled bed linen, reuse towels ● Launder linen off-site through contractors or MOUs ● Utilise disposable linen from DPMU Strategic supply Infection control: ● Use water and soap only to clean soiled hands Catering: ● Utilise processed and pre-prepared foods only (tins, packets) ● Distribute bottled water ● Organise alternative catering arrangements through external contractor or supplier Fire Fighting: ● Organise bulk water tanks / trucks ● Increase portable fire extinguisher capacity Laboratory: ● Process only urgent blood samples ● Divert all non-urgent blood samples to alternative locations General Nursing: ● Use sterilised/bottled water for essential patient cleaning requirements ● Ask staff to organise meals and drinks that do not require scheme water Air-Conditioning: ● Turn off all air-conditioning All interventions as above, plus: Renal: ● Emergency renal dialysis only Phase 2 WA Health Directives < 24 hours water supply remaining Theatres ● Scrub hands with sterilised bottled water Consider preparations for the evacuation of the hospital Infection control: ● Utilise alcohol gels to clean hands ● Use water and soap only to clean soiled hands ● Discharge cleaning with alcohol wipes all interventions as above, plus: Phase 3 State Mandated Actions No Water Supply Laboratory Arterial Blood Gas Sampling only Commence the orderly evacuation of the hospital Air-Conditioning: ● Turn off all air-conditioning 85 State Health Business Continuity Plan Appendix 7: Contaminated Water – Demand Management Strategies ● Maintain hand hygiene with alcohol hand rub Phase 1 WA Department of Health Recommendations ● Where appropriate consider surface cleaning with other methods Contaminated Water ● No showers or baths ● No hair washing ● Bed Bath with sanitary wipes only ● Trucking clean water to the site ● Deploy large clean water containers to patient care areas 86 This document can be made available in alternative formats on request for a person with a disability. © Department of Health 2012