Indirect Calorimetry - CriticalCareMedicine
advertisement
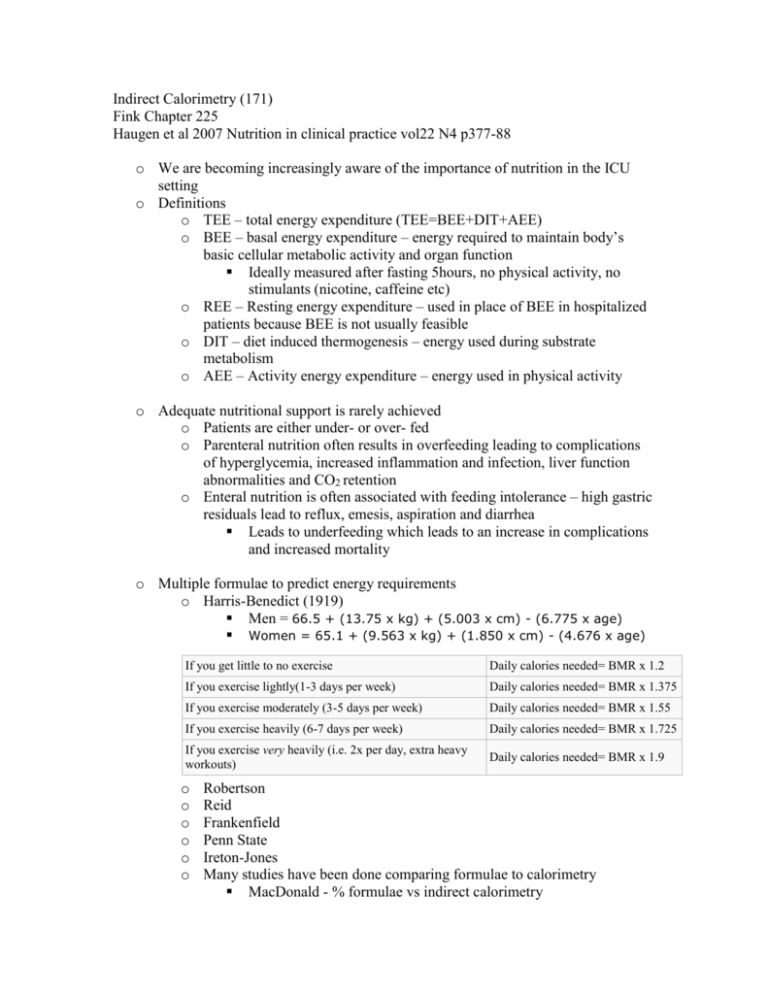
Indirect Calorimetry (171) Fink Chapter 225 Haugen et al 2007 Nutrition in clinical practice vol22 N4 p377-88 o We are becoming increasingly aware of the importance of nutrition in the ICU setting o Definitions o TEE – total energy expenditure (TEE=BEE+DIT+AEE) o BEE – basal energy expenditure – energy required to maintain body’s basic cellular metabolic activity and organ function Ideally measured after fasting 5hours, no physical activity, no stimulants (nicotine, caffeine etc) o REE – Resting energy expenditure – used in place of BEE in hospitalized patients because BEE is not usually feasible o DIT – diet induced thermogenesis – energy used during substrate metabolism o AEE – Activity energy expenditure – energy used in physical activity o Adequate nutritional support is rarely achieved o Patients are either under- or over- fed o Parenteral nutrition often results in overfeeding leading to complications of hyperglycemia, increased inflammation and infection, liver function abnormalities and CO2 retention o Enteral nutrition is often associated with feeding intolerance – high gastric residuals lead to reflux, emesis, aspiration and diarrhea Leads to underfeeding which leads to an increase in complications and increased mortality o Multiple formulae to predict energy requirements o Harris-Benedict (1919) Men = 66.5 + (13.75 x kg) + (5.003 x cm) - (6.775 x age) Women = 65.1 + (9.563 x kg) + (1.850 x cm) - (4.676 x age) If you get little to no exercise Daily calories needed= BMR x 1.2 oIf you O exercise lightly(1-3 days per week) Daily calories needed= BMR x 1.375 w If you exercise moderately (3-5 days per week) Daily calories needed= BMR x 1.55 e If you exercise heavily (6-7 days per week) Daily calories needed= BMR x 1.725 n oIf you R exercise very heavily (i.e. 2x per day, extra heavy Daily calories needed= BMR x 1.9 workouts) o o Robertson o Reid o Frankenfield o Penn State o Ireton-Jones o Many studies have been done comparing formulae to calorimetry MacDonald - % formulae vs indirect calorimetry No formula was good for all BMIs in all conditions o Calorimetry o Measurement of heat produced to quantify TEE o Total body heat is measured in a thermally sealed chamber o Very accurate but cumbersome, expensive and requires technical expertise o Indirect Calorimetry o Used in place of direct calorimetry o Energy expenditure is quantified under specific conditions by measuring respiratory gases (O2 consumed and CO2 produced) These numbers are then inserted into the Weir equation o o o Energy Expenditure (kcal/day) = [(VO2 X 3.941) + (VCO2 X 1.11) + (uN2 X 2.17)] X 1440 The urinary Nitrogen (uN2) factor is usually excluded because it accounts for <4% of the true energy expenditure Can also be done using the Fick equation by comparing the A-V O2 contents and using cardiac output Period of measurement 24 hours is the old standard Recent evidence suggests that 30 minutes is almost as accurate One trial demonstrated that 5 minute measurements were as good as 30 minutes – but the patients had to be stable One measurement or many There is a great deal of day to day variation in energy expenditure (may be as great as 35%) Day to day measurements affected by temperature but not by illness severity score Daily measurements may be necessary Value of energy balance o Negative energy balance is associated with Longer duration of mechanical ventilation Longer ICU stay Development of pressure sores Renal failure Sepsis Hemodynamic instability *it may be that the sicker patients don’t get fed rather than not being fed makes them sicker Energy balance of -10, 000kcal associated with increased mortality o Respiratory Quotient (RQ) o Ratio between VCO2 and VO2 (VCO2/VO2) o If glucose is completely oxidized in a system the quotient is 1 o Lipid = 0.69, Protein = 0.81 o If a value for RQ is found to be outside the “normal” range (0.67-1.2) then the measurement is likely inaccurate o Poor measurement occurs when Poor seal with air leak Hemodialysis Patient agitation or pain Residual anesthetic gasses FiO2 >60% o Limitations of IC o VCO2 and VO2 are calculated using volumes of inspired and expired volumes (Ve) but Inspired volumes (Vi) are difficult to accurately measure so they are estimated using the Haldane transformation which assumes static volumes of N2 in inspired and exhaled gasses Vi = [(FeN2/FiN2) Ve] o Types of machines o Douglas Bag GOLD STANDARD Person breathes ambient air through a 1-way valve connected to an airtight container (Douglas bag) Expired gas is sampled; relative concentrations of O2 and CO2 are measured by electronic gas analyzers Comparison is made between the composition of inspired and expired air: VO2 and VCO2 are determined Challenges: expensive analyzer equipment, requires technical expertise o Metabolic Cart (this is what we use) Person breathes into mask or through mouthpiece connected to metabolic cart Gas analyzers and airflow measurement Mixing chamber: gas samples are continuously obtained and analyzed from a mixing chamber within the metabolic cart Breath-by-breath: analysis from an external sample port on a breathing valve In some instances, the metabolic cart has been designed to collect a gas sample using either mixing chamber or breath-by-breath procedure Accurate and well-accepted in clinical settings Challenges: costly and requires technical expertise to maintain o Special considerations o Extreme obesity – (BMI>40) It is very difficult to estimate energy expenditure in these patients and IC may be the onlt useful method o Post op bariatric surgery Energy expenditure may change very rapidly with changing gbody composistion o HIV infected patients Hypermetabolism may play a role in wasting associated with the disease Difficult to estimate using formulae o IHD Hemodialysis removes CO2 from the venous bed and therefore changes the FeCO2 and it may take 24 hours to reequilibrate - as such wait 24 hours after hemo run o CRRT Similar problem removes CO2 but not O2 can lose up to 35% of CO2 In addition the temperature of the patient may decrease on CRRT No good guidelines for the interpretation of IC in these situations o Deep sedation/paralysis Significantly reduce energy expenditure IC should be performed during and post deep sedation