Male Erectile Dysfunction :
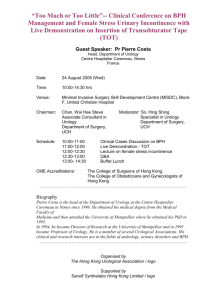
advertisement

Proceedings of the Annual Meetings of the World Chinese Urological Society (WCUS) 2006 - 2011 Editors: Kew-Kim Chew Run Wang Tom F Lue Contents Page The World Chinese Urological Society 2 Tom F Lue The Scientific Committee 4 Run Wang The Proceedings 5 Kew-Kim Chew World Chinese Urological Society (WCUS) Meetings 1. WCUS Meeting 2006 6 Message Program 7 9 2. WCUS Meeting 2007 12 Message Scientific Committee Program Abstracts 13 15 18 24 3. WCUS Meeting 2008 65 Program 66 4. Meeting 2009 72 Message Program 73 75 5. WCUS Meeting 2010 82 Message Program 83 85 6. WCUS Meeting 2011 91 Message Program 92 94 1 The World Chinese Urological Society Tom F Lue MD ScD (Hon) FACS Founded by 8 urologists on 22 February 1902, the American Urological Association (AUA), with a membership in 2011 of 17,690 including 3,877 international members, has been holding annual meetings at which world-class urologists and uroscientists give state-of-the-art lectures and present new discoveries in plenary sessions, poster sessions, symposiums and postgraduate courses. There are more than 10,000 urologists of Chinese decent in the world and many have actively participated in the activities of the AUA. In 2005, the then AUA President Dr. Joseph N. Corriere Jr. and Secretary Dr. Carl A. Olsson authorized the establishment of a Chinese urology program at the annual AUA meeting. This idea received much enthusiastic support from Chinese urologists worldwide and the first World Chinese Urological Society (WCUS) meeting at the AUA was held in Atlanta, Georgia, on 20 May 2006. In 2009, the WCUS became an official affiliate society of the AUA. At the inaugural meeting in 2006, three academicians, Yinglu Guo, Luke S. Chang and Tung-Tien Sun were among the moderators. The presidents of 5 Chinese urological associations gave the State-of-Chinese-Urology lectures. They were Yanqun Na, Chinese Urological Association; Dah-Shyong Yu, Taiwan Urological Association; Christopher Cheng, Singapore Urological Association; Chi Wai Man, Hong Kong Urological Association and Ho Chun, Macao Urological Association. Leland Chung helped arrange the local program. This highest level of enthusiastic support was unprecedented in the history of urology. It opened a new era of cooperation, friendship, respect and love among Chinese urologists and uroscientists. 2 The number of participants in the WCUS had increased to about 500 at the 2010 San Francisco AUA meeting, thanks to the hard work of the Scientific Committee headed by Run Wang. The scientific program has also changed from presentations toward more expert lectures and “take home messages”, in response to comments and suggestions by participants and officials from the 5 urological associations. At this time, we do not have an “official” organization and membership. We are very grateful to Pfizer, American Medical Systems and Bayer for their generous support to make the meetings possible. The WCUS is one of the most successful affiliate societies of the AUA. Despite a number of growing pains and financial difficulty, it has survived and is growing stronger. It is time that we review our goals and purpose, and plan ahead for the future. The Society will thrive only if more urologists and uroscientists of Chinese decent participate, contribute and lead. We hope the WCUS will be one of the best urological societies in the world in the not too distant future. 3 The Scientific Committee Run Wang MD FACS The most important event at the present time for WCUS is the Annual Meeting at the AUA. Ensuring a high quality program is the major task of the Scientific Committee. Year after year, many talented individuals volunteer their time and expertise to select the best topics that cover cutting edge progress in urology, particularly amongst the Chinese urological community worldwide. Each regional society is also actively involved in the selection of speakers that will well represent the respective society. The Proceedings reminds us of the unselfish contributions of all the Committee members and the hard work from each regional society. Having the WCUS as one of the most attended sub-specialty meetings at the AUA is a great reward for the efforts of all the speakers and moderators. 4 The Proceedings Kew-Kim Chew MBBS PhD FRCPEdin FRCPGlasg With a record of the Inaugural Meeting and all the subsequent Annual Meetings, The Proceedings has provided the historical perspective to the World Chinese Urological Society (WCUS) from its inception in 2006. Attendances at these Meetings are an indication of the relentless enthusiasm of the many Chinese Urologists from all over the world. The presentations on basic science, epidemiological and clinical research represent some of the magnificent achievements and significant contributions to knowledge in the fields of Urology, Sexual Medicine and Andrology. For the attendees, The Proceedings is a reminder of their participation at these Meetings in the pursuit and sharing of knowledge. For those who had been unable to attend, it provides a summary of events and possibly a source of inspiration for the awakening of talent and professional advancement. 5 1. WCUS Meeting 2006 Date: Saturday, May 20, 2006 Venue: Hyatt Regency, Atlanta, Georgia, USA Theme: State-of-Chinese Urology 6 The Inaugural Pre-AUA Meeting of the World Chinese Urological Association Tom F. Lue and Leland W. K. Chung Thanks to the great efforts of president Corriere and secretary Olsson, the inaugural meeting of the World Chinese Urological Association will take place in Atlanta prior to the Annual Meeting of the AUA on May 20, 2006. This opportunity is warmly embraced by the Chinese-speaking urologists and urological scientists from China, Taiwan, Singapore, Hong Kong and other countries who regularly attend the AUA annual convention. The spirit of this inaugural meeting sponsored by AUA is to provide a forum for exchanging views among Chinese and nonChinese speaking urologists and urological scientists, which will be a real asset for our professional communications. This is a timely and even historic event, expanding the current spectrum of international coverage of the AUA meeting. We are particularly pleased to see the AUA leadership endorse this meeting since an increasing number of Chinese-speaking urologists and urological scientists attend the AUA meeting. Recent economic growth and political changes in mainland China have increased the number of Chinese urologists and urological scientists who visit institutions around the world, establish joint research and training centers, and attend international meetings. There are more than 10,000 Chinese speaking urologists in the world and many of them consider the AUA Annual Meeting to be the most prestigious and significant urology meeting internationally. Language and cultural barriers that discourage them from attending the meeting have been a major hurdle for communication. In the past 10 years, the Postgraduate College of the Institutes of Urology, Peking University, Beijing, China has held many urology courses as a part of their continued education effort. These courses were taught by experts from China and abroad, and significantly elevated the quality of urological care in both urban and rural China. We anticipate that an 7 increasing number of new Chinese-speaking urologists and urological scientists will be joining the AUA. They will be eager to participate in our Annual Meeting and other organized professional activities, presenting and exchanging innovative ideas and experiences with urologists from America as well as other countries. The presidents of the Chinese Urological Association, Association of Chinese Urologists, Taiwan Urologic Association, Hong Kong Urological Association, and Singapore Urological Association will each present on the state-of-urology in their respective countries or regions. This will be followed by scientific presentations and state-of-the-art lectures on various basic and clinical topics by top urologists and urologic scientists. To facilitate free communication and interchange of ideas, and foster closer ties and friendship among the participants, the language of the first meeting will be Mandarin Chinese. The meeting will be held in Hyatt Hotel and will be open to all who are interested in participating in this exciting new AUA event. 8 Program - 2006 8:00 - 8:10 am Welcome and introduction Tom F. Lue, USA 8:10 - 9:10 am Session I: State-of-Chinese Urology Moderators: Yinglu Guo, China and Luke S. Chang, Taiwan Yanqun Na, President, Chinese Urological Assoc. Dah-Shyong Yu, President, Taiwan Urological Assoc. Christopher Cheng, President, Singapore Urological Assoc. Chi Wai Man, President, Hong Kong Urological Assoc. Ho Chun, President, Macao Urological Assoc. 9:10 - 10:30 am Session 2: Scientific Program Upper urinary tract Moderators: Yanqun Na, China and Leland Chung, USA Treatment of staghorn calculi by Chinese minimally invasive percutaneous nephrolithotomy Xun Li, China Retroperitoneal laparoscopic ureteropyeloplasty Liqun Zhou, Nichen Li,Zhisong He, Ming Li, Shiliang Wu,Yanqun Na and Yinglu Guo, China Retroperitoneal laparoscopic techniques for nephron-sparing surgery: the experience of Tongji Hospital Xu ZHANG, China Complete laparoscopic approaches to adrenal tumors— from hand-assisted to pure needlescopic instruments Shih-Chieh Chueh, Taiwan Discussion 10:30 - 10:45 am Tea and Coffee Break 10:45 - 12:00 noon Session 3: Scientific Program 9 Lower urinary tract Moderators: Lili Liang, China and Tung-Tien Sun, USA The management pathway for patients with LUTS Keong Tatt Foo, Singapore Continence urinary diversion in Hong Kong Bill Tak-Hing Wong, Hong Kong Is low PSA cutoff point applicable to Chinese men? Ming Li, China What’s new in urinary incontinence research? Donna Deng, USA Discussion 12:00 - 1:00 pm: Box Lunch Special Lecture: History of Chinese Urology Yinglu Guo, China 1:00 - 2:15 pm Session 4: Scientific program: Basic research Moderators: Kew Kim Chew, Australia, and Ju-Ton Hsieh, Taiwan Central control of sexual function Kuang-Kuo Chen, Jen-Hwey Chiu, and Luke S. Chang, Taiwan Traditional Chinese medicine in ED and PE Zhong Cheng Xin, China Akt-mediated phosphorylation of Ezh2 suppresses lysine 27 methylation in histone H3 Tai-Lung Cha, Guang-Huan sun, Dah-Shyong Yu, Sun-Yran Chang, Mien-Chie Hung, Taiwan Androgen receptor functions as suppressor to prostate metastatic tumor invasion: new challenge to current androgen ablation therapy. Chawnshang Chang, USA Discussion 2:15 - 2:30 pm: Tea and Coffee Break 2:30 - 3:45 pm Session 5: Scientific Program 10 Topics of interest Moderators: Hui Meng Tan, Malaysia and Run Wang, USA Epidemiological studies on the prevalence of upper urinary calculi in Taiwan Lee YH, Chang LS, Taiwan Innovative techniques in GU surgery Rei K. Chiou, USA How to advance in the world of urology by Chinese urologists Chung Lee , USA Penile transplantation: a case report Weilie Hu, China Discussion 3:45 - 4:00 pm Closing Remarks Yanqun Na, China & Luke S. Chang, Taiwan 11 2. WCUS Meeting 2007 Date: Saturday, May 19, 2007 Venue: The Hilton Towers, Anaheim, California, USA Theme: State-of-World Chinese Urology 12 Welcome to WCUS meeting 2007 Dear Colleagues and Friends: On behalf of the scientific committee, it is our great pleasure to invite you to attend the 2nd AUA World Chinese Urological Society (WCUS) meeting which will be held at the Hilton Anaheim hotel in Anaheim, California on May 19, 2007. The 1st AUA WCUS meeting held in Atlanta, Georgia in 2006 was a great success with more than 300 Chinese-speaking urologists and urologic scientists attending the meeting. The 2007 meeting in Anaheim promises to be an even more exciting event. The meeting will begin with a series of lectures by the presidents of the urological associations of China, Taiwan, Singapore, Hong Kong and Macao on the “Highlights of Chinese Urology.” Following these lectures, experts in various fields – including benign prostatic enlargement, bladder cancer, endourology, pediatric urology, Nanomedicine and urinary stones – will lecture on “Practical Approaches to Patient Management.” In light of the tremendous advancements in basic and clinical research from the countries and regions mentioned above, we have also invited many accomplished urologists and scientists to present their findings and discoveries. In addition, the conference will feature a poster session that will provide yet another venue for discussion with the experts. The purpose of the AUA WCUS meeting is to facilitate exchange of ideas and experiences and foster communication and collaboration among Chinese-speaking urologists and urological scientists. Our goal is to attract the best and brightest Chinese scholars to attend and present at the annual AUA meetings. Although the presentations will be in Mandarin, the slides and posters will be in English. We welcome anyone with an interest in Chinese urology to attend the meeting. 13 Tom F. Lue, MD, FACS Chairman, Scientific Committee Run Wang, MD, FACS Executive Chairman, Scientific Committee Guiting Lin, MD, PhD Secretary 14 Scientific Committee - 2007 Tom F. Lue, MD, FACS-Chair (USA) Department of Urology University of California at San Francisco USA tlue@urology.ucsf.edu Run Wang, MD, FACS-Executive Chair (USA) Department of Urology University of Texas Medical School at Houston University of Texas MD Anderson Cancer Center USA Run.Wang@uth.tmc.edu Yinghao Sun, MD, PhD (Shanghai) Department of Urology The 2nd Military Medical University Shanghai China sunyh@medmail.com.cn Hong Li, MD (Chengdu) Department of Urology Sichuan University Chengdu China hy7580@126.com Ningchen Li, MD (Beijing) Beijing Urology Institute Beijing University Beijing China ningchenli@yahoo.com Liqun Zhou, MD (Beijing) Beijing Urology Institute Beijing University Beijing China zhoulqmail@china.com 15 Yutian Dai, MD, PhD (Nanjing) Department of Urology Nanjing University Medical College Nanjing China ytdai@hotmail.com Joseph Chin, MD (Canada) Department of Urology University of West Ontario London Canada Joseph.Chin@lhsc.on.ca Eugen Yuhui Wang, MD, PhD (Sweden and Norway) Department of Urology Aker University Oslo Norway yuhuiwang@msn.com Shu Tung, MD (USA) Division of Urology University of Texas Medical School at Houston USA Tung.Shu@uth.tmc.edu Philip Li, MD (USA) Department of Urology Cornell University Medical School New York USA psli@med.cornell.edu Jun Chen, MD (Taiwan) chenjun@ha.mc.ntu.edu.tw Ian Lap Hong, MD, PhD (Macau) Department of Urology CHCSJ Hospital Macau China ianlap@macau.ctm.net 16 In-Hei Lee, MD (Taiwan) yhlee@mail.chimei.org.tw Tak-Hing Bill Wong, MD, FRCS (Hong Kong) Department of Urology Chinese University of Hong Kong Hong Kong China billwong@pedderclinic.hk Apichat Kongkanand, MD (Thailand) Bangkok Thailand Kongkanand@yahoo.com Hui Ming Tan, MD (Malaysia) Kuala Lumpur Malaysia perandro@streamyx.com Keong Foo, MD (Singapore) keongfoo@yahoo.com Leland Chung, PhD (USA) Emory University Atlanta USA lwchung@emory.edu Kew- Kim Chew, MD, PhD (Australia) Perth Australia kewkimchew@hotmail.com 17 Program - 2007 8:00 - 8:07 am Welcome and introduction Tom F. Lue, USA 8:07 - 8:10 am Report from Scientific Program Committee Run Wang, USA 8:10 - 9:00 am Session 1: Highlight on Chinese Urology Moderators: Chung Lee, USA; Luke S. Chang, Taiwan; Tak-Hing Bill Wong, Hong Kong 8:10 - 8:20 am 8:20 - 8:30 am 8:30 - 8:40 am 8:40 - 8:50 am 8:50 - 9:00 am Yanqun Na, President, Chinese Urological Assoc. Han-Sun Chiang, President, Taiwan Urological Assoc. Christopher Cheng, President, Singapore Urological Assoc. Wai Sang Wong, President, Hong Kong Urological Assoc. Son Fat Ho, President, Macao Urological Assoc. 9:00 - 9:10 am WCUS awards 9:10 -10:30 am Session 2: Scientific Program Practical Approach to Patient Management Moderators: Yanqun Na, China; Leland Chung, USA; Apichat Kongkanand, Thailand 9:10 - 9:30 am Revisit balloon dilation for BPH: 10-year experience Yinglu Guo, Liqun Zhou, China (Abstract 1) 9:30 - 9:50 am How do I manage patient with bladder cancer? Joseph Chin, Canada (Abstract 2) 9:50 - 10:10 am How do I handle difficult urological problems in children? Chung Kwong Yeung, Hong Kong (Abstract 3) 10:10 - 10:30 am Tricks on Management of Urinary Stone Disease? Marshall Stoller, USA (Abstract 4) 18 10:30 - 10:45 am Tea and Coffee Break 10:45 - 12:00 noon Session 3: Scientific Program Basic Science Forum Moderators: Dalin He, China; Philip Li, USA; Hui Meng Tan, Malaysia 10:45 - 11:00 am Nanotechnology, Nanomedicine, and Nanosurgery: An Urologist’s Perspective Joseph C. Liao, USA (Abstract 5) 11:00 - 11:15 am Intravesical and intraprostatic botulinum toxin administration in rat models of interstitial cystitis and non-bacteria prostatitis ( Yao-Chi Chuang, Naoki Yoshimura, Chao-Cheng Huang, Po-Hui Chiang, Pradeep Tyagi, and Michael B. Chancellor, Taiwan and USA (Abstract 6) 11:15 - 11:30 am Effect of changes of detrusor-original excitability on the overactive detrusor Bo Song, China (Abstract 7) 11:30 - 11:45 am Bladder primary sensory neuron block: animal and clinical application Zhichen Guan, China (Abstract 8) 11:45 - 12:00 noon Discussion 12 Noon - 1:00 pm Box Lunch and Viewing of Posters and Videos 1:00 pm - 2:00 pm Session 4: Scientific program Discussion of Posters and Videos Moderators: Shujie Xia, China; Eugen Y. Wang, Sweden; Jun Chen, Taiwan Upper Urinary Tract 1:00 - 1:03 pm Pyeloplasty: retroperitoneal laparoscopic vs. open approaches Xu Zhang, China (Abstract 9) 19 1:03 - 1:06 pm Graft Outcome of Living Donor Renal Transplantation in the Elderly Recipients Feng-Pin Chuang, Andrew C Novick, Guang-Huan Sun, Michael Kleeman, Stuart Flechner, V. Krishnamurthi, Charles Modlin, Daniel Shoskes, David A.Goldfarb, Taiwan and USA (Abstract 10) 1:06 - 1:09 pm Laparoscopic repair of injury to the inferior vena cava-report of three cases (Video) Liqun Zhou, China (Abstract 11) 1:09 - 1:12 pm Retroperitoneal laparoscopic Radical Nephrectomy and regional lymphadenectomy for Renal Cell Carcinomas Wei Zhang, China (Abstract 12) 1:12 - 1:15 pm Correlation of COX-2 Expression in Stromal Cells with High Stage, High Grade and Poor Prognosis in Urothelial Carcinoma of Upper Urinary Tracts Chih-Hsiung Kang, Po-Hui Chiang, Shun-Chen Huang, and Hsuang-Lan Yu, Taiwan (Abstract 13) 1:15 - 1:18 pm Endoluminal ureteroplasty for ureteroenteric stricture – a feasibility study in porcine model. Victor Chia-Hsiang Lin, Allen W. Chiu, Mihir M. Desai, Inderbir S. Gill,Taiwan and USA (Abstract 14) 1:18 - 1:21 pm Laparoscopic radical nephroureterectomy with concomitant radical cystectomy for multi-focal transitional cell carcinoma in uremic patients: initial experience Victor C. Lin, Allen W. Chiu, Y. H. Lee, T. J. Yu, Taiwan (Abstract 15) Prostatic Diseases 1:21 - 1:24 pm Prostate cancer management consensus and guidelines between China and Taiwan Chih-cheng Lu, Chia-Ho Lin, Dennis Chian-Shiung Lin, Eric W. Fan, TseChou Cheng, Taiwan (Abstract 16) 1:24 - 1:27 pm The guidelines or consensus in managing benign prostatic hyperplasia among China, Singapore and Taiwan Chih-cheng Lu, Chia-Ho Lin, Dennis Chian-Shiung Lin, Eric W. Fan, TseChou Cheng, Taiwan (Abstract 17) 20 1:27 - 1:30 pm Hemospermia associated with prostatic cyst: diagnosis by transrectal ultrasonographic finding and endorectal coil MR imaging. Twenty four case reports Wei-Dong Song, Liang Chen, Zhong-Cheng Xin, Long Tian, Bao-Xing Liu, Xiao-Jun Wu,China (Abstract 18) Andrology 1:30 - 1:33 pm China experience of penile prosthesis implantation for sever erectile dysfunction Zhong Cheng Xin, Zhi Chao Zhang, Wei Dong Song, Long Tian, China (Abstract 19) 1:33 - 1:36 pm Sural Nerve Grafting During Laparoscopic Radical Prostatectomy Initial experiences of two patients Xin Gao, China (Abstract 20) 1:36 - 1:39 pm Erectile Dysfunction Following Transurethral Electrovapor Resection for Different Sized Prostates Chih-Kuang Liu, Ming-Chung Ko, Huey-Sheng Jeng, Wen-Kai Lee, HongJeng Yu, Han-Sun Chiang, Taiwan (Abstract 21) 1:39 - 1:42 pm A mode of treatment for penilie incarceration ----an unusual complication of masturbation Jesun Lin, Gin-Bow Chang, Herng-Jye Jiang, Mon-I Yang, Huai-Long Tai, and Bai-Fu Wang, Taiwan (Abstract 22) 1:42 - 1:45 pm Effect of Cox7a2 on LH induced testosterone production and expression of StAR protein, P450scc and 3β-HSD enzymes in TM3 mouse Leydig cells Liang Chen,Zhong-Cheng Xin , Long Tian, Yi-Ming Yuan, Gang Liu , Ying-Lu Guo, China (Abstract 23) 1:45 - 1:48 pm Association of the phenotype of seminal vesicles and cftr gene mutation in patients with congenital bilateral absence of the vas deferens Chien-Chih Wu, Chia-Hung Liu, Han-Sun Chiang, Taiwan (Abstract 24) Urinary Bladder 1:48 - 1:51 pm Proteomic analysis of human urinary cancer proteome using reverse phase nano-high-performance liquid chromatography / electrospary ionization tandem mass spectrometry. Tan Lia-Beng, Liao Pao-Chi, and Guo Haw-Ran,Taiwan. (Abstract 25) 21 1:51 -1:54 pm Survival Analysis of Patients with Bladder Transitional Cell Carcinoma after Open or Laparoscopic Radical Cystectomy Allen W. Chiu, Thomas Y. Hsueh, Steven K. Huan, Yi-Hsiu Huang, Taiwan (Abstract 26) Stem Cells 1:54 - 1:57 pm Characterization and Differentiation of Human Muscle Derived Stem Cells. Shing-Hwa Lu, An-Hang Yang, Chou-Fu Wei, Kuang-Kuo Chen,Luke S. Chang, Taiwan (Abstract 27) 1:57 - 2:00 pm Brief Break 2:00 - 2:40 pm Session 5: CUA Lectures Moderators: Liqun Zhou, China; Shu Tung, USA; Shaw W. Zhou, USA 2:00 - 2:20 pm Endourology in China: Current status and future direction Yinghao Sun, China (Abstract 28) 2:20 - 2:35 pm Evidence-based Urology: report from China Qiang Wei, China (Abstract 29) 2:35 - 2:40 pm Discussion 2:40 - 2:50 pm Tea and Coffee Break 2:50 - 3:50 pm Session 6: Scientific Program Research Moderators: Hong Li, China; Po-Hui Chiang, Taiwan; Ningchen Li, China 2:50 - 3:05 pm The Incidence and Clinical Significance of High-Grade Prostatic Intraepithelial Neoplasia on Prostate Biopsy in Taiwanese Asian Men Yen-Hwa Chang, Yi-Chun Chiu, Chin-Chen Pan, Kuang-Kuo Chen and Luke S. Chang, Taiwan (Abstract 30) 22 3:05 - 3:15 pm Prostate cancer in Macau S.A.R Lap hong Ian, Macau (Abstract 31) 3:15 - 3:30 pm Efficacy and Safety of Tolterodine and/or Tamsulosin in Men with Lower Urinary Tract Symptoms (LUTS) Including Overactive Bladder (OAB): Results from a Four-Arm, Placebo-Controlled Trial Zhonghong (Eric) Guan, USA (Abstract 32) 3:30 - 3:40 pm Laparoscopic Radical Cystectomy with Orthotopic Ileal Neobladder: A Report of 85 Cases Jian Huang, China (Abstract 33) 3:40 - 3:50 pm "Sliding Knot Vesicourethrostomy" in LRP and LRC Ho Son Fat, Macau (Abstract 34) 3:50 - 4:00 pm Diabetic Erectile Dysfunction: Animal Studies Yu-tian Dai, Yun Chen, Run Wang, Zeyu Sun, Rong Yang, Leshen Yao, Dong Chen, Sanxiang Li, China (Abstract 35) 4:00 - 4:10 pm Discussion 4:10 - 4:20 pm Closing Remarks Yanqun Na, China & Luke S. Chang, Taiwan 23 Abstracts 1. Revisit balloon dilation for BPH: 10-year experience - The Treatment of BPH by Muti-Balloon Dilation (MBD) Yinglu Guo MD. Department of Urology, First Hospital of Peking University, Urologist Training College of Peking University. Beijing, 100034, PR China While China has stepped into the aged society, there are more then several ten millions people are suffering from the BPH. An effective and economic therapy method is eagerly required for those people of BPH because there is no good method to prevent and to eliminate it totally in China nowadays. Also, lots of other factors have blocked the process to reach this aim in China, such as equipments, skilled urologist, and the economic condition of those patients in the rural areas. The single balloon dilation, a method for treating BPH that had been applied in the clinic in the middle of 80s’, was an effective approach to treat those patients with minimum symptoms, although it has been abounded for bleeding after the dilation and the long-term effects. Ten years later, this technique has been improved into another effective method, the muti-balloon dilation (MBD), which was applied in the clinic successfully with an excellent outcome. There are several key techniques were developed for the muti-balloon dilation. To stop the bleeding after dilation, the period of dilation has been prolonged to 24 hr, which resulted the necroses and apoptosis of glands and sympathetic nerve ending in the prostate. To increase the effectiveness of dilation, several other tissues have been recruited in, such as bladder neck and urethral sphincters. It is need to be noticed that the balloon on the site of urethral sphincters was released immediately after dilation in case of the incontinence. The muti-balloon dilation has been applied to treat those BPH patients with residual urine. Five days later after the dilation, all the patients regained the urination although some of them with temporary stress incontinence. The urination was successfully improved during the post dilation period. The maximum urinate rates were reached to 11ml/s in all those patients and some of them reached to 20ml/s even after 12 years of dilation. To explore the mechanism of this new method, the animal experiments and more clinic trails will be applied. Also, the catheter and the balloon will be improved for the best outcome. 24 2. How do I manage patient with bladder cancer? Joseph Chin, MD Professor of Surgery, UWO, Head, Surgical Oncology, London Health Sciences Centre, Victoria Hospital, Canada The goals of therapy for non-invasive transitional cell bladder cancer are (1) Prevent recurrence and progression, (2) Minimize morbidity and expense e.g. with cystectomy and (3) Identify refractory/progressive disease before it becomes metastatic. One should remember that only 2% of TaG1-2 cancers progress. However, 50% of Tis progress and that 25% of T1G3 die of TCC without extirpative therapy. Sixty percent of such patients are 60% cured with radical cystectomy if they have timely aggressive intervention. Approximately 50% of those who pursue bladder–sparing therapy can be cured with radical radiotherapy with or without systemic chemotherapy, but 40% require salvage cystectomy. Low-Risk Non-Invasive Cancers Approximately 60% of newly diagnosed cases are low-risk (Grade 1 - 2, Stage Ta, T1). Transurethral resection (TUR) should include biopsy of tumor base. Since approximately 50% will recur and 15 - 25% recur with higher grade disease, the key question is whether and when to institute intravesical therapy. My criteria for intravesical therapy after initial TUR in non-invasive disease include : 1. Presence of CIS, 2. T1 disease, 3. Presence of multiple tumors, 4. Large initial tumor (>3 cm.diameter), 5. Grade 3 disease. A second TUR is performed within 6 weeks if the initial TUR failed to include muscularis propria in the specimen or if there is doubt about the completeness of the initial resection. Fluorescence-Assisted TUR may be useful in cases of suspected carcinoma in situ, to detect “occult”. In case of early recurrences (within 2 -3 moths), intravesical therapy with BCG would be instituted promptly. Another indication for intravesical therapy is presence of unresectable superficial TCC due to difficult anatomy and location. High Risk Non-Invasive Cancers Since 80% of T1 Grade 3 disease, with or without concomitant CIS, will recur and since up to 45% of these may develop invasion and eventually become metastatic, T1G3 disease has to be regarded as high-risk and treated aggressively. Intravesical therapy is used early in the disease course. The threshold for radical cystectomy should be low, if there is any early sign of failure of conservative therapy. Intravesical Therapy BCG is usually used as first-line with a 6 week-course. Maintenance regimen is routinely used monthly for 3 months. Occasionally, more intensive and longer maintenance regimens (e.g. as per Dr. Lamm) are used. Second-line therapy commonly sued are Mitomycin and low-dose BCG plus interferon. 25 Invasive Disease and Failed Treatment in Non-Invasive Disease Radical Cystectomy is usually undertaken in these circumstances, provided the patient’s operative risks are reasonable. A bladder-sparing approach, with a combination of external beam radiotherapy and systemic chemotherapy may be used, especially if the patient has high risks with medical co morbidities. The choice of urinary diversion depends on (1) patient age, (2) co-morbidities, (3) tumor stage/type/location, (4) patient preference. My personal break-down is approximately 65%/35% ileal conduit/Studer ileal neobladder. Advanced Disease Neoadjuvant chemotherapy (most commonly cis platinum and Gemcitabine combination) is used occasionally to downsize locally advanced bulky cancers in patients being considered for aggressive surgical therapy. The alternative is to proceed with cystectomy first and then institute adjuvant chemotherapy in those deemed to likely benefit from adjunctive systemic therapy. 26 3. How do I handle difficult urological problems in children? Chung Kwong Yeung, Hong Kong 27 4. Tricks on Management of Urinary Stone Disease Marshall Stoller Department of Urology, University of California at San Francisco. USA Percutaneous nephrolithotomy (PNL) Positioning and Set up: 1. Flexible cystoscopy on gurney 2. Placement of localizing ureteral catheter 3. Connect ureteral catheter to extension tubing (12-14 inches), then a syringe of contrast (flush tubing, careful not to get contrast into catheter) 4. Secure to Foley 5. Flip patient prone onto bolsters (made of rolled up blankets, gel rolls can compromise Xray/images) 6. Shoulders and elbows flexed less then 90 degrees 7. Pad all pressure points and secure patient to table 8. Ensure easy access to syringe for retrograde contrast injection Imaging: 1. Lower room lights and bring patient as close to C-arm sensor (beam should come from under the table to reduce radiation exposure) 2. Take scout film 3. Under active fluoroscopy, inject contrast via localizing catheter at a slow rate 4. Understand stone and renal collecting system anatomy 5. Lower pole inferior calyx is typically no the most inferior Access: 1. Goal is to access the posterior calyx at its tip to minimize the distance of renal tissue traversed (this will minimize bleeding) 2. The access tract should be straight onto the stone 3. 18ga needle with removable cutting inner obturator/stylet Anatomy & Puncture Site: 1. Identify the 11th and 12th rib 2. Identify the paraspinous muscles 3. Start with X-ray in AP view 4. For lower pole punctures, a. Enter skin 2cm later to the lateral edge of the paraspinous muscles and 2cm inferior to the rib (Petit’s Triangle) b. Enter at 30 degrees from the skin surface and aim towards contralateral nipple c. rotate C-arm sensor towards you to assess depth of puncture d. If the needle is under the stone your needle is too superficial 28 5. For upper pole punctures, a. Select either medial or lateral calyx b. Enter directly over stone (“bull’s eye”) c. Use packing forceps to direct needle and reduce radiation exposure d. Rotate C-arm sensor away from you to assess puncture depth 6. Aberrant anatomy may require ultrasound guidance or CT imaging Tract Dilation: 1. Once in collecting system, pass J-tip, flexible wire into collecting system do not spend much time trying to get guidewire down ureter and into bladder 2. If wire does not pass easily, you may be in an anterior calyx 3. In general, only dilate into a posterior calyx 4. Dilate tract via 8F fascial dilators (can increase stiffness by soaking in ice-slush) 5. “Push/Pull” technique. As you advance the dilator, actively push and pull wire 1-2mm to keep wire straight (this avoids kinking of the working wire) 6. Repeat process for the 8/10F safety wire introducer 7. Place a second, safety, wire when possible 8. If significant bleeding is encountered during dilation, place nephrostomy tube and clamp it to tamponade bleeding, reassess after 5 minutes Balloon systemTip of radiomarker advanced just into tip of calyx Dilate to 24 or 30F under fluoroscopy Advance sheath to the “waist” of the balloon Careful not to over advance sheath onto the “cone” portion of the balloon AlkenEnsure tight and snug fit of all dilators in set Do not skip a dilator size Control tip of dilator at all times Amplatz Dotter catheter must be placed over wire first Dotter tip just into collecting system Sequential dilation must not go too medial Working sheath to the “waist” of the dilator Careful not to over advance sheath onto the “cone” portion of the dilator Initial Entry: 1. Rigid nephroscope must have adjustable suction (e.g., ultrasound lithotrite) when first entering collecting system 2. Look up at 12 o’clock if can not find your way in Operative hints: 1. Suction management 2. Irrigation management (both from nephroscope and from retrograde ureteral catheter 29 3. Use a broad front for larger stones 4. Use room temperature saline for irrigation (set at 30-40 cm above kidney) to help reduce fogging of camera/lens Physiology, minimizing bleeding 1. Avoid hypothermia, use active warming blanket system 2. Mannitol 12.5 g IV can decrease venous bleeding by swelling kidney 3. Avoid excessive torque and force on kidney (safer to use second puncture or flexible nephroscope) Nephrostomy Tube Placement 1. Direct a stiff wire or a 5F ureteral catheter into desired location 2. Cut off the tip of any Foley catheter 1mm distal to the balloon 3. “Push/Pull” the Foley catheter into desire location (confirm with contrast in the balloon, then with a nephrostogram) 4. In obese patients with thick subcutaneous tissue, place nephrostomy tube as far in as possible (e.g., in an upper-pole calyx for a lower pole puncture; or in a lower-pole calyx for an upper-pole puncture) 5. In obese patients, a nephroureteral catheter also can be used 30 5. Nanotechnology, Nanomedicine, and Nanosurgery: An Urologist’s Perspective Joseph C. Liao, M.D. Department of Urology S-287, Stanford University School of Medicine, 300 Pasteur Dr. Stanford, CA 943055118,USA Intravesical and Intraprostatic Botulinum Toxin A Administration in Rat models of Interstitial Nanotechnology is the understanding and manipulations of natural and manmade materials at dimensions of 1 to 100 nanometers. This is the length scale of biological molecules (e.g. DNA and proteins), where manmade materials exhibit unique properties that enable novel applications. Nanomedicine is the highly specific medical intervention at the molecular scale for curing disease or repairing damaged tissues. Nanomedicine holds the promise of revolutionizing medical diagnostics with ultrasensitive nanosensors for detection of biological molecules, imaging with nanoparticles for in vivo, real time visualization of disease processes, and therapeutics through highly precise targeted drug delivery systems. While fundamental understanding of nanoscale research may not be essential for the urologists, it is important to grasp basic concepts of nanotechnology as it will undoubtedly impact the clinical practice in the near future. Proof of concept clinical application of nanotechnology and its microscale counterpart—microelectromechanical system (MEMS)—have already been demonstrated in urology. This includes detection of urinary pathogens and cancer biomarkers using highly sensitive micro/nanosensor arrays. Use of lymphotropic magnetic nanoparticles in conjunction with MRI have been demonstrated to improve detection of numerous urological cancers, including prostate, bladder, and penile. Therapeutic applications of nanoparticles have also begun to emerge in pre-clinical settings for highly specific, targeted delivery of chemotherapeutic agents for prostate cancer. Currently, nanomedicine is still at its infancy and nanosurgery, as the ultimate minimally invasive surgery, has yet to be realized. Nanomedicine is a highly translational research area that requires inter-disciplinary collaboration from engineering, basic science and clinical medicine. Institutional commitment towards development of centers of excellence that promote interdisciplinary collaboration is not only preferred, but necessary. Participation of the urologist in the team is essential given the potential for exciting novel diagnostic and therapeutic modalities for urological diseases. 31 6. Cystitis and Non-bacteria Prostatitis Yao-Chi Chuang 1, Naoki Yoshimura 2, Chao-Cheng Huang 3, Po-Hui Chiang 1, Pradeep Tyagi 2, and Michael B. Chancellor 2 Department of Urology 1, Pathology 3, Chang Gung Memorial Hospital, Kaohsiung Medical Center, Chang Gung University College of Medicine, Kaohsiung, Taiwan and Department of Urology, University of Pittsburgh School of Medicine 2, Pittsburgh, Pennsylvania Introduction and Objectives: There is increasing evidence that botulinum toxin A (BoNT-A) might have analgesic properties but the mechanisms by which BoNT-A alter pain remains largely unexplored. In the bladder, afferent nerve fibers contain calcitonin gene-related peptide (CGRP), which modulates sensory transmission from the bladder. In this study we first investigated the effect of intravesical BoNT-A administration on CGRP immunoreactivity and bladder hyperactivity in acetic acid -induced bladder pain model in rats. Second, an animal model for non-bacterial prostatitis in rats was developed using intraprostatic injection of capsaicin, an agent thought to excite C-afferent fibers and cause neurogenic inflammation. The analgesic and anti-inflammatory properties of BoNT-A was tested in this model. Materials and Methods: For bladder experiments, experimental and control animals were catheterized and intravesically exposed to protamine sulfate (PS, 1 ml, 10 mg/ml) followed by BoNT-A (1 ml, 25 unit/ml, Allergan, Irvine, CA) or saline respectively. Three or seven days after intravesical therapy, continuous cystometrograms (CMGs) were performed under urethane anesthesia by filling the bladder (0.08 ml/min) with saline, followed by 0.3% acetic acid. Bladder immunohistochemistry was used to detect CGRP. For prostate experiments, adult male S.D. rats were injected with varying doses of capsaicin into the prostate. The nociceptive effects of capsaicin were evaluated for 30 min by using a behavior approach and then the prostate was removed for histology and cyclo-oxygenase (COX)-2 protein concentration measurement. Evans blue (50mg/kg) was also injected intravenously to assess for plasma protein extravasation. A second set of animals were injected with up to 20U of BoNT-A into the prostates 1 week prior to intraprostatic injection of 1000 M capsaicin. Results: For the bladder experiments, intercontraction interval (ICI) was decreased after intravesical acetic acid (50.2% decrease, from 22.11.8 min to 11.31.8 min and 65.0% decrease, from 20.62.1 min to 7.21.5 min) in the control group at day 3 and day 7, respectively. However, rats that received BoNT-A showed a significantly reduced response (ICI 28.6 % decrease, from 26.92.4 min to 18.23.1 min) to acetic acid instillation at day 7. This effect was not observed at day 3 (ICI 62.2 % decrease, from 26.20.9 min to 9.91.2 min). Increased CGRP immunoreactivity was detected from BoNT-A treated group at day 7, which was not detected at day 3. For the prostate study, capsaicin dose-dependently induced pain behavioral modifications: closing of the eyes, and hypolocomotion, and induced inflammatory changes: increase of inflammatory cell accumulation, COX-2 expression and plasma extravasation at the acute stage, but completely recovered at 1 week. BoNT-A pretreatment dose-dependently reversed pain behavior and inflammation. BoNT-A 20U significantly 32 decreased inflammatory cell accumulation, COX2 expression, and Evens blue extraction (82.1%, 83.0%, and 50.4%, respectively), and reduced pain behavior (66.7% for eye score and 46.5% for locomotion score). Conclusions: Intravesical BoNT-A administration blocked the acetic acid-induced bladder pain responses and inhibited CGRP release from afferent nerve terminals. Protamine pretreatment allows liquid BoNT-A to be physiological effective. These results support clinical application of BoNT-A for the treatment of PBS/IC. Intraprostatic capsaicin injection induced neurogenic prostatitis and prostatic pain and may be a useful research model. BoNT-A pretreatment produced anti-inflammatory and analgesic effects and support clinical evaluation in nonbacterial prostatitis. 33 7. Effect of changes of detrusor-original excitability on the overactive detrusor Bo Song, Longkun Li, Xiyu Jin, Qiang Fang, Gensheng Lu, Weibing Li Urological center, Southwest Hospital, Third Military Medical University, Chongqing, PR China Background: Overactive detrusor is due to an un-inhibitable detrusor contraction during bladder storage, which always occurs in the pathologic changes such as bladder outflow obstruction and neurogenical bladder. The mechanism is still not well clarified and several hypotheses are presented , the most popular one is the neurogenical theory. Unfortunately the antimuscarinic drugs are not always satisfactory for overactive detrusor according to this theory. Besides the integrity innervation, is there any myocyte-original regulation on the bladder excitability, like in the heart or the intestinal organs? Detrusor-original regulation on the bladder excitability must have such characteristics: spontaneous excitability even undergone denervation; existence of cell-to-cell excitability transconduction; peacemaker cells or peacemaker spots initiating the excitability. To our knowledge, there are few reports on it. Materials and methods: Three kinds of rats models with normal, super-sacral spinal cord transsection and posterior urethral obstruction were constructed, the overactive detrusor from the super-sacral spinal cord trans-section and the posterior urethral obstruction models were selected for the studies. 1) The frequency and intensity of the detrusor spontaneous contraction were evaluated with cystometry in vivo, whole-bladder cystometry in vitro, and detrusor muscle strip test in vitro. The effect of the activators of autonomic nerves on the three models were accessorily detected. 2) The gap junctional intercellular communication in the overactive detrusor was observed with fluorescent bleach technique. 3)To find out the interstitial cells of Cajal (ICC)-like cell with histochemistry, which may behavior as the peacemaker in gastrointestinal. The action potential of the ICC-like cell was also studied with patch-clamp. Results and Conclusions: 1) The stretch load which can induce the contraction in overactive detrusor was much less than that in normal detrusor, but with no significant difference between the overactive detrusor models in neurogenic and bladder outflow obstruction; the activators of autonomic nerves were effective on the frequency of detrusor-original contraction secondary to the stretch load, but cannot eliminate the contraction. Moreover, even tetrodotoxin cannot eliminate the stretch-induced spontaneous detrusor contraction. 2) The gap junction can transfer the cell-cell communication, and this function was enhanced in overactive detrusor myocytes, which indicated the existence of the detrusor-original gap junctional intercellular communication. 3) ICC-like cell exists in bladder, and with the similar potential characteristic as the heart peacemaker, which implied a potential peacemaker in bladder excitability. Prospect: Bladder excitability is always thought as one thing between the autonomic and nonautonomic. Our series of studies verified the existence of detrusor-original element in excitability regulation, and also verified the importance of detrusor-original excitation in the occurrence of overactive detrusor. But the role of detrusor-original excitability in normal bladder still need further studies. 34 8. Bladder primary sensory neuron block: animal and clinical application Zhichen Guan M.D. Department of Urology, Peking University Shen Zhen Hospital, China Objective To study the role of primary sensory neurons block using intravesical vanilloids (capsaicin and resiniferatoxin) both in animal and human. Material and Method From 1994 to 2004, six studies using 27 dogs and 123 rats were done to evaluate the urodynamic, neurotransmitter (substance p) and histological changes after bladder instillation of Capsaicin. Consequently, three studies including 102 patients were carried out using intravesical capsaicin or resiniferatoxin (RTX). The intravesical concentration of capsaicin was 1uM – 2MM/L and RTX was 100nM /L. Result During the first 35 minutes, multiple spontaneous bladder contractions were elicited in 85.71% and 50% of dogs after 100 uM and 1 uM capsaicin bladder instillation, respectively. A significant increase in the bladder volume at leakage point (82.93+3.51 cc vs. 122.22+11.32 cc) was noted. The SP concentration was 2.88+0.55pg/g in control group and the SP concentration were 1.54+0.25 pg/g and 1.29+0.16 pg/g in 1 uM and 100 uM groups after 12 weeks bladder instillation, respectively. Capsaicin reversibly abolished the bladder instability, improved bladder function and increased the ability to compensate in rats with partial bladder outflow obstruction. In a study of 30 OAB cases, RTX instillation didn’t cause vesical irritation and no local anaesthesia was required. The symptoms were improved immediately in all the patients after 1 day of RTX intervention. The decreases in both diurnal (5 to 15 times, mean 8.9 times) and nocturnal (0 to 5 times, mean 3.0 times) frequencies were significant (p<0.001) according to voiding diaries at 1 week and 1 month after treatment. Conclusion The experimental and clinical evidence demonstrated that vanilloids regulated the volume threshold for eliciting micturition reflex, improved bladder response to partial bladder outflow obstruction, had long lasting effects on overactive bladder resulting from a variety of reason. RTX, which produced both an immediate and a prolonged desensitization, appeared to be less irritating than capsaicin and it may be more useful clinically. 35 9. Pyeloplasty: retroperitoneal laparoscopic vs. open approaches Xu ZHANG*, Hong-Zhao LI, Xin MA, Tao ZHENG, Bin LANG, Jun ZHANG, Bin FU, Kai XU Departments of Urology, Tongji Hospital (XZ, XM, BL, JZ, BF, KX), Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, Xiangya Hospital of Central South University (HZL), Changsha and Xiangfan Central Hospital (TZ), Tongji Medical College, Huazhong University of Science and Technology, Xiangfan,. Purpose: We evaluated the clinical value of retroperitoneal laparoscopic dismembered pyeloplasty for ureteropelvic junction obstruction compared with open surgery. Materials and Methods: The clinical data of 56 patients who underwent retroperitoneal laparoscopic dismembered pyeloplasty were retrospectively compared with those of 40 patients who underwent open dismembered pyeloplasty through a retroperitoneal flank approach. Student t-test, Pearson Chi-square test and Mann-Whitney rank sum test were applied for statistical analysis as appropriate. Results: Patient's demographic data were similar between the two groups. In the laparoscopic group, operative time (80 vs 120minutes), estimated blood loss (10 vs 150mL), recovery of intestinal function (1 vs 2days), analgesic requirements (75 vs 150mg), incision length (3.5 vs 21cm), and postoperative hospital stay (7 vs 9days) were better than in the open group (p<0.001 for all). No intraoperative complications occurred in either group. The incidence of postoperative complications (2 of 56, 3.6% vs 3 of 40, 7.5%, p =0.729) and success rates (55 of 56, 98.2% vs 39 of 40, 97.5%, p = 0.058) were equivalent in the 2 groups. Conclusions: Retroperitoneal laparoscopic dismembered pyeloplasty is a minimally invasive, safe and effective therapy for ureteropelvic junction obstruction with low morbidity, shorter convalescence and excellent outcomes and can be accomplished reasonably quickly in experienced hands. 36 10. Graft Outcome of Living Donor Renal Transplantation in the Elderly Recipients Feng-Pin Chuang 1,2, Andrew C Novick 1, Guang-Huan Sun 2, Michael Kleeman,Stuart Flechner 1, V. Krishnamurthi 1,Charles Modlin 1, Daniel Shoskes 1 , David A.Goldfarb 1 1 Glickman Urological Institute, Cleveland Clinic Foundation, Cleveland, Ohio, USA; 2 Division of Urology, Department of Surgery, Tri-Service General Hospital, NationalDefense Medical Center, National Defense College, Taipei, Taiwan, R.O.C. Background: Living donor renal transplantation is a treatment option for patients on dialysis in view of the ever-growing transplantation waiting lists and the stagnation in the number of deceased donors. In the past, advanced age has been considered to be not a good candidate for living donor renal transplantation. The aim of this study is to analyze whether old age affects the outcome of living donor renal transplantation. Methods: 527 first-time living donor kidney transplants were performed between January 1, 1995 and January 1, 2006. The patient population was divided into two subgroups base on the patient’s age at the time of transplant. Old patients were all recipients age 60 years old and above at time of transplant; the control group was all other patients. Results: There is a significant difference in readmission rate (p= 0.031) and patient survival rate (p< 0.001) between two groups. There is not a significant difference in graft survival rate (p=0.808), acute rejection rate (p= 0.7), serum creatinine level and length of stay between these two groups (t=1.75, p=0 .083). Conclusions: Living donor renal transplantation has been controversial in elder recipients. From the clinical reviews, our results confirm that many older patients may benefit from living donor renal transplantation. 37 11. Laparoscopic repair of injury to the inferior vena cava-report of three cases (Video) Liqun Zhou*, Zhisong He, Ningchen Li, Ming Li. Department of Urology, Peking University First Hospital The Institute of Urology, Peking University 8 Xi Shi Ku Street, West District, Beijing 100034, China Introduction and Objective: During laparoscopic surgery, the injury to large vessels, such as inferior vena cava (IVC), often leads to open procedure for repair to avoid bleeding in large amount. We report our primary experience of 3 cases to repair IVC injury laparoscopically and evaluate the safety and efficacy of such laparoscopic repair. Methods: From March of 1992 to August of 2006, we have done 1,668 cases of laparoscopic procedures and met 3 cases (0.18%) of IVC injury, which were partial adrenalectomy, radical nephrectomy and radical ureteronephrectomy. These injuries were caused by dissection with electrocautery hook and harmonic scalpel and 1.2cm, 0.2 cm (2 0.2cm fissures in 1 case) and 0.5cm in length respectively. We repaired the fissures of IVC laparoscopically with intermittent sutures of 3-0 Vincryl threads. The key point for suturing is to work in suction and needle holder in order to show the fissures clearly and suture them accurately. Results: All 3 cases were repaired successfully under laparoscopy and needed 4, 2 and 1 suture respectively. It took 21, 13 and 11 minutes and the amount of bleeding was just 120, 80 and 65ml for repair separately. One case developed partial unconsciousness, language and arm disability after operation and computerized tomography showed several small infarction foci in brain, which might be caused by gas embolism. She recovered full consciousness 1 week later and normal language and arm ability 6 weeks later, but remained the intermittent and slight headache for 3 months. Other 2 cases had no complications. There may be no bleeding at all when IVC injury just occurs and can’t be found in time due to much higher pressure used for pneumoperitonium (14mmHg) than that of IVC (12cmH2O). It would make more gas enter into IVC and gas embolism develop, which is more dangerous for patient. Conclusion: Laparoscopic repair of IVC injury is safe and effective on skilled hands. The earlier the injury is found and repaired, the less complications the patient develops. 38 12. Retroperitoneal laparoscopic Radical Nephrectomy and regional lymphadenectomy for Renal Cell Carcinomas Wei Zhang, Changjun Yin, Wei Zhang, Min Gu, Xiaoxin Meng, Qiang Lv, Lixin Hua, Zhengquan Xu, Yuangeng Sui Department of Urology, The First Affiliate Hospital of Nanjing Medical University, Nanjing 210029, China Objective: To investigate the feasibility and the clinical application value of the retroperitoneal laparoscopic radical nephrectomy and regional lymphadenectomy of renal cell carcinoma (RCC). Methods: Between July 2000 and May 2006, 242 patients (159 males and 83 females) underwent retroperitoneal laparoscopic radical nephrectomy of RCC, of which 58 cases also underwent regional lymphadenectomy. Result: All cases finished successfully. The mean operation time was 170 min (range from 150200 min); the mean blood lose was 150 ml (range from 100-170 ml); the mean tumor diameter ranged from 3-7cm. No case of local or systemic relapse or adrenal metastases, but three cases of lymph node positive and five cases of homonymy adrenalectomy were observed by a follow-up of 1-5 years. Conclusion: The retroperitoneal laparoscopic and open radical nephrectomy of RCC can achieve the same effect, and the former has the advantages of minimal invasion and quicker recovery; however, the former should obey the same operative principle with the latter. 39 13. Correlation of COX-2 Expression in Stromal Cells with High Stage, High Grade and Poor Prognosis in Urothelial Carcinoma of Upper Urinary Tracts Chih-Hsiung Kang, Po-Hui Chiang, Shun-Chen Huang*, and Hsuang-Lan Yu Department of Urology and *Pathology, Chang Gung Memorial Hospital, Kaohsiung Medical Center, Chang Gung University, Taiwan Introduction: To investigate cyclooxygenase-2 (COX-2) expression in carcinoma and stromal cells in patients with urothelial carcinoma of upper urinary tracts (UCUUT), and determine whether expression patterns are associated with clinical characteristics and survival. Methods: Immunohistochemistry for COX-2 was performed on paraffin embedded tumors from UCUUT specimens from 79 patients. The level of expression in carcinoma cells, the presence of stromal cell expression, and the infiltration of inflammatory cells were evaluated. Results: Strong and moderate expression of COX-2 in carcinoma cells was observed in 19 (24.1%) and 46 (58.2%) cases, respectively. In 36 (45.6%) cases COX-2 expression was present in stromal cells. The level of COX-2 expression in carcinoma cells was not correlated with pathological stage ( P = 0.22), and not with grade (P = 0.45). COX-2 expression in stromal cells was correlated with high stage (P < 0.0001) and high grade (P < 0.0001). The patient’s survival was reduced if the tumor revealed strong or moderate expression of COX-2 in carcinoma cells (P = 0.03), the presence of COX-2 expression in stromal cells (P < 0.0001), and infiltrating inflammatory cells (P = 0.0001) by log rank test. Prognosis was poor if the tumor was positive for both COX-2 expression in stromal cells and inflammatory cell infiltrate (P < 0.0001). Conclusion: COX-2 expression in stromal cells shows greater correlation with high stage and high grade than strong COX-2 expression in carcinoma cells. It is suggested that stromal COX-2 expression could be used as a marker of poor prognosis in patients with UCUUT. 40 14. Endoluminal Ureteroplasty for Ureteroenteric Stricture – A Feasibility Study in Porcine Model Victor Chia-Hsiang Lin1, Allen W. Chiu2, Mihir M. Desai3, Inderbir S. Gill3 1E-Da Hospital/I-Shou University, Kaohsiung, Taiwan, 2Chung-Hsiao Mucinipal Hospital, Taipei, Taiwan, 3Cleveland Clinic, Cleveland, USA Introduction: We describe a novel technique of endoluminal endoscopic ureteroplsty for ureteroenteric stricture in which the conventional longitudinal incision is precisely repaired by sutures via the stoma of ileal conduit in a survival porcine model. Method: Under general anesthesia, totally 9 farm pigs underwent laparoscopic cystectomy and ileal conduit. Left ureteroenteric stricture was created by an additional suture near the ureteroenteric junction. 3-4 weeks later, these 9 pigs received endoluminal ureteroplasty. The first 3 pigs underwent the procedures in acute setting to establish and standardize the optimal technique. The latter 6 pigs underwent the operation in chronic setting and were sacrificed 4 weeks later. The serum creatinine, electrolyte, intravenous urography and loopgram were performed before reconstruction and before euthanasia. The tissue near ureteroenteric junction was sent for histopathologic exams. Result: The mean operation time for laparoscopic cystectomy and ileal conduit were 291.7 minutes. The mean operation time for endoluminal ureteroplasty was 60 minutes. Intravenous urography before reconstruction revealed left hydronephrosis and hydroureter in all 6 pigs with significant in 3, moderate in 2 and mild in 1. After correction, all the 6 pigs revealed patent ureteroenteric junction on loopgram. However, 2 pigs had complication of ileal stoma stenosis. Conclusion: Endoluminal endoscopic ureteroplasty is technical feasible, safe and effective. The merits of minimal invasiveness can be maintained without the need of new incision and the good full-thickness healing with primary intent, minimal urinary extravasation can be achieved. We believe the techniques can be spread to human surgery in the near future. 41 15. Laparoscopic Radical Nephroureterectomy With Concomitant Radical Cystectomy for Multi-Focal Transitional Cell Carcinoma in Uremic Patients: Initial Experience Victor C. Lin1, Allen W. Chiu2, Y. H. Lee3, T. J. Yu1 1E-Da Hospital/I-Shou University, Kaoshiung, 2Chung-Hsiao Municipal Hospital, Taipei, 3Chi-Mei Medical Center, Tainan, Taiwan Introduction: Transitional cell carcinoma (TCC) is the most common urinary tract cancer in patients on dialysis in Taiwan. It tends to be multi-focal, high recurrent, and intolerant to chemotherapy and radiotherapy. We present our experience of one session en-bloc laparoscopic unilateral or bilateral nephroureterectomy with radical cystectomy to treat multifocal TCC in uremic patients. Method: 7 uremic patients who were diagnosed multifocal TCC were enrolled. 4 patients were male and 3 patients were female. 5 had undergone ipsilateral nephroureterectomy or radical nephrectomy due to previous history of unilateral upper tract cancer. These 5 patients underwent laparoscopic unilateral nephroureterectomy and concomitant radical cystectomy due to multifocal recurrence of urothelial carcinoma. The other 2 female patients had simultaneous upper tract and bladder TCC in the first time diagnosis and both underwent one session laparoscopic bilateral nephroureterectomy with concomitant radical cystohysterectomy. 6 trocar ports were used in our series. Bilateral nephroureterectomy was performed under lateral position by turning the operation table and the cystectomy was performed under the Tredelenberg position. The specimen was retrieved either from vaginal route in female patients or from old scar or midline in male patients. Result: Mean time for unilateral nephrectomy was 90 minutes. Mean time to complete radical cystecotmy with prostatectomy or hysterectomy was 147 minutes. Mean blood loss was 530 ml. Mean postoperative hospital stay was 7 days. Conclusion: In our initial experience, laparoscopic nephroureterectomy with concomitant radical cystectomy for multifocal TCC in uremic patients is a technically feasible, safe and efficacious modality. 42 16. Prostate cancer management consensus and guidelines between China and Taiwan Chih-cheng Lu, Chia-Ho Lin, Dennis Chian-Shiung Lin, Eric W. Fan, Tse-Chou Cheng Divisions of Urology, Department of Surgery, Chimei Foundation Hospital, Liouying, Tainan, Taiwan Purpose: To compare the clinical practice guidelines in managing prostate cancer(CaP) between China and Taiwan. Materials and Methods: The printed and online materials in medical guidelines or consensus for CaP by Chinese Urological Association(CUA), and Taiwan Cooperation Oncology Group(TCOG) were reviewed. It consisted of published date, revision history, diagnostic methods, and especially the treatment options. Results: The online guidelines for CaP by CUA were available since July, 2006. The TCOG had the first edition of CaP practice guidelines since 1999, and the second edition in 2003. While China version was made by CUA, the Taiwan version was by interdisciplinary experts in TCOG. Magnetic resonance image (MRI) was suggested before transrectal prostatic biopsy in China but not in TCOG. Both agreed to start checking prostate specific antigen(PSA) level when the patient was 45 year-old with a family history of CaP or 50 year-old. PSA normal range was based on Chinese people data with age specific consideration by CUA and based on USA data by TCOG. In predicting local staging and lymph nodes, MRI was considered more informative by CUA than TCOG. The staging system was based on AJCC 2002 by CUA and AJCC 1997 by TCOG, respectively. At least there were no T2c in AJCC 1997 edition. In treatment, HIFU(high intensity focused ultrasound) and CSAP(cryo-surgical ablation of the prostate) was informed by CUA only. Hormone refractory CaP was clearly defined with biochemical data by CUA and mainly based on clinical condition by TCOG. Neither CUA nor TCOG suggested phytotherapy as an option of treatment. Conclusions: In this limited study, we demonstrated several varieties in the guidelines between both regions. Urologists should be aware of the differences between the Chinese versions when applying CaP guidelines to evaluate the Mandarin speaking patients with prostate cancer. 43 17. The Guidelines or Consensus in Managing Benign Prostatic Hyperplasia among China, Singapore and Taiwan Chih-cheng Lu, Chia-Ho Lin, Dennis Chian-Shiung Lin, Eric W. Fan, Tse-Chou Cheng Divisions of Urology, Department of Surgery, Chimei Foundation Hospital, Liouying, Tainan, Taiwan Purpose: To analyze the updating guidelines or consensus in managing benign prostatic hyperplasia (BPH) around the Asian Chinese. It included China, Singapore and Taiwan. Materials and Methods: The printed and online materials in guidelines or consensus for BPH by Chinese Urological Association(CUA), Singapore and Taiwanese Urological Association(TUA) were reviewed. Several statements were compared including published date, revision history, any Chinese translation version, patient selection, diagnostic methods, and treatment options. Results: The online guidelines for BPH by CUA were available before August 2006. The TUA had the Chinese translation(complex characters) of International Prostate Symptom Score(IPSS) and consensus of combination medical therapy in February and May 2006, respectively. The earliest Chinese version of IPSS was published by Ministry of Health of Singapore. Both of the Chinese version by CUA and Singapore were written in simplified characters. Neither CUA nor TUA interpreted precisely IPSS, which consists of 8 questions. The summed score 0 to 35 is from the 7 urinary indexing symptoms. Among these Chinese editions of IPSS, only the translated title was the same. The following 7 urinary symptoms indexing questions and the eighth question about quality of life were semantically different. Only in the guidelines by Singapore established trans-abdominal prostatic grading and staging systems for BPH as non-invasive methods for evaluation and treatment. Either trans-abdominal or transrectal route for sonography was accepted by all. The Age over 50 was announced suitable for guidelines both in CUA and Singapore. There were documented industrial support in building the guidelines or consensus; it was Merck for CUA and Yamanouchi(now as Astellas) for TUA. The CUA considered 5-alpha reductase inhibitors as options of the first line therapy; while the TUA restricted them to be the second line therapy. The use of 5-alpha reductase inhibitors by TUA was not compatible with the rules set by National Health Insurance of Taiwan. Long term of phytotherapy for clarification was suggested by CUA and Singapore while no consensus was done by TUA. Conclusions: Mandarin is currently used without significant difficulty around these regions. People are traveling and communication more and more; the urologists should be aware of the differences among the Chinese versions when applying IPSS to evaluate the Mandarin speaking patients. Also, this updating comparison could do some help in establishing the practice guidelines, which is unpublished, in managing BPH by TUA, since the consensus remains fragmented. 44 18. Hemospermia Associated With Prostatic Cysts: Diagnosised by Transrectile Ultrasonographic and Endocrectal Coil MR Imaging SONG Wei-dong, XIN Zhong-cheng, ZHANG Zhi-chao, GAO Bing, TIAN Long, LIU Bao-xing, WU Yiguang, WU Xiao-jun, GUO Ying-lu Andrology Center, Peking University First Hospital, Peking University,Beijing(100009), China Objective: Hemospermia often associated with prostate cysts or perioprostatic tissues the radiological diagnosis of prostatic or periprostatic cysts could be an ideal methods for define the relationship of a cyst to surrounding structures, such as the vas deferens, seminal vesicles, and ejaculatory ducts. To evaluate the role of transrectal ultrasonography (TRUS) and endorectal coil MR in the diagnosis of hemospermia associated with prostatic cysts. Methods: One hundred twenty patients with hemospermia were performed transrectal ultrasound between August 2005 and March 2007, and 28 cases (23.3%) were found medical prostatic cysts, among of them 24 cases were further evaluated clinical symptoms and performed endorectal coil MR. Results: Of the 24 men, 16 (67%) complained of prostatitis-like symptoms, 12 (50%) with scrotal pain, 7 (29%) with small volume ejaculation, and 5 (21%) with painful ejaculation. All patients had normal follicle stimulating hormone levels, normal or low fructose levels in the seminal fluid. On the basis of MR imaging appearance, 18 (75%) had no anatomic ejaculatory duct abnormalities. Of the remaining patients, 4 (17%) had seminal vesicle dilatation, 2 (8%) had seminal vesicle hypoplasia. Prostatic cysts are easily identified on MR imaging by virtue of their high signal on T2-weighted images and can be characterized because of their typical locations and the high resolution and multiple imaging planes provided by MR. Conclusion: With these results suggested that TRUS and endorectal coil MR are important non-invasive diagnostic tools that minimize the need for more invasive studies in the evaluation of hemospermia, particularly when associated with prostatic cysts. TRUS and endorectal coil MR were not only helpful in establishing the diagnosis but also in determining the choice of treatment. 45 19. China Experience of Penile Prosthesis Implantation for Sever Erectile Dysfunction Zhong Cheng Xin, Zhi Chao Zhang, Wei Dong Song, Long Tian Andrology Center of Peking University First Hospital, Peking University, Beijing(100009),China Purpose: In order to evaluate the effects of different kinds of penile prosthesis implantation for Chinese patients with sever erectile dysfunction (SED). Subjects and methods: Total 98 cases of Chinese patients with SED were treated by different kinds of penile prosthesis implantation during Oct. 2001-Jan. 2007 were followed up using questionnaire form. Mean age of patients was 33.410.6 years old and duration of SED was 5.54.5 years. Among of them the vasculargenic SED was 63 cases (64.3%), neurogenic ED was 20 cases (20.4%), DM 10 cases(11.2%), Peyronine’s disease 4 cases(4.1%). Three piece penile prosthesis AMS700 CXM for 69 cases(70.4%) and Manto alpha I for 3 cases(3.1%) and AMS 650 malleable prosthesis 26 cases(26.6%). Among of them, 3 cases were performed one stage implantation of AMS700CXM with visual internal urethrotomy. Patients and partner’s satisfaction with penile prosthesis implantation were followed up with questionnaires form. Results: Among of patients 2 cases (2.0%) mechanical malfunction, 1 case mechanical malfunction with tube rupture in DM patients with sever cacernosum fibrosis was reimplanted AMS650 malleable and I case malfunction with fluid leakage, however, the patients was satisfied with oral medication with PDE5i such as Sildenafil, Tadanafil and Vardenafil. Patients and partner’s satisfaction with penile prosthesis implantation were 92.4% and 89.8%. Conclusion: Different kinds of penile prosthesis implantation was ideal methods for treatment of SED in Chinese patients, and one stage implantation AMS700CXM with visual internal urethrotomy seams safe and effective method for treatment of SED with urethra stricture. 46 20. Sural Nerve Grafting During Laparoscopic Radical Prostatectomy - Initial experiences of two patients Xin Gao, Xiaopeng Liu, Jianguang Qiu, Hengjun Xiao, Tujie Si Dept. of Urology, the Third Affiliated Hospital of Sun Yat-sen University, 510630, Guangzhou, China. Introduction and Objectives: Sural nerve grafting for patients undergoing radical prostatectomy (RP) has been previously reported using open and robotic laparoscopic methods. We report our initial experiences with sural nerve interposition during laparoscopic radical prostatectomy (LRP). Methods:Between April and July 2005, two potent men were underwent sural nerve grafting during LRP in our department. The age of patient was 59 and 61, respectively. A plastic surgery team harvested 10 to 15 cm of sural nerve from the left leg. The neurovascular bundles (NVB) were extensively excised in left side of patient 1 and both sides of patient 2. With the hem-o-lock located the stump of NVB, sural nerve interposition was performed using 2 stitches of each end with 6-0 polypropylene. Postoperative sexual rehabilitation included oral small dosage of sidenafil (25mg/d) after catheter removed and intracavernosal injection of PGE1 10-30μg, once weekly, which helped the penile engorgement occasionally. Postoperative potency was defined as the ability to penetrate and complete sexual intercourse with or without the use of oral agents. The follow-up was 14-18 months. Patients’ potency was evaluated with IIEF-5 and NPT test by Rigiscan. Results:The sural nerve grafting through LRP was performed successfully in both patients with mean operating time of 5.5 hours. During a follow-up of 6 months, both patients reported penile engorgement with sidenafil but not sufficient for penetration. At the 12th month, patient 1 reported spontaneous erection without any help, erectile number was 1-2/night, erection time was 13±3.5min (70-80%rigidity or greater). Patient 2 was potent enough to penetrate with oral sidenafil, erectile number was 0-1/night, and the erection time was 25±6.5min (20-40%rigidity). Conclusions:Sural nerve graft interposition during LRP is technically feasible and benefits for postoperative erection. Post-operative sexual rehabilitation is safe and useful for potency recovery. 47 21. Erectile Dysfunction Following Transurethral Electrovapor Resection for Different Sized Prostates Chih-Kuang Liu1, 3, Ming-Chung Ko1, 3, Huey-Sheng Jeng1, 2, Wen-Kai Lee1, Hong-Jeng Yu2, HanSunChiang3 1 Department of Urology, Taipei City Hospital, 2Department of Urology, National Taiwan University Hospital, 3College of Medicine, Fu-Jen Catholic University, Taipei, Taiwan Objective: To assess and compare the relationship between erectile function and intraoperative rectal temperature changes of potent patients with different prostate sizes undergoing transurethral electrovapor resection treatment (TUVRP). Patients and Methods: 86 potent patients with lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH) were recruited. Patients were divided to group1-small prostates (<40 ml), and group 2-large prostates (≧40 ml) as determined by transrectal ultrasound (TRUS) measurement. The intraoperative rectal temperature was evaluated by transrectal thermosensor and the temperature differences (the highest intraoperative temperature minus the preoperative temperature) were recorded. The erectile function at baseline, 3 months and 1 year postoperatively were assessed by the International Index of Erectile Function-5 (IIEF-5) Questionnaire. Results: The intraoperative rectal temperature differences were 0.54 ± 0.24 oC in the group 1 (n=45) versus 0.44 ± 0.20 in the group 2 (n=41), (p=0.04). The erectile function data were available for 84 and 78 patients at 3 and 12 months, respectively. The IIEF-5 scores were 20.9±1.6 (group1) versus 20.6±1.6 (group 2) at baseline (p=0.32), 17.3±2.9 versus 18.7±3.2 (p=0.037) at 3 months, and 17.9±2.7 versus 18.7±3.0 (p=0.17) at 1 year postoperatively, respectively. The deterioration of erectile function at baseline and 3-month postoperatively were observed (p<0.001) for both groups. The percentage of retrograde ejaculation between two groups were not significant (p=0.33) at 3-month postoperatively. Conclusions: Our study reveals that higher intraoperative rectal temperature difference caused by transurethral electrovapor resection for treatment of symptomatic prostatic hyperplasia might affect the postoperative erectile function, particularly in a small prostate. 48 22. A Mode Of Treatment For Penilie Incarceration – An Unusual Complication Of Masturbation Jesun Lin, Gin-Bow Chang, Herng-Jye Jiang, Mon-I Yang, Huai-Long Tai,and Bai-Fu Wang Department of Urology, Changhua Christian Hospital, Changhua, Taiwan Purpose: We investigated a technique for releasing an incarcerated penis from the hole of a thick steel plate with minimal invasion. Material and Methods: The patient had his penis incarcerated in a 2 cm diameter hole with 2 cm thick steel plate. We aspirated the congested blood from the glans penis and incised the edema and ecchymosis prepuce to facilitate the escape of subcutaneous congestion blood and fluid. A rubber band was wrapped around the penile shaft immediately distal to the thick steel plate. A fine mosquito hemoclamp was then inserted to grasp the end of the rubber band through the hole. The thick steel plate was gradually worked along the penile shaft until it was free from incarceration. Results: This mode can be used to release the penis from incarcerating objects in emergency situation. The method can be performed in an operating room with minimal equipments and simple technique. The penis is able to sustain very little injury. Discussion: The penile incarceration in a thick steel plate. It is impossible to cut the thick steel without injury of the penis in an emergency state. The patient has been followed up for more than ten years and no any deficit in sexual or urinary condition. Conclusion: We recommend this procedure for the treatment of penile incarceration in similar conditions because it is simple and effective. 49 23. Effect of Cox7a2 on LH induced testosterone production and expression of StAR protein, P450scc and 3β-HSD enzymes in TM3 mouse Leydig cells Liang Chen, Zhong-Cheng Xin,,Long Tian, Yi-Ming Yuan, Gang Liu , Ying-Lu Guo Andrology Center, Peking University, First Hospital, Peking University, Beijing 100009, China Objective: The cloning of Cox7a2 one respiratory chain related gene showed highly expressed in aging male testis tissue in previous study and the effect of Cox7a2 on steroidogenesis and the involved mechanism was investigated. Methods: In the present study, TM3 cells are over-expressed Cox7a2 by transient transfection of recombinant Cox7a2 cDNA plasmid. LH-induced testosterone production is observed by ELISA, and the expression of StAR, P450scc and 3β-HSD was investigated by Western blotting in TM3 cells over-expressing Cox7a2 fusion protein. Results: Cox72 inhibited the LH-induced testosterone in TM3 mouse Leydig cells. In the results of Western blotting, the expression of StAR protein decreased in TM3 cells over-expressed Cox7a2, but the expression of P450scc and 3β-HSD did not altered obviously. Conclusion: Data presented here reveal an unknown role of Cox7a2 in the regulation of the expression of StAR protein, and in its consequent mediating androgen biosynthesis. In TM3 cells, the negative regulatory effect of Cox7a2 on steroidogenesis is, at least, a result of the decreased expression of StAR protein. 50 24. Association of the phenotype of seminal vesicles and CFTR gene mutation in the patients with congenital bilateral absence of the vas deferens Chien-Chih Wu1,2, Chia-Hung Liu2, Han-Sun Chiang1,3 1Department of Urology, School of Medicine, Taipei Medical University, Taipei, Taiwan 2Department of Urology, Taipei Medical University Hospital, Taipei, Taiwan 3Fu Jen Catholic University, Taipei, Taiwan Purpose: Cystic fibrosis (CF) is caused by the mutation of cystic fibrosis transmembrane conductance regulator (CFTR) gene; different composition of the mutated genes resulted in varied degrees of anomaly in phenotype. Among these, congenital bilateral absence of the vas deferens (CBAVD) is recognized as a mild form of CF. Besides the defect of bilateral vas deferens in CBAVD patients, there are various anomalies in the expression of seminal vesicles, including agenesis, hpoplasia, and even normal expression. This study is to analyze the association of seminal vesicle phenotype and the mutation spectrum of CFTR gene in CBAVD patients. Materials and Methods: DNA samples were collected from 20 CBAVD patients. Temporal temperature gradient gel electrophoresis (TTGE) followed by DNA sequencing was used to screen CFTR mutation for all collected DNA samples, which were then classified into homozygous (the same mutations both in 2 alleles), compound heterozygous (2 different mutations separately in each allele), heterozygous (one mutation in one of the 2 alleles), and wild (no mutation detected in both alleles). Transrectal ultrasound was applied for these 20 CBAVD patients to record the phenotype of the seminal vesicles, the results were classified into agenesis, hypoplasia, and present. Results: The CFTR mutations were homozygous in 4 of the patients, and their seminal vesicles showed agenesis in 2 of them (50%), hypoplasia in the other 2 (50%). The CFTR mutations were heterozygous in 9 of the patients, and their seminal vesicles showed agenesis in 1 (11.1%), hypoplaisa in 7 (77.7%) and present in 1 (11.1%) respectively. No CFTR mutation was detected in the rest 7 patients, and their seminal vesicles showed agenesis in 1 (14.3%), hypoplasia in 6 (85.7%). No compound heterozygous mutation was detected in all 20 CBAVD patients. Conclusion: Our result shows that the frequency and severity of seminal vesicles, although not statistically significant, has the tendency to be related to the CFTR genotype; the phenotype of seminal vesicles has the tendency to show agenesis when CFTR mutation shows homozygous or compound heterozygous, while the seminal vesicles show mainly hypoplasia when CFTR screen shows heterozygous mutation or wild. 51 25. Proteomic analysis of human urinary cancer proteome using reverse phase nano-high-performance liquid chromatography / electrospary ionization tandem mass spectrometry. Tan Lia-Beng 1, Liao Pao-Chi 2 , and Guo Haw-Ran 2 Departement of Urology, God Help Hospital ,Taipou, Chai Hsien, Taiwan 1Department of Enviromental and Occupational Health, Cheng-Kung University, Tainan, Taiwan. Purpose : The development of certain disease may change contents of protein in body fluids, and these proteins are potential markers for the diagnosis and mechanistic research. Because urine can be easily obtained without invasive procedures, the analysis of proteins in urine is an ideal candidate for diagnosing bladder cancer. The application of reverse phase nano-high performance liquid chromatography / electrospary ionization tandem mass spectrometry (nanoHPLC -ESI-MS/MS) is possible to identify proteins in urine. The purpose of this study is plan to apply this novel technology in the diagnosis of bladder cancer. Materials and Methods : Patients age and sex-matched cancer and healthy urine specimens were collected through catheterization. To concentrate proteins and remove salts from the urine samples, 5KDa cutt-off centrifugal tube was applied for ultrafiltration and chose multiple affinity removal system (MARS) column to enrich protein identification in urine. To enable us to identify proteins otherwise undetectable due to the high abundance of organic and inorganic substances in urine, the urine was solubilized in TCA in acetone. The protein pellet was resolubilized and digested by trypsin for LC-MS/MS analysis. A nano-HPLC -ESI-MS/MS was used to generate SELDI patterns from 16 primary transitional cell carcinoma (TCC) urine, including 8 with sex and age-matched healthy urine specimens. Quantitative proteomics was applied to one urine specimen and the expression pattern was verified by western blotting. Results : A total of 3192 peptides, corresponding to 934 unique proteins were identified from the urine samples, in which 60 proteins with higher confidence levels. Three proteins, including transferring, prostaglandin D2 synthase (PTGDS), and SET domain and mariner transposase fusion gene (SETMAR) identified in this study are those have not been reported in the urine of bladder TCC before. In addition, we found that lopocalin-type prostaglandin D2 synthase (PTGDS) , as depressed in malignant stages. These proteins could originate from blood and /or bladder cancer tissue of the patients. They also represent potential candidates of useful biomarkers of bladder TCC and could be measured in the urine. Further studies directed toward a multitude of possible protective mechanisms of this enzyme in bladder cancer are warranted. Conclusions : Nano-HPLC -ESI-MS/MS is enables detection of cancer-specific proteins in complex biological mixtures such as urine. These tumor specific urine proteins may proved to be useful for developing a novel of non-invasive, highly sensitivity and acceptable specificity screening tests for the asymptomatic of early-stage bladder caner. 52 26. Survival Analysis of Patients with Bladder Transitional Cell Carcinoma after Open or Laparoscopic Radical Cystectomy Allen W. Chiu, Thomas Y. Hsueh, Steven K. Huan1, Yi-Hsiu Huang Section of Urology, Department of Surgery, Taipei City Hospital, Section of Urology, Department of Surgery, Chi Mei Medical Center, Tainan1, Department of Urology, National Yang-Ming University, Taipei Medical University, School of Medicine, Taipei, Taiwan Purpose: To evaluate the stage and grade specific survival at a mean follow up of 3 years in patients with bladder transitional cell carcinoma received open or laparoscopic radical cystectomy Patients and Methods: A total of 62 patients with bladder transitional cell carcinoma treated with either open (n=21) or laparoscopic radical cystectomies (n=41) were enrolled in this study. Perioperative and pathological data were collected by retrospective chart review. The mean follow-up period was 38.4 months in open and 38.7 months in laparoscopic group. Bilateral limited pelvic lymphadenectomy was performed in selected patients in both groups. There were 5 patients in open and 8 patients in laparoscopic group survived longer than 5 years. Survival analysis with stage and grade stratification was analyzed by Kaplan Meyer method, and the local recurrence and distant metastasis rate were reported. Results: The surgical mortality was 9.5% in the open and 2.4% in the laparoscopic group. The 5-year disease specific survival of pT1 patients was 100% in the open group while 81.8% in the laparoscopy group (p=0.329). The 5-year disease specific survival was 60% in the open and 72.9% in the laparoscopic group in pT2 (p=0.259) patients. As for stage pT3, the 5-year survival was 66.7% in the open group while 85.0% in the laparoscopic group (p=0.269). The grade stratified survival analysis showed no difference in patient received either open or laparoscopic operation. The incidence of local recurrence after the operation was 9.5% in the open group and 9.7% in the laparoscopy group. The incidence of distant metastasis after the operation was 9.5% in the open group while 14.6% in the laparoscopy group. Discussion: The value of pelvic lymphadenectomy in open or laparoscopic radical cystectomy regarding the similar survival analysis in this study. The stage or grade specific survival showed no statistical significance in patient received open or laparoscopic radical cystectomy in a mean follow-up of 3 years. However, a prospective study with longer follow-up is required to verify the real role of laparoscopic radical cystectomy for bladder cancer. 53 27. Characterization and Differentiation of Human Muscle Derived Stem Cells Shing-Hwa Lu1,2,5, An-Hang Yang3, Chou-Fu Wei2, Kuang-Kuo Chen3,5, Luke S. Chang3,5 Department of Urology, Taipei City Hospital1; Division of Urology3, Department of Surgery2, and Department of Pathology4, Taipei-Veterans General Hospital; Department of Urology, National Yang-Ming University5 Purposes: To isolate, purify, characterize and differentiation of the human muscle derived stem cells (MDSCs). Materials and Methods: Isolation of human muscle derived stem cells with modified preplate technique, CD 34-positive stem cell isolation, invitro differentiation of MDSCs, myogenic, adipogenic and osteogenic induction of D 34+ cells, immunolabeling procedures for flow cytometry, flow cytometry analysis, immunohistochemical staining, lipid droplet staining with Oil Red O, Alkaline phosphatase staining, and immunofluorescence study were done. Results: The MDSCs were isolated using modified preplate technique and were purified using Dyna-bead method. The growth doubling time of MDSCs was about 45 hours. Immunohistochemical staining showed positive for several CD markers, VCAM, VEGFR-2, CXCR4, CD56, and Desmin staining. Using special growth factors, the MDSCs could be differentiated into smooth muscle, skeletal muscle, adipocyte, and osteocyte. The differentiation was proved by immunohistochemical study. Conclusions: The isolation, purification, characterization and differentiation of MDSCs were successfully conducted. The MDSCs may provide another novel way for the management of urinary sphincter deficiency and bladder reconstitution. 54 28. Endourology in China: Current status and future direction Yinghao Sun, MD, PhD Department of Urology, The 2nd Military Medical University, Shanghai, China During the past 30 years, the endourology in China has been improved dramatically. For the treatment of BPH, TUR had been introduced to China in the late 1970’s, and now this technique has been spreaded widely in the country as a gold standard of BPH therapy. On the other hand, other emerging techniques for BPH treatment, such as laser prostatectomy, have become available in general practice outside of the investigational setting in China during the past 10 years. On the therapy of stone, ureteroscopy and PCN technique have been popular. Furthermore, some new ideas have been offered, such as the application of high power holmium laser in PCNL. Laparoscopic nephrectomy and Laparoscopic adrenalectomy have also been routine practice. Some complicated operations have also been performed in the Medical Center of metropolis, for example radical prostatectomy, radical cystectomy and partial nephrectomy.It is the main problem that the endourology in china develops disparately. In some regions, such as Peking, Shanghai, Guangzhou, et al, total technical level is relatively high. However, in most of other regions, the endourological technique still occupies lagging status. In the same region, there is distinguished gap between large medical center and basic medical institution. In order to improve the status, Chinese urological Association found the group of Endourology in 1985, which goes in for spreading endourological technique and encouraging communication. Up to date, Chinese endourology has gained full-grown progression. We believe that Chinese endourology should keep up with the world in the near future. 55 29. Evidence-based Urology: report from China Wei Qiang, Han Ping Department of Urology, West China Hospital, Sichuan University, Chengdu, P. R. China Background: Along with progress of evidence-based medicine, clinical medicine is undergoing transformation from empirical medicine into evidence-based medicine, which can not be ignored by urological surgeons as much as other clinical physicians. To learn and master evidencebased medicine, and to combine the best evidence reflected by modern urologic investigation with expertise of urologic physicians will greatly help us to improve the clinical diagnostic and therapeutic levels, providing patients with the best management decisions. Object: To introduce the current status of popularization, application and research of evidencebased medicine of urology in China. Methods: Databases (including MEDLINE, EMBASE, CBMA and Cochrane Library), journals, guidelines and literatures were searched to extract and analyze the information concerning research on evidence-based medicine of urology in China. Results: Concepts of evidence-based medicine were popularized mainly by special theses published in professional journals of urology in China. Since 2003, Chinese Journal of Urology has continuously published a series of special columns on evidence-based medicine, systematically introducing basic concepts and origins of evidence-based medicine, best evidences, the relationship between urology and evidence-based medicine, as the leading platform for promoting and popularizing evidence-based medicine in China. Chinese Urological Association (CUA) organized specialists in all fields of urology of China to systematically analyze and review relevant domestic and international literatures according to principles and measures of evidence-based medicine. Based on the best results of urologic surgery, the CUA evidence-based Guidelines on BPH, OAB, RCC and PCA were compiled and established, which are helpful and active for standardizing diagnostic and therapeutic principles for common diseases in urology and directing clinical practice of urological surgeons in China. For studying evidence-based medicine, together with my colleagues, we successfully registered multiple research proposals in Cochrane Library and published several systematic reviews and metaanalysis in Journal of Urology, Journal of Andrology, Asian Journal of Andrology, Chinese Journal of Urology, Chinese Journal of Evidenced Based Medicine, covering prevention, diagnostics and therapies of urologic diseases as update clinical evidence for practice in urology. Conclusion: Great effort was made by Chinese professionals for popularization, promotion, application and research of evidence-based medicine in urology, which contributed much for about 200 thousand urologic physicians in China to perform clinical management and improve medical treatment quality with best evidences of evidence-based medicine. 56 30. The Incidence and Clinical Significance of High-Grade Prostatic Intraepithelial Neoplasia on Prostate Biopsy in Taiwanese Asian Men Yen-Hwa Chang1, Yi-Chun Chiu1, Chin-Chen Pan2, Kuang-Kuo Chen1 and Luke S. Chang1 1Division of Urology, Department of Surgery, and 2Department of Pathology, Taipei Veterans General Hospital and Department of Urology, School of Medicine, National Yang-Ming University, Taipei, Taiwan, R.O.C Purpose: High-grade prostatic intraepithelial neoplasia (HGPIN) is considered a prostate cancer-associated lesion. There is little information about the characteristics of HGPIN among Asian men. We retrospectively reviewed patients with HGPIN on prostate needle biopsy to analyze the clinical significance of HGPIN among Taiwanese men and to postulate the implication for patient care. Materials and Methods: From August 1999 to April 2004, 4250 patients who underwent transrectal ultrasound (TRUS)-guided prostate biopsy at our hospital due to elevated PSA and/or abnormal digital rectal examination (DRE). Patients with HGPIN were recommended to have follow-up biopsy unless it was rejected. Clinical parameters and characteristics of these patients were evaluated. Results: A total of 112 (2.63%) had HGPIN. The mean age at diagnosis was 73.8 years (range, 51–93). Of these HGPIN patients, 95 (84.8%) had isolated HGPIN and 17 (15.2%) had concurrent HGPIN and prostate cancer (PCa). 69 out of 95 (73.6%) patients with isolated HGPIN underwent follow-up biopsy, and PCa was identified in 18.8% of patients with 92.3% of PCa detected on the first two follow-up biopsies. There was no correlation between clinical parameters (PSA value, DRE and TRUS findings) and the risk of PCa on subsequent biopsy. Conclusions: HGPIN in Taiwanese men is uncommon comparing to those reported in the contemporary Western series. Clinical findings are not predictive of PCa on repeat biopsy. If cancer is not found on the first two follow-up biopsies, the risk of PCa is low. These patients should then be followed up clinically to determine whether subsequent biopsy is required. 57 31. Prostatic Cancer in Macau S.A.R. Lap Hong Ian M.D Department of Urology, Centro Hospitalar C.S. Januario, Macau S.A.R. Prostate cancer is the second leading cause of cancer-related death men in the United States. The incidence of prostate cancer in Asia is far more lower which may be related to multiple factors including genetic, diets, and economic environment. As the rapid economic and social development of Asia countries and areas, such as Macau S.A.R., in the last 10 years, the incidence and cancer-related mortality of prostate cancer in men are increasing markedly in trace. Screening, early detection, improved imagiology and surgical technology of prostate cancer are become the major goal in Urologic Oncology in Macau S.A.R. 58 32. Efficacy and Safety of Tolterodine and/or Tamsulosin in Men with Lower Urinary Tract Symptoms (LUTS) Including Overactive Bladder (OAB): Results from a Four-Arm, Placebo-Controlled Trial Zhonghong (Eric) Guan, MD, PhD Medical Director, Global Medical, Urology, Pfizer Background: As the storage domain of LUTS, OAB is a syndrome characterized by urinary urgency, with or without urgency urinary incontinence, usually with increased micturition frequency during the day and at night. OAB is often attributed to detrusor overactivity (DO), a condition characterized by involuntary detrusor contractions during bladder filling. In men, detrusor overactivity may coexist with or be secondary to bladder outlet obstruction (BOO) due to benign prostatic hyperplasia (BPH). Since both BOO and DO contribute to LUTS, it is logic to target both prostate and bladder for the pharmaceutical intervention for LUTS including OAB. The current standard of care for male lower urinary tract symptoms is treatment with αadrenergic receptor antagonists. However, many men with LUTS including OAB may not respond to monotherapy with α-receptor antagonists. Methods: This is the first study to evaluate the efficacy and safety of tolterodine, an antimuscarinics for the treatment of OAB, and/or tamsulosin, α-receptor antagonist for the treatment of BPH, in men who met research criteria for both OAB and BPH. In this randomized, double-blind, placebo-controlled trial, men (≥40 y) with total International Prostate Symptom Score (IPSS) ≥12; IPSS quality-of-life (QoL) item score ≥3; self-rated bladder condition of at least moderate bother; and bladder diary-documented micturition frequency (≥8 micturitions/24 h) and urgency (≥3 episodes/24 h), with or without urgency urinary incontinence were included. Patients were randomized to placebo (n=222), tolterodine ER (4 mg; n=217), tamsulosin (0.4 mg; n=215), or tolterodine ER/tamsulosin (n=225) for 12 weeks. Results: A significantly greater percentage of patients receiving tolterodine ER/tamsulosin (80%) reported treatment benefit by week 12 compared with placebo (62%, P<0.0001), tamsulosin (71%, P<0.05), or tolterodine ER (65%, P<0.01). The tolterodine ER/tamsulosin group (vs placebo) demonstrated significant reductions in urgency urinary incontinence (−0.88 vs −0.31, P<0.01), urgency episodes without incontinence (−3.33 vs −2.54, P<0.05), micturitions per 24 hours (−2.54 vs −1.41, P<0.001), and micturitions per night (−0.59 vs −0.39, P<0.05). Tolterodine ER also reduced urgency urinary incontinence (−0.83 vs −0.31, P<0.01). Patients receiving tolterodine ER/tamsulosin demonstrated significant improvements on the total IPSS (−8.02 vs placebo, −6.19, P<0.01) and QoL item (−1.61 vs −1.17, P<0.01). The post hoc analysis found that, in patients with larger prostate and higher PSA, only tolterodine plus tamsulosin significantly improved OAB/storage LUTS symptoms; however, in patients with smaller prostate and lower PSA, tolterodine monotherapy was almost as effective as combination of tolterodine and tamsulosin on OAB/storage LUTS symptoms. All interventions were well tolerated; the incidence of acute urinary retention requiring catheterization was low (tolterodine ER/tamsulosin, 0.4%; tolterodine ER, 0.5%; tamsulosin, 0%; placebo, 0%). Tolterodine with or without tamsulosin did not significantly change Qmax and PVR. 59 Conclusions: These results strongly suggest that treatment with tolterodine ER with or without tamsulosin is a safe and effective pharmacotherapy for men with LUTS including OAB. 60 33. Laparoscopic Radical Cystectomy with Orthotopic Ileal Neobladder: A Report of 85 Cases Jian Huang2, Tianxin Lin, Kewei Xu, Hai Huang, Chun Jiang , Jinli Han , Yousheng Yao, Zhenghui Guo and Wenlian Xie Department of Urology, Second Affiliated Hospital, Sun Yat-sen University, Guangzhou 510120, China Introduction: The preliminary results of laparoscopic radical cystectomy in 85 cases were presented in this study. The functional and oncological outcomes of this procedure in these cases were discussed. Patients and Methods: Between December 2002 and May 2006, we performed 85 cases of laparoscopic radical cystectomies with orthotopic ileal neobladder for bladder cancer on 77 male and 8 female patients. A 5-port transperitoneal approach was applied. The standard bilateral pelvic lymphadenectomy was done first, the radical cystectomy was then completed laparoscopically. The construction of ileal neobladder and the anastomosis of ureter-neobladder were performed extracorporeally. The neobladder was anastomosed to the urethral stump under laparoscopy. The nerve sparing procedure was performed for 8 cases. Results: The mean operation time was 326 min, and the mean blood loss was 316 ml. Conversion to open surgery was not necessary for all patients. The average time to oral intake after operation was 3.9 days. There were no peri-operative mortalities. The complication rate was 14.1% (12/85), including 3 uretero-pouch anastomotic stricture, 1 vesico-urethral anastomotic stricture, 1 pouch-vaginal fistula, 1 caceo -pouch fistula,1 ileo-pouch fistula ,3 partial ileus,1 pneumonia and 1 urinary tract infection. The daytime continence rate was 94.1 % and nighttime continence rate was 91.2 % in 6 month postoperatively. The neobladder capacity was about 343 ml. Surgical margins were tumor free for all cases. 4 of the 8 nerve-sparing patients had potency for intercourse. Over a follow-up of 1 to 41 months (average 23.3 months), 3 cases had local recurrence, 1 case had trocar site seeding, 6 cases had distant metastasis and 5 of whom died. Conclusions: Laparoscopic radical cystectomy with extracorporeal formation of neobladder is a feasible procedure with low morbidity and acceptable neobladder function. Long term follow-up is needed to confirm the oncological outcomes. 61 34. "Sliding Knot Vesicourethrostomy" in LRP and LRC Ho Son Fat Urology Department, CHCSJ, Macau Lapoaroscopy Radcal Prostatectomy and Laparoscopy Radical Cystoprostatectomyectomy are difficult urologic operations, and the vesicourethrostomy is the most difficult step in these two operations, especially for the beginner. Bsaed on continue suture method of vesicourethrostomy, I created "Sliding Knot Vesicourethrostomy" method. I have used "Sliding Knot Vesicourethrostomy" in 13 Lapoaroscopy Radcal Prostatectomies and 2 Laparoscopy Radical Cystoprostatectomyectomies, it make the Vesicourethrostomy simple, easy, quick and safe. 62 35. Diabetic Erectile Dysfunction: Animal Studies Yu-tian DAI1, Yun CHEN1, Run WANG2, Zeyu SUN1, Rong YANG1, Leshen YAO1, Dong CHEN1, Sanxiang LI1 1 Department of Urology, Affiliated Drum Tower Hospital, Nanjing University ,School of Medicine, Nanjing, Jiangsu 210008, China 2 Department of Urology, University of Texas Health Science Center at Houston and MD Anderson Cancer Center, Houston 77030, USA Diabetes mellitus (DM) and its complications are major causes of morbidity and mortality in the developed countries. Erectile dysfunction (ED) is one of the most common complications in diabetic men. Sometimes, ED can even be the first sign of DM. The pathogenesis of diabetic erectile dysfunction is very complex, involved in nerve, neurotransmitter, blood vessel, endothelial function, metabolism, endocrine and so on. The neural factor plays a crucial role. Without influence of vascular pathological changes, there was found diffuse neuropathic changes in penis and pelvic ganglia in the BB/WOR rat model. We did some work on the neural factors. We found that the proteins of NGF, BDNF, NT-3 and NT-4 were all detected in the cavernous tissue. We found that NGF, NT-3, NT-4 proteins expression in cavernous tissue of diabetic ED rats were all up-regulated compared to normal control rats while BDNF was down-regulated. The exogenous administration of NGF or using AdV vector mediated NGF or using HSV vector mediated NT-3 can partly revise the erectile function of diabetic ED rats. The neurotransmitter factor is a very important role. As we all known, the relaxation of the corpus cavernosum was mediated by the L-Arg-NO-cGMP pathway. In diabetic ED rats, we could find the decreased level and activity of penile nitric oxide synthase (NOS) and increased expression of arginase II. Arginase is the enzyme that may downregulate NO production by competing with NOS for L-Arg. Gene transfer of endothelial NOS (eNOS) recombinant adenovirus or calcitonin gene related peptide (CGRP) recombinant adeno-associated virus or vasoactive intestinal polypeptide (VIP) cDNA could enhance the erectile response in diabetic rats. Macroangiopathy caused the defect of hemoperfusion to penis, and microangiopathy caused the ultrastructural changes of penis in diabetic animals. Blood vessel endothelium function is another factor. The impaired endothelium caused the increased level of endothelin-1 (ET-1) and endothelin receptor B (ETRB), and the cavernous smooth muscle contracted. The penile expression of vascular endothelial growth factor (VEGF) and its receptors were decreased. The exogenous of VEGF could improve the erectile response in diabetic rats. We found the increased level of angiotensin-I and the decreased level of angiotensin subtype 1 receptor in the diabetic ED rats. Valsartan, the effective antagonist of AT1R, can reverse the erectile dysfunction of DM rats. Metabolism factor contains the evaluated advanced glycation end-products (AGEs) and superoxide anion. The treatment with the Chinese drug “Jiang Tang Qi Wei He Ji”or extracellular superoxide dismutase gene therapy can partly reverse the erectile dysfunction of DM rats. 63 The upregulated RhoA/Rho-kinase pathway in diabetic rats mediated ED through decreased production of NO in the penis. The inhibition of RhoA/Rho-kinase improves eNOS protein content and activity thus restoring erectile function in diabetes. The ion channel and cell gap junction also have some effect on DM ED. Though the multiple factors may play some roles on pathogenesis of DMED, we should use combined therapy according to the multifactorial pathogenesis of diabetic ED, in order to elevate the therapeutic effect on DMED. The most important treatment is to regulate the blood glucose level to normal. In the same time, we should protect the pelvic splanchnic nerves, vessel endothelium function, L-Arg-NO-cGMP pathway, oxidative stress-antioxidative system, androgen supplement, cleaning of AGEs, and so on. We believed that gene therapy could bring us a surprise in the future. 64 3. WCUS Meeting 2008 Date: Saturday, May 17, 2008 Venue: Orlando, Florida, USA Theme: State-of-World Chinese Urology 65 Program - 2008 8:00 - 8:07 am Welcome and introduction Tom F. Lue, USA 8:07 - 8:10 am Report from Scientific Program Committee Run Wang, USA 8:10 - 9:00 am Session 1: Highlight on Chinese Urology Moderators: Yinglu Guo, China; Luke S. Chang, Taiwan; Keong Foo, Singapore 8:10 - 8:20 am 8:20 - 8:30 am 8:30 - 8:40 am 8:40 - 8:50 am 8:50 - 9:00 am Yanqun Na, President, Chinese Urological Assoc. Han-Sun Chiang, President, Taiwan Urological Assoc. Chin Chong Min, Vice-President, Singapore Urological Assoc. Wai Sang Wong, President, Hong Kong Urological Assoc. Son Fat Ho, President, Macao Urological Assoc. 9:00 - 9:10 am Integration of Chinese and Western Medicine in Urology Yaqiang Zhang, China 9:10 - 9:20 am WCUS awards 9:20 -10:45 am Session 2: Scientific Program Renal and Urothelial Tumours Moderators: Yanqun Na, China; Rei K. Chiou, USA; Chi-Rer Yang, Taiwan 9:20 - 9:30 am Epithelial-mesenchymal transition/mesenchymal-epithelial transition and tumor invasion Dalin He, China 9:30 - 9:40 am The relationship between bladder and upper urinary tract in urothelial neoplasm Guang Sun, China 9:40 - 9:50 am Proteomic analysis of human urinary bladder cancer proteome using reverse phase nano-high performance liquid 66 chromatography/electrospray inonization tandem mass spectrometry Lia-Beng Tan, Taiwan 9:50 - 10:00 am Laparoscopic radical cystecomy with orthotopic ileal neobaldder in woman Jian Huang, China 10:00 - 10:10 am Robotic-assisted laparoscopic radical cystectomy in the management of bladder cancer Guan Wu, USA 10:10 - 10:20 am Endoscopy-assisted radical nephrectomy Chuize Kong and Xiankui Liu, China 10:20 - 10:30 am Data Analysis of 1228 Patients with Renal Cell Carcinoma in East China Yiran Huang and Baijun Dong, China 10:30 - 10:45 am Discussion 10:45 - 11:00 am Tea and Coffee Break 11:00 - 12:00 noon Session 3: Scientific Program Prostate Cancer Moderators: Yinghao Sun, China; Leland Chung, USA; Apichat Kongkanand, Thailand 11:00 - 11:10 am Dietary factors and prostate cancer Bill Nelson, USA 11:10 - 11:20 am Prostate cancer treatment in Sweden: an update Yuhui Wang, Sweden and Norway 11:20 - 11:30 am Robot-assisted laparoscopic radical prostatectomy: where we stand in 2008 Li-Ming Su, USA 11:30 - 11:40 am Salvage therapies following radiation failure for prostate cancer Joseph Chin, Canada 11:40 - 11:50 am Comparison of robotic and open radical prostatectomy: histopathologic outcomes Steven Shen, USA 11:50 - 12:00 noon Discussion 12 Noon - 1:00 pm Box Lunch and Viewing of Posters and Videos 67 1:00 pm - 2:00 pm Session 4: Scientific program Poster Presentations and Discussion (I) Moderators: Guang Sun, China; Son Fat Ho, Macao; Liqun Zhou, China Adrenal Disease 1:00 - 1:03 pm Laparoscopic surgery on ectopic para-aortic pheochromocytoma (report of 2 cases) Liming Li, Yi Lin, Jun Zhu, Hui zhang, China 1:03 - 1:06 pm Clinical analysis of cystic mass at the site of adrenal gland. Liming Li, Yi Lin, Jun Zhu, Hui zhang, China Upper Urinary Tract 1:06 - 1:09 pm A comparison of perioperative data between open and laparoscopic nephroureterectomy for upper urinary tract transitional cell carcinoma Ning-chen Li, Li-qun Zhou, Ming Li, Zhi-song He, Yan-qun Na, China 1:09 - 1:12 pm Rare cases of non-tuberculosis, non-reflux, and non-obstructive megaureter in an adult Allen W. Chiu, Taiwan 1:12 - 1:15 pm Gasless hand assisted retroperitoneoscopic nephroureterectomy Po Hui Chiang, Taiwan 1:15 - 1:18 pm Urine chemokine/cytokine change in patients with urolithiasis Yii-Her Chou, Taiwan Prostatic Diseases 1:18 - 1:21 pm Outcome of incidental prostate cancer in Macau Lao Hoi Fai, Ian Lap Hong, Macau 1:21 - 1:24 pm FACT-P survey for quality of life among patients with advanced prostate cancer in China Kan Gong, Kai Zhang, Li-qun Zhou, Yan-qun Na, China 1:24 - 1:27 pm Thurlium-YAG laser vaporesection of prostate for patients with BPH-Taipei city hospital experience. Shing-Hwa Lu, Taiwan 1:27 - 1:30 pm PSA, % fPSA and prostate volume as diagnostic parameters of prostate carcinoma for Chinese men. Chuanliang Xu, Yinghao Sun, Xiaofeng Gao, et al, China 1:30 - 1:33 pm Characterization of normal prostate on transabdominal ultrasound Lim Kok Bin, Singapore 1:33 - 1:36 pm Intraprostatic botulinum toxin A injection inhibits cox-2 expression and suppresses prostatic pain on capsaicin induced prostatitis model in rat Yao-Chi Chuang, Taiwan 68 1:36 - 1:39 pm The radiation response of hormone-resistant prostate cancer induced by long-term hormone therapy Chun-Te Wu, Taiwan 1:39 pm - 2:12 pm Session 5: Scientific program Poster Presentations and Discussion (II) Moderators: Jianye Wang, China; Kenneth C. Hsiao, USA; JT Hsieh, Taiwan Adrology 1:39 - 1:42 pm Traditional medicine in ED in Asia-experience from the Asian males Hui Meng Tan, Chirk Jenn NG, Malaysia 1:42 - 1:45 pm The role of meiosis regulator BOLL and its downstream substrate CDC25A in human spermatogenesis. Yung-Ming Lin, Taiwan 1:45 - 1:48 pm Array-CGH identifies copy number alterations (CNAS) of reproduction-related genes in Taiwan congenital bilateral absence of the vas deferens Chien-Chih Wu, Taiwan 1:48 - 1:51 pm The effect of different severity in bladder dysfunction on corpus cavernosum smooth muscle and Rho-kinase in rabbits. Wei-Yu Lin, Taiwan Urinary Bladder 1:51 - 1:54 pm Pure laparoscopic radical nephroureterectomy with concomitant radical cystectomy for multi-focal transitional cell carcinoma in uremic patients Victor C. Lin, Taiwan 1:54 - 1:57 pm A training model of laparoscopic urethrovesical anastomosis Tianxin Lin, Jian Huang, Kewei Xu et al, China 1:57 - 2:00 pm The enhancement of neovascularization for the tissue engineering urinary bladder, A experiment study in vivo and in vitro Yutian Dai, Bin Yang, Zeyu Sun, China 2:00 - 2:03 pm Immunotherapy for orthotopic murine bladder cancer using BCG recombinant protein MPT-64 Dah-Shyong Yu, Taiwan 2:03 - 2:06 pm Functional effects of suburethral sling on female bladder outlet: comparison between fascial sling and prolene mesh tape sling. Alex T.L, Lin, Taiwan 2:06 - 2:09 pm Beneficial effects of antrodia comphorata on bladder function before and after ischemia/reperfusion of rabbit bladder. Alpha Dian-Yu Lin, Taiwan Medical Legal Issues 69 2:09-2:12pm Experience of reducing medical legal issues from an award-wining personal website. Chih-Cheng Lu, Taiwan 1212 - 2:15 pm Brief Break 2:15 - 2:40 pm Session 6: TUA Lectures Moderators: Zeyu Sun, China; Hui Meng Tan, Malaysia; Jun Chen, Taiwan 2:15 - 2:25 pm Prognostic significance of P53 and x-ray repair crosscomplementing group 1 polymorphisms on PSA recurrence after radical prostatectomy. Shu-Pin Huang, Taiwan 2:25 - 2:35 pm The effect and mechanism of epimedium brevicornum maxim extract on rat penile and rabbit clitorial intracavernous pressure. Kuang-Kuo Chen, Taiwan 2:35 - 2:40 pm Discussion 2:40 - 2:50 pm Tea and Coffee Break 2:50 - 3:55 pm Session 7: Scientific Program New Technology and Practice Tips in Urology Moderators: Zhangqun Ye, China; Bill Wong, Hong Kong; Kuang Kuo Chen, Taiwan 2:50 - 3:00 pm Mechanism of pelvic pain syndrome Bo Song, China 3:00 - 3:10 pm Indications of Robot in Urology Tung Shu, USA 3:10 - 3:20 pm Retroperitoneoscopic ligation of renal lymphatic vessels for the treatment of chyluria-----Surgical tips and our experience Gongxian Wang, China 3:20 - 3:30 pm Laser Prostatectomy in 2008 Carson Wong, USA 3:30 - 3:40 pm Sacral neuromodulation for lower urinary tract dysfunction caused by spinal cord injury Ho Son Fat, Macau 3:40 - 3:50 pm Male identity: a missing link in the formula to promote men’s health 70 Chirk Jenn NG and Hui Meng Tan, Malaysia 3:50 - 3:55 pm Discussion 3:55 - 4:00 pm Closing Remarks Yanqun Na, China; Luke S. Chang, Taiwan 71 4. WCUS Meeting 2009 Date: Saturday, April 25, 2009 Venue: Hyatt Regency, McCormick Place, Chicago, USA Theme: State-of-World Chinese Urology 2009 The World Chinese Urological Society (WCUS) meeting in Chicago, 2009 Tom F. Lue, MD, FACS and Run Wang, MD, FACS The World Chinese Urological Society (WCUS) has been very active at the AUA annual meetings. The number of participants has increased from 300 at the 1 st meeting held in Atlanta, Georgia in 2006 to more than 500 at the 3 rd meeting held in Orlando, Florida in 2008. Chinese-speaking urologists and urologic scientists attended the meeting from all corners of world including China, Taiwan, Hong Kong, Macao, Singapore, Thailand, Malaysia, Australia, Europe and North America. Based on the suggestions from previous participants we will have several new and exciting features at the 2009 Chicago meeting. These include more time for the participants to mingle and make new friends at the poster session, expert panels to discuss prostatitis and cystitis, two commonly mismanaged conditions in China, as well as highlight sessions on various subspecialties that will help the participants to be familiar with the state-of-the-art of urology. The meeting will begin as usual with updates by the presidents of the urological associations of China, Taiwan, Singapore, Hong Kong and Macao. This will be followed by a two-hour poster session so that the participants have plenty of time to discuss the science and practice of urology as well as getting to know one another. Following this session, experts from different regions will present their practical approaches to prostatitis which is a very common, yet, controversial topic in China. The afternoon session will begin with a panel discussion of cystitis glandularis that has caused a management dilemma in China recently. In light of the overwhelming information and limited time during the AUA, the meeting will invite accomplished urologists and scientists to give the AUA abstract highlights for kidney, bladder and prostate cancers, BPH, voiding dysfunction/female 73 urology, sexual dysfunction, and infertility. We hope this will stimulate the members of WCUS to participate in the remaining AUA scientific activities. The annual AUA-WCUS meeting is designed as a platform for effective communication among Chinese-speaking urologists and urological scientists. However, it will also serve as a venue to share the advancements in basic and clinical research from the countries and regions mentioned above with the AUA members from other parts of the world since the slides and posters will be in English. We certainly welcome you to attend this meeting and to meet the best and brightest Chinese colleagues. 74 Program - 2009 8:00 - 8:07 am Welcome and introduction Tom F. Lue, USA 8:07 - 8:10 am Report from Scientific Program Committee Run Wang, USA 8:10 - 9:00 am Session 1: Highlight on Chinese Urology Moderators: Zeyu Sun, China; Kuang Kuo Chen, Taiwan; Richard Lo, Hong Kong 8:10 - 8:20 am 8:20 - 8:30 am 8:30 - 8:40 am 8:40 - 8:50 am 8:50 - 9:00 am Yanqun Na, President, Chinese Urological Assoc. Jong Khing Huang, President, Taiwan Urological Assoc. Chin Chong Min, Vice-President, Singapore Urological Assoc. Ming Kwong Yiu, President, Hong Kong Urological Assoc. Hong Lap Ian, Secretary, Macao Urological Assoc. 9:10 - 9:20 am WCUS awards 9:20 - 11:20 am Session 2: Scientific Program View and Discuss Posters Moderators: Tinghao Sun, China; KK Chew, Australia; Wai Hong Pun, Macau Kidney Disease and Urinary Stone The Effects of Irrigating Fluid Absorption in Percutaneous Nephrolithotripsy Shaobin Ni, China The Treatment and the Composition of Melamine-Contaminated Infant Formula Induced Upper Urinary Calculi Guohua Zeng, China Treatment of Upper Ureteral Stones with Ntrap Combined with Ultrasonic and Pneumatic Lithotripter under Ureteroscopy Tiejun Pan, China Safety of PNL in Solitary Kidney Jianxing Li, China Non-enhanced helica CT Three-dimensional Reconstruction Axis Rotation Movie Images in Percutaneous Nephrolithotripsy and its Clinical Significance. Linwu Chen, China 75 Recent advances in the management of RCC in China Ding Wei Ye, China "Marginal donors in renal transplantation: our experience" VY Chung, LY Ho, HH Hung, J Fenn; Hong Kong The effect of “Shiwei“ on the urine biochemistry of male patient suffering form urinary calculi. CF Ng, K Ip, D Gohel; Hong Kong Comparing extracorporeal shock wave lithotripsy (SWL) with percutaneous nephrolithotomy (PCNL) for lower pole stones larger than 10 mm: Tuen Mun Hospital experience MA Wai-Kit, YU Cheong, LAM Kin-Man, CHU Sau-Kwan Peggy, MAN Chi-Wai; Hong Kong Percutaneous nephrostomy versus internal stenting in the management of acute pyonephrosis, a retrospective study. HY Ngai, PS Szeto, HS So, V Velayudhan; Hong Kong Flexible Ureteroscope in management of upper ureteric stone Chan Tai Ip, Macau Results of urological screening for adults claiming to have ingested melaminecontaminated diary foods in a community hospital in Taiwan. Yuh-Chen Kuo , Taiwan Overexpression of her-2 is a poor prognostic factor in upper tract urothelial carcinoma post-radical nephroureterectomy Chun-Hsiung Huang, Taiwan Innovated concept in percutaneous nephrolithotomy – single institute 780 case report Cheng-Huang Shen, Taiwan Bladder Diseases Clinical Investigation on the Relationship between Upper Urinary Tract Obstruction and the Accompanied Chronic Cystitis Aihua Li, China Pelvic Floor Innnervation and LUTS Bo Song, China The Study of Diagnostic Criteria of Bladder Outlet Obstruction in Female Kexin Xu, et al., China 76 Radical Cystectomy for Carcinoma of the Bladder in Older Patients Chen Xiao, et al., China Improvements and Long-term Outcomes of Orthotopic Urinary Diversion (376 cases) Jiong-ming LI, China Use of Intravesical Hyaluronic Acid in Patients with “Street Ketamine”Aassociated Bladder Dysfunction: A Pilot Study MA Wai Kit, CHU Wing Hong, YIU Ming Kwong; Hong Kong Differential roles of neuronal- and urothelium-derived no in the spontaneous activity of mouse detrusor smooth muscle En Meng, Taiwan Cystitis glandularis – case analysis Ching-Hsin Chang, Taiwan Prostate Cancer Robot-assisted Radical Laparoscopic Prostatectomy (16 cases) Jiangping Gao, China Brachytherapy for localized Prostate Cancer in Hong Kong Patients Richard Lo; Hong Kong Does extended transrectal ultrasound-guided prostate biopsy protocol improve cancer detection in Chinese patients – Transitional zone versus Peripheral zone approach. KL Ho, SM Chu, PC Tam; Hong Kong Short-term Outcome of Patients with Robot-assisted Versus Open Radical Prostatectomy: Prince of Wales Hospital, Hong Kong Experience S Yip, KL Lo, A Wong, CF Ng; Hong Kong Prostate Valume is a effective predictor of cancer detection with serum PSA between 4 and 10ng/ml Ian Lap Hong, Lao Hio Fai, Pun Wai Hong, Li Kin, Tse Man Kin, Ho Son Fat; Macau Association study of rs1447295 at 8q24 with prostate cancer in Taiwanese men Marcelo Chen , Taiwan Glycemia disorders and risk of prostate cancer mortality: an evidence for the insulin hypothesis Hui-Ming Chung , Taiwan A multivariable logistic regression equation to screen for prostate cancer Jhih-Cheng Wang, Taiwan 77 Clinicopathological Characteristics and Long-term Prostate-Specific Antigen Recurrence -free Survival of Prostate Cancer Post Radical Prostatectomy in Taiwan Shu-Pin Huang , Taiwan Update of Guidelines in Managing Benign Prostatic Hyperplasia among China, Singapore and Taiwan Chih-Cheng Lu, Taiwan hK7 promotes the invasion and induces the epithelial-mesenchymal transition (EMT) like morphological changes of human prostate cancer cell DU145 Zengnan Mo et al, China The impact of estrogen in prostate development and cancer Shuyuan Yeh, PhD, USA BPH / LUTS The vaporesection for Management of Benign Prostatic Hyperplasia Using 2 Micron Continuous Wave Laser: A Prospective Trial with 1-year Follow-up Weiju Fu, China The Detection and Treatment of Satellite Lesion of Bladder Tumor Using Narrow Band Imaging Flexible Cystoscopy Jingchun Xing, China Survey on Current Situation of Pathogenesis of Prostate Hyperplasia in Multicenters of Beijing Communities Ye Tian, China Transurethral Electrovaporisation of Prostate in Saline: Histology Study SWH Chan, HP Mo, NH Chan, MK Yiu; Hong Kong Long-term outcome of TURP: a local experience LY Ho, MH Wong, HY Lau, KL Lo, VY Chung, HH Hung, J Fenn; Hong Kong Metabolic syndrome and prostate volume Hsu-Han Wang, Taiwan Laparoscopic simple prostatectomy with prostatic urethra preserved for benign prostatic hyperplasia Nianzeng Xing et al, China Andrology / Sexual Dysfunction Initial Study on Gene Recombination Induced Human Protein OCTN2 and 78 Epididymis Sperm Maturation Dongming Gong, et al., China Knock Down PDE5A3 Gene of Human Corpus Cavernosum Smooth Muscle Cells by siRNA in vitro Ji-Hong Liu et al, China Biodegradable poly-lactic-co-glycolic acid Maxpol-T/S as novel scaffold for adipose derived stem cells and fibroblast growth in vitro Zhong-Cheng Xin et al, China Effect of TGF-beta/Smad signaling on sertoli cell and possible mechanism related to complete sertoli cell-only syndrome. Zhongcheng Xin et al, China Use of Organ Culture to Study the Mouse Genital Tubercle Development: Effect of Exogenous Estrogen Zhong Wang et al, China Macau Sex Survey Pun Wai Hong, Macau Cardiovascular disease subsequent to erectile dysfunction – the new dimension to an intimate nexus: findings of a linked dataset. KK Chew, Australia Erectile dysfunction: Two common social habits, two divergent implications KK Chew, Australia The efficacy and safety of microsurgical parafrenular penile dorsal nerve neurotomy in the treatment of premature ejaculation Yu Chen, Taiwan Erectile Dysfunction Evaluated by the Use of Erection Hardness Score and Quality of Erection Questionaire in Taiwan TIS Hwang, Taiwan Electrical stimulation of cavernous nerve elicits simultaneous increase of intracavernous and seminal vesical pressure in the rat Kuang-Kuo Chen, Taiwan Priority of sex and importance of erection hardness among Chinese Thomas IS Hwang, Taiwan Epidemiology / Other The link between Obesity and Urological conditions - Findings from Subang Aging Male Study (SAM) 79 Hui Meng Tan, Malaysia Prevalence and Correlates of OAB in a multiethnic population Hui Meng Tan, Malaysia 11:20 -12:00 noon Session 3: Scientific Program Prostatitis – Clinical Strategy Moderators: Guang Sun, China; Ming Kwong Yiu, Hong Kong; Jong Khing Huang, Tawain 11:20 - 11:30 am North America Experience Durwood Neal, USA 11:30 - 11:40 am Experience from China Jihong Liu, China 11:40 - 11:50 am Experience from Taiwan Po-Hui Chiang, Taiwan 11:50 - 12:00 noon Experience from Malaysia Men Long Liong, Malaysia 12:00 - 12:10 pm 12:10 - 1:00 pm Discussion Lunch 1:00 - 1:30 pm Session 4: HKUA Lectures Moderators: Jianye Wang, China; Rei K. Chiou, USA; Lap Hong Ian, Macao 1:00 - 1:10 pm Use of Photoselective Vaporization of the Prostate for BPH in Hong Kong Chinese Patients" Richard Lo, Francis Lee and Bill Wong, Hong Kong 1:10 - 1:20 pm The destruction of the urinary tract by ketamine- HK perspective Peggy CHU Sau Kwan, Hong Kong 1:20 - 1:30 pm Discussion 1:30 - 2:10 pm Session 5: Panel Discussion Cystitis Glandularis - what is it? Moderators: Shan Chen, China; Joseph Chin, Canada; Thomas IS Hwang, Taiwan 1:30 - 1:40 pm Cystitis Glandularis - what is it? 80 Kuang Kuo Chen, Taiwan 1:40 - 1:50 pm The situation and challenge of Cystitis Glandularis in China QiangWei, China 1:50 - 2:00 pm Pathology nature of cystitis glandularis Steven Shen, USA 2:00 - 2:10 pm Discussion 2:10 - 3:50 pm Session 6: Moderators: 2009 AUA Abstract Highlights Liping Xie, China; Yuhui Wang, Sweden; Hui Meng Tan, Malaysia 2:10 - 2:20 pm Kidney Cancer Casey K. Ng, USA 2:20 - 2:30 pm Prostate Cancer Joseph Chin, Canada 2:30 - 2:40 pm Bladder Cancer Guan Wu, USA 2:40 - 2:50 pm BPH Carson Wong, USA 2:50 - 3:00 pm Voiding Dysfunction / Female Urology Donna Deng, USA 3:00 - 3:10 pm Sexual Dysfuntion Rei K. Chiou, USA 3:10 - 3:20 pm Infertility Philip Li, USA 3:20 - 3:30 pm Urolithiasis/Endourology Yuhui Wang, Sweden and Norway 3:30 - 3:40 pm Laproscopy/Robotic Surgery Tung Shu, USA 3:40 - 3:50 pm Urological Oncology: basic research Edmund Chiong, Singapore 3:50 - 4:00 pm Closing Remarks Zhangqun Ye, China; Jong Khing Huang, Taiwan 81 5. WCUS Meeting 2010 Date: Saturday, May 29, 2010 Venue: Moscone Centre, San Francisco, USA Theme: The Challenge in the World Chinese Urology 82 The 5th World Chinese Urological Society (WCUS) meeting in San Francisco, 2010. Tom F. Lue, MD, FACS and Run Wang, MD, FACS Since the inception of the 1st World Chinese Urological Society (WCUS) meeting at the AUA annual meeting held in Atlanta, Georgia in 2006, the WCUS has become one of the most active sub-specialty societies at the AUA. The initial participants included members from China, Taiwan, Hong Kong, Macau, Singapore, Thailand, Malaysia, Australia and North America. This was expanded to include people from Europe at the 2nd WCUS meeting held in Anaheim, California in 2007. At the upcoming 5th Annual WCUS meeting in San Francisco, we anticipate that more than 500 Chinese-speaking urologists and urologic scientists will be in attendance from all corners of the world including urologists from Mongolia who will be joining the family of the WCUS. The 5th Annual WCUS meeting will be condensed from the previous full day meeting to a full morning session with a noon poster assembly to allow plenty of time for all participants to mingle and make new friends. The theme of the 2010 meeting is the challenges for World Chinese Urologists, particularly facing the injuries from natural disasters and wars. These features are emphasized in this meeting from the lessons learned by the devastating earth quakes in China, 2008 and in Taiwan, 2009. The meeting will begin with a session to discuss experiences treating urethral strictures, a very common trauma disorder in Asia. Experts from China, Hong Kong and North America will review the evidence-based information and give their personal experiences regarding ideal surgical techniques for various complex urethral strictures or disruption. Following this session, two urologists with military backgrounds from China and North America will present their first hand experience facing natural disasters and war which may confront us during our careers. In light of the overwhelming information and limited time during the 83 AUA, we will continue to invite accomplished urologists and scientists to give the AUA abstract highlights for kidney, bladder and prostate cancers, BPH, voiding dysfunction/female urology, sexual dysfunction, and infertility. The AUA abstract highlight session in the last WCUS meeting was regarded highly by participants to catch the cutting edge of the basic and clinical science of urology. Again, holding the WCUS meeting during the annual AUA meeting serves as a venue to share the advancements in basic and clinical research in urology from the countries and regions mentioned above with the AUA members from other parts of the world. Even though our goal is to provide a platform for effective communication among Chinese-speaking urologists and urological scientists, the slides and posters will be presented in English, and we certainly welcome urologists and urological scientists from the entire world to attend this meeting and to meet our friendly and gifted Chinese colleagues. 84 Program - 2010 8:00 - 8:07 am Welcome and introduction Tom F. Lue, USA 8:07 - 8:10 am Report from Scientific Program Committee Run Wang, USA 8:10 - 9:00 am Session 1: Urethral Stricture – What is the Ideal Procedure? Moderators: Yanqun Na, China; Thomas IS Hwang, Taiwan; PC Tam, Hong Kong 8:10 - 8:20 am North America Experience Allen Morey, USA 8:20 - 8:30 am Mainland China Experience Yuemin Xu, China 8:30 - 8:40 am Hong Kong Experience Peggy Chu, Hong Kong 8:40 - 8:50 am Discussion 8:50 - 9:00 am WCUS awards 9:00 - 10:00 am Session 2: Urological Surgeons Facing War and Disasters Moderators: Zeyu Sun, China; Jong-Khing Huang, Taiwan; Tan Yeh Hong, Singapore 9:00 - 9:30 am Surgeon’s Challenge in Wars Arthur Smith, USA 9:30 - 9:50 am Surgeon’s Challenge in Earthquake Fengshuo Jin, China 9:50 - 10:00 am Discussion 10:00 -10:30 noon Session 3: MUA Lectures Moderators: Guang Sun, China; Ho Lap Yin, Hong Kong; Chi-Rei Yang, Taiwan 10:00 - 10:10 am Outcome of Radical Prostatectomy Li Kin, Pun Wai Hong, Ian Lap Hong, Lao Hio Fai, Tse Man Kin, Ho Son Fat; Macau 10:10 - 10:20 am Local Experience of Flexible Ureteroscopic Application Chan Tai Ip; Macau 85 10:20 - 12:10 pm Session 4: 2010 AUA Abstract Highlights Moderators: Jianye Wang, China; Ian Lap Hong, Macau; Hui Meng Tan, Malaysia 10:20 - 10:30 am Kidney Cancer Dingwei Ye, China 10:30 - 10:40 am Prostate Cancer Ming Li, China 10:40 - 10:50 am Bladder Cancer Guan Wu, USA 10:50 - 11:00 am BPH Xianghua Zhang, China 11:10 - 11:20 am Voiding Dysfunction/Female Urology Dongwen Wang, China 11:20 - 11:30 am Sexual Dysfunction Yutian Dai, China 11:30 - 11:40 am Infertility Philip Li, USA 11:40 - 11:50 am Urolithiasis/Endourology Simon SM Hou, Hong Kong 11:50 - 12:00 noon Laproscopy/Robotic Surgery Yuhui Wang, Sweden and Norway 12:00 - 12:10 pm Urological Oncology: basic research Benyi Li, USA 12:10 - 1:00 pm Session 5: View and Discuss Posters Kidney Disease and Renal Surgery Moderators: Shan Chen, China; Edmund Chiong, Singapore; Sidney Yip, Hong Kong 1. Is Contrast Enhanced Ultrasound a valid alternative diagnostic tool for Renal Cell Carcinoma in patients with renal impairment? Tay KJ, Ho H, Low A, Cheng C, Singapore 2. Laparoscopic Partial Nephrectomy Made Easy Francis Lee, Bill Wong, Richard Lo, Hong Kong 3. Severe renal infections - A review of clinical outcomes James C.M.Li, Chung Y, Tai CK, Fan CW; Hong Kong 4. 10 years Outcome of Radical Nephrectomy. Pun Wai Hong, Zhang Chong Yu, Ian Lap Hong, Li Kin, Lao Hio Fai, Tse Man Kin, Ho Son Fat, Macau 5. Retroperitoneal laparoscpic partial nephrectomy. Changjun Yin, Xiaoxin Meng, Ji Li, China 86 6. The long-term follow-up for living-related donors undergoing laparoscopic nephrectomy (158 cases). Lulin Ma, China 7. The experience of single-port laporoscopic surgery. Yinhao Sun, China 8. Impact of Kidney Disease Outcomes Quality Initiative (KDOQI) Guidelines on the Prevalance of Chronic Kidney Disease (CKD) After Living Donor Nephrectomy Tan L, Wu Fiona, Raman L, Tai BC, Consigliere D, Tiong HY; Singapore Adrenal Surgery and Urinary Lithiasis Moderators: Jian Huang; China, SK Mak; Hong Kong; George Lee, Malaysia 9. Experience of laparoscopic treatment of complicated pheochromocytoma. Hanzhong Li, Weigang Yan, Weifeng Xu, China 10. The risk factor analysis of the 24-hour urine components for patients with lithiasis Guohua Zeng, China 11. Treatment of renal calculi with Holmium laser lithotripsy through digital flexible ureteroscope. Yue Cheng, Xiaodong Shi, Jiasheng Hu, Zejun Yan; China 12. Anterograde flexible ureteroscopic lithotripsy in the management of ureterointestinal anastomotic calculus in patients with Bricker urinary divesion. Wei Xue, China. 13. Study on expression of Calcium oxalate crystals stimulating macrophages NADPH oxidase. Yaoliang Deng , Binghua Sun, Chengyang Li; China. 14. Experimental investigation of the idiopathic hyperoxaluria formation mechanism in rats. Zhiqiang Chen, China Bladder Diseases and Surgery Moderators: Liping Xie, China; Po-Hui Chiang, Taiwan; Kavirach Tantiwongse, Thailand 15. A Retrospective Review of the Effect of Botulinum Toxin A on Nonneurogenic Detrusor External Sphincter Dyssynergia (DESD) Tricia Kuo, Ng Lay Guat, Singapore 16. In vitro and in vivo Relaxation of Urinary Bladder Smooth Muscle by the Selective Myosin II Inhibitor, Blebbistatin Xinhua Zhang, Dwaraka Srinivasa R Kuppam, Arnold Melman, Michael E DiSanto, USA 17. The mechanism of the detrusor damage for patients with diabetes. Dongwen Wang, China 18. The prevalence of OAB in China. 87 Kexin Xu,China 19. Overative bladder (OAB) and its relationship with prostatic calcification Tan WS, Malaysia 20. Management of the Distal Ureter/Bladder Cuff in Laparoscopic Nephroureterctomy Richard Lo, Bill Wong, Francis Lee, Hong Kong Prostate Cancer Moderators: Qiang Ding, China; Shu-Pin Huang, Taiwan; Berry Fung, Hong Kong 21. Robotic-assisted transperineal prostate biopsy: 3-years experience Henry Ho, Preethi M, Yuen JY, Lim E, Li DL, Ng WS, Cheng C, Singapore 22. Pathologic outcome in men with prostate cancer suitable for active surveillance after radical prostatectomy Grace Tan, Weber Lau, Huang HH, C Cheng, Singapore 23. Infectious Complication after Transrectal Ultrasound-guided Prostate Biopsies: A Review of 1525 Cases CH Cheng, CH Yee, Y Chiu, WF Lee, HC Chan, CK Tai, C Yu, HS So, SK Chu, CW Fan, MK Yiu, V Velayudhan, CW Man; Hong Kong 24. Early continence outcomes after robotic radical prostatectomy - impact of vesicourethral reconstruction Ho KL, Wong CW, Au WH, Chu SM, Tam PC, Hong Kong 25. Experience of Hormone Therapy for Advanced Prostate Cancer. Lao Hio Fai, Ian Lap Hong, Pun Wai Hong, Li Kin, Tse Man Kin, Ho Son Fat; Macau 26. Extraperitoneal laparoscopic radical prostatectomy (162 cases). Jian Huang, Tianxin Lin, Cun Chang; China 27. The survey of the PSA level of 16233 healthy Chinese male. Zhicheng Gua; China 28. Zoledronic Acid Enhanced Growth Inhibition and Apoptosis in Both Hormone-Refractory and Hormone-Sensitive Prostate Cancer Cell Lines Yi-Chia Lin, Taiwan 29. Localized Prostate Cancers Treated with CyberKnife Delivered Hypofractionated Radiotherapy:An initial Experience and Outcome Analysis Chia-Cheng Su, Taiwan 30. Association Analysis of the WNT Pathway Genes on Prostate Specific Antigen Recurrence after Radical Prostatectomy Shu-Pin Huang, Taiwan 31. Prognostic Significance of Prostate Cancer Susceptibility Variants on Prostate-Specific Antigen Recurrence after Radical Prostatectomy Shu-Pin Huang, Taiwan BPH/LUTS/Urethral Disease Moderators: Daling He, China; Gregory Y. Jia, USA; Nansalmaa Naidan, Mongolia 32. A randomized control trial on the prevention of secondary haemorrhage after TURP with perioperative antibiotics prophylaxis 88 CH Yee, LY Ho, Hong Kong 33. Metabolic Syndrome & LUTS Tan HM, Malaysia 34. LUTS & QoL issue Tong SF, Malaysia 35. The associations among enos g894t gene polymorphism, erectile dysfunction, and benign prostate hyperplasia-related lower urinary tract symptoms Shu-Pin Huang, Taiwan 36. The experience in the treatment of complicated urethral stricture. Hong Li, China 37. Application of Animal Tissue Model for 2 micro Laser Technique Training. Gang Zhu, China 38. Iatrogenic Urethra Trauma of Male Patient Results from Urethra Catheterization---- A Private Community Hospital Experience Shiang-Ming Lin, Taiwan 39. Inlay Buccal Mucosal Graft: A Novel Technique for Re-operative Posterior Urethroplasty Shou-Hung Tang, Taiwan 40. The experience of treatment for severe hypospadias in 25 years Jesun Lin, Taiwan 41. Prevalence of the lower urinary tract symptoms in Chinese males: Results of the Chinese EPIC study Yan B, Lin TL, Yang Y, Chan CK, USA, Taiwan, China, Hong Kong Andrology / Sexual Dysfunction Moderators: Xiaofeng Wang, China, Li Man Kay, Singapore; KK Chew, Australia 42. Pattern of mortality in men with erectile dysfunction KK Chew, Australia. 43. The Streptozotocin-induced Type 1 Diabetes (T1D) Rat Model Exhibits Altered Smooth Muscle Myosin Isoform Composition Consistent with Heightened Corpus Cavernosum Smooth Muscle Tone and Erectile Dysfunction Xinhua Zhang, Dwaraka Srinivasa R Kuppam, Arnold Melman, Michael E DiSanto, USA 44. Diabetes Upregulates the Sphingosine-1-Phosphate (S1P) and RhoA/Rho-kinase Signaling Pathways in Both Rat and Human CCSM Resulting in Enhanced S1P-induced CCSM Contractility Xinhua Zhang, Dwaraka Srinivasa R Kuppam, Arnold Melman, Michael E DiSanto, USA 45. Sphingosine-1-phosphate in vitro and in vivo Modulates Corpus Cavernosum Smooth Muscle Tone Xinhua Zhang, Dwaraka Srinivasa R Kuppam, Arnold Melman, Michael E DiSanto, USA 46. Sexuality and Management of Benign Prostatic Hyperplasia with Alfuzosin Thomas IS Hwang, Taiwan 47. Elicitation of simultaneous increase of bilateral seminal vesical pressures after electrical stimulation of lesser splanchnic nerve in the rat 89 Kuang-Kuo Chen, Taiwan 48. Response of corpus cavernosum to vasoactive agent in the hyperprolactinemic rat Kuang-Kuo Chen, Taiwan 49. The prevalence of and risk factors for androgen deficiency in aging Taiwanese men Shu-Pin Huang, Taiwan 50. Update of the Asian Journal of Andrology 2010 Dangqing Ren, AJA 51. Vacuum therapy in penile rehabilitation via anti-hypoxic, anti-apoptotic mechanism Jiuhong Yuan, Haocheng Lin, Angel Paredes, Yutian Dai, O. Lenaine Westney, Run Wang, USA 52. Gene Therapy with SuperEnzyme for ED after cavernosal nerve crush injury in rat Haocheng Lin, Jiuhong Yuan, Ke-He Ruan, Yutian Dai, Run Wang, USA 1:00 - 1:10 pm Abstract Award and Closing Remarks Zhangqun Ye, China; Ming-kwong Yiu, Hong Kong 2010 WCUS Best Posters. 1. The long-term follow-up for living-related donors undergoing laparoscopic nephrectomy (158 cases). Lulin Ma, China 2. Study on expression of Calcium oxalate crystals stimulating macrophages NADPH oxidase. Yaoliang Deng , Binghua Sun, Chengyang Li; China. 3. Management of the Distal Ureter/Bladder Cuff in Laparoscopic Nephroureterctomy Richard Lo, Bill Wong, Francis Lee, Hong Kong 4. Robotic-assisted transperineal prostate biopsy: 3-years experience Henry Ho, Preethi M, Yuen JY, Lim E, Li DL, Ng WS, Cheng C, Singapore 5. The associations among enos g894t gene polymorphism, erectile dysfunction, and benign prostate hyperplasia-related lower urinary tract symptoms Shu-Pin Huang, Taiwan 6. Gene Therapy with SuperEnzyme for ED after cavernosal nerve crush injury in rat Haocheng Lin, Jiuhong Yuan, Ke-He Ruan, Yutian Dai, Run Wang, USA 6. WCUS Meeting 2011 90 Date: Saturday, May 14, 2011 Venue: Walter E Washington Convention Centre, Washington DC, USA Theme: Prostate, Evidence Based Medicine and Men’s Health 91 The 6th World Chinese Urological Society (WCUS) meeting in Washington DC, 2011. Tom F. Lue, MD, ScD (Hon), FACS and Run Wang, MD, FACS The World Chinese Urological Society (WCUS) will hold its 6th annual meeting in Washington DC on May 14, 2011. The WCUS is a thriving organization that is enthusiastically supported by the AUA, the Chinese Urological Association (CUA), Taiwanese Urological Association (TUA), Hong Kong Urological Association (HKUA), Macao Urological Association (MUA) and the Singapore Urological Society as well as numerous urologists from all over the world. It has become one of the most active sub-specialty societies at the AUA. We anticipate that more than 500 Chinese-speaking urologists and urologic scientists will be in attendance from all corners of the world. The 6th Annual WCUS meeting will be a 5-hour session with special lectures, topic-oriented mini-symposiums and AUA highlights. Dr. Paul Lange will give the inaugural Lo Ping-wan Memorial Lecture entitled “Provenge and the endangered surgeon scientists”. Chinese urologists and uro-scientists hold the key to deliver world-class urologic care for the more than 1.3 billion Chinese people worldwide. All the above-mentioned societies and governments are making great efforts to support and encourage physicians to engage in research and scientific discovery and we hope this lecture will inspire many in the audience to purse an exciting career. Lower urinary tract symptom (LUTS) from benign prostatic hyperplasia (BPH) is one of the most common urologic diseases in Chinese patients. The plethora of treatment is often confusing to the public as well as many practicing urologists. A mini- symposium to address diagnosis and various treatment options will help clarify the confusion. The past decade has seen an increasing incidence of prostate cancer in Chinese speaking regions of the world. Another minisymposium will be devoted to this topic. A male health symposium that will 92 feature a lecture on “Obesity and Testosterone deficiency” and a lecture entitled “prosthetic devices for men”. Although far from perfect, evidence-based medicine is a well-established practice in the US. Dr. Steven Canfield, the AUA evidence based medicine course director will also give a special lecture to explain and encourage this practice. Three industry-sponsored lectures will be given by Dr. Harn Chorng Kuo (Pfizer), Dr. Farid Saad (Bayer) and Dr. Run Wang (AMS). In consideration of the overwhelming information and limited time during the AUA meeting, we will continue to invite accomplished urologists and scientists to give the AUA abstract highlights for kidney, bladder and prostate cancers, BPH, voiding dysfunction/female urology, stone, endourology/robotic surgery, sexual dysfunction and infertility. The AUA abstract highlight sessions in the past WCUS meetings were rated highly by participants. Holding the WCUS meeting during the annual AUA meeting serves as a venue to share cutting edge information in basic and clinical urology for Chinese speaking urologists and friends as well as for social networking. Even though our goal is to provide a platform for effective communication among Chinese-speaking urologists and urological scientists, the slides will be presented in English, and we welcome all urologists and urological scientists to attend this meeting and to meet our friendly and gifted Chinese colleagues. 93 Program - 2011 8:00 - 8:05 am Welcome and introduction Tom F. Lue, USA 8:05 - 8:10 am Scientific Program Run Wang, USA 8:10 - 8:35 am Session 1: Lo Ping-wan Memorial Lectureship Moderators: Richard Lo, Hong Kong; Hong-Jeng Yu, Taiwan; Apichat Kongkanand, Thailand 8:10 - 8:30 am Provenge and the endangered surgeon scientists Paul Lange, USA 8:40 - 8:50 am Discussion 8:35 - 9:10 am Session 2: Endourology and BPH Moderators: Zeyu Sun, China; Tung Shu, USA; Ming-Kwong Yiu, Hong Kong 8:35 - 8:45 am The first step to be a good endourologist: urologists training with simulators in China Yanqun Na, China 8:45 - 8:55 am Revisiting the management of Male LUTS – can we use symptoms to guide initial diagnosis and treatment? Kuo Harn Chorng, Taiwan 8:55 - 9:05 am TUR in saline plasma vaporization (Button) Peggy Chu, Hong Kong 9:05 - 9:10 am Discussion 9:10 - 9:15 am WCUS awards 9:15 - 9:50 am Session 3: Evidence Based Medicine in Urology Moderators: Yinghao Sun, China; Yao-Chi Chuang, Taiwan; Kavirach Tantiwongse, Thailand 9:15 - 9:30 am Evidence Based Medicine for Urologists: a review from AUA evidence based medicine course director Steven Canfield, USA 94 9:30 - 9:45 am Evidence Based Medicine for Urologists: status in China Qiang Wei, China 9:45 - 9:50 am Discussion 9:50 - 10:40 pm Session 4: Radical Prostatectomy: Surgical Tips and Outcomes Moderators: Guang Sun, China; Steve Chan, Hong Kong; Edmund Chiong, Singapore 9:50 - 10:05 am Robotic Assistant Christopher Cheng, Singapore 10:05 - 10:20 am Laparoscopic Lulin Ma, China 10:20 - 10:35 am Open Chi-Rei Yang, Taiwan 10:35 - 10:40 am Discussion 10:40 - 11:15 am Men’s Health Issues Session 5: Moderators: Tiejun Pan, China; Shaw Zhou, USA; Ban-Ping Jiann, Taiwan 10:40 - 10:55 am Combined surgical therapy for male stress incontinence and ED Run Wang, USA 10:55 - 11:10 am Obesity and testosterone deficiency - why this is of interest for the urologist Farid Saad, Germany 11:10 - 11:15 am Discussion 11:15 - 12:35 pm Session 6: 2011 AUA Abstract Highlights Moderators: Liping Xie, China; Lao Hio Fai, Macau; Carson Wong, USA 11:15 - 11:25 am Kidney Cancer Liping Xie, China 11:25 - 11:35 am Bladder Cancer Dai-Lung Cha, Taiwan 11:35 - 11:45 am Prostate Cancer Ningchen Li, China 11:45 - 11:55 am BPH Chan Tai Ip, Macau 95 11:55 - 12:05 pm Voiding Dysfunction/Female Urology Dominic Lee, Australia 12:05 - 12:15 pm Urolithiasis/Endourology Kwan Lun Ho, Hong Kong 12:15 - 12:25 pm Sexual Dysfunction / Andrology/Infertility Eric Chung, Australia 12:25 - 12:35 pm Laproscopy/Robotic Surgery Yuhui Wang, Sweden and Norway 12:35 - 12:40 pm Session 7: Scientific Publication Moderators: Guan Wu, USA; Philip Li, USA; Yutian Dai, China 12:35-12:45pm 12:45-12:55pm 12:55 - 1:00 pm How to get your urological-andrology research published at the AJA successfully? Danqing Ren, AJA How to demonstrate the research outcomes? Suning You, Chinese Medical Association Closing Remarks Zhangqun Ye, China 96 97