Diet and bone health
advertisement

Diet and bone health A Vegan Society briefing paper Stephen Walsh January 2002 Overview Calcium is essential to life. The body acts to keep calcium levels in the blood within a very narrow range by regulating absorption of calcium from the gut and from bone, and to a lesser extent by regulating losses of calcium in urine. Unfortunately, these regulating mechanisms do not adequately preserve bone in older people in developed countries. Measures to promote bone health are important throughout life to assist in building bone and to reduce later losses of bone. In all developed countries with ageing populations, thinning of bones due to loss of calcium is a major public health issue. As bones thin, risk of fracture increases. Hip fracture is a particularly devastating injury, with many people dying within a year of suffering such a fracture. Osteoporosis and vertebral fractures give rise to the familiar loss of height with age and to the painfully familiar bent over stance of many elderly people. Preventing such fractures is one of the most important public health issues for the 21st century, as populations across the world grow older and more prosperous. There are three main approaches to tackling this problem: drugs, diet and lifestyle. This paper will consider diet and, to a lesser extent, physical activity and sun exposure. Dietary recommendations have focussed almost exclusively on increasing calcium intake. Increasing calcium intake is not wrong in itself but, in relation to bone health, its undue pre-eminence over reducing sodium intake, increasing vitamin K and potassium intakes, moderating protein intake, increasing physical activity and adequate sun exposure is a serious error in public policy. There are five components to promoting bone health through diet: providing the ingredients of bone (protein, phosphorus and calcium); reducing calcium losses from the body; making absorption of calcium from the gut easy; making absorption of calcium from bone difficult; promoting bone strength independently of bone mass. Providing the ingredients of bone (protein, phosphorus and calcium) About 1.0 g of protein per kg of body weight per day is widely accepted as an adequate intake for most people over the age of 10, though athletes may require about 1.5 g per kg per day. About 1.25 g of phosphorus per day is also widely accepted as an adequate intake for most people. Most people in developed countries get adequate protein and phosphate, though some elderly individuals do not. Elderly people may need to emphasise foods rich in these nutrients as their calorie consumption declines. Calcium intakes of 800-1500 mg per day are considered adequate by various expert bodies. However, calcium requirements cannot be considered separately from other dietary components, particularly those determining calcium losses. Reducing calcium losses from the body Calcium is lost from the body in urine, gut secretions and sweat. The key to avoiding bone loss is to ensure that calcium absorbed from food in the gut balances the losses. Otherwise, the body will take calcium from bone to maintain the required level of calcium in the blood. The body contains about 1 kg of calcium in the bones. If calcium losses exceed absorption from the gut by just 30 mg per day, 1% of the calcium in the bones will be lost each year. In people following typical North American and European diets, calcium loss is driven with approximately equal importance by four dietary components: high sodium, high protein, low potassium and low bicarbonate intakes. Increasing sodium intake from 1000 to 4000 mg per day causes an additional 52 mg of calcium loss per day. Increasing protein intake from 40 to 100 g per day increases losses by 66 mg per day. Decreasing potassium intake from 8000 to 2000 mg per day increases losses by 31 mg per day. Decreasing bicarbonate intake from 100 to 20 mmol per day increases losses by 32 mg per day. These entirely plausible changes in daily intake of the four key components can therefore cause calcium losses from the body to increase from about 60 mg per day to about 240 mg per day. Fractional calcium absorption (the fraction of dietary calcium absorbed from the gut) decreases as calcium intake increases, so each successive increase in calcium intake has less effect. For a typical 55 year old woman, the required calcium intake to meet 60 mg per day of losses would be just 200 mg per day, while the required intake to meet losses of 240 mg per day would be 2300 mg per day. Appendix 1 explains the calculation of these figures. In children, adolescents and younger adults, calcium absorption is more efficient and adapts better to increased losses. In these groups the beneficial effect of increasing calcium intake on calcium balance is stronger, due to better average absorption, and the adverse effect of increased losses is less, due to better adaptation of absorption to increased losses. Older men and older women show a decline in absorption (Institute of Medicine, 1997; Agnusdei, 1998; Barger-Lux, 1995), with average fractional calcium absorption being about 30-40% lower at eighty than at thirty. In this briefing paper the analysis will focus on adults with an average age of about 55. Any diet adequate to support bone health in older adults will be adequate for younger people, but in the very old reducing calcium losses will be even more important than this analysis indicates, as calcium absorption will be lower. Calcium requirements to balance a given calcium loss will also be higher for those with relatively low calcium absorption for their age. Such individuals are at particularly high risk of osteoporosis (Need, 1998; Ensrud, 2000). About one in ten postmenopausal women show absorption more than 40% below the average (Heaney, 1986) and are therefore at particularly high risk of bone loss. As already noted, the fraction of calcium absorbed also declines as overall calcium intake increases. A useful way of examining foods is to evaluate their net impact on calcium balance (calcium absorbed from the gut minus calcium losses) at a given level of calcium intake. To fully appreciate the impact of a food on high risk individuals its effect should be evaluated with calcium absorption 40% below typical levels. Table 1 shows the effect of some representative foods on calcium balance, in mg of calcium per 100 g of food, at calcium intakes between 500 and 1000 mg per day and between 1000 and 1500 mg per day, both for typical calcium absorption and for 40% reduced absorption (high risk). Chicken (average) Fish (average) Eggs Cottage cheese Feta cheese Cheddar cheese Cow's milk Wheat grain (dry) Brown rice (dry) Chickpeas (dry) Soybeans (dry) Almonds Peanuts Potatoes Peppers Oranges Bananas Kale Spring greens Normal absorption 40% reduced absorption 500-1000 mg 1000-1500mg 500-1000 mg 1000-1500 mg calcium intake calcium intake (high risk) (high risk) -27.3 -27.6 -27.8 -28.0 -23.6 -24.3 -24.9 -25.3 -18.2 -19.5 -20.7 -21.5 -15.6 -16.8 -18.0 -18.7 12.5 2.4 -6.9 -12.9 18.6 7.0 -3.7 -10.7 8.5 6.1 3.8 2.3 -11.6 -12.2 -12.8 -13.2 -7.1 -7.6 -8.0 -8.3 -6.1 -6.4 -6.7 -6.9 6.6 2.4 -1.6 -4.1 14.8 9.7 5.0 1.9 -6.6 -8.0 -9.3 -10.1 1.8 1.6 1.3 1.2 2.6 2.4 2.2 2.1 5.6 4.8 4.0 3.5 4.6 4.5 4.4 4.3 17.6 14.5 11.7 9.9 20.7 16.4 12.4 9.8 Table 1: Effect of representative foods on calcium balance Foods can be categorised based on whether they are high or low in calcium and whether they increase or decrease calcium losses. The ideal foods for bone health are foods that are high in calcium and reduce calcium losses. Adding these foods to the diet will benefit everyone, including those requiring high calcium intakes and having low absorption. Green leafy vegetables such as kale and spring greens are the best example of such foods. In contrast, all dairy foods increase losses of calcium as well as providing calcium, so their effectiveness declines dramatically with increased calcium intakes and with decreased absorption. Foods such as meat, fish and eggs, which are low in calcium but cause high losses, reduce everyone’s calcium balance uniformly, while low calcium foods which reduce losses, such as peppers, bananas and oranges, provide everyone with a modest boost. For an individual trying to improve calcium balance, fruit and vegetables are the best foods to add, as they are rich in potassium and bicarbonate which reduce calcium losses. Adding 100 g of each of the five vegetables and fruits at the bottom of Table 1 would add 400 mg of calcium to the diet and 30 to 35 mg to the calcium balance of a high risk person with low absorption, or 40 to 50 mg for a person with typical absorption. In contrast, a pint of cow’s milk would add about 700 mg of calcium to the diet, but would improve calcium balance by only 13 to 22 mg and 35 to 50 mg respectively. 100 g of cheddar cheese would also add 700 mg of calcium to the diet, but would actually take away 11 to 4 mg of calcium from the high risk person while adding only 7 to 19 mg to calcium balance for the person with average risk. In all cases, the benefit is less at higher calcium intakes. More calcium is a good thing, but the package it comes in is critical, particularly for individuals at high risk. Although increased protein intake increases calcium losses, an adequate protein intake is essential to provide the ingredients for muscle and bone, without which the body will degenerate. Consuming less than the recommended amount of protein in order to reduce calcium loss is therefore a false economy. However, the choice of protein source can make a great deal of difference. A person trying to increase protein intake using chicken or fish will lose 25 mg of calcium from their body for every 100 g eaten. In contrast, a 100 g portion of beans (by dry weight) has an approximately neutral effect on calcium balance while providing the same amount of protein. Reducing salt intake by 5 g per day will eliminate 2000 mg of sodium, reducing calcium losses by about 35 mg per day. Reducing sodium intake; increasing potassium and bicarbonate intake from fruit and vegetables; meeting protein needs from legumes rather than meat, fish or egg; and getting calcium from green leafy vegetables rather than dairy products can reduce the losses of calcium from the body substantially. As already noted, if calcium losses exceed calcium absorption by just 30 mg per day about 1% of bone calcium will be lost each year. Reducing calcium losses while consuming ample calcium (about 1000 mg per day) provides a robust foundation for bone health by making it easier for the body to replenish its losses from the diet. Making absorption of calcium from the gut easy Faced with a given calcium loss, the body will try to maintain calcium levels in the blood by taking calcium from the gut or from bone. If calcium is readily available from food in the gut, the body is less likely to remove it from bone, so bone loss will be less. The body maintains blood levels of calcium primarily by adjusting parathyroid hormone (PTH). Increased PTH increases the production of calcitriol from calcidiol (stored vitamin D) as well as directly stimulating removal of calcium from bone. Calcitriol stimulates absorption of calcium both from the gut and from bone. Calcidiol has similar effects to calcitriol, though these effects are weaker at normal concentrations. If calcium intake is sufficient to meet calcium losses with a low fractional calcium absorption and vitamin D is adequate, the body will show low PTH, moderate to high calcidiol and low calcitriol. This combination favours calcium being taken from the gut rather than from bone and indicates ideal calcium metabolism. If vitamin D is adequate but calcium intake is not ample, the body will show moderate PTH, moderate to high calcidiol and high calcitriol. This is undesirable as calcium is likely to be absorbed from bone as well as from the gut and bone loss may be significant. If vitamin D is inadequate, the body will show high PTH, low calcidiol and low calcitriol. In this case, calcium will be lost from bone. Severely inadequate vitamin D levels manifest as rickets in children and as osteomalacia in adults. Severe magnesium deficiency impairs calcium absorption from the gut (Sojka, 1995). Magnesium is abundant in unrefined plant foods, including whole grains. Caffeine reduces absorption of calcium from the gut. One cup of caffeine-containing coffee per day reduces calcium balance by about 4 mg (Barger-Lux, 1995b). This is a very significant reduction in older adults, leading to about 0.1% loss of bone per year if not compensated for by some other means. Optimal bone health requires adequate stored vitamin D (calcidiol) and magnesium combined with sufficient calcium intake to allow calcium losses to be met from the gut even with a low fractional absorption. Making absorption of calcium from bone difficult The other side of ensuring that calcium comes from the gut and not from bone is making bone resistant to calcium loss. When the body demands more calcium to balance losses, by raising PTH and calcitriol, both the gut and the bone will respond. Making it easy to absorb calcium from the gut helps to protect bone. Helping bone to resist demands for more calcium is just as important. Bone is built by osteoblast cells and demolished by osteoclast cells in an ongoing cycle of renewal and repair. Strengthening osteoblast activity relative to osteoclast activity makes bone more resistant to demands for release of calcium to the blood. Increased resistance means that more of the calcium losses will be met by absorption from the gut and less by absorption from bone. During childhood and adolescence, growth hormones strongly stimulate osteoblast activity, promoting a positive calcium balance. Growth hormones decline with age. Particularly severe declines in bone growth hormones occur if dietary protein, phosphate or zinc become inadequate. Oestrogen levels also decline with age in both men and women, with a particularly dramatic drop in women at menopause. Oestrogen promotes a positive calcium balance in many ways, including making bone more resistant to releasing calcium in response to increased PTH, reducing urinary calcium loss and possibly increasing calcium absorption (Nordin, 1999; Riggs, 1998). These age-related changes shift the balance in favour of osteoclast activity with age, making bone loss in response to calcium losses more likely. A key component of bone is osteocalcin, a protein produced by osteoblasts. Osteocalcin must be carboxylated to bind most effectively with calcium. Elevated undercarboxylated osteocalcin (ucOC) strongly predicts fracture risk and is associated with both decreased bone density and weaker bones at a given density (Weber, 2001). Elevated ucOC can be readily corrected by increased vitamin K intake. Vitamin K is found in large quantities in green leafy vegetables and broccoli and in the fermented soy product, natto. Absorption of vitamin K from green leafy vegetables is enhanced by the presence of fat, e.g. from a salad dressing, cooking oil or other accompanying food. Booth (2000) found high vitamin K intake (250 micrograms per day) to be associated with a 65% reduction in fracture risk. 250 micrograms of vitamin K can be obtained from 100 g of broccoli or green cabbage, 200 g of lettuce or just 40 g of kale (Shearer, 1996). The beneficial effect of vitamin K is particularly notable in postmenopausal women who are not receiving oestrogen treatment, suggesting that it counters some of the adverse effects of declining oestrogen levels (Feskanich, 1999). In those postmenopausal women showing particularly high calcium losses a 1000 microgram vitamin K supplement resulted in a marked reduction in urinary calcium losses (Knapen, 1989). A 1000 microgram supplement is equivalent to about 150 g of kale. Vitamin K may also be important, together with ample calcium intake, in ensuring a beneficial impact of increased levels of vitamin D (Feskanich, 1999). Blood pH is also a significant factor in osteoblast and osteoclast activity. As pH drops, the balance is shifted in favour of osteoclasts and bone density declines (Bushinsky, 2000; Giannini, 1998). Blood pH decreases with age, as kidney efficiency declines, and is sensitive to the balance between acid and bicarbonate from the diet (Sebastian, 1994; Frassetto, 1996). Consuming alkaline foods (typically high in potassium relative to protein) increases blood pH, thereby shifting the balance in favour of the osteoblasts. However, low protein diets have the opposite effect as they cause a decline in growth hormones. It is therefore very important to maintain adequate protein intakes while using plenty of alkaline foods such as fruits and vegetables to balance the acid from the protein. Vegetable sources of protein (other than grains and some nuts) are usually alkaline, while animal sources of protein are usually acid. Milk is approximately neutral, but cheese is even more acid than meat or fish. Table 2 shows the contribution of different types of food to net alkali. For the detail of the calculation of net alkali see Appendix 1. Acid foods show a negative value for net alkali. net alkali (mmol) Chicken (average) fish (average) Eggs cottage cheese feta cheese Cheddar cheese cow's milk wheat grain (dry) brown rice (dry) chickpeas (dry) soybeans (dry) Almonds Peanuts potatoes Peppers Oranges bananas Kale spring greens -11.1 -8.7 -10.8 -8.1 -13.3 -21.6 -0.3 -8.3 -10.3 0.0 12.2 2.5 -1.1 5.3 3.6 3.8 6.9 9.1 4.1 Table 2: The effect of representative foods on net alkali Retinol consumption probably has an adverse effect in older adults by stimulating release of calcium from bone and also by interfering with absorption of calcium from the gut (Binkley, 2000; Johansson, 2001). Major studies in both Scandinavia and the USA have linked retinol intakes above 1500 micrograms per day with an almost doubled risk of hip fracture compared with retinol intakes below 500 micrograms per day (Melhus, 1998, Feskanich, 2002). Both studies found that plant carotenes, from which the body can make its own vitamin A as required, were not associated with increased risk. Retinol is found in animal products, particularly liver and cod liver oil. It is also found in some fortified foods, including most milk sold in Sweden and the USA, and many multivitamin supplements. Plant carotenes are abundant in carrots, dark green leafy vegetables and red peppers. Vitamin C promotes the formation of osteoblast-derived proteins required in bone. Omega-3 fatty acids may have a positive effect in shifting the balance in favour of osteoblasts (Kruger, 1998; Requirand, 2000; Watkins, 2001). Physical activity has a huge impact in promoting osteoblast activity, thus encouraging the body to take the necessary calcium from the gut rather than the bones. For a given dietary intake, greater physical activity such as walking, running, racket sports and weight training will promote the development and retention of bone (Uusi-Rasi, 1998; Wolff, 1999). In the face of high physical activity, the body will follow the path of least resistance and take extra calcium from the gut rather than from bone. The optimal combination is a diet requiring a relatively low fractional absorption of calcium to balance losses and a combination of physical activity and dietary factors promoting osteoblast activity so as to make the bones resistant to the body’s demands for calcium. Promoting bone strength independently of bone mass Bone mass is not the end of the story. A large, dense bone is usually a strong bone, but is not necessarily so. As discussed above, increased vitamin K intake is associated with reduced fracture risk independent of bone density. Magnesium in bone promotes a fine crystalline structure and greater bone strength, so ample magnesium intake may enhance bone strength (Sojka, 1995). Recommendations Eat plenty of low oxalate high calcium green leafy vegetables Dairy products are not the ideal food for bone health. 100 g of a low oxalate high calcium green leafy vegetable such as kale, turnip greens or spring greens (young cabbage without a heart) will have at least as much beneficial effect on calcium balance as 200 g of milk or 100 g of cheddar cheese. Using the green stuff instead of the white stuff avoids the adverse effects of dairy fat on cardiovascular health. Dark green leafy vegetables will also protect and strengthen bone by raising blood pH and providing vitamin K and vitamin C. They are a good source of plant carotenes which meet the body’s needs for vitamin A safely and naturally. Green leafy vegetables are also high in folate, which is very beneficial to general health. It is hard to imagine a food more supportive of bone health than kale or spring greens. Some vegetables such as spinach, beet greens, purslane, amaranth and rhubarb are high in oxalate, which hinders absorption of their calcium. Use of these foods is not harmful to bone, but their effective calcium content is only about 20% of the measured content. Reduce sodium intake If you use salt, substitute one of the widely available low sodium alternatives containing at least twice as much potassium as sodium by weight. Anyone relying on iodised salt as a source of iodine should take a 150 microgram iodine supplement three times a week if the low sodium substitute does not provide iodine. Use low sodium bread or consume bread moderately, as bread is a major source of sodium. Some low sodium breads are also fortified with calcium. Use herbs and spices instead of salt and salty pickles. There are often similar products in terms of taste with very different salt levels. Get at least 600 mg of calcium per day from calcium rich foods or supplements Kale and spring greens provide about 150 mg of calcium per 100 g raw weight. Almonds, carob and molasses each provide about 250 mg of calcium per 100 g. While these foods are too concentrated to consume in large amounts, they can make a useful contribution. These sources of plant calcium also provide alkali to boost blood pH. In contrast, milk is neutral and cheese is acid. Tofu is high in calcium only if calcium has been used in preparing it. Some tofu is highly salted. Tofu can therefore vary from substantially increasing calcium balance to substantially decreasing it. The calcium content of tahini is also very variable, ranging from 140 to 960 mg per 100 g. The amounts of calcium and sodium in these foods should be checked on the labels and not taken for granted. There should be at least as much calcium as sodium for a beneficial effect on calcium balance. Calcium-fortified foods or calcium supplements provide another source of calcium. Calcium supplements are at least as natural as dairy products or soy products as humans have consumed calcium carbonate, introduced via stone grinding of grain, for about 10,000 years. If phosphate intakes are low (unusual for vegans), calcium phosphate may be preferable to calcium carbonate or calcium citrate. Calcium carbonate should always be consumed with meals. If stomach acid is low something other than carbonate should be used. 600 mg of calcium per day from calcium rich foods, plus calcium from other foods, should give an adequate calcium intake. Get an adequate protein intake This is mainly an issue for elderly people and others with a relatively low calorie intake (less than 30 kcal per kg of body weight), but can be of critical importance. If protein intake is inadequate, the body lacks the building blocks for muscle and bone, and growth hormones which stimulate muscle and bone building will decline to undesirable levels. A cup (250 ml) of soya milk a day provides about 8g of protein and can make a significant contribution to maintaining an adequate protein intake. Most dry beans contain about 25 g of protein per 100 g. Wheat is higher in protein than rice and potatoes, and using nuts and seeds rather than oils and fats will boost protein intake. Nuts which are high in monounsaturated fat, such as almonds, hazelnuts (filberts) and cashews, are ideal as they will also promote cardiovascular health. Almonds are the most beneficial for bone health as they have the most positive effect on calcium balance. Maintain an adequate store of vitamin D Get frequent short exposures of skin to sun whenever the sun is at least 30 degrees above the horizon. At latitudes above about 50 degrees North, this is not practical from November to March, and vitamin D stores will decay substantially during this “vitamin D winter”. Within 30 degrees of the equator there is no vitamin D winter. A fifteen minute exposure to sun is ample to boost vitamin D while avoiding damaging sunburn. For the part of the year when such sun exposure is not possible, do one of the following: take a mid-winter holiday somewhere sunny and expose skin to sun frequently; use a sunlamp with at least 3% of its energy between 290 nanometres and 315 nanometres once a week, being careful to avoid overexposure; take 10 micrograms of vitamin D2 (ergocalciferol) per day. Make unrefined plant foods your main source of protein Legume and dairy proteins have a lower sulphur amino acid content (the active component in causing calcium loss) per gram of protein than meat, fish, egg or grain proteins, and therefore cause less calcium loss for a given protein intake. Meat, fish and eggs have a pronounced negative effect on calcium balance. Grains have a moderately negative effect. Some highly processed plant protein sources, such as certain soy protein isolates, have an adverse effect on calcium balance due to loss of beneficial minerals and addition of sodium during processing. Highly salted nuts also have an adverse effect. Of the animal protein sources, only milk and yoghurt can be expected to have a consistently positive effect on calcium balance. Most plant protein sources (fruits, vegetables, legumes and many nuts and seeds) come in a nutritional package which has a positive or neutral effect on calcium balance. Unrefined plant foods are also excellent sources of magnesium. Eat plenty of vegetables and fruit Vegetables and fruit promote bone health by improving calcium balance, providing plentiful vitamin C, and raising blood pH. Several recent studies have shown that increased fruit and vegetable intake is associated with increased bone mineral density and decreased loss of bone (Tucker, 1999; New, 2000). Include omega-3 fatty acids in your diet These probably promote osteoblast (bone-building) activity. The simplest way for vegans to top up omega-3s is to consume 1-2 teaspoons of flaxseed oil per day. Limit caffeine consumption Caffeine has been shown to reduce calcium absorption. Low caffeine teas, such as Redbush (Rooibosch), provide a tasty and healthful alternative. Get your vitamin A from plant carotenes, not from retinol This allows the body to regulate production of vitamin A and avoids the probable ill effects of retinol on bone. Note that cow’s milk is fortified with retinol in Sweden, the USA and some other countries. Some vegan supplements contain retinol or related compounds – ingredients beginning with “retin” should be avoided. Good sources of plant carotenes include carrots, pumpkin, sweet potato, dark green leafy vegetables, such as kale, spring greens and spinach, and red peppers. 100 grams per day of any combination of these will meet vitamin A requirements safely and naturally. Finally, don’t forget physical activity: just as exercise helps to build and maintain muscle, it also helps to build and maintain bone Recommendations on any health issue need to be consistent with overall health. Increased potassium and calcium intakes and reduced sodium intake strongly promote lower blood pressure and reduced risk of stroke and kidney disease. Increased calcium or vitamin D appears to reduce risk of colorectal cancer and may also reduce risk of breast cancer. Increased vitamin D may also reduce the risk of prostate cancer and auto-immune diseases. However, there is a consistent association between increased milk consumption and increased risk of prostate cancer. Giovannucci (1998) suggested that this association may reflect, at least in part, an adverse effect of calcium. The main evidence for this suggestion was that high use of calcium from supplements (more than 900 mg per day) was associated with an increased risk of prostate cancer even at moderate intakes of dietary calcium. Use of calcium supplements providing 1-900 mg per day, with dietary calcium intakes below 1000 mg per day, was associated with a very modest decrease in risk which may have been due to chance. Looking at combined dietary and supplementary calcium, a significant increase in risk (200% greater than for low calcium intakes) was observed only for total calcium intakes above 2000 mg per day. As discussed in Appendix 2, calcium intakes above 2000 mg may have adverse effects even from the point of view of bone health. The recommendations in this paper aim for a calcium intake of about 1000 mg, so the results of Giovannucci give no cause for concern. The Vegan Society briefing paper on Milk and Breast Cancer, produced in November 2001, provides further information on milk and cancer ( www.vegansociety.com/briefings/milkbreastcancer.htm ). Increased consumption of foods rich in plant carotenes is associated with reduced risk of cancer. Increased consumption of omega-3 fatty acids, particularly from plant sources, is strongly associated with reduced risk of heart disease. Omega-3 fatty acids may also reduce risk of depression and schizophrenia. Increased consumption of unrefined plant foods, particularly fruit and vegetables, nuts, seeds and whole grains, is associated with wide-ranging health benefits and can be expected to promote a longer and healthier life. Two serious errors in public policy on bone health Having set out the basis of bone health, it is appropriate to reflect on public policy. The first serious error in public policy is the undeserved pre-eminence accorded to calcium in relation to bone health. Calcium is a very good thing, but increasing calcium intake from 500 mg per day to 1500 mg per day will add less than 90 mg per day to the calcium balance of most older adults, and less than 50 mg per day to the calcium balance of many such adults. 10 g of salt per day will take about 70 mg per day away from calcium balance. 4000 mg of extra potassium from a diet rich in vegetables, fruits and other unrefined plant foods will add 60 mg per day to calcium balance. At the same time, the alkali from such foods will help bone keep its calcium where it belongs. Vitamin K from green leafy vegetables and broccoli will do the same and promote stronger bones at the same time. The second serious error is equating calcium with dairy products. Dairy products are not the best source of calcium as they promote calcium losses at the same time as increasing calcium intake. This is particularly true of cheese, which will degrade the calcium balance of individuals most at risk of osteoporosis: the very old and people with relatively poor absorption of calcium. In terms of bone health, dairy products fortified with retinol are a poisoned offering. Heaney (2000d) provides a particularly clear illustration of the current tendency to equate calcium with dairy: In general, antidairy groups are forced logically to take an anticalcium stance (not just an antidairy stance). Since in the diets of the industrialized nations 65-80% of calcium intake comes from dairy products to be against dairy forces one to be against calcium. Yet in the same article Heaney states: It is now fairly generally accepted that the diets of evolving hominids exhibited high calcium densities. Both nonhuman primates today and contemporary hunter-gatherer peoples regularly consume diets with calcium densities above 2 mmol/100 kcal [2000 mg per day]. Much of this calcium would have come from vegetable sources… In fact, the most authoritative source (Eaton, 1991) states that about 90% of that high calcium intake came from plants. A high intake of vegetables, fruits, roots and flowers also provided abundant potassium, alkali, magnesium, vitamin K and vitamin C, all in quantities far above modern norms. Salt was notably absent. Nutritional science is in its infancy with regard to the interactions between these nutrients, but it is clear that all of them, not just calcium, contribute to bone health and other aspects of health. While many modern cultivated foods are sadly much less rich in calcium than the wild plants with which we evolved, green leafy vegetables are an exception and therefore of particular importance for modern humans. Human use of dairy products is a recent and unnecessary development. A diet rich in vegetables, fruits and root crops provides the best path back to healthy bones. Appendices The appendices to this paper provide important supporting material. Appendix 1 sets out the model used for evaluating calcium balance. This is a novel synthesis of research results over the past twenty years. This appendix underpins the conclusions of the paper. Appendix 2 reviews the evidence from long term supplementation trials with calcium or vitamin D and concludes that the evidence for a beneficial effect on bone health from increased calcium intakes, not exceeding 2000 mg per day, is very strong. This review provides additional support for the recommendations to include at least 600 mg per day of calcium from calcium-rich foods or supplements and to ensure an adequate store of vitamin D. Appendix 3 reviews the results of prospective epidemiological studies on dietary calcium and bone health, with particular emphasis on Feskanich (1997, 1998) as these studies have been the subject of recent controversy. This review concludes that findings of increased fracture risk with increased dietary (dairy) calcium intake in these studies, in contrast to Holbrook (1988), reflects the high retinol content of low fat milk in the USA; distortion of the results due to people at high risk of osteoporosis consuming more dairy products; increased use of cheese compared with milk. The review in Appendix 3 also confirms that there is no reliable evidence indicating an adverse effect of calcium in itself on bone health, at least at intakes below 2000 mg per day. Overall, epidemiological studies of dairy calcium are consistent with a protective effect in childhood and adolescence which declines with age and may be reversed in older adults, particularly in relation to cheese and to dairy products fortified with retinol. Appendix 4 reviews the controversy over protein. This review concludes that there is real advantage in using vegetable protein sources (except grains) rather than animal protein sources (except milk and yoghurt) to ensure an adequate protein intake. Appendix 1: A model for calcium balance Many of the elements of calcium balance are well known. Each extra mmol of sodium in the urine is associated with 0.01 extra mmol of calcium in the urine (Massey, 1996). About 95% of dietary sodium is excreted in the urine. Short term metabolic loading studies tend to show a slightly weaker effect, and cross-sectional studies of free-living populations tend to show a slightly stronger effect. A recent large cross-sectional study (Ho, 2001) found a coefficient of 0.014 rather than 0.01. Overall, a robust approximation is given by UCa (mmol) = 0.01 * Na (mmol) 1 where UCa is the change in urinary calcium and Na is the change in dietary sodium. The effect of protein intake on urinary calcium loss is also well established (Barzel, 1998; Heaney, 1998; Weaver, 1999). The effect is proportional to the sulphur content of cysteine and methionine in the diet (though not to the sulphur content of taurine, which is often excreted intact) and is equivalent to about 0.1 mmol of urinary calcium loss for each mmol of sulphur (S) consumed in the diet in the form of methionine or cysteine. That is UCa (mmol) = 0.1 * S (mmol) S (mmol)= cysteine (g)* 8.3 + methionine (g) * 6.7 2 3 Heaney (1998) confirms that this effect is seen in cross-sectional studies as well as short term loading studies, with an observed calcium loss of 0.85 mg per gram of protein. As each gram of protein in a typical diet contributes about 0.275 mmol of sulphur, the predicted effect of a gram of protein would be 0.0275 mmol (1.1 mg) of calcium. The short term studies appear to capture a persistent effect. At this point consensus fades. Some authors consider the effect of sulphur to be due to the acid created when sulphur-containing amino acids are metabolised (2 mmol of acid for each mmol of sulphate). This is made more plausible by the observation that adding potassium bicarbonate (KHCO3) to the diet causes a decrease in the excretion of calcium in the urine. However, the extent of the decrease should be 0.05 mmol of calcium per mmol of bicarbonate if both effects are operating through the mechanism of net acid excretion. Lemann (1993) provides a very pertinent summary of short term metabolic loading tests: UCa (mmol) = -0.015 * KHCO3 (mmol) UCa (mmol) = 0.0 * NaHCO3 (mmol) UCa (mmol) = -0.005 * KCl (mmol) 4 5 6 These three relationships can be combined with the effect of sodium (1) and rearranged to give an equivalent set of equations in terms of the effects of individual ions: UCa (mmol) = -0.005 * K (mmol) UCa (mmol) = 0.0 * Cl (mmol) UCa (mmol) = 0.01 * Na (mmol) UCa (mmol) = -0.01 * HCO3 (mmol) 7 8 9 10 It is striking that the effect of bicarbonate is only -0.01 mmol/mmol while the effect implied if the influence of protein is mediated by acid is -0.05 mmol/mmol. This counts strongly against the claim that the effect of protein is governed by the associated acid, and indicates that sulphate and bicarbonate effects need to be modelled separately. Sebastian (1994) observes an effect of urinary potassium, provided by the addition of potassium bicarbonate to the diet, on urinary calcium of -0.022 mmol/mmol. This is only slightly greater than that indicated by equation 4, particularly when we note the absorption of dietary potassium to be about 90%, giving an expected effect of about -0.017. This observation therefore supports the model above. Sebastian (1994) also notes that earlier work found a reduction in urinary calcium by potassium citrate but not by sodium citrate. As citrate is metabolised in the body equivalently to bicarbonate, this observation is also consistent with the above model. Breslau (1988) provides data on the effect of varying intakes of cysteine and methionine on urinary calcium losses. Intakes of most minerals are kept approximately constant between the different test diets, but there is an 8 mmol per day decrease in potassium between the soy protein and animal protein diets as well as a 10 mmol per day increase in sulphate from protein. From the model, the sulphate increase should cause a 40 mg increase in calcium excretion and the potassium decrease should cause a 5 mg increase in calcium excretion (if associated with bicarbonate). The predicted increase of 45 mg per day in urinary calcium matches the observed increase of 47 mg per day well. Ho (2001) estimates the effect of urinary potassium (about 90% of dietary potassium) on urinary calcium in a free-living population to be UCa (mmol) = -0.012 * UK (mmol) 11 This substantially exceeds the predicted effect for potassium alone (-0.005), but the effective provision of bicarbonate from the diet is governed by an ion balance: HCO3 = 0.9*K-1.8*0.65*P+0.95*(Na-Cl)+2*0.4*Mg+2*FA*Ca 12 This expression is adapted from Remer (1994, 1995) with the substitution of slightly different estimates for the fractional absorption of potassium (0.9), magnesium (0.4), calcium (see below) and phosphorus (0.65). All quantities are in mmol. Phosphorus is denoted by P and magnesium by Mg. It should be noted that the term bicarbonate is used to represent any salt that will act as a source of alkali in the body. The effect of a food on net alkali in the body can be calculated by subtracting twice the sulphur (equation 3) from the bicarbonate (equation 12). In typical modern diets, sodium and chloride are approximately equal and the dominant factor in providing base is potassium, though its effect is modified (slightly attenuated) by correlations with other ions in the diet, particularly phosphate. This means that in practice potassium acts as an approximate proxy for bicarbonate as well as in its own right. The earlier equations for the effect of potassium (7) and bicarbonate (10) therefore predict that the apparent effect of dietary potassium on urinary calcium will be close to -0.015 mmol urinary calcium per mmol dietary potassium (the sum of the potassium and bicarbonate effects), which is consistent with equation 11. Ho (2001) failed to find an effect of dietary protein, evaluated by a food frequency questionnaire, on urinary calcium excretion. This is unsurprising, as the estimated protein intake will be much less accurate than the measures of urinary sodium and potassium. In contrast, Heaney (1998, 2000) used chemically analysed diets and did find such an effect. Sodium, potassium, bicarbonate and protein have not been found to affect either gut losses of calcium or losses of calcium in sweat, so the effect on urinary loss of calcium appears to be the net effect on calcium losses from the body. This is in contrast to phosphorus which decreases urinary losses while increasing gut losses, giving no overall effect on calcium loss (Heaney, 1994). To complete the model, the dependence of calcium absorption on dietary calcium intake needs to be quantified. The fractional absorption of calcium from a single portion (load) of dairy products is given by Weaver (1999) as Calcium Fraction Absorbed = 0.89 - 0.096 * ln(calcium in portion in mg) 13 This predicts a strong decline in absorption with calcium intake, in a given meal, but does not lend itself to direct application to calculating the expected absorption for a given daily intake of calcium. Heaney (2000) notes that the average fractional absorption is given by Calcium Fraction Absorbed = 0.22 * (daily calcium in grams) ^ (-0.44) 14 Assuming daily intake to constitute a single load, equations 13 and 14 are very consistent for calcium intakes above 500 mg per day. This indicates that the decline in absorption reflects primarily a short term load effect rather than a longer term adaptation to dietary calcium intake or to calcium losses. Gonnelli (2001) presents similar relationships, but with slightly lower absorption at moderate intakes and a more rapid decline in absorption with intake: 0.18* (daily calcium in grams) ^ (-0.6) for men, and 0.155* (daily calcium in grams) ^ (-0.66) for women. Agnusdei (1998) indicates a fractional absorption of 0.19* (daily calcium in grams)^(-0.54). This paper will use equation 14, but it should be noted that this choice may somewhat overestimate calcium absorption, particularly at high intakes. However, as calcium intake increases so do urinary losses of calcium and endogenous faecal losses (loss of calcium from the gut without reabsorption). This means that the net absorption of calcium is less than indicated above. Recker (1977) examines the effect of calcium carbonate supplementation on calcium balance in women with an average age of 57. Calcium balance rises by 72 mg, while calcium absorption rises by 108 mg, as calcium intake goes from 530 mg to 1480 mg. The expected absorption for the change in intake is 220 * (1.48 ^0.56 – 0.53^0.56), that is 120 mg. This prediction is a good match to the observed absorption of 108 mg. However, about a third of the absorbed calcium disappears as increased losses reduce net absorption by one third compared to gross absorption. It would be preferable to have data from a number of different calcium supplementation trials to verify the estimate that one third of absorbed calcium disappears in extra losses, but such data do not seem to be available. Other sources of evidence do not allow a better model of calcium dependent losses, though they do indicate that the scale of the losses is at least as a third of absorbed calcium. Correlation studies of urinary calcium loss and dietary calcium intake suggest that about 6 mg of calcium is lost in the urine per 100 mg of calcium intake (Heaney, 1999). This observed loss will reflect a combination of the actual effect of calcium on urinary losses and the effect of associated nutrients in dairy foods, which are accounted for separately in the model above. This value for calcium-dependent losses may also overestimate losses at higher calcium intakes, since losses can be expected to decrease as fractional absorption decreases with increasing calcium intake. Heaney (1994) provides a relationship between absorption fraction and endogenous faecal losses. Examining this relationship shows that these gut losses amount to about 10% of absorbed calcium for calcium intakes between 500 mg and 1500 mg. This indicates that the dominant calcium-dependent loss is the urinary loss. Both Heaney (1986) and Heaney (1999) indicate that a simple straight line relationship between absorbed calcium and urinary calcium explains a high proportion of the variation in urinary losses, but neither paper states the slope of the fitted line. Even if the slope were given, it would be influenced by associated nutrients as well as by calcium itself. The available data do not justify a more precise model than assuming that calcium-dependent losses are a constant proportion of the absorbed calcium and estimating this proportion from the results of Recker (1977) to be one third. The following equation will therefore be used to define the typical absorbed fraction of calcium, while the increased losses associated with absorbed calcium will be ignored in calculating the calcium losses. Net calcium fraction absorbed = 0.15 * (daily calcium in grams) ^ (-0.44) 15 Where overall daily calcium intake is not known, as in the examination of the effects of individual foods on calcium balance, the effect on balance will be evaluated for several different ranges of calcium intake. For example, for an intake range of 500 mg to 1000 mg, the effective absorption can be estimated as 0.15 * (1^0.56 – 0.5^0.56) / 0.5, so 0.096 is the expected net fractional absorption. The final element for computing the calcium balance is an estimate of calcium losses when all dietary drivers (calcium, sodium, potassium, protein and bicarbonate) are zero. Trial and error comparison with known variations in total calcium losses indicates 2.0 mmol (80 mg) per day to be appropriate. The overall expression for the calcium balance is therefore Calcium balance (mg) = Ca (mg) * FA – 80 + 40 * (0.005 * K + 0.01 * HCO3 – 0.01 * Na – 0.1 * (8.3 * cysteine (g) + 6.7 * methionine (g) ) ) 16 where FA is the net fractional absorption of dietary calcium and HCO3 is calculated from equation 12. All quantities are in mmol unless otherwise stated. If data on cysteine or methionine are missing, but data on protein are available, then sulphur from protein, in mmol, can be estimated, based on a typical methionine and cysteine content of protein, as 0.275 * protein (g), instead of using equation 3. Equation 16 can be used in several ways: The effect of individual foods on calcium balance can be evaluated by assuming an appropriate net fractional absorption (FA) for the range of calcium intakes being considered and evaluating the change in calcium balance due to the mineral and amino acid content of the food. For a given dietary composition, the predicted overall calcium balance at typical net fractional absorption (equation 15) can be calculated. The required calcium intake to give calcium balance at typical calcium absorption can be calculated, keeping other nutrients constant. The required fractional absorption (RFA) to achieve calcium balance can be calculated by finding the fractional absorption which gives a zero calcium balance. The RFA can be divided by the typical fractional absorption from equation 15 to give a normalised required fractional absorption (NRFA). The NRFA provides a direct measure of how well the overall diet supports bone health. The lower the NRFA, the better the diet. As variations of more than a factor of 2 around the absorption predicted from equation 14 are unusual (Heaney, 1986; Heaney, 2000), an NRFA below 0.5 can be considered an excellent assurance of bone health, while an NRFA above 2 indicates a seriously deficient diet. This approach can be illustrated by examining four example diets: a typical Western omnivore diet, an estimated palaeolithic diet, a typical Western vegan diet, and the diet recommended in the overview. All the diets are based on a 70 kg person consuming 2500 kcal per day. Table 3 also shows the net alkali contribution of the diet as the difference between the estimated intake of bicarbonate (equation 12) and the intake of acid from protein. 80% protein absorption is assumed, with acid equal to twice the sulphur content of the absorbed protein. omnivore palaeolithic vegan recommended Ca (mg) 800 1500 600 1000 Na (mg) 3000 700 3000 1500 Protein (g) 100 200 50 70 K (mg) 2500 8000 3500 6000 Cl (mg) 4800 1400 4900 2600 Mg (mg) 250 800 350 600 P (mg) 1500 3000 1500 2000 NRFA Net alkali (mmol) 1.68 -27 1.28 -12 1.46 -12 0.84 34 Calcium balance (mg) -92 -53 -53 +24 Table 3: Diet types, net alkali and calcium balance The typical omnivore diet has the highest NRFA and the highest calcium loss. The typical vegan diet and the palaeolithic diet have similar calcium losses, but because of the higher calcium content in the palaeolithic diet it would be easier to achieve balance by adaptation mechanisms increasing the fractional absorption. In contrast, the recommended diet can maintain calcium balance with fractional absorption below average. This analysis sheds an interesting light on how our palaeolithic ancestors maintained healthy bones while consuming large quantities of protein. Despite a calcium to protein ratio (mg per g) of just 7.5, they are closer than either typical modern omnivores or vegans to having an adequate diet to support bone health. Also, the level of base in their diet adequately counters the acidifying effects of the high protein intake, so blood and urine pH would not be expected to be low by Western standards. With high levels of physical activity and sun exposure, it is likely that they had better calcium absorption than is now typical, further improving bone health. Interestingly, Eaton (1991) shows that almost all of the palaeolithic calcium intake came from plant sources. Unfortunately, with the exception of green leafy vegetables, the calcium content of cultivated fruits and vegetables is often much inferior to that of their wild counterparts (Milton, 1999), so vegans need to take some care in their dietary choices to get sufficient calcium, despite exclusive use of plant foods. Assuming calcium absorption follows equation 15, the required calcium intake to bring each diet into balance is 2000 mg (omnivore), 2300 mg (palaeolithic), 1200 mg (vegan) and 735 mg (recommended). The corresponding required calcium to protein ratios of the four diets are 20, 11.5, 24 and 10.5. Heaney (1998) suggests that a calcium to protein ratio of 20 is adequate for bone health. While calcium intake and protein intake are two of the strongest influences on calcium balance, they should not be considered in isolation from sodium, potassium and bicarbonate. Promoting bone health points towards increasing calcium and potassium intakes, moderating protein intake and substantially decreasing sodium intake, compared with Western standards. This combined strategy has a much better chance of success than the current (correct but unbalanced) emphasis on calcium as it is less vulnerable to poor calcium absorption. Application of the model to specific foods In calculating calcium balances for the food tables provided in this paper, food composition data were taken from USDA (1999). Calcium bioavailability in plants was adjusted where good data were available. The available calcium in high oxalate plants (spinach, rhubarb, Swiss chard) was reduced by 80% compared with their nominal content (Weaver, 1997). Kale, broccoli and Chinese cabbage had available calcium increased by 10% (Weaver, 1997; Benway 1993, Weaver, 1999). Soy products had their calcium bioavailability reduced by 25%, while other beans had their bioavailability reduced by 50% (Weaver, 1993). The bioavailability of calcium from other foods was not adjusted. The impact on the calcium balance calculations was substantial for the high oxalate foods. As the USDA database does not have data on chloride content, a correction was made by estimating the excess of chloride over sodium based on McCance and Widdowson (1991). This adjustment was most significant for meat and fish, for which it increased the net alkali by 1.5 mmol per 100 g. For whole grains, particularly brown rice, and for bananas, it decreased the net alkali significantly. The impact on the calcium balance calculations was negligible. Validation of the model The key test of this model is its ability to predict the effects of specific foods. One of the most thorough studies of the effect of milk supplementation is Recker (1985). This study examined the effect on calcium balance of adding 24 oz (670g) of milk to the diet of 13 postmenopausal women. Calcium balance was measured one year after supplementation commenced and compared with control subjects who did not receive extra milk. The one year interval is vital, as it allows the bone remodelling transient to decay and the body’s adaptation mechanisms to operate, so the measured balance should reflect the long term effect (Heaney, 2001). Calcium intake increased from 680 mg per day to 1470 mg per day. The observed effect on calcium balance was an improvement of 45 mg per day. Using the model in Appendix 1, the predicted effect on calcium balance of an extra 670 g of cow’s milk, starting from an initial intake of 680 mg per day, is 48 mg per day – a very good match. If the change in calcium intake had been accomplished using calcium carbonate, the predicted change in balance would have been 65 mg. The difference reflects the losses associated with the milk and confirms the validity of the model for predicting the effect of dairy products on calcium balance. It is also noteworthy that after allowance for calcium losses in sweat (about 50 mg per day), which were not considered in this study, the extra milk changed the overall calcium balance from a loss of 110 mg per day to a loss of 65 mg per day. Therefore this study shows that increased calcium consumption from dairy products up to the highest recommended intake fails to prevent a net loss of calcium in postmenopausal women. Nonetheless, the 40% reduction in loss observed is a major improvement. Another key study is Devine (1995). This study used supplementation of either calcium lactate gluconate or powdered milk to increase calcium intakes by about 1000 mg per day in two thirds of the study group. The study then examined changes in bone mineral density over two years. It would have been preferable to start the bone mineral density measurements after one year to avoid the remodelling transient, as the remodelling transient will increase the apparent effect of increased calcium intake beyond what would be sustained after the transient has passed. Calcium intake was estimated from dietary records and sodium intake from urinary sodium excretion. Models were then developed by statistical regression for the effects of calcium, sodium and weight on the change in bone mineral density at different parts of the skeleton. At two bone sites both calcium and sodium were found to have a statistically significant effect on rate of change of bone mineral density, with the effect of 100 mg of calcium being positive and about two times larger than the negative effect of 100 mg sodium. The predicted effect of milk at the median calcium intake of 1500 mg is about 5.5 mg per 100 g of milk, or 4.6 mg per 100 mg of milk calcium. The expected effect of the calcium supplement is about 7 mg per 100 mg of calcium. The predicted average effect of calcium intake on calcium balance is therefore an increase of 5.8 mg per 100 mg. The expected effect of sodium on calcium balance is a decrease of 1.7 mg per 100 mg. The predicted relative effect of calcium and sodium is therefore 3.4:1, compared with the observed relative effect of about 2:1. This suggests that the model is giving a useful prediction of the observed effect but may be underestimating the adverse effect of sodium relative to the beneficial effect of calcium. If we took the coefficient for the effect of sodium from Ho (2001), the predicted effect of 100 mg of sodium on calcium balance would become a decrease of 2.4 mg calcium per 100 mg sodium, making the expected relative effect 2.4:1. Overall, the degree of consistency between the model and the observations is very encouraging. Heaney (1998) argues that increased losses are of limited importance when calcium intakes are high, as the body will successfully increase calcium absorption from the gut to compensate for increased losses. There is some truth in this, in that the body can balance increased losses by absorbing more calcium from the gut or by absorbing more calcium from bone. However, the success of the model above in predicting the results of Recker (1985), indicates that the ability to compensate for increased losses by increased absorption of calcium from the gut is limited in post-menopausal women and that increased losses due to components of milk other than calcium are still reflected directly in reduced balance after a year of adaptation. As noted in Recker (1985), “examination of the correlation between protein intake and calcium balance with calcium intake held constant showed a reasonably strong negative correlation”. Increased protein intake was also associated with increased bone resorption after adjustment for calcium intake. At least for postmenopausal women, the degree of adaptation appears to be limited, even at high calcium intakes, and the model’s predictions of the net effect of foods on calcium balance appear to be valid. Appendix 2: The results of long term trials on calcium supplementation The strongest evidence for the effect of diet on health comes from investigator-controlled intervention studies of sufficient duration to allow the full effect of the dietary change to be observed. The fundamental advantage of such studies is that the results are not distorted (confounded) by associations between individual dietary choices and other characteristics. However, most intervention trials on calcium supplementation, either with supplements or with dairy products, are of such short duration as to be virtually meaningless. When calcium intake increases substantially the level of PTH in the blood drops substantially. This reduces the rate of creation of new sites for bone remodelling – removal of bone by osteoclasts and its replacement by osteoblasts. However, existing sites continue to be remodelled. This creates a transient imbalance between osteoclast activity starting at new sites and osteoblast activity continuing at old sites. The net result is an increase in bone mass over a period ranging from 6 months in children to 18 months in elderly adults. If supplementation is stopped, this transient is reversed. If supplementation is continued beyond the duration of the bone remodelling transient, we see the underlying long term effect of the supplementation. Trials of sufficient duration to see the long term effect of supplementation on bone density, particularly if they also assess impact on fracture incidence, provide the strongest evidence for the effect of calcium on bone health. The handful of trials satisfying this criterion are reviewed below. In comparing the effect of supplementation on changes in bone density relative to changes in unsupplemented (control) subjects, the rate of change in bone mineral density in the supplemented subjects will be calculated between two years after the start of the trial and the end of the trial. The rate of change in the control subjects will be calculated over the entire trial duration. There have been three trials of supplementation of calcium, without vitamin D, lasting for four years and reporting detailed BMD changes in each year of the study. The rates of change of BMD at various bone sites are summarised below. For Riggs (1998b) only the rate of change of the supplemented group relative to the control group can be reported. Reid (1995) Supp Cont Riggs(1998b) Supp Cont Peacock (2000) Supp Cont Age Initial calcium mg per day 58 760 59 710 66 710 66 720 74 600 73 600 Final calcium mg per day 1760 710 2300 717 1350 600 % per year at hip -0.2 -0.7 0 % per year at spine +0.1 -0.4 -1 % per year Fracture total body incidence -0.1 -0.5 +0.15 +0.1 -0.2 -0.25 -0.6 -0.9 -0.1 1.5% per year 5% per year N/A N/A 18 cases 23 cases Table 4: Results of long term calcium supplementation trials The results from Reid (1995) and Peacock (2000) are impressive. Both show a notable reduction in rate of bone loss. This reduction is consistent with the estimated 40% improvement in calcium balance observed in Recker (1985) on making a similar shift in calcium intake using milk and the estimated 50% improvement in calcium balance observed by Recker (1977) using calcium carbonate. Reid shows a statistically significant reduction in fracture risk. Peacock shows a non-significant reduction in fracture risk. Recker (1996) also carried out a four year supplementation trial increasing calcium intake from 450 mg per day to 1650 mg per day using calcium carbonate. This trial did not report detailed BMD changes year by year, but did report a significant reduction in fracture incidence in women with a history of vertebral fractures (7% per year compared with 13% per year). This adds up to a powerful case for improved bone health with calcium supplementation. In contrast, Riggs (1998b) shows no benefit and indeed shows a notable loss of BMD in the spine in the supplemented group compared with the non-supplemented group over the last two years of the study. Riggs (1998b) showed gains in BMD of between 1% and 2.5% at the different bone sites over the first two years of the study. The contrast between the first two years and the second two years show that eliminating the bone remodelling transient is vital in any analysis of the effect of a treatment on bone health. There were differences in the forms of supplements used. Riggs used citrate, Peacock used citrate malate and Reid and Recker used carbonate. This seems unlikely to account for the differences in results. The only other obvious difference is that the supplemented calcium intake in Riggs was higher than in any other study. It is possible that very high calcium intakes have adverse effects. For example, calcium intakes above 2000 mg per day combined with high phosphate intakes could disrupt magnesium absorption (Hardwick, 1990). In Riggs (1998b), a third of those receiving supplements exhibited greatly increased losses of calcium in the urine requiring reduction of the supplement dose, indicating that calcium intake was being pushed beyond desirable levels. Overall, the lesson from Riggs (1998b) appears to be that calcium intakes beyond 2000 mg per day should not be encouraged. The observation that many primates have much higher calcium intakes relative to body size than a human consuming 2000 mg per day does not provide assurance of safety as these primates consume high levels of calcium in the context of a diet rich in other minerals, including magnesium and potassium (Milton, 1999). Fracture rates have also been reduced using combined calcium and vitamin D supplementation (Chapuy, 1992; Chapuy, 1994; Dawson-Hughes, 1997). Chapuy (1992,1994) supplemented 1.2 g of calcium, as calcium phosphate, and 20 micrograms of vitamin D3 on top of a dietary calcium intake of 500 mg per day and initial calcidiol levels of about 40 nmol/l. Fracture rate was reduced by 25% over three years. Dawson-Hughes (1997) supplemented 500 mg of calcium, as calcium citrate malate, and 17.5 micrograms of vitamin D3 on top of a dietary calcium intake of 700 mg per day and initial calcidiol levels of 75 nmol/l. Non-vertebral fractures were reduced by 60% over three years. The effect on bone mineral density change from the end of the first year to the end of the third year was a reduction in loss of about 0.35% per year, similar to the changes observed with calcium only. In contrast, supplementation with vitamin D alone appears to have no significant effect on fracture risk, in general populations, despite a modest reduction in bone loss (Lips, 1996; Peacock, 2000). The initial calcidiol levels in Lips (1996) were 25 nmol/l, so the failure to find a benefit is not explicable by higher initial levels of calcidiol. This illustrates the importance of tackling fracture risk on a broad front rather than relying on a single intervention. Overall, the evidence from intervention trials shows a benefit of increasing calcium intake to between 1000 and 2000 mg per day, with a possible further benefit on fracture rate by simultaneously ensuring adequate vitamin D intake. Greater increases in calcium intake are not supported by existing studies. The positive effects of calcium supplementation on bone mass and fracture risk observed in intervention trials make a conclusive case for a benefit of calcium. Heaney (2000b) states that “no further distinction need be made between dietary and supplemental sources of calcium” but this assertion is not well founded. The results of Recker (1985) discussed above indicate that the effect of milk on calcium balance is about 70% of the effect of its calcium content, as predicted by the model presented in Appendix 1. The model further predicts that not all dairy products are alike. At moderate calcium intakes some cheeses make a modest positive contribution to calcium balance while others make a negative contribution. For individuals with relatively low calcium absorption, increased consumption of cheese will generally cause a reduction in calcium balance, so cheese cannot be expected to act as an effective source of calcium. Milk and yoghurt are the only dairy products that are likely to improve calcium balance on calcium intakes above 500mg per day, though even they will be less effective than many other sources of calcium. There is only one long term trial of increasing dairy product consumption. Baran (1990) used unspecified dairy products to increase calcium consumption from 900 mg per day to 1500 mg per day in premenopausal women. The study showed a statistically significant difference in vertebral bone density after 30 months. This was largely due to an apparent 3% drop in BMD in the unsupplemented control group between 18 months and 30 months. Neither group showed any clear change in BMD during any other time interval. This pattern does not allow evaluation of the effect of the intervention after the remodelling transient has ended as it suggests a higher degree of random error in the measurements than indicated in the paper or some artefact such as one or more women in the control group entering menopause: there is no reason to expect premenopausal women to lose 3% of bone mineral density in a year. There are no experimental data which contradict the expectation, based on the model in Appendix 1, that increased milk consumption will show less benefit than expected based on its calcium content and that increased cheese consumption will show negligible benefit and may indeed have a modest adverse effect on high risk individuals with relatively low calcium absorption. Results from epidemiological observations are consistent with this view. These results are discussed in more detail in Appendix 3. Appendix 3: Epidemiological studies on dietary calcium and bone health There is considerable evidence from studies in Asia, such as Hirota (1992), Hu (1993), Fujiwara (1997) and Lau (2001), that increasing calcium intake to above 500 mg per day benefits bone health. It would be astonishing if it did not. In many cases, the additional calcium is provided by milk or other dairy products. Calcium intakes below 500 mg per day are not consistent with optimal bone health in any society with an ageing population. Such low calcium intakes will reduce bone growth during childhood and adolescence, increasing the adverse effect of later losses. Heaney (2000c) provides many other examples of studies supporting this conclusion. The strongest evidence short of intervention studies comes from prospective studies. In prospective studies, the characteristics of healthy individuals are recorded prior to observing their health over a number of years. This avoids bias due to current diet and recollection of past diet being altered by existing illness. However, such studies are still subject to confounding by associations between different characteristics of the same individual. For example, Cumming (1997) found a 50% increased risk of vertebral or hip fracture in calcium supplement users. This observation contradicts the results of the intervention trials discussed in Appendix 2. The results were unlikely to be due to chance, so potential explanations need to be considered. The obvious explanation is that individuals who perceive themselves to be at high risk of fracture are more likely to take calcium supplements than individuals with robust bone structure and no family history of osteoporosis. The higher pre-existing risk for such individuals then becomes associated with the use of calcium supplements. Indeed, the authors found “supplement users were more likely than were nonusers to have a history of falls, fractures or osteoporosis” and considered this to be the most likely explanation of the observed association. Cumming (1997) also found a similar, but not statistically significant, association between both dietary calcium and milk intake and vertebral fracture, which may be subject to the same explanation. Holbrook (1988) found an increase of 200 mg of dietary calcium per 1000 kcal to reduce fracture risk by 40%. This result is consistent with the intervention studies discussed above. Most other prospective studies found no significant effect of dietary calcium. This may, in part, reflect the difficulty of accurately measuring calcium consumption. It may also reflect the expected difference in effect between different sources of calcium. There is also likely to be a variable degree of confounding due to high risk individuals choosing to consume more dietary calcium. However, Feskanich (1997) found an adverse association between dietary calcium intake and dairy calcium intake and risk of hip fracture. The highest quartile of either dietary or dairy calcium intake showed a 100% increase in risk of hip fracture compared with the lowest quartile. That is, those individuals in the top 25% by calcium consumption had a risk of fracture twice that of those in the bottom 25%. There was also a tendency towards an adverse association between current milk consumption and hip fracture rate, which was statistically significant for consumption of three or more glasses of milk per day (increased risk of 75%). Feskanich also found a tendency towards a protective association from increased childhood milk consumption (decreased risk of 47% for three or more glasses of milk per day) and no change in risk associated with life-long high milk consumption. The trend in these results is as expected from the basic mechanics of calcium balance set out in the present paper. That is, the benefit of a high calcium intake is expected to be greatest in children and younger adults, who show better absorption of calcium. The balance between increased calcium intake and increased calcium losses with increased dairy product consumption will thus be more favourable for them than for older adults. The observation that milk consumption is associated with a less pronounced adverse effect than overall dietary calcium is also unsurprising. However, the apparent increase in risk of fracture by a factor of two with high current dietary calcium intake in older adults is not expected from the predicted effect of dietary calcium sources on calcium balance, which only suggests only a modest adverse impact of cheese in high risk individuals. It is possible that the Feskanich study was confounded by high risk individuals choosing to drink milk and consume more dairy products in an attempt to reduce risk. This is made more probable as the study was carried out among nurses in the USA who would be well aware of conventional risk factors for fracture and influenced by strong promotion of dairy products as a protective measure. This effect of high risk groups adopting behaviours believed to be protective is well established and is the reason why the analysis in Feskanich (1997) was carried out after eliminating calcium supplement users. This explanation of the observed results is supported by analysing the results of Feskanich (1998) which differentiated the same study population based on a genetic risk factor for osteoporosis. Each hip fracture case was matched with two controls with no fracture, and a genetic test was carried out to unmask the genetic risk factor. The high risk (BB) genetic subgroup had a twofold increase in hip fracture risk compared with the other subgroups (Bb and bb). Elevated risk of fracture was observed only in the BB group with low calcium intake compared to other groups with low calcium intake. The results presented in the paper were analysed further by reconstructing unpublished data on the numbers of study members in each genetic group and calcium intake level combination. This reconstruction is shown in Table 5. Low calcium cases Low calcium controls High calcium cases High calcium controls BB 6 6 8 10 Bb 8 22 13 24 bb 6 27 9 11 Table 5: Distribution of cases and controls by genotype and calcium intake This indicates that 60% of the high genetic risk (BB) group were in the high calcium intake group. The high risk individuals in the high calcium group show a modest reduction in risk. That is, unmasking the hidden risk factor indicates the expected modest protective effect of high dietary calcium (-20%) rather than an apparent adverse effect when the entire high calcium group is compared with the low calcium group (+50%). This analysis shows that at least some of the apparent adverse effect of dietary calcium is due to confounding by high risk individuals choosing a behaviour believed to be protective. Indeed, it is possible that a true protective effect of dietary calcium is being masked by this confounding, though it is likely that any such effect is modest compared with other risk factors. It is also possible that some factor in dairy products, other than their mineral and protein content, is having an adverse effect. Melhus (1998) sheds some light on this possibility. An analysis of fracture data in a Swedish cohort, adjusting for multiple nutrients, showed an adverse effect of calcium on fracture risk. However, Melhus noted an association of fracture risk with intake of retinol (pre-formed vitamin A). Compared with intakes of less than 500 micrograms per day, there was a 30% increase in risk for intakes between 1000 and 1500 micrograms per day and a 95% increase in risk for intakes above 1500 micrograms per day. Adding retinol to the nutrients being considered eliminated the elevated risk associated with high calcium intake. This did not, however, eliminate milk consumption as a risk factor since in Sweden low fat milk contains 450 micrograms of retinol per litre. This study illustrates the fallacy of regarding milk as equivalent to calcium. Milk contains many substances and cannot be assumed to act simply as a calcium source The association of high retinol intakes with osteoporosis was recently confirmed in the USA (Feskanich, 2002). An 89% increase in risk of fracture was observed for total retinol intakes of more than 2000 micrograms per day compared with intakes of less than 500 micrograms. A 69% increase in risk was found for retinol intakes from food above 1000 micrograms per day compared with less than 400 micrograms. Beta carotene (converted in the body to vitamin A) was not associated with excess risk in either Melhus (1998) or Feskanich (2002). The consistency of results between Sweden and the USA, despite many other differences between the two countries, strongly supports a true adverse effect of retinol and the absence of any adverse effect from plant carotenes. Retinol may have notably influenced the results in Feskanich (1997, 1998), as US milk which has been fortified with vitamin A (the most common sort) contains about 600 micrograms of retinol per litre compared with 450 micrograms per litre in Swedish milk. While the USA does not make extensive use of cod liver oil, which is a major source of retinol in Scandinavia, there is extensive use of multivitamins containing retinol. High consumption of milk fortified with vitamin A will make a significant contribution to total retinol intake and thus to the likelihood of consuming more than 1500 micrograms per day, the apparent threshold for a notable adverse effect. Trends in dairy product consumption in the USA (Miller, 2000) may contribute strongly to the difference between the results of Holbrook (1988) and Feskanich (1997). Between 1970 and 1995, milk consumption declined from 320 ml per person per day to 240 ml per person per day. Whole milk consumption declined by over 60%, while low fat milk consumption increased from less than 20% to more than 60% of total milk consumption. Cheese consumption increased from 13 g per person per day to 34 g per person per day. Holbrook (1988) was based on a sample from a community in California, aged 50 to 79 at the start of the study, over the period 1973 to 1987. Feskanich (1997) was based on US nurses, aged 34 to 59 at the start of the study, over the period 1980 to 1992. Differences in patterns of consumption of dairy products between the two groups may have been greater than indicated by national trends, due to differences in age and professional background. Full fat milk contains only about 200 micrograms of retinol per litre compared with about 600 micrograms per litre in fortified low fat milk. The analysis in the current paper also shows that for people at high risk of osteoporosis due to relatively low calcium absorption cheese will make calcium balance worse. Honkanen (2001) also provides an interesting insight into the complexity of the effect of dietary calcium. High dietary calcium intake (>900 mg per day) was associated with a modest and nonsignificant increase in bone loss at the spine (-0.48% compared with –0.35%) in postmenopausal women who did not regularly use hormone replacement therapy (HRT). In contrast, high calcium intake was associated with reduced bone loss (+0.3% compared with –0.05%) in regular HRT users. As oestrogen treatment makes calcium metabolism more like that of younger women, this effect is consistent with the prediction in this paper that the benefit of dairy products for bone health will diminish or even reverse with age. Overall, epidemiological studies of dietary calcium are consistent with a protective effect in childhood and adolescence which declines with age and may be reversed, particularly for cheese, in older adults at high risk for osteoporosis due to low calcium absorption. For older adults, the addition of retinol to milk may introduce an increase in risk greater than any benefit from the calcium provided. Appendix 4: Protein and bone health Comparisons between countries (Frassetto, 2000) indicate that an increase in the ratio of animal to vegetable protein is strongly associated with increased age-adjusted hip fracture rates in women over the age of fifty. In the original 33 countries analysed, 70% of the variation was explained by animal to vegetable protein ratio, but the observed effect is likely to have been inflated by confounding. The effect is reduced when comparisons are restricted to 20 predominantly Caucasian countries with female disability-adjusted life expectancy over 71, but is still statistically significant (p=0.014) and explains 25% of the variation of hip fracture incidence among these countries. In the 20 country analysis carried out by Stephen Walsh, there was no effect from total protein intake or disability-adjusted life expectancy, but both were uniformly high (70 to 110 g protein per person per day and 71 to 77 years life expectancy). In the Graph 1, age-adjusted hip fracture incidence is plotted against the ratio of animal protein to vegetable protein (blue diamonds). The purple squares indicate the best straight line fit obtained by regressing hip fracture incidence against the ratio. 20 country analysis 250 hip fracture incidence 200 150 100 50 0 0 0.5 1 1.5 2 2.5 Animal protein/ Vegetable protein Graph 1: Inter-country comparison of hip fracture incidence and ratio of animal to vegetable protein The observed association remained significant when the cluster of four countries at the top right of the graph (Germany, Denmark, Sweden and Norway) was eliminated from the analysis. Such comparisons between countries are vulnerable to confounding, but the results are consistent with a real benefit from consuming a higher proportion of protein from vegetable sources while maintaining an adequate protein intake. Frassetto (2000) suggests that this association may reflect the effect of animal and vegetable protein sources on net alkali consumption. This is a possible factor, but many concentrated sources of vegetable protein, such as soy and beans, have a positive impact on calcium balance while meat, fish and eggs have a negative effect. Milk also has a positive effect, albeit much less than that of kale and spring greens. Some cheeses have a modestly positive effect, though the positive effect of cheese disappears at higher overall calcium intakes. The effect of different protein sources on calcium balance provides a clear and direct explanation for the observed association, though the balance between protein from milk and protein from other animal sources would be expected to alter the observed effect of animal protein considerably. It should be emphasised that inadequate overall protein intakes can be expected to adversely affect bone health. However, at any given protein intake bone health is expected to be favoured by a high ratio of vegetable to animal protein. This is exactly what was observed by Sellmeyer (2001). Age-adjusted bone mineral density was positively associated with the ratio of animal to vegetable protein, but on adjustment for total protein intake and other factors the apparent relationship was reversed, though this was not statistically significant. The picture on hip fracture incidence was more straightforward, with the age and weight adjusted risk of fracture rising with animal protein intake and falling with vegetable protein intake. Bone loss was observed to increase with increasing ratio of animal to vegetable protein even before adjustment for total protein. Feskanich (1996) found a 25% increase in risk of forearm fracture as animal protein intake rose from 50 g per day or less to 80 g per day or more. There was no apparent effect of animal protein on hip fracture risk. Change in vegetable protein intakes from less than 12 g per day to 20 g per day or more showed no apparent effect. However, considering only Sellmeyer (2001) and Feskanich (1996) gives a misleading impression of the balance of evidence. Hannan (2000) found reduced bone loss at the hip and spine over four years in individuals in the highest quartile of animal protein intake, whether measured in grams per day or as a percentage of calories. Kerstetter (2000) found BMD of the femur to be 3.5% higher in the top quartile of protein intake compared with the bottom quartile. No distinction was made between animal and vegetable protein. Munger (1999) found a 70% reduction in hip fracture risk in the highest quartile of animal protein intake compared with vegetable protein intake. Heaney (1998) reviews studies on protein intake and bone health up to 1998 noting that 3 showed and adverse effect, three showed a beneficial effect and two showed no significant effect. Heaney argues that the effect of protein on bone will be modified substantially by the associated ratio of calcium to protein, suggesting that there should be no adverse effect of protein on bone if about 20 mg of calcium are consumed for each gram of protein. That is, the effect of animal protein will depend on the ratio of high calcium dairy products to other animal protein sources. It is also likely that the effect of protein will be different as protein intake increases to adequate levels and then moves beyond such levels. There is some evidence that protein requirements may be higher in older adults than in younger adults (Hannan, 2001). Heaney (2001b), in an editorial on Sellmeyer (2001), argues that there is no valid scientific reason for making a distinction between animal and vegetable protein. Heaney notes correctly that grain protein is higher in sulphur amino acids than many meat proteins. However, the concentrated plant proteins that would be used to increase protein intake on a vegan diet, such as soy products and beans, are relatively low in sulphur amino acids. Moreover, other components of plant sources of protein, particularly potassium and bicarbonate, also exert an influence on calcium balance and, with the exception of grains, this influence is markedly in favour of vegetable sources of protein. The evidence on protein strongly supports an overall benefit for bone health of higher protein intakes, provided a good calcium balance is maintained and the diet is not excessively acidic. The ratio of animal to vegetable protein does not adequately capture these provisos, so conflicting results are to be expected. Replacing protein from meat, fish or eggs with protein from milk or yoghurt will improve calcium balance. Eliminating all animal proteins and living almost exclusively on grains can be expected to be harmful. Replacing meat, fish or eggs with soy and other legumes will benefit bone health, as will replacing milk with green leafy vegetables. References Agnusdei (1998): D Agnusdei et al., Calcified Tissue International, 1998; 63: 197-201, Age-related decline of bone mass and intestinal calcium absorption in normal males. Baran (1990): Daniel Baran et al., Journal of Clinical Endocrinology and Metabolism, 1990; 70: 264270, Dietary modification with dairy products for preventing vertebral bone loss in premenopausal women: a three-year prospective study. Barger-Lux (1995): M Janet Barger-Lux et al., Journal of Clinical Endocrinology and Metabolism, 1995; 80: 406-411, An investigation of sources of variation in calcium absorption efficiency. Barger-Lux (1995b): M J Barger-Lux and R P Heaney, Osteoporosis International, 1995; 5: 97-102, Caffeine and the calcium economy revisited. Barzel (1998): Uriel S Barzel and Linda K Massey, Journal of Nutrition, 1998; 128: 1051-1053, Excess dietary protein can adversely affect bone. Benway (1993): Denise A Benway and Connie M Weaver, Journal of Food Science, 1993; 58: 605-608, Assessing chemical form of calcium in wheat, spinach and kale. Binkley (2000): Neil Binkley and Diane Krueger, Nutrition Reviews, 2000; 58: 138-144, Hypervitaminosis A and bone. Booth (2000), Sarah L Booth et al., American Journal of Clinical Nutrition, 2000; 71: 1201-8, Dietary vitamin K intakes are associated with hip fracture but not with bone mineral density in elderly men and women. Breslau (1988): Neil A Breslau et al., Journal of Clinical Endocrinology and Metabolism, 1988; 66: 140146, Relationship of animal protein-rich diet to kidney stone formation and calcium metabolism. Bushinsky (2000): David A Bushinsky and Kevin K Frick, Current Opinion in Nephrology and Hypertension, 2000; 9: 369-379, The effects of acid on bone. Chapuy (1992): Marie C Chapuy et al., The New England Journal of Medicine, 1992; 327: 1637-1642, Vitamin D3 and calcium to prevent hip fractures in elderly women. Chapuy (1994): Marie C Chapuy et al., British Medical Journal, 1994; 308: 1081-1082, Effect of calcium and cholecalciferol treatment for three years on hip fractures in elderly women. Cumming (1997): Robert G Cumming et al., American Journal of Epidemiology, 1997; 145: 926-934, Calcium intake and fracture risk: results from the Study of Osteoporotic Fractures. Dawson-Hughes (1997), Bess Dawson-Hughes et al., The New England Journal of Medicine, 1997; 337: 670-676, Effect of calcium and vitamin D supplementation in men and women 65 years of age or older. Devine (1995); Amanda Devine et al., American Journal of Clinical Nutrition, 1995; 62: 740-745, A longitudinal study of the effect of sodium and calcium intakes on regional bone density in postmenopausal women. Eaton (1991): S Boyd Eaton and Dorothy A Nelson, American Journal of Clinical Nutrition, 1991, 54; 281S-7S, Calcium in evolutionary perspective. Ensrud (2000): Kristine E Ensrud et al., Annals of Internal Medicine, 2000; 132: 345-353, Low fractional calcium absorption increases the risk for hip fracture in women with low calcium intake. Feskanich (1996): Diane Feskanich et al., American Journal of Epidemiology, 1996; 143: 472-479, Protein consumption and bone fractures in women. Feskanich (1997): Diane Feskanich et al., American Journal of Public Health, 1997; 87: 992-997, Milk, dietary calcium and bone fractures in women: a 12-year prospective study. Feskanich (1998): Diane Feskanich et al., Epidemiology, 1998, Vitamin D receptor genotype and the risk of bone fractures in women. Feskanich (1999): Diane Feskanich et al., American Journal of Clinical Nutrition, 1999; 69: 74-79, Vitamin K intake and hip fractures in women: a prospective study. Feskanich (2002): D Feskanich et al., JAMA- Journal of the American Medical Association, 2002; 287: 47-54, Vitamin A intake and hip fractures among postmenopausal women. Frassetto (1996): Lynda A Frassetto et al., American Journal of Physiology, 1996; 271: F1114-F1122, Effect of age on blood acid-base composition in adult humans: role of age-related renal functional decline. Frassetto (2000): Lynda A. Frassetto et al., Journal of Gerontology: Medical Sciences, 2000; 55A: M585M592, Worldwide incidence of hip fracture in elderly women: relation to the consumption of animal and vegetable foods. Fujiwara (1997): Saeko Fujiwara et al., Journal of Bone and Mineral Research, 1997; 12: 998-1004, Risk factors for hip fracture in a Japanese cohort. Giannini (1998): S Giannini et al., Clinical Nephrology, 1998; 50: 94-100, Bone density and skeletal metabolism are altered in idiopathic hypercalciuria. Giovannucci (1998): Edward Giovannucci et al., Cancer Research, 1998; 58: 442-447, Calcium and fructose intake in relation to risk of prostate cancer. Gonnelli (2001): Stefano Gonelli et al., Intestinal calcium absorption in normal men and women, in Nutritional Aspects of Osteoporosis, ed. Peter Burckhardt et al, 2001, ISBN 0-12-141703-4 Hannan (2001): Marian T. Hannan, Dietary protein and effects upon bone health in elderly men and women, in Nutritional Aspects of Osteoporosis, ed. Peter Burckhardt et al, 2001, ISBN 0-12-141703-4 Hannan (2000): Marian T Hannan et al., Journal of Bone and Mineral Research, 2000; 15: 2504-2512, Effect of dietary protein on bone loss in elderly men and women: the Framingham osteoporosis study. Hardwick (1990): Laurie L Hardwick et al., Journal of Nutrition, 1990; 121: 13-23, Magnesium absorption: mechanisms and the influence of vitamin D, calcium and phosphate. Heaney (1986): Robert P Heaney and Robert R Recker, American Journal of Clinical Nutrition, 1986; 43: 299-305, Distribution of calcium absorption in middle-aged women. Heaney (1994): Robert P Heaney, Journal of Bone and Mineral Research, 1994; 9: 1621-1627, Determinants of endogenous fecal calcium in healthy women. Heaney (1998): Robert P Heaney, Journal of Nutrition, 1998; 128: 1054-1057, Excess dietary protein may not adversely affect bone. Heaney (1999): Robert P Heaney et al., Osteoporosis International, 1999; 9: 13-18, Urinary calcium in perimenopausal women: normative values Heaney (2000): Robert P Heaney, American Journal of Clinical Nutrition, 2000; 72: 758-61, Dietary protein and phosphorus do not affect calcium absorption. Heaney (2000b): Robert P Heaney, American Journal of Clinical Nutrition, 2000; 71: 658-661, There should be a dietary guideline for calcium. Heaney (2000c): Robert P Heaney, Journal of the American College of Nutrition, 2000; 19: 83S-99S, Calcium, dairy products and osteoporosis. Heaney (2000d): Robert P Heaney, The dairy controversy: facts, questions, and polemics, in Nutritional Aspects of Osteoporosis, ed. Peter Burckhardt et al, 2001, ISBN 0-12-141703-4 Heaney (2001): Robert P Heaney, Nutrition Reviews, 2001; 59: 327-334, The bone remodelling transient: interpreting interventions involving bone-related nutrients. Heaney (2001b): Robert P Heaney, American Journal of Clinical Nutrition, 2001; 73: 5-6, Protein intake and bone health: the influence of belief systems on the conduct of nutritional science. Hirota (1992): Takako Hirota et al., American Journal of Clinical Nutrition, 1992; 55: 1168-1173, Effect of diet and lifestyle on bone mass in Asian young women. Ho (2001): S C Ho et al., Osteoporosis International, 2001; 12: 723-731, Sodium is the leading dietary factor associated with urinary calcium excretion in Hong Kong Chinese adults. Holbrook (1988): Troy L Holbrook et al., The Lancet, 1988; ii:1046-1049, Dietary calcium and risk of hip fracture: 14-year prospective population study. Honkanen (2001): Risto Honkanen et al., Effect of calcium on bone loss and fractures according to estrogen repletion status, in Nutritional Aspects of Osteoporosis, ed. Peter Burckhardt et al, 2001, ISBN 0-12-141703-4 Hu (1993): Ji-Fan Hu et al., American Journal of Clinical Nutrition, 1993; 58:219-227, Dietary calcium and bone density among middle-aged and elderly women in China. Institute of Medicine, (1997): Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D and fluoride, 1997, ISBN 0-309-06403-1. Johansson (2001): S Johansson and H Melhus, Journal of Bone and Mineral Research, 2001; 16: 18991905, Vitamin A antagonises calcium response to vitamin D in man. Kerstetter (2000): J E Kerstetter et al., Calcified Tissue International, 2000; 63: 313, Low dietary protein and low bone density. Knapen (1989): Marjo H J Knapen et al., Annals of Internal Medicine, 1989; 111: 1001-1005, The effect of vitamin K supplementation on circulating osteocalcin (bone Gla protein) and urinary calcium excretion. Kruger (1998): M C Kruger et al., Aging Clinical and Experimental Research, 1998; 10: 385-394, Calcium, gamma-linolenic acid and eicosapentaenoic acid supplementation in senile osteoporosis. Lau (2000): E M C Lau et al., Journal of Bone and Mineral Research, 2001; 16: 572-580, Risk factors for hip fracture in Asian men and women: the Asian Osteoporosis Study. Lemann (1993): Jacob Lemann Jr et al., Journal of Nutrition, 1993; 123: 1623-1626, Potassium causes calcium retention in healthy adults. Lips (1996): Paul Lips et al., Annals of Internal Medicine, 1996; 124: 400-406, Vitamin D supplementation and fracture incidence in elderly persons: a randomized, placebo-controlled clinical trial. Massey (1996): Linda K Massey and Susan J Whiting, Journal of Bone and Mineral Research, 1996; 11: 731-736, Dietary salt, urinary calcium and bone loss. McCance and Widdowson (1991): McCance and Widdowson: The composition of Foods (Fifth edition, 1991, HMSO). Melhus (1998): Hakan Melhus et al., Annals of Internal Medicine, 1998; 129: 770-778, Excessive dietary intake of vitamin A is associated with reduced bone mineral density and increased risk for hip fracture. Miller (2000): Gregory D Miller et al., 2000, Handbook of Dairy Foods and Nutrition, National Dairy Council, ISBN 0-8493-8731-0. Milton (1999): Katharine Milton, Nutrition, 1999; 15: 488-498, Nutritional characteristics of wild primate foods: do the diets of our closest living relatives have lessons for us? Munger (1999): Ronald G Munger et al., American Journal of Clinical Nutrition, 1999; 69: 147-152, Prospective study of dietary protein intake and risk of hip fracture in postmenopausal women. Need (1998): A G Need et al., Clinical Endocrinology, 1998; 48: 163-168, Intestinal calcium absorption in men with spinal osteoporosis. New (2000): Susan A New et al., American Journal of Clinical Nutrition, 2000; 71: 142-151, Dietary influences on bone mass and bone metabolism: further evidence of a positive link between fruit and vegetable consumption and bone health? Nordin (1999): B E C Nordin et al., Osteoporosis International, 1999, 9: 351-357, Biochemical variables in pre- and postmenopausal women: reconciling the calcium and estrogen hypotheses. Peacock (2000): Munro Peacock et al., Journal of Clinical Endocrinology and Metabolism, 2000; 85: 3011-3019, Effect of calcium and 25OH vitamin D3 dietary supplementation and bone loss at the hip in men and women over the age of 60. Recker (1977): Robert R Recker et al., Annals of Internal Medicine, 1977; 87: 649-655, Effect of estrogens and calcium carbonate on bone loss in postmenopausal women. Recker (1985): Robert R Recker and Robert P Heaney, The American Journal of Clinical Nutrition, 1985; 41: 254-263, The effect of milk supplements on calcium metabolism, bone metabolism and calcium balance. Recker (1996): Robert R Recker et al., Journal of Bone and Mineral Research, 1996; 11: 1961-1966, Correcting calcium nutritional deficiency prevents spine fractures in elderly women. Reid (1995): Ian R Reid et al., The American Journal of Medicine, 1995; 98: 331-335, Long-term effects of calcium supplementation on bone loss and fractures in postmenopausal women: a randomized controlled trial. Remer (1994): Thomas Remer and Friedrich Manz, American Journal of Clinical Nutrition, 1994; 59: 1356-61, Estimation of the renal net acid excretion by adults consuming variable amounts of protein. Remer (1995): Thomas Remer and Friedrich Manz, Journal of the American Dietetic Association, 1995; 95: 791-797, Potential renal acid load of foods and its influence on urine pH. Requirand (2000): P Requirand et al., Clinical Nutrition, 2000; 19: 271-276, Serum fatty acid imbalance in bone loss: example with periodontal disease. Riggs (1998): B Lawrence Riggs et al., Journal of Bone and Mineral Research, 1998; 13: 763-773, A unitary model for involutional osteoporosis: estrogen deficiency causes both type I and type II osteoporosis in postmenopausal women and contributes to bone loss in aging men. Riggs(1998b): B Lawrence Riggs et al., Journal of Bone and Mineral Research, 1998; 13: 168-174, Long-term effects of calcium supplementation on serum parathyroid hormone level., bone turnover, and bone loss in elderly women. Sebastian (1994): Anthony Sebastian et al., The New England Journal of Medicine, 1994; 330: 17761781, Improved mineral balance and skeletal metabolism in postmenopausal women treated with potassium bicarbonate. Sellmeyer (2001): Deborah E Sellmeyer et al., American Journal of Clinical Nutrition, 2001; 73: 118122, A high ratio of dietary animal to vegetable protein increases the rate of bone loss and the risk of fracture in postmenopausal women. Shearer (1996): Martin J Shearer et al., Journal of Nutrition, 1996; 126: 1181S-1186S, Chemistry, nutritional sources, tissue distribution and metabolism of vitamin K with special reference to bone health. Sojka (1995): J E Sojka and C M Weaver, Nutrition Reviews, 1995; 53: 71-80, Magnesium supplementation and osteoporosis. Tucker (1999): Katherine L Tucker et al., American Journal of Clinical Nutrition, 1999; 69:727-36, Potassium, magnesium, and fruit and vegetable intakes are associated with greater bone mineral density in elderly men and women. USDA (1999), U.S. Department of Agriculture, Agricultural Research Service, 1999, USDA nutrient database for standard reference, Release 13, Nutrient data laboratory home page, http://www.nal.usda.gov/fnic/foodcomp Uusi-Rasi (1998): Kirsti Uusi-Rasi et al., Journal of Bone and Mineral Research, 1998; 13: 133-142, Associations of physical activity and calcium intake with bone mass and size in healthy women at different ages. Watkins (2001): Bruce A Watkins et al., Experimental Biology and Medicine, 2001; 226: 485-497, Omega-3 polyunsaturated fatty acids and skeletal health. Weaver (1993): C M Weaver et al., Journal of Food Science, 1993; 58: 1401-1403, Absorbability of calcium from common beans. Weaver (1997): C M Weaver et al., Journal of Food Science, 1997; 62: 524-525, Calcium bioavailability from high oxalate vegetables: Chinese vegetables, sweet potatoes and rhubarb. Weaver (1999): Connie M Weaver et al., American Journal of Clinical Nutrition, 1999; 70: 543S-548S, Choices for achieving adequate dietary calcium with a vegetarian diet. Weber (2001): Peter Weber, Nutrition, 2001; 17: 880-887, Vitamin K and bone health. Wolff (1999): I Wolff et al., Osteoporosis International, 1999; 9:1-12, The effect of exercise training programs on bone mass: a meta-analysis of published controlled trials in pre- and postmenopausal women. Notes Stephen Walsh holds the copyright to this paper. It may be reproduced freely but only in full, including this copyright declaration. Stephen Walsh may be contacted by email: stephenwalsh@vegans.fsnet.co.uk The Vegan Society (7 Battle road, St Leonards-on-sea, East Sussex, TN37 7AA) may be contacted by email (info@vegansociety.com) and has a website www.vegansociety.com Acknowledgements My thanks to Vanessa Clarke for editing successive drafts of this paper in the interests of clarity.

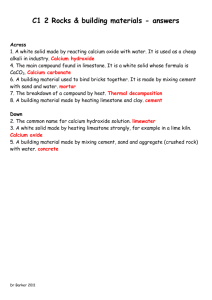




![2012 [1] Rajika L Dewasurendra, Prapat Suriyaphol, Sumadhya D](http://s3.studylib.net/store/data/006619083_1-f93216c6817d37213cca750ca3003423-300x300.png)