EHR workshop Recommendations - Interaction Model
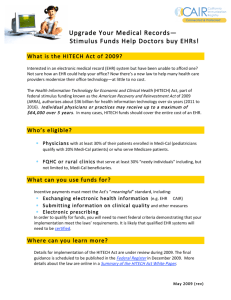
advertisement

Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 Primary and secondary use of EHR systems: Enhancing clinical research for better health and high quality healthcare Recommendations from STREAM A. Interaction Model Isabelle de Zegher, co-chair, Novartis, EFPIA Georges De Moor, co-chair, EUROREC Marc Peeters, rapporteur, Roche, EFPIA Note: This document reports the work of a workshop on interaction model and organizational aspects in the context of Primary and secondary use of EHR systems. The recommendations included will develop as the work continues and should be read as a work in progress. Any comments should be sent to the co-chairs. Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 Table of contents 1. SCOPE AND OBJECTIVE ........................................................................................... 3 1.1 Background......................................................................................................... 3 1.2 Details on use case ............................................................................................. 4 1.2.1 Patient recruitment ............................................................................... 4 1.2.2 Electronic data capture ......................................................................... 5 1.2.3 Safety.................................................................................................... 5 2. SUMMARY OF KEY DISCUSSION POINTS ........................................................... 5 2.1 Common Issues .................................................................................................. 5 2.1.1 Source & quality (completeness & accessibility) of data: .................... 5 2.1.2 Usage of data for “commercial” purpose ............................................. 6 2.1.3 Workflow: how to ensure seamless integration ................................... 6 2.2 Third Party .......................................................................................................... 6 2.3 “Business case” .................................................................................................. 7 2.4 Framework for interaction .................................................................................. 7 3. RECOMMENDATIONS ............................................................................................... 8 3.1 Develop Service definition for EHR usage ........................................................ 8 3.2 Communication on eHR use and benefits: ......................................................... 8 3.3 Third party: ......................................................................................................... 8 3.4 Collaboration forum: .......................................................................................... 9 3.5 Roadmap............................................................................................................. 9 3.5.1 2008 Milestones description ................................................................ 9 3.5.2 2009 Milestones description .............................................................. 10 4. CONCLUSION AND NEXT STEPS .......................................................................... 10 5. APPENDICES ............................................................................................................... 11 5.1 Agenda.............................................................................................................. 11 5.2 Participants to the STREAM ............................................................................ 13 5.3 Details from Brainstorming session ................................................................. 14 5.3.1 Service Definition .............................................................................. 14 5.3.2 Communication .................................................................................. 15 5.3.3 Third Party.......................................................................................... 16 5.3.4 Common Discussion Forum ............................................................... 16 5.3.5 Roadmap ............................................................................................ 17 Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 1. SCOPE AND OBJECTIVE 1.1 Background There are about 15 different use cases for the potential usage of EHRs in the context of clinical research as indicated in the following figure (source: Slipstream project). There are no evident quick wins, but some use cases are more feasible than others. Clinical Research Clinical Development 1. Genetic Regulatory / Safety 3. Clinical Trial Execution Association and Linkage Analysis 10. Post-Marketing a. Connect Patients to Trials a. Safety / Adverse Event Monitoring b. Data Collection & Mgmt 2. Clinical c. Investigator Services Validation – Target, Biomarker, and Diagnostic b. Pharmacovigilance d. Compliance e. Placebo Populations c. P-Epi & Data Mining Prioritized High-Level Use Cases Commercial 12. Pharmacoeconomics 13. Marketing Comparative Studies 14. Pharmaceutical/ Disease Management Programs 4. Clinical Trial Simulation 15. e-Prescribing 5. New Indication 11. Manufacturer’s Identification Recall 6. Interim analyses 7. Personalized Medicine – Pharmacogenomics 8. Outcomes Studies 9. Disease and Care Management Modeling Today however there is insufficient communication: clinical care and clinical research are two totally separate “electronic worlds” (except for some aspects of EDC) that would benefit by “breaking the wall” to get to real electronic data exchange Patient recruitment GP’s Office GP’s Office Clinical trial simulation GP’s Office GP’s Office New indication identification Personalized medicine Pharma Industry Hospital Hospital Pharmacovigilance GP’s Office Pharmaco-economics Pharma Industry GP’s Office ePrescribing GP’s Office Hospital Hospital GP’s Office Predictive safety Pharma Industry Pharmaceutical/disease management Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 To break the wall, technology and technical standards (discussed in Stream B) are necessary but not sufficient. We need as well to clarify the legal hurdle (discussed in Stream C) and the organizational aspects, including financial aspects. Benefits of EHR integration for clinical research are MAJOR; but the costs are ALSO major if we keep the current interaction model: “one hospital/one sponsor” , representing “n to m” electronic interfaces. The basic questions that were addressed to the team A are: How to adapt interaction models & processes to ensure benefit at affordable cost? – Should internal processes change both in providers & sponsors organization ? – Should we define new roles and new skills ? – Should we put in place new actors such as a third party ? How to build a common vision across Health Care to implement these changes – How can we build a shared understanding of the needed changes – How can we build a communication forum across Health Care to ensure effective implementation ? 1.2 Details on use case Three use cases were proposed to the participants – with more specific questions Patient recruitment Electronic data capture Safety 1.2.1 Patient recruitment Scope There are different components in patient recruitment Evaluation of protocol feasibility based on availability of patient population as specified by inclusion/exclusion (i/e) criteria. The ability to do this more effectively before starting a study allows more “feasible” protocols to be designed and therefore to move faster in trials Identification and enrollment of investigators who have patients with identified i/e criteria. There is no benefit to this step – taken alone; identification of patient and investigator does not guarantee actual patient recruitment. Actual enrollment of patient within a study – following evaluation of i/e criteria Protocol feasibility Investigator enrollment Patient enrollment Potential changes required for more effective use of EHR New roles and processes – Within sponsors, there is a need to generate protocols in a more“structured” way (i.e. with computable i/e criteria that can easily be checked across different EHRs) – Increase IT skills/collaboration during the whole process Would a third party be useful?. If yes which type, which services ? – A third party could decrease constraints related to privacy issues (this needs to be verified by Stream C) – A third party could decrease cost of technical integration (going from “n to m” interfaces to only m) Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 – A third party could provide additional services (act on behalf of caring physician,…) to speed up the process 1.2.2 Electronic data capture Scope/Issues. Today it is estimated that about 80% of the data needed for clinical research are already collected in clinical care (paper or electronic format). How can we have easier access to these data, what about the additional “new” data (integration and ownership)? Potential changes New roles and processes – Should we have a tighter integration of clinical care and clinical research processes within the provider organizations ? – How to “seamlessly” adapt EHR for “new” data acquisition ? – Any changes in the role of CRA versus investigator ? Would a third party be useful. If yes , which services ? Would it be another type of CRO ? 1.2.3 Safety Scope pre-launch versus post-launch Signal detection versus Adverse Events reporting Potential changes How do we ensure that we have “validated” information on drugs ACROSS Europe to ensure correct imputation To enable predictive safety with effective data mining – assuming data can be pooled and integrated within existing EHR databases – are the current types of organizations, skills and processes right ? Do we really need to have electronic data exchange or should the sponsors work directly with the providers within their organization (no need for data exchange) What is the impact on pharmacovigilance ? Should we revise the process ? 2. SUMMARY OF KEY DISCUSSION POINTS All presentations will be available at the following address http://www.eurorec.org/EHRWorkshop/model.cfm?selection=model&actief=EHRWorkshop (additional presentations from the other streams are also available at the same site). In the following we only summarize key discussion points, consolidated during the workshop across the 3 uses case 2.1 2.1.1 Common Issues Source & quality (completeness & accessibility) of data: Data coming from providers/clinical care : most of the data are coming from billing o Registry & billing (information available as well within payers): 90% in EU o CPOE: 18% in Sweden… (if this is available + possible to do safety) o Ambulatory eHR system: 2% in Sweden o Clinical data repository: starting…. Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 => information – such as knowledge of AE - is available in text BUT NOT available in in structured form in EHRs. => possibility to increase with financial incentive ? Data coming from clinical research (clinical researchers in provider organization, pharma) o Clinical research data Clinical trial Data are there but not available – pharma would be open to make available protocol and meta-data (such as class side-effect) but not results DB o What should be ready to share ? GTB DB from AMIA is not a success Clinical care: GIGO (Garbage In Garbage out) Clinical research: GIGO (Gold In Gold Out)) => SIGO (Silver In – Gold Out) 2.1.2 2.1.3 Usage of data for “commercial” purposes We need to identify better sources of available data => we do not even a catalog of data; need to have a typology of the data as well Need to change mindset and culture: clinical research leads to improved care => it should not be considered as a “secondary” use ! Currently we need authorization to access the data for usage which is not the original use, e.g. Informed consent => takes time, puts excessive load on daily practice. o We should put in place solutions such as preview mechanism, financial reward, work delegation possible o Do we really need informed consent in a world where physicians and sponsor are “responsible” parties…. Workflow: how to ensure seamless integration EHR versus eCRF: How to ensure seamless integration of clinical care and clinical research as a continuum rather than two different entities with redundant patient data entry How to monitor data for AE that will come in the future => how to ensure that data from clinical research are integrated into clinical care (will be critical mostly for devices in the future) 2.2 Third Party Different potential models for third parties (several already in place in Europe) public : money from government; e.g. GPRD: model of “real-world” data collected longitudinal record business (e.g. CRIX), public-private partnership, non –profit but self sustained e.g. CRIX: model of sequencing: first efficacy and safety before launch and then monitoring data collected as part of existing process academic: research money (from grants and government) e.g. Erasmus University Rotterdam – hospital Which of the model offers the most trustworthiness and the highest quality of data (accuracy, completeness)? Difficulties to set up a third party ? political environment more difficult than technology ! Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 technical integration and legal aspects - critical to have a Trusted Third Party to solve the different technical and legal aspects feasible in the pharma/regulatory world – but for EHR integration would require gradual integration Several third parties of different types already exist in Europe => need to make inventory . possibility of federation of existing third parties ? What are the requirements/services for a third party Technical integration Legal “guardian” Third party data can bring as well services to patients ? usage of patient as placebo data ? Handles all data versus data on demand and build Intermediate between hospital and payers 2.3 “Business case” Benefits of EHR integration is potentially huge – faster and more efficient clinical development process, increase safety – but the cost of a fully scalable solution may be even higher unless we change the way we work. Who makes the money ? when hospital and GP – and patients - become aware of the value of their data the model may change – however there is value on the data only if they are pooled not at individual level ! The society benefits NOT the individual EU will work as there is collective health – in US it is the individual protection first however there is still a benefit to share the data 2.4 Framework for interaction We need a paradigm shift Quality of data : From low data, reactive high cost – to high data pro-active Data mining – hypothesis testing can be possible – only if there is a strict governance process: how can we go hypothesis strengthening in the real word Availability/sharing of data: Definition of interaction model is composed of Description of the processes & workflow - where it applies (from end to end – with the need for change from the current situation to the future) Definition of Pre and post conditions Description of input and output (concepts and controlled terminologies) Implementation of new interaction model will require a framework with Governance structure of transformation Budget – with realistic scope Organization & People and stakeholder management Technology infrastructure Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 3. RECOMMENDATIONS Four focus areas were identified during the workshop and further elaborated. In the following we only provide a summary of the ideas (see appendix for further details) 3.1 Develop Service definition for EHR usage Scope Which type of services must be defined to allow for EHR integration. How de we define and implement services, how do we get a holistic approach (people/process, technology and business case). How can IT vendors be involved as a consortium (integrating EHR vendors and EDC vendors); need to clarify role of certification We need to understand which type of data are available (catalogue of data ?) We need to start with a pilot and get more input from pharma & health care (only one step but a piece of the puzzle) – define interaction model Proposal is to support the CRFQ project (clinical research filter query – see presentation from Mead on site); with links between GPs, hospitals and vendors to ensure applicability of services like CRFQ across different computer systems Practical next steps: start with a pilot building upon CRFQ to learn on how to work together for defining services in a more structured way Evaluate implementation of a standard service such as Clinical Research Filtered Query (CRFQ). A request would be issued by a clinical research organization, be forwarded to Health Care providers (hospital, third parties like GPRD, other regional or national Databases) to evaluate patient population against specific criteria. Evaluate business process changes in the context of protocol feasibility, patient recruitment and safety monitoring Evaluate business case – benefits and cost for full implementation across the health Care chain Evaluate how to work together as a Health Care “continuum” to further defined service in the clinical research area 3.2 Communication on EHR use and benefits: Scope One of the concerns is the time required to have patient approval for usage of data – communication on the value of using pooled/integrated EHR data should be communicated We need to re-insure patient representatives/ press / media that there is nothing that should frighten the public in using their data => explain why we need access to data and decrease the worry => explain the semantic / decrease misunderstanding/emotions Practical next steps: need to defined strategy and communication plan – no precise action taken yet 3.3 Third party: Scope We need to clarify the following aspects what are the existing third parties in Europe, Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 how do we set up a third party in Europe, what should be the business model how to integrate services - like CRFQ - within third party and related process changes => will this accelerate the implementation ? Practical next steps: Need to define a Third party – taking into account technical (from Stream B) and legal (from Stream C) requirements. Agreed in plenary to start a project working on the definition of a European Third party 3.4 Collaboration forum: Scope We need to have a structured way of collaborating – currently HC providers and pharma do not have a common collaboration forum. We need to clarify the mission statement and governance model of this collaboration forum and identify possibility to expand existing collaboration forum – rather than to build and maintain another one Practical next steps Need to follow up between European Commission, EUROREC, EFPIA 3.5 Proposed Roadmap Operational level CRFQ pilot Strategic level 2008 Strategic plan 2009 CRFQ in production (onco ?) Catalog of data 2010 2011 CRFQ model as basis across EHR Free access to catalog of data EU Third Party Kickoff or NO GO Public DB with info on medicinal products First Communication 1st draft guidance IMI call 3.5.1 2008 Milestones description CRFQ pilot Agreed project definition, catalogue of available resources, strategy for further funding, success criteria: CRFQ Proof of concept complete, Communications strategy implemented, Positive feedback Communication : publish within `news monitor` Catalogue of data Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 3.5.2 o Develop a catalogue of databases, built from EHRs, that are currently available across Europe for researchers – both within the source institutions and beyond – to access and use. Euro-EHR data compendium adopting UK example Develop strategic place Capture case studies + best practices + develop 1st draft guidance Have at least one large scale Academia – Hospital – IT industry – Pharma project topic defined within the IMI call process 2009 Milestones description I/E CRFQ implemented on existing EHRs (Cancer) o CRFQ operational in 3 sides o CRFQ as DSTU in Q1 2008 + OMG RFP in Q2 2008 o One service in pilot , is the basis of learnings needed to build roadmap Collaboration Forum in place o Organization / framework for decision making in place o Charter agreement of common discussion forum o Definition of an IHE Technical Framework for clinical research (to be able to test something at the 2009 or 2010 Connectathon Go / no go understanding of need and value of third party o Mobilize Pharma industry to identify / launch a common EHR platform (summit) o Third party business case assessed + deliverables of Discussion Forum achieved o Public template for workflows within study protocols Pilot of first service 2010 - Milestone description CRFQ as standard connectors - Run a pilot study on a fully integrated EHR across boarders; Assess need for a follow-up project European free official database of drugs, usage, important adverse events, brandname in each country, unique ID etc. Catalogue of data available freely. Publish answer to the question `how much data is available in EHRs that can be used directly in clinical trials` 4. CONCLUSION AND NEXT STEPS Focus up to February 2008 (next meeting) will be on o Developing a project around of CRFQ (technical aspects being developed under HSSP, project to focus on testing, organizational aspect and business case). Project charter to be defined for a kick-off in November. o Collaborating with stream B on the establishment of a third party Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 5. APPENDICES 5.1 Agenda (note: all presentations can be found under www.eurorec.org – see EHR workshop on the left hand side – then select “interaction model” tab in the page Thursday 11th October (afternoon) Time Title Author Overall introduction 14:30 – 14:45 Introduction to the session: participants and expectation G. De Moor, (15 min) I. de Zegher 14:45 – 15:05 Lessons learnt on secondary usage of data from the UK J. Parker (20 min) NHS CRC study 15:05 – 15:25 Lessons learnt from CRIX, a third party in place in the J. Bland (20 min) US: interaction model, setting up, benefits and concerns of several months of operations Focus on Patient recruitment. Patient recruitment: from today’s paper based process to “24 hours recruitment”” is a technology supported by process changes enough or do we need a third party to solve legal issues and technical heterogeneity. 15:25 – 15:45 Identifying and recruiting patients for clinical trials in R. Thwaites (20 min) the future: a pharma perspective 15:45 – 16:15 Hospital/Health care perspective J. van der Lei (20 min) 16:15 – 16: 30 BREAK (15 min) 16:30 – 16:50 IT perspective C. Mead 16:50 – 17:15 Discussion and recommendations for actions I. de Zegher, (25 min) G. De Moor, Focus on Electronic data capture. Can EHR replace the need for eCRF, what is the impact on the investigator-clinical monitor roles 17:15 – 17:35 A detail on the process: pharma perspective H. Donovan (20 min) 17:35 – 17:45 Hospital/Health care perspective C. Le Bozec (20 min) 17:45 – 18:05 IT vendors perspective JF Penciolelli (20 min) 18:05 Close of session 18:30 – 19:30 Meeting Organizing Committee Organizing BU33 0/54 Committee Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 Friday 12th October (morning) Time Title Author Focus on Electronic data capture. Can EHR replace the need for eCRF, what is the impact on the investigator-clinical monitor roles 08:30 – 09:00 Discussion and recommendations for actions G. De Moor, (30 min) I. de Zegher Focus on Safety. Availability of EHR database and data warehouse: a new safety model ? impact on the current pharmacovigilance models ? 09:00 – 09:20 A detail on the process: pharma perspective S. Markel-Fox (20 min) 09:20 – 09:40 Hospital/Health care perspective C. Lovis (20 min) 09:40 – 10:00 IT vendors perspective Sarah Payne (20 min) 10:00 – 10:20 Authorities perspective N.N. EMEA, (20 min) TBC 10:20 – 10:40 BREAK (20 min) 10:40 – 11:10 Discussion and recommendations for actions on safety I. de Zegher, (30 min) G. De Moor Consolidated recommendations (Identify person responsible for reporting during plenary) 11:10 – 12:30 Key messages from the different focus areas G. De Moor, (1h 20 min) Consolidated recommendations I. de Zegher Practical next steps 12:30 Close of session - LUNCH Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 5.2 Participants to the STREAM James Michael Georges Isabelle Hugh Danielle Christel Christian Suzanne Charlie John Sarah Jean Francois Marc Barbara Rob Johan Alain Tim Bland Dahlweid de Moor de Zegher Donovan Dupont Le Bozec Lovis Markel-Fox Mead Parkinson Payne Penciolelli Peeters Tardiff Twaites van der Lei Venot Buxton CRIX Agfa Healthcare Eurorec Novartis Accenture BMS APHP / INSERM Geneva Univ Hospitals GSK NCI – Booz Allen MHRA, GPRD, UK IBM Oracle Roche Parexel GSK Erasmus Rotterdam SMBH EMEA james.l.bland@crixintl.org michael.dahlweid@agfa-healthcare.fr Georges.DeMoor@UGent.be isabelle.dezegher@novartis.com hugh.c.donovan@accenture.com danielle.dupont@bms.com Christel.Lebozec@spim.jussieu.fr christian.Lovis@sim.hcuge.ch Suzanne.L.Markel-Fox@gsk.com mead_charlie@bah.com John.Parkinson@mhra.gsi.gov.uk sarah.payne@uk.ibm.com jean-francois.penciolelli@oracle.com Marc.peeters@roche.com barbara.tardiff@parexel.com rob.m.thwaites@gsk.com j.vanderlei@erasmusmc.nl avenot@smbh.univ-paris13.fr Tim.Buxton@emea.europa.eu Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 5.3 Details from Brainstorming session Four topics were identified (service definition, communication on eHR use and benefits, third party, collaboration forum) during the workshop. The participants of the work stream were asked to provide one specific idea/next step related to each topic – and then to put a critical milestone in the roadmap. This is the detailed results. All ideas have been captured and grouped, and reproduced herewith exactly as written by participants. 5.3.1 Service Definition How do we define services Develop cost/benefit analysis for each and any service Case definition service is the key to aggregation across Europe. Who is doing it now. Capture the details of the case studies + use learning to define guidance around governance, people, processes and technologies Define a proof of concept and execute a proof of concept implementation strategy Specific clinical service definition should be coupled with terminology service definition since the semantic is a so important issue +++ In today`s Health Information Systems (the Source level), be it in hospital care or ambulatory care settings, we need to develop new subsystems, components, modules (with processes around) to address the specific purpose of research. We need a requirements analysis. A first step could be to define business functions, content criteria serving as quality criteria for those systems. Certification can help to bring together Pharma and IT vendors. Pharma industry should provide label information in an electronic form, structured so that the information can be easily handled electronically to develop alerts and guidance…..will need for example, conditions to be coded (eg ICD) relevant to values to be coded (LOINC etc.) How do we define services: expand on CRFQ pilot Define a `standard template` for service definition taking CRFQ as an example Bring CFRQ / IHE together in a specialized IHE profile (EC funded workstream) Review CRFQ RI + continue to expand UC catalogue around CRFQ usage context Implement CRFQ at a few sites Test CRFQ I/E on existing data sources (EMR/EHR/EPR) Test CRFQ safety model in 2-3 different systems Apply CRFQ + idea to the Pharma Clinical Trial Databases Understanding available data Catalogue and sort by usages the available info sources; Develop a catalogue of databases (1) short term (2) medium term. Develop a catalogue of databases (built upon EHRs) that (1) are currently available for researchers to use – eg review safety submissions and publications to find the databases to include in version 1, then (2) it could be available, but have not so far been used outside their source institutions – will need a survey Using CDASH output, determine how much is available in EHRs at representative hospitals Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 Which types of services Pharma industry to make its product information dissemination computable Implementation of eCRF linked closely to the EHR Reporting systems for adverse events closely linked to EHR EHR to support EU patient registries for targeted therapeutic areas/diseases in real life settings and epidemiology studies etc. Implement clinical workflows at 3 test sites Pharma: use of EHR to conduct drug utilization review, post marketing surveillance and care gap analysis in real life settings Generation of reports of adverse events directly from EHR Access / submission of supplemental information regarding patients clinical care experience around an adverse event on demand as part of investigation of AE for expanded databases etc. Services related to drug identification Drug identification + Drug structured information A single drug dictionary globally Drug Lexicon / id Drugs enter drug dictionary at start of Phase 3 trials 5.3.2 Communication How do we communicate: setting up strategy Declaration of Helsinki: Citizens OR Data Subjects Define the strategy: Target stakeholders, Messages to be passed, Catalogue of channels, Goals of the strategy, funding model What do we communicate Use case studies + success stories to lobby key stakeholders + identify the stakeholder`s decision makers Position EHR as a tool to facilitate optimal disease management, to insure patient safety and to maximize health outcomes Regulators, Patients, and Pharma to accept the notion of risk Minimum requirements for Privacy Enhancing Technologies Encourage patients understanding and involvement by use of `healthspaces` Introduce specified medical research use of clinical care data to healthcare IT community, the software vendors ans system integrators How do we communicate: communication plan (stakeholders, media, timelines, ..) Make sure that EFPIA taskforce outcomes are circulated among Member State Governance bodies by mid 2008 Use the `patient – centered` EHR model to engage Pharma Engage patients as stakeholders in a revision of Helsinki requirements Weekly / monthly `news monitors` email to build awareness of incremental steps being made Pharma / Healthcare org JOINT communiqués on data sharing Communication to patients: integrate to eHealth Initiatve Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 5.3.3 Third Party Business models Implement service delivery platforms (SDP) as FMVK able to deliver billable services (secondary use) Pharmacists are missing Draft binding set of principles and guidelines that are supportive of R&D that regulate the (1) access to patient / claims data (need for protocols, objectives and methods review, approval,..) and (2) publishing of results (need for methods and statistical review, approvals,…) Business entity that can establish business model, write business plans, and raise money to develop and deliver services for multiple use of electronic health records (see them as product offerings that might be developed over time) Document business case from perspective of all stakeholders At the European level should be : driven by Healtcare Authorities, with scientific board from Academia, and built by IT vendors, using standards : IHE and CDISC, HL7,.. Business Place Pharma, IT Vendors, Governance, Providers, as a template / funded research project Setting up the Third Party Survey / Inventory across Europe: available / under development, business model , financing Accept that there will not be a EURO-EHR common definition for at a minimum 5 years ……so federate There are many potential third parties each with different roles eg `secure data repositories`, facilitators, providers of shared IT eg processing power. We need to understand who they are and their role Type of services Promote catalogue of data Stimulate and catalogue GPRD – like initiatives ans list their mandate constraints vis-à-vis research work Set / common EHR platform of interest for the pharma industry with patient access focus (EHR to shorter R&D time, facilitate preparation of valuee propositions to payers and increase patient access. Build / Assemble cross-organisation CRFQ test data sets Joined research from different databases 5.3.4 Common Discussion Forum Scope and objective – mission statement Defining conditions for making it possible the access of EHR to various stakeholders Define terms of relevance, include a fixed term, mandate deliverables, ask CEN to champion Purpose of the Discussion Forum is to provide a place where all stakeholders can be invited (from across Europe) to shave information on initiatives and to identify areas where collaboration will lead to mutual benefits. Next step: identity and approach `umbrella ` group where this forum would belong. Decide upon ONE framework as the official` EHR related one ie enhance it with Clinical LLSE. Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 Unique EHR with primary care and hospital data in every country of the European Union (political decision) Forum/framework/governance: Organisational entity of recognized leaders that will develop executable strategic plan and build trust in one another Build new group to increase efficiency Common discussion : overall it needs governance , it needs to be a place where all stakeholders can contribute , it might include a number of for a to drill into the details Assemble a multi-disciplinary team and produce RI of scope / vision document and governance documents Governance of the uses of the data – each protocol , an ABSOLUTE Candidate groups IHE is excellent framework with good involvement of all actors (users, IT vendors,…) of EUROPEAN countries. Create a SPECIFIC DOMAIN dedicated to CLINICAL RESEARCH (to define the needs and workflows) Peer Review process among Database providers internationally CDISC eSDI IT vendors Information + Use existing patient associations to inform about secondary use. EUROREC – pharma not present/active yet How to do Involve EHR vendors, make them aware of Research Requirements Develop EHR applications (tailored to address top priorities / stakeholders) using a patientcentered model as common discussion framework. Work with IT industry to agree the common core data elements / standards to be included in applications 5.3.5 Roadmap Group 1 (short term) - 2008 CRFQ pilot Agreed project definition, catalogue of available resources, strategy for further funding, success criteria: CRFQ Proof of concept complete, Communications strategy implemented, Positive feedback Communication `news monitor` Develop a catalogue of databases, built from EHRs, that are currently available across Europe for researchers – both within the source institutions and beyond – to access and use. Euro-EHR data compendium adopting UK example Develop strategic place Capture case studies + best practices + develop 1st draft guidance Have at least one large scale Academia – Hospital – IT industry – Pharma project topic defined within the IMI call process AER on existing EHRs Primary and secondary use of EHR: Enhancing clinical research Brussels 11th and 12th October 2007 Some practical , pragmatic, reachable milestones with direct benefit in EHR Group 2 (mid term) – 2009 I/E CRFQ implemented on existing EHRs (Cancer) o CRFQ operational in 3 sides o CRFQ as DSTU in Q1 2008 + OMG RFP in Q2 2008 o One service in pilot , is the basis of learnings needed to build roadmap Collaboration Forum in place o Organisation / framework for decision making in place o Charter agreement of common discussion forum o Definition of an IHE Technical Framework for clinical research (to be able to test something at the 2009 or 2010 Connecthatlon Go / no go understanding of need and value of third party o Mobilize Pharma industry to identify / launch a common EHR platform (summit) o Third party business case assessed + deliverables of Discussion Forum achieved o Public template for workflows within study protocols Pilot of first service Group 3 (long term) CRFQ as standard connectors Run a pilot study on a fully integrated EHR across boarders Assess need for a follow-up project European free official database of drugs, usage, important adverse events, brandname in each country, unique ID etc. Publish answer to the question `how much data is available in EHRs that can be used directly in clinical trials` The Connectathlon: test the first integration profile dedicated to clinical research `patient recruitment`or including a CRF in EHR` Executing Entity in place capturing and aggregating supplemental medical record information of selected AEs