BHS 116.2- Phyisology II Date: 1/16/13 Notetaker: Stephanie Cullen
advertisement

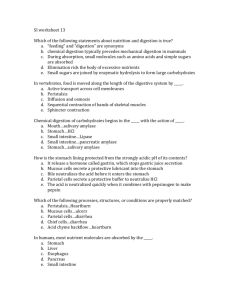
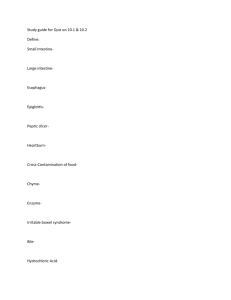
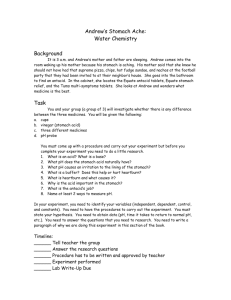
BHS 116.2- Phyisology II Notetaker: Stephanie Cullen Date: 1/16/13 Page: 1 Objective: Describe the functions of the stomach. Function of the Stomach - Storage of large quantities of food until they can be processed by the intestines o MAIN FUNCTION o Not digestion! - When food enters the stomach, a vago-vagal reflex reduces the tone of the muscular stomach wall o Efferent and afferent vagal fibers that trigger relaxation so the stomach can accept the food o Receptive relaxation o Max volume: 1-1.5 L Motor Function of the Stomach - Mixing the food w/ gastric secretions until it forms chyme o Need to break it down to an extent until it is liquid - When the stomach contains food, slow waves initiate weak peristaltic constrictor waves “mixing waves” - As these waves progress from the body of the stomach towards the antrum, they become more intense, providing powerful action potential-driven constrictor rings mixing the stomach content and pushing it toward the pyloric sphincter (separates the stomach from the SI) o Upper part: fundus o Bulk: body o Last part w/ thicker muscular layer: antrum - At the pyloric sphincter, most of the chyme is propelled back into the mixing waves since it is closed (tonically constricted) o Food is pushed up then washed back to get the mixing - Emptying of the stomach is promoted by strong peristaltic contractions in the stomach antrum toward the pyloric sphincter o Only a small amount leaks out into the small intestine each time Once it gets into a liquid state o Allows for a slow emptying of chyme into the small intestine at an appropriate rate for digestion and absorption Allows that little bit to be processed and assimilated before the next batch comes through Wouldn’t be able to absorb a good portion of the nutrients w/o this process - The pyloric pump o Contractions 6x stronger in the anturm than mixing contractions o Forces several (5-10) ml of chyme through pyloric sphincter into duodenum VIDEO Objective: Describe the regulation of stomach emptying (stomach, duodenal, and nervous factors). Regulation of Stomach Emptying - Primary factor stimulating stomach emptying o Increased food volume As the food volume increases, the need to empty the stomach increases BHS 116.2- Phyisology II Notetaker: Stephanie Cullen o - - - - - Date: 1/16/13 Page: 2 Other factors Fluidity of the chyme is also an influence More liquefied chyme = easier to empty the stomach contents Hormonal control: The antral mucosal cells of the stomach secrete gastrin which enhances the activity of the pyloric pump Increases strength of pyloric/antral contractions Primary factor inhibiting stomach emptying o Food entering the duodenum Triggers multiple nervous reflexes to trigger inhibition of movement of more food Enteric nervous system (short): Enterogastric Reflex o Entero = small intestine o Gastric = stomach o Reflex from the small intestine to the stomach to inhibit stomach motility Sympathetic nervous system (long) o Starts w/ afferent in the SI o Goes to sympathetic chain o Goes to stomach Main duodenal factors are fat (most important), acid (pH), hypertonicity (salt), and distension (stretching of the duodenum) o As fats enter the duodenum, they bind receptors on the epithelial cells o In turn, the epithelial cells secrete hormones into the blood which travel to the stomach Inhibit the pyloric pump Strengthen the pyloric sphincter Cholecystokinin (CCK) o Secreted by the mucosa of the duodenum and jejunum in response to FAs in the chyme o Blocks the effects of gastrin on stomach motility Inhibits gastric motility Secretin o Secreted by the mucosa of the duodenum in response to gastric acid release from the stomach o Inhibits gastric motility Gastric inhibitory peptide (GIP) o Secreted from the upper small intestine primarily in response to FAs in the chyme o Stimulates insulin secretion Primary effect o Can inhibit gastric motility: More prominent function if the other hormones fail W/in the stomach: volume of chyme is more important Once chyme enters the SI, geared toward inhibiting gastric motility BHS 116.2- Phyisology II Notetaker: Stephanie Cullen Date: 1/16/13 Page: 3 Objective: Describe movements through the SI and colon and the various controls (hormones and reflexes). Movements of the Small Intestine - Mixing contractions (segmentation contractions) o When chyme distends the small intestine, the wall is stretched Elicits concentric contractions spaced at intervals lasting a fraction of a minute Mix w/ enzymes to breakdown contents of chyme into nutrients o Divide intestine into a “chain of sausages” Max frequency of these contractions is determined by the frequency of the slow waves o Help propel chyme through the small intestine To a smaller degree since the main function is mixing Net movement of chyme is very slow (1cm/min) o Usually takes 3-5 hours for chyme to reach the ileocecal valve (junction of the small intestine and large intestine) which is through the entire SI - Propulsive contractions o Chyme is primarily propelled through the small intestine by peristaltic waves Migrating motility complex (occurs between meals) After stomach has processed chyme and it has been released into SI These waves can occur anywhere in the SI Weak and usually die out in 3-5 cm Pushes food a little further Get contractions for a little while then its pushed along again by another migrating motility complex - Peristalsis is greatly increased after a meal due to neuronal and hormonal control o Gastroenteric reflex is responsible for this effect Initiated by distension of stomach and triggers the SI Speeds along food into the SI because more food has just entered the stomach Conducted primarily by myenteric plexus of the enteric nervous system o Hormonal control Gastrin, CCK, insulin, and serotonin all enhance SI motility Gastrin = stomach hormone to move food into SI CCK = released when fat enters duodenum to further trigger movement Insulin = stimulates motility of SI b/c the faster its moving, the less being absorbed into the blood o Know there is enough glucose in the blood when insulin is present o Insulin wants to move the food along so no more is absorbed Secretin and glucagon inhibit SI motility Secretin = released in response to acid o Need to neutralize the acid (using HCO3-) as to not damage the epithelium of the GI tract w/ the low pH chyme Glucagon = released w/ low blood sugar o Slows down movement to absorb more glucose into the blood BHS 116.2- Phyisology II Notetaker: Stephanie Cullen Date: 1/16/13 Page: 4 Ileocecal Junction - Ileocecal valve o Primarily prevents backflow of fecal content from colon into SI - Ileocecal sphincter o Remains mildly constricted o Constriction is regulated by the pressure in the cecum o Slows the emptying of the SI into the cecum Movements of the Colon - Normally very sluggish because the functions of the colon (absorption and storage) do not require intense movements o Does a lot of the absorption of water in the chyme - Mixing movements are similar to segmented movement of SI but are more powerful o Can sometimes constrict colon to occlusion o Causes unstimulated portion of the muscle to bulge out (haustrations) o Provide a minor amount of movement o Responsible for much of the movement in the cecum and ascending colon Takes 8-15 hours to get through this section of colon - Propulsive movements (mass movements) o Responsible for movement beginning w/ the transverse colon (and in descending colon) o Occur only 1-3 x per day Many times after a meal - Mass movement o Modified form of peristalsis o Constriction of rings in response to a distended colon that move along the colon o Constriction for 30 sec followed by relaxation of 2-3 min then another very strong constriction o Whole series of mass movements may occur for 10-30 min and then may stop for half a day o Initiation after meals is facilitated by gastrocolic and duodenocolic reflexes Results from distension of the stomach and duodenum Triggers movement from the stomach to large intestine or small intestine to large intestine Initiated by the autonomic nervous system Shouldn’t feel it Involuntary o When they force material into the rectum, the desire for defecation is felt Voluntary o When it becomes convenient for defecation, a deep breath can elicit the defecation reflex: Valsalva maneuver Builds up abdominal pressure Important role: Valsalva Retinopathy- Vision loss after asthma attack Caused by weight lifting (blood pressure is too high and retinal blood vessels can burst) BHS 116.2- Phyisology II Notetaker: Stephanie Cullen Date: 1/16/13 Page: 5 Objective: Describe the various secretions of the GI tract as well as their functions and regulation (salivary, esophageal, stomach). Secretion of Saliva - Saliva is produced by the parotid, submandibular, sublingual, and many buccal glands o Acini (cells): produces the serous and mucus parts of saliva o Duct: carries saliva to the mouth o Cells of the duct absorb Na and Cl from serous fluid causing saliva to be devoid of these Why we are sensitive to the taste of salt - Serous (watery) secretion containing ptyalin (α-amylase, salivary amylase) that breakdown starch and lysozyme that breaks down bacterial cell walls - Mucus (sticky) secretion containing mucin for lubricating and protection - pH between 6-7 (neutral) - 0.5 ml/min is secreted during waking hours o Produce 1 L of saliva/day o All secretions from the GI tract: 7 L/day Most are reabsorbed so not losing that fluid Function of Saliva in Oral Hygiene - Wash bacteria away from teeth to prevent cavities - Wash food stuff away from teeth - Begin to digest food (polysaccharids like starch) o Amylase - Destroy bacteria w/ proteolytic enzymes o Lysozyme - Destroy bacteria w/ antibodies o IgA o Also helps to destroy bacteria in the food or in the mouth Regulation of Salivation - Salivation is controlled mainly by parasympathetic signals from the salivatory nuclei in the brain stem that are stimulated by both taste and touch o Physical pressure of food on the tongue stimulates salivation - The appetite area of the central nervous system (anterior hypothalamus) can stimulate salivation in response to the smell or taste of a favorite food - Reflexes from the stomach and intestines can stimulate salivation (long reflex) Esophageal Secretion - Mucus glands secrete mucus that acts to lubricate and protect the epithelial walls o Lubrication eases the movement of the bolus of food into the stomach Gastric Secretion - Surface mucus cells (epithelia) along the entire lining o Alkaline mucus secretion o Protects against digestive enzymes and acid that damage of the epithelium BHS 116.2- Phyisology II Notetaker: Stephanie Cullen - - - Date: 1/16/13 Page: 6 Gastric glands located in the body and fundus of the stomach secrete: o Pepsinogen (chief and mucous cells) Inactive form Breaks down proteins o Hydrochloric acid (parietal cells) o Intrinsic factor (parietal cells) Important for the absorption of vitamin B12 in the intestine into the bloodstream Pernicious anemia results from lack of vitamin B12 o Mucus (mucous neck cells) Have to protect the gland o Histamine (ECL (enterochromaffin) cells) Both endocrine and paracrine function Acts distally and locally on its neighboring cells Pyloric glands located in the antrum of the stomach secrete: o Pepsinogen (chief cells) o Mucus (mucous neck cells) o Gastrin (G cells) o Somatostatin (D cells) Pancreas, hypothalamus (GHIH), and now stomach Stimulated by acid Inhibits the actions by the G cells (parietal, chief cells) Pepsinogen is converted to the active proteolytic enzyme (pepsin) in the presence of acid (HCl) and other pepsin proteins o Pepsin is a protease that breaks down proteins o Pepsin can further convert other pepsinogen molecules into pepsin Regulation of Gastric Secretion - Gastrin (hormonal) o Released from G cells in response to protein in the stomach o Stimulates chief cells to secrete pepsinogen o Stimulates parietal cells to secrete HCl HCl helps convert pepsinogen into pepsin and prevent bacterial infection due to the low pH o Stimulates enterchromaffin cells to secrete histamine Histamine stimulates parietal cells to secrete more HCl (paracrine function of histamine) - Acetylcholine (nervous) o Released from vagal nerve endings o Stimulates chief cells to secrete pepsinogen o Stimulates enterochromaffin cells to secrete histamine Histamine stimulates parietal cells to secrete HCl o Stimulates G cells to secrete gastrin Stimulates chief cells to secrete pepsinogen Stimulates parietal cells to secrete HCl o Overactive vagus stimulation in the stomach produces excess HCl and pepsin Ulcers occur when tissues and cells in the stomach are broken down when there is no food in the stomach - Acid in the stomach and ACh released from vagus nerves cause the release of pepsinogen - Feedback inhibition of both HCl and pepsinogen secretion by excessive acidity that prevents the stomach pH from getting too low (< 3) BHS 116.2- Phyisology II Notetaker: Stephanie Cullen Date: 1/16/13 Page: 7 Objective: Describe the phases of gastric secretion. Phases of Gastric Secretion - Cephalic phase o Occurs before food enters the stomach o Due to sight, smell, thought, and taste o Neurogenic signals from the cerebral cortex and the appetite center transmit through the vagus nerves (via ACh) resulting in production of 20-30% of the gastric juices secreted during a meal - Gastric phase o Occurs once food enters the stomach eliciting the secretion of 70% of the gastric juices secreted during a meal Due to both nervous reflexes (ACh) and the production of gastrin from the pyloric glands - Intestinal phase o Occurs as food enters the SI o Inhibits the production of gastrin and the production of the remaining gastric juices CCK Clicker Question: Which is not a function of the stomach? a. Mixing b. Storage c. Digestion d. Absorption of nutrients - only aspirin and alcohol are absorbed in the stomach