Gouty Hands
advertisement
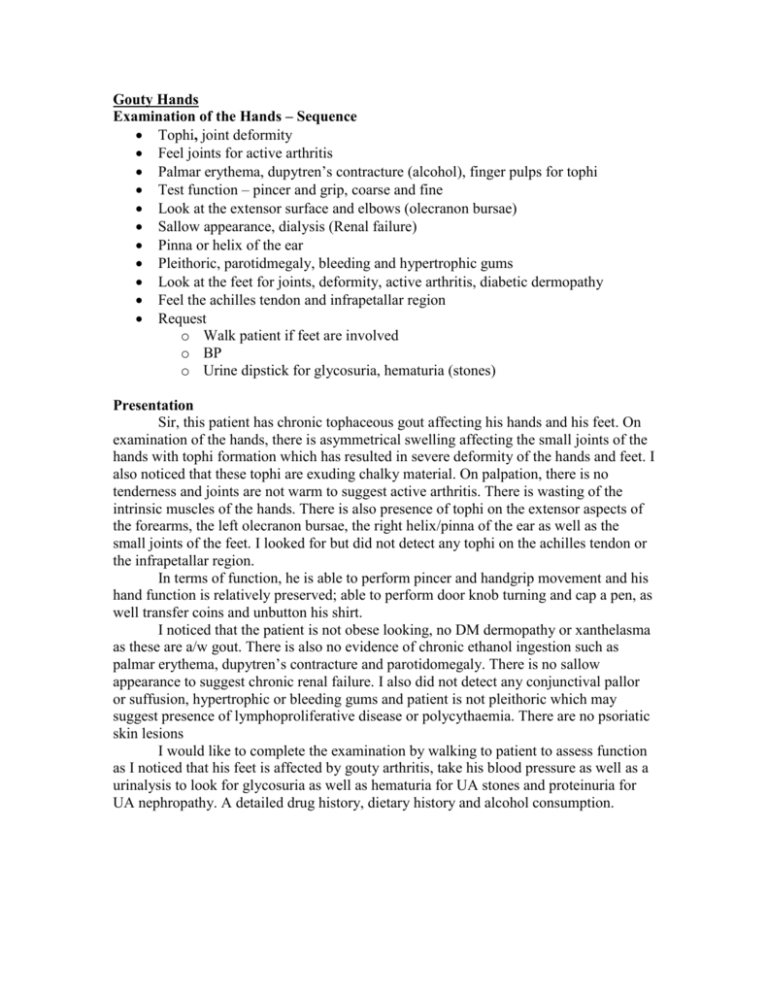
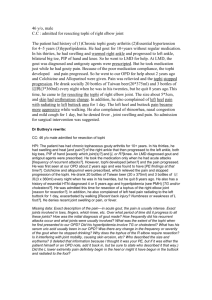
Gouty Hands Examination of the Hands – Sequence Tophi, joint deformity Feel joints for active arthritis Palmar erythema, dupytren’s contracture (alcohol), finger pulps for tophi Test function – pincer and grip, coarse and fine Look at the extensor surface and elbows (olecranon bursae) Sallow appearance, dialysis (Renal failure) Pinna or helix of the ear Pleithoric, parotidmegaly, bleeding and hypertrophic gums Look at the feet for joints, deformity, active arthritis, diabetic dermopathy Feel the achilles tendon and infrapetallar region Request o Walk patient if feet are involved o BP o Urine dipstick for glycosuria, hematuria (stones) Presentation Sir, this patient has chronic tophaceous gout affecting his hands and his feet. On examination of the hands, there is asymmetrical swelling affecting the small joints of the hands with tophi formation which has resulted in severe deformity of the hands and feet. I also noticed that these tophi are exuding chalky material. On palpation, there is no tenderness and joints are not warm to suggest active arthritis. There is wasting of the intrinsic muscles of the hands. There is also presence of tophi on the extensor aspects of the forearms, the left olecranon bursae, the right helix/pinna of the ear as well as the small joints of the feet. I looked for but did not detect any tophi on the achilles tendon or the infrapetallar region. In terms of function, he is able to perform pincer and handgrip movement and his hand function is relatively preserved; able to perform door knob turning and cap a pen, as well transfer coins and unbutton his shirt. I noticed that the patient is not obese looking, no DM dermopathy or xanthelasma as these are a/w gout. There is also no evidence of chronic ethanol ingestion such as palmar erythema, dupytren’s contracture and parotidomegaly. There is no sallow appearance to suggest chronic renal failure. I also did not detect any conjunctival pallor or suffusion, hypertrophic or bleeding gums and patient is not pleithoric which may suggest presence of lymphoproliferative disease or polycythaemia. There are no psoriatic skin lesions I would like to complete the examination by walking to patient to assess function as I noticed that his feet is affected by gouty arthritis, take his blood pressure as well as a urinalysis to look for glycosuria as well as hematuria for UA stones and proteinuria for UA nephropathy. A detailed drug history, dietary history and alcohol consumption. Questions What is gout? Gout is a disorder of purine metabolism, resulting in hyperuricaemia either from overproduction(75%) or undersecretion of uric acid, resulting in deposition of urate crystals in the joints or bursae. Patients typically present with acute monoarthritis of the first MTPJ, with pain swelling and exquisite tenderness which peaks within hours and lasts for days. It affects the joints of the lower limbs initially in the majority of patients which includes the MTPJ, ankles and knees. It can also subsequently affects the joints of the upper limb. What are the stages of gout? Acute gouty arthritis Intercritical period Chronic tophaceous gout What does tophi indicate? Severe, recurrent and chronic gout. Where are the commonly areas to look for gouty tophi? Hands, extensor aspect of the forearms, olecranon bursae Helix if the ears Toes, Achilles tendons, infrapetaller regions What are the clinical manifestations of gout? Asymptomatic hyperuricaemia Acute arthritis Chronic, recurrent arthritis Tophaceous gout Uric acid nephrolithiasis Uric acid nephropathy What are the triggering factors of gout? Alcohol ingestion Foods – sweetbreads, liver, kidneys and sardines Drugs – Thiazide diuretics, aspirin, cyclosporine, pyrazinamide and ethambutol Dehydration and fasting Surgery, Trauma What are the causes of gout? Primary – associated with obesity, diabetes mellitus, hypertension and high TGs Secondary Drugs Chronic ethanol ingestion Chronic renal failure Polycythaemia, lymphoproliferative, myeloproliferative Psoriasis How would you investigate? Definitive investigation would be aspiration of the involved joint, looking for intracellular deposition of needle-shaped crystals that is negatively birefringent under polarised light, within leukocytes. They react with nitric acid and NH4OH to give a purple color (Murexide test) Blood Ix – Uric acid levels which may be normal during an acute attack X-ray of the joints may show erosive arthropathy from tophi with overhanging edges associated with punctuate to diffuse calcification. How would you manage? Education and counselling, including dietary advice and avoidance of alcohol PT/OT if tophaceous gout for preservation of function Manage associated hypertension and diabetes mellitus Medications – acute attack and prophylaxis Surgery – rarely for cosmetic reasons, arthroplasty How would you treat an acute attack? NSAIDS – Indomethacin (50mg tds) Colchicine 2 ways: 0.5mg hrly till GI side effects or max of 5 mg, or 0.5mg tds Intrarticular steroids (triamcinolone 20mg) Systemic steroids (Prednisolone 30mg OM and tails over 7-10 days) How would you prophylax against gouty attacks? Prophylactic agents used are iniated under colchicine cover which includes: Xanthine oxidase inhibitor Allopurinol New agents – Uricase, febuxostat Uricosuric acid agents probenecid or sulfinpyrazone losartan fenofibrate What are the indications for allopurinol? Recurrent gouty attacks > 3 times a year Chronic tophaceous gout Uric acid nephropathy Persistently high uric acid level Conditions that may predispose an individual to gouty attacks, prior to chemotherapy or radiotherapy which may induce tumor lysis What are the side effects of allopurinol? Side effects occur in 3-5% Rash, diarrhea, drug fever Leucopenia, thrombocytopenia Allopurinol hypersensitivity syndrome Erythematous rash, fever, hepatitis, hypereosinophilia and renal failure What are the other crystal arthropathy that you know about? Pseudogout – Acute arthritis resulting from deposition of calcium pyrophosphate dihydrate crystals in the joints which are rhomboid shaped positively birefringent crystals under polarised light. Calcium hydroxyapatite crystals deposition in the large joints such as knees and shoulders, affecting the elderly. What are the differential diagnoses? Septic arthritis Overlying cellulitis Trauma What is your differential diagnosis for chronic tophaceous gout? Florid tendon xanthomata Yellow and not chalky Adherent to tendon and not joint Does not involve the bursae, ie no olecranon or pinna lesions No active arthritis