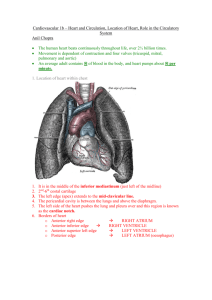
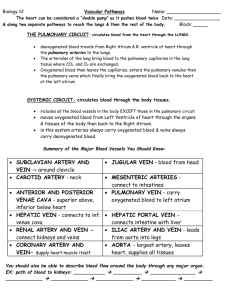
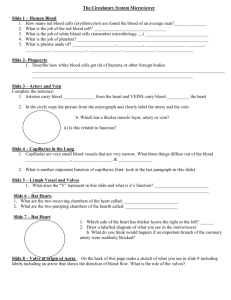
Anatomy – Exam 1 (Part 2)
advertisement

Anatomy – Exam 1 (Part 2) Thoracic Wall, Lungs and Pleura ○ Objectives Thoracic Wall Describe the boundaries and reference lines of the thoracic cavity and the skeletal components (thoracic cage) of the thoracic wall What are the functions and surface landmarks associated with the thoracic cage? Describe the anatomy and articulations of a typical rib Describe the process of respiration and the associated movements of the thoracic wall Describe the anatomy of the breast. What is the clinical significance of the lymphatic drainage in this region? Describe the muscles that make up the thoracic wall What nerves, arteries and veins supply the thoracic wall? Describe the arrangement of the intercostals nerve, artery and vein within the intercostals space Describe the major anatomical compartments within the thoracic cavity: pleural cavities and the mediastinum Lungs and Pleura What distinguishes parietal from visceral pleura? Describe the 4 regions of parietal pleura What is the pleural cavity. How does it relate to the thoracic cavity. What are the costodiaphragmatic and costomediastinal recesses of the pleural cavity? Describe pathologies associated with the pleural cavity including: pneumothorax, hemothorax, chylothorax, and pleuritis (pleurisy) Describe the surfaces, lobes, and fissures of the right and left lung Describe the anatomy associated with the root or hilum of the lung Describe the anatomy of the trachea and bronchi. Why are aspirated foreign objects found in the right lung? Be able to explain the concept of bronchopulmonary segments Describe the blood circulatory systems (pulmonary and bronchial) associated with the lungs Describe the autonomic innervation of the lungs Describe the lymphatic drainage of the lungs Be able to relate the borders, lobes, fissures and sounds of the lungs as well as the pleural recesses to the surface anatomy of the thorax ○ Functions of Thoracic Cage Ventilation part of respiration Protects viscera Provides anchoring points for skeletal muscles ○ Structures Thorax – superior portion of the trunk Jugular notch – in between the sternocleidomastoid muscles Sternal angle (of the manubriosternal joint) – landmark for 2nd rib which is basically the first one you can palpate Costal margin – made of cartilage Midclavicular line – inside nipple Intercostal space – takes the number of the rib above it Note – diaphragm comes up into the thorax a good bit ○ Skeletal Components Sternum Manubrium – top part; body; xyphoid process Ribs – 12 pairs True Ribs – ribs 1-7, line up with thoracic vertebrae False Ribs – ribs 8-10, because they share a common costal cartilage to attach to sternum ○ Note – 7th rib is a little funny Floating Ribs – ribs 11-12, don’t attach to sternum Costal Cartilages – links ribs 1-10 with body of sternum Superior thoracic aperture (thoracic inlet) – bordered by T1 vert, medial 1st rib and manubrium Not bordered by clavicle Inferior thoracic apterture (thoracic outlet) – bordered by T12, 11th & 12th ribs, costal margin, xyphosternal juncture Where diaphragm attaches Ribs Neck, Head, Shaft Articular Tubercule – where rib articulates with transverse process Nonarticular Tubercule – provides attachment for back muscles Costal Angle – on posterior side where rib starts to bend Superior & Inferior Facets – where ribs form joints with vertebrae Crest of head – in between facets, where rib binds with IV disc Costal Groove – goes along entire rib, where the vein, artery and nerve run ○ Joints Costovertebral – rib connects to inferior facet of same number and superior facet of lower # vert Costotransverse – rib connects to TP of same number Costochondral – transition from bone to cartilage on anterior side near sternum Sternocostal – joint between cartilage and sternum, is a synovial joint ○ Thoracic Cage and Ventilation Ventilation – movement of air Inspiration – requires ↑ in volume of thoracic cavity, creating a ↓ in air pressure in lungs Quiet Inspiration – diaphragm contracts → lowers diaphragm → increase in vertical dimension of thoracic cavity Active Inspiration – other respiratory muscles contract → elevate ribs → ↑ transverse and anterior/posterior dimensions of thoracic cavity Pump Handle Movement – ribs and sternum rotate up to change depth, changes anterior/posterior Bucket Handle Movement – ribs pivot to change width of thorax, changes transverse axis Quiet Expiration – passive, powered by recoil of elastic fibers in lungs Emphasema destroys this Active Expiration – abdominal muscles contract ○ Thoracic Wall Skin Breast – hemispheric mass of subcutaneous tissue containing mammary gland & overlying skin ○ Nipple – skin elevation containing smooth muscle and opening of lactiferous glands ○ Areola – pigmented skin surrounding the nipple, rich in sebaceous glands (gives newborns a bigger target) Subcutaneous Tissue Breast made out of adipose tissue, fat is the major component Mammary Glands – contains compound alveolar glands connected by lactiferous ducts to the surface ○ Lactiferous Sinuses – dilated portions of ducts which hold some milk ○ Suspensory Ligaments – maintain shape and attach to dermis of skin (not the pec) ○ Retromammary space – space between skin and pec Innervation – 4th – 6th intercostal nerves Arteries - Tributaries of Internal Thoracic Artery (medial), Pectoral branch of Thoracoacromial Artery (superior portion), Lateral Thoracic Artery (lateral), Posterior Intercostal Artery (lateral, posterior?) Veins – Axillary vein & Internal Thoracic vein Lymphatic Drainage Axillary process/Axillary tail – extension of the breast toward the axilla, is a passageway for lymph ○ Most of the lymph drainage from breast goes through here Small portion comes from Clavicular (drains superiorly), Sternal (drains medially), Phrenic (associated with diaphragm) Muscles Peripheral Muscles – can be used for active inspiration (pec major, serratus ant., serratus post. sup) Intercostal Muscles – used for active respiration ○ External Intercostal Muscle – elevates ribs during active inspiration Membranous anteriorly Fibers angled down toward midline (as if you were putting your hands in your pocket) ○ Internal Intercostal Muscle – interosseous part depresses the ribs, interchondral part elevates the ribs Membranous posteriorly Fibers angled down and away from the midline ○ Innermost Intercostal Muscle – same as internal, but separated from it by the neurovascular bundle in costal groove (really only on the lateral aspect of thorax) Vein – drains into azygous system, internal thoracic vein Artery – posterior intercostal artery supplied by thoracic aorta, anterior intercostal artery supplied by internal thoracic Nerves – ventral rami of T1-T11, T12 = subcostal nerve. For dermatomes and myotomes? “VAN” – in that order from top to bottom Transverse Thoracic Muscle – on anterior inside of ribs, connects sternum to ribs ○ weakly depresses ribs Subcostal Muscles – on posterior inside of ribs, connects one rib to the rib two above it (skips one) ○ Depresses the ribs Endothoracic Fascia – loose CT inside the parietal pleura Parietal Pleura – innervated by intercostal nerve, thus if aggravated it causes a sharp pain Note – visceral pleura is innervated by sympathetic nerves and makes dull, unlocalized pain ○ Thoracic Cavity Has 3 compartments: 2 pulmonary cavities and 1 central mediastinum Pleura and Lungs Subdivisions of parietal pleura: costal, diaphragmatic, mediastinal, cervical (above 1st rib) ○ The cervical portion makes the cupola a dome shaped structure Visceral pleura – lines the lungs ○ Does not have sensory innervation Costodiaphragmatic recess – lung doesn’t fill entire pleural cavity and so this is the extra space ○ ‘Below lungs’ At ribs 6-8, 8-10, 10-12 (What does that mean?) Costomediastinal recess – medial to the lungs Note – these recesses are good places for pleural taps Hilum of Lungs – where parietal and visceral pleura meet at root of lung (bronch-) Root of Lung – bronchus with associated bronchial arteries and veins, pulmonary artery, pulmonary veins, lymph nodes and vessels, autonomic nerves ○ Primary bronchi identifiable because it is harder due to cartilage ○ Pulmonary arteries usually on cranial aspect and are big and muscley ○ Bronchial vessels are small ○ Pulmonary veins are thin and flexible, usually on caudal aspect ○ Lymph nodes are usually full of carbon and are black Pulmonary Ligament – a continuation of the hilum caudal to it, is just the pleura Right Lung Anatomy 3 Lobes, 2 Fissures – Superior, Horizontal fissure, Middle Lobe, Oblique Fissure, Inferior Lobe Horizontal fissure – follows 4th rib Oblique Fissure – associated with cartilage of rib 6 (huh?) Apex – extends above 1st rib in the cupola Base is concave because of diaphragm Has costal, mediastinal and diaphragmatic surfaces Left Lung Anatomy 2 Lobes, 1 Fissure - Superior Lobe, Oblique fissure, Inferior Lobe Note – superior lobe has the cardiac notch and the lingula of the superior lobe Also has groove for descending aorta Airways and Lower Respiratory Tract Trachea – ○ Carina – end of trachea where it splits into two bronchi, nerve endings trigger coughing If flat then it indicates enlarged lymph nodes Primary Bronchi (main) – right and left ○ The right primary bronchi is more vertical and larger in diameter than left so things usually end up here Secondary Bronchi (lobar) – one for each lobe Tertiary Bronchi (segmental) – 10 on each side ○ Bronchopulmonary Segments – segments of lung based on the fact that each is supplied by a separate bronchi and branch of pulmonary artery Pulmonary veins travel across segments however Pulmonary Circulation Right side of heart → pulmonary trunk → left and right pulmonary arteries (non-oxygenated blood) → bronchial arteries → bronchial veins → azygous vein (for right side) or accessory hemiazygos vein (for left side) Lymphatic Drainage Superficial - bronchopulmonary nodes → tracheobronchial nodes → bronchomediastinal trunk (tracheal) → right lymphatic duct or thoracic duct ○ OR Deep - pulmonary nodes → bronchopulmonary nodes → the above pathway Nerves Parasympathetic - vagus nerve → pulmonary plexus (which follows bronchi into lungs) ○ Efferet – bronchoconstrict, vasodilate, secretory ○ Afferent – cough reflex Sympathetic – paravertebral sympathetic ganglia → pulmonary plexus ○ Efferent – bronchoconstrict, vasodilate, inhibit secretions ○ Afferents – visceral pain (dull, hard to localize) Histology of the Respiratory System ○ Objectives Identify the anatomical components of the respiratory system Differentiate between the ventilation system, conducting and respiratory portions of the respiratory system. Be able to describe their components, morphology and functions Define the tissue layers and cell types found in the nasal cavity, pharynx, larynx, trachea, bronchi, bronchioles, and alveolar airways. Relate the structure to the function of each of the above organs Know how the epithelium of the larynx is adapted for voice production or altered by cigarette smoke Describe how the histology of the respiratory system is designed to meet functional requirements associated with gas exchange between the body and the atmosphere Explain the structure of the alveolarcapillary membrane Be able to describe the location and structure of ciliated cells, mucus producing cells, alveolar macrophages, type I and type II pneumocytes and how they relate to their individual functions in the respiratory system Identify the respiratory system cell types involved in and their functional relationship with carcinoid disease, asthma, respiratory distress syndrome, heart failure and emphysema ○ Primary Function – gas exchange between atmosphere and blood ○ Secondary Function – air conditioning, olfaction, phonation ○ Major Divisions of the Respiratory System Conducting Portion – all the secondary functions From nasal cavity to bronchioles Respiratory Portion – where gas exchange occurs From respiratory bronchioles to alveolar sacs ○ Generalized Respiratory Tissue Layers (from inside to out) Respiratory Mucosa Respiratory Epithelium – pseudostratified ciliated columnar epithelium (PCCE) with goblet cells ○ Cells contained in respiratory epithelium Basal Cells – stem cells for goblet, ciliated and brush cells, these do not reach surface Ciliated Columnar Cells – for the mucociliary escalator Goblet Cells – produce mucinogen and mucin Brush Cells – narrow columnar, microvilli cells, sensory Serous Cells – columnar, microvilli cells that secrete watery substance Small Granule Cells (DNES cells) – secrete hormones and biogenic amines ○ Carcinoid Disease – a pulmonary cancer not related to smoking, affects females 10:1 Causes cells to release a bunch of biogenic amines and results in carcinoid syndrome, flushing of skin, diarrhea, heart problems Lamina Propria – loose fibroelastic CT running longitudinally (perpendicular to cross section) ○ Contains lymphatic tissue ○ Smooth muscle cell layer – sometimes present Submucosa – contains mucus and seromucus glands Rich vascular supply, some lymph vessels Dense, irregular fibroelastic tissue (less elasticy) Periosteum/perichondrium Adventitia – attaches respiratory tract to adjacent structures Made of fibroelastic CT Contains hyaline cartilage rings ○ Anatomy of Respiratory System Conducting Portion External Nares – skin (keratinized epithelium) Vestibule – where you pick your nose, contains hairs ○ Keratinized stratified squamous epithelium, sweat and sebaceous glands Nasal Cavity, Paranasal sinuses & Nasopharynx ○ Tissue Outer Epithelium – Normal PCCE Lamina Propria – contains Swell bodies (large arterial plexi and venous sinuses) for cooling/warming air ○ Includes pharyngeal tonsils (adenoids) which are lymphoid tissues ○ Paranasal sinuses are connected to nasal cavity but aren’t really used ○ Nasal cavity contains bony protrusions that make air turbulent so that air is cleaned ○ Olfactory Epithelium – located on roof of nasal cavity Outer Epithelium - Pseudostratified columnar epithelium without goblet cells (not similar ciliated cells) ○ Contains specialized cells Olfactory Cells – bipolar, unmyelinated neurons with non-motile cilia Sustentacular Cells – insulate olfactory cells, have microvillus border and secretory granules Basal Cells – can develop into olfactory and sustentacular cells Brush Cells – sensory, synapse with CN V (trigeminal nerve) Lamina Propria – contains Bowman’s Glands which are cells that make serous (watery) secretion that continually washes the olfactory cilia Oral Pharynx and Laryngeal Pharynx – from soft palate to epiglottis ○ Outer Epithelium - stratified (non-keratinized) squamous epithelium Squamous because this is a place of high mechanical stress ○ Lamina Propria – normal Larynx ○ Outer Epithelium – normal PCCE except at vocal fold and epiglottis ○ Is a framework of hyaline and elastic cartilage ○ Epiglottis – anterior surface covered by stratified squamous epithelia Prevents food from going down and thus this surface must be strong ○ Vestibular Fold (False Vocal Fold) – no known function ○ Ventricle – invagination between false and real vocal cord ○ Vocal Fold – voice box Outer Epithelium - stratified (non-keratinized) squamous epithelia (makes sense) Lamina Propria – contains seromucus glands and a bunch of structures ○ Vocal Ligament – elastic structure that moves with phonation Seromucus glands absent here ○ Vocalis Muscle – muscle controls vocal ligament ○ Squamous Metaplasia (Smoker’s Cough) – when PCCE is turned into stratified squamous epithelia due to environmental factors like smoking Trachea ○ From larynx to carina ○ Mucosa – normal PCCE with lamina propria (including longitudinally oriented elastic fibers) ○ Submucosa – contains mucous and seromucous glands ○ Adventitia - Has C-Shaped hyaline cartilage rings ○ Trachealis Muscle – band of smooth muscle connecting the 2 free ends of the cartilage ring Bronchi ○ Primary Bronchi – two of them, histology basically identical to trachea ○ Secondary Bronchi (Lobar) – identifiable by the irregularly shaped cartilage plates Contains bands of smooth muscle between lamina propria and submucosa ○ Tertiary Bronchi (Segmental) – basically the same as secondary ○ Note – all bronchi have normal PCCE Bronchioles ○ Identifiable because they don’t have cartilage bands and don’t have glands ○ Outer Epithelia – simple columnar ciliated epithelium with ↓ing goblet cells and epithelium becomes thinner Clara Cells – non-cilliated columnar cells with microvilli that secrete glycoproteins to reduce surface tension and also degrade toxins ○ Lamina Propria - thick smooth muscle layer and elastic bands ○ Bronchial Asthma – triggered by allergies, results in hyperresponsive airways and bronchoconstriction Immediate phase – bronchospasm (cough, weeze) Late phase – inflammation, edema, airway remodeled Terminal Bronchioles - ciliated cuboidal cells without goblet cells, with Clara cells Beginning of Respiratory Portion Respiratory Bronchiole - cuboidal epithelium with Clara cells, interrupted by occasional alveolus Alveolar Ducts – linear airway terminating in alveolar sacs Alveolar Sacs – dead ends lined with alveoli, many alveoli branch off of an atrium Alveoli – functional unit of repiratory system (external repiration) ○ Alveolar pores – communications between alveoli which allow air pressure equalization between alveoli ○ Interalveolar Septum – contains lots of capillaries for gas exchange, made by reticular fibers, elastic fibers and basal lamina ○ Emphysema – overactive macrophages due to smoke etc. release proteases which degrade elastic fibers Causes problems getting air out of lungs and patients develop Barrel Chest ○ Types of Cells Type I Pneumocyte (alveolar cell) – where gas exchange occurs ○ simple squamous, very thin and surface area-y ○ Alveolar capillary membrane - basal lamina often fuse with adjacent capillaries Type II Pneumocyte (alveolar cell) – make surfactant and have microvilli ○ Cuboidal cells which can form both type I and type II cells ○ Surfactant – phospholipid-protein mixture that reduces surface tension ○ Premature babies don’t have these Alveolar Macrophage – find stuff to eat in alveoli then ride the mucociliary escalator to oropharynx ○ AKA Heart Failure Cells – because after heart attack characteristic things get in lungs and these cells proliferate to eat it Respiratory Membrane – where exchange of gas from alveoli to blood occurs ○ Gas has 4 Layers to cross Wall of Type I Pneumocytes Fused alveolar epithelial/capillary basement membrane Endothelial cell of capillary Mediastinum ○ Objectives Delineate the superior, anterior, middle, and posterior mediastinum. Describe the major structures associated with the four regions of the mediastinum. Identify the contents of the superior mediastinum and relationship to the heart and lungs. Identify the borders of the posterior mediastinum. List the major vessels that occupy the posterior mediastinum. Define the origin, course, and termination of the thoracic duct. Describe the path of the esophagus and trachea through the thoracic cavity. Describe the azygos system of veins. Describe and contrast the distribution of the vagi and phrenic nerves throughout the thoracic cavity. Discuss the relationship of the heart, pericardium, lungs, and pleura to structures in the posterior mediastinum. ○ Mediastinum The anatomic region located between the lungs separating two pleural cavities. Contains all the principal tissues and organs of the chest except the lungs. It contains the heart, thymus gland, portions of the esophagus and trachea, and other structures Boundaries Sternum → vertebral column Laterally by the pericardium, the membrane enclosing the heart AND mediastinal pleurae, (part of parietal pleura that lines the thoracic cage). Sternal Angle – 2nd costal cartilage to T4/T5 intervertebral disc Junction of manubrium and sternum Compartments Superior Mediastinal Compartment – above sternal angle ○ Borders Posteriorly – first four thoracic vertebrae Above - continuous with the neck; Below - continuous with both anterior and posterior mediastinal compartments. ○ 2nd costal cartilage to T4/T5 interveterbral disc Laterally - limited by parietal (mediastinal) pleura. ○ Contents of the Superior Mediastinum: Thymus Aortic arch – including the Brachiocephalic trunk, left common carotid artery, left subclavian artery ○ Everything below the sternal angle (below superior mediastina) is not the aortic arch Superior Vena Cava – including the left and right brachiocephalic veins Trachea – ends at bifurcation of the trachea Esophagus Right vagus nerve Left vagus nerve – including the Left recurrent laryngeal nerve Phrenic nerves Thoracic duct ○ ○ ○ ○ ○ Inferior Mediastinal Compartment – below sternal angle ○ Anterior Mediastinal Compartment Borders - sternum anteriorly and pericardial sac posteriorly. Contents - sternopericardial ligament, fat and lymph nodes ○ Middle Mediastinal Compartment – contains heart and pericardium Borders - the anterior mediastinal compartment ventrally and the posterior mediastinum dorsally Contents - the pericardium, heart, phrenic nerves, pericardiacophrenic vessels, stems of great vessels. ○ Posterior Mediastinal Compartment Borders - pericardial sac anteriorly and the anterior surface of the vertebral bodies posteriorly Contents - descending aorta, esophagus, azygous system of veins, vagus nerve, thoracic duct, lymph nodes, thoracic splanchnic nerves. The Thymus A primary lymphoid organ Located in the lower part of the neck and the anterior part of the superior mediastinum Posterior to the manubrium and extends into the anterior mediastinum The thymus continues to grow (age of 5-6 years) but after puberty it is largely replaced by fat Blood supply – inferior thyroid and internal thoracic Internal Thoracic (mammary artery) – descends into thorax lateral to the edge of the sternum, ends at 6th rib Innervation - branch from vagus and sympathetic trunk Lymphatics - anterior mediastinal nodes Function – development and maintenance of immune system Portions of the Aorta Ascending aorta - from left ventricle to aortic arch mostly within pericardial sac Aortic arch - above plane of sternal angle; courses posteriorly and laterally Branches – all travel superiorly ○ Brachiocephalic – moves to right of the trachea (others move to left) Divides into right subclavian and right common carotid ○ Left Common Carotid – ○ Left Subclavian – lies against left lung and pleura Descending portion of thoracic aorta continuation of arch on left side of vertebrae reaches midline at T12 as it passes through diaphragm "I Ate 10 Eggs At Noon" – Inferior vena cava pierces at T8, Esophagus at T10, Aorta at T12 Pulmonary Trunk and Pulmonary Arteries Pulmonary Trunk - Courses upward and to the left Divides into left and right pulmonary aa. in concavity of aortic arch ligamentum arteriosum – connects pulmonary trunk to aorta (remnant from development) Right pulmonary artery - posterior to ascending aorta Left pulmonary artery - anterior to descending aorta Great Veins of the Thorax Generally veins are in plane anterior to arteries Inferior vena cava - pierces diaphragm at T8 - immediately enters pericardium and heart Left brachiocephalic vein - internal jugular + subclavian → joins right brachiocephalic vein (behind intercostal space 1) → superior vena cava courses obliquely to right in front of great aa. Right brachiocephalic vein - joins left brachiocephalic vein → s. vena cava formed similar to left - course vertically behind manubrium Superior vena cava – azygous veins + two brachiocephalics → superior vena cava formed behind intercostal space 1 Connects to right atrium Pulmonary veins - directly from root of lung to left atrium ○ Lymphatics of the Thorax Anterior Mediastinal Nodes – near great vessels of mediastinum Middle Mediastinal Nodes – drains bottom of trachea and proximal bronchioles Posterior Mediastinal Nodes – drains area around heart Thoracic Duct drains all of body below diaphragm and left side of thorax. cisterna chyli - dilation of origin of thoracic duct (abdomen) Pathway - ascends through aortic hiatus of diaphragm. ascends between azygous vein and aorta to T4-5 plane. crosses to the left at T4-5 to ascend behind the esophagus into neck Empties into - internal jugular and subclavian veins. Right Lymphatic Duct - 3 branches drains what the thoracic duct doesn't (upper right portion of thorax) right jugular: drains the right side of head and neck subclavian: drains right upper limb bronchomediastinal: drains the right side of the thorax Structure of lymph node – has 4 vessels going in, 2 vessels going out so that lymph has time to stay in node and get cleaned ○ The Trachea D-shaped tubes supported by cartilage Path Bifurcation at T4-5 Anteriorly: great vessels and thymus, Posteriorly: esophagus, Azygous vein to right of bifurcation, Aortic arch to left of bifurcation Carina divides the bronchi Blood supply: bronchial aa. and inferior thyroid aa. Innervation: pulmonary plexus and branches of vagus and sympathetic trunk ○ The Esophagus Muscular tube - striated muscle in neck, smooth muscle in lower third, mixed in middle Left atrium is indented into the esophagus Constrictions – cancers can happen here because of mechanical stress superior end in neck where aorta and left bronchus compress it near gastric end Innervation (all by vagal nerve) Striated muscle – innervated by vagal (recurrent branch) Smooth muscle – innervated by parasympathetic vagal Esophageal plexus - surrounds lower thoracic esophagus, contains mostly vagal fibers but some sympathetic Arteries - esophageal branches of thoracic aorta anastomose with inferior thyroid aa. and left gastric aa. Veins submucosal plexus and surface plexus, drain to azygos system, may drain superiorly to inferior thyroid vv., may drain inferiorly to gastric vein (portal-caval) Courses through superior and posterior mediastinum (don't worry about this) continuous superiorly with pharynx in neck pierces diaphragm at T10 to join stomach upper portion in thorax, slightly left of midline at lower end passes through diaphragm to left of midline pushed toward midline by aortic arch Associations Anterior - trachea, l. bronchus (crosses it), pericardium (l. atrium), posteriorly: vertebral bodies, thoracic duct, azygos system, intercostal aa. right: terminal azygos, left: aortic arch crosses ○ Phrenic Nerve In the surface of the pericardium Motor - all of diaphragm (C3-5) Sensory - parietal pleura, pericardium, central diaphragm Right phrenic - descends along right side great veins: right brachiocephalic vein, s. vena cava, right atrium, i. vena cava, anterior troot of lung Left phrenic - courses along left side of subclavian artery crosses left side of aortic arch anterior troot of lung, along left side of pericardial sac ○ Vagus Nerve Preganglionic parasympathetic fibers for thoracic and abdominal viscera Right vagus – not as close to lungs? enters thorax posterolateral to brachiocephalic vein, anterior to rt. subclavian artery right recurrent branch hooks under subclavian artery to ascend near trachea and esophagus descends to lateral side of trachea posterior to root of lung descends on posterior esophagus to form esophageal plexus passes through diaphragm with esophagus as posterior vagal trunk Left Vagus – closer to lungs? enters thorax between carotid and subclavian arteries descends to cross left side of aortic arch Left Laryngeal Recurrent branch curves around aortic arch and ligamentum arteriosum to ascend in neck between trachea and esophagus Posterior to root of lung onto anterior esophagus - forms esophageal plexus Goes through diaphragm with esophagus as anterior vagal trunk Branches of vagus in thorax: left recurrent laryngeal, br. to pulmonary plexus, br. to esophagus, br. to cardiac plexus ○ Azygos System of Veins Generally drains intercostal veins, some lumbar segmental veins Azygos vein formed by union of right ascending lumbar vein and right subcostal vein ascends along right side of vertebral column to T4 superficial to intercostal aa. thoracic duct to the left arches over bronchus to join superior vena cava tributaries (not as important)- right posterior intercostal vv. - 5-11 right superior intercostal vein - drains ICS 2-4 hemiazygous vein accessory hemiazygous vein esophageal, mediastinal, pericardial, bronchial veins Accessory hemiazygos vein formed by posterior intercostals 4-8 descends on left of vertebral column crosses to join azygous at T8 Hemiazygos vein (bottommost branch) formed by union similar to azygous ascends on left of vertebral column crosses over to join azygous at T8-9 posterior to aorta and esophagus tributaries - left posterior intercostal veins 7-11, esophageal, mediastinal, pericardial veins Left superior intercostal vein (topmost) formed by upper posterior intercostal veins drains to left brachiocephalic vein ○ Clinical Cases Superior Mediastinal Mass Head on Car Accident Syncope & Facial Flushing – distended veins, superior vena cava syndrome Chylothorax – leakage of lymph Development of the Respiratory System ○ Objectives Define: pharynx, larynx, foregut, pharyngeal arches and pouches. List the germ layers of origin for: epithelium, glands, cartilage, smooth muscle, and blood vessels of the respiratory system Describe the laryngotracheal groove. Define/describe the development of the laryngeal cartilages and musculature. Describe the process by which the trachea is separated from the esophagus by the tracheoesophageal septum (folds). Describe the probable process by which a congenital tracheoesophageal fistula is created. What are the consequences of this defect? Define/describe the lung buds. Correlate the first, second, and third divisions of the distal end of the primitive trachea with the bronchi of the adult lung. Define/describe the four major phases in lung development. Describe the processes by which the intraluminal fluid contents of the respiratory system are removed at and immediately after birth. Define/describe: surfactant. Where and when is it produced? What is its function? What are the consequences of a lack of surfactant in the lung? Define/describe: respiratory distress syndrome (RDS)/ hyaline membrane disease (HMD). How are these pathological processes treated currently? Explain the formation of: congenital lung cysts, lung agenesis, and lung hypoplasia. Describe the major features of the time line for respiratory system development. How do these features relate tthe survivability of a premature infant. ○ Structures Laryngopharynx – inferior 1/3 of pharynx, develops from the foregut Larynx – airway supported by thyroid, cricoid, arytenoid and epiglottic cartilages Upper Respiratory Tract – external nares to laryngopharynx Lower Respiratory Tract – larynx, trachea, bronchi and lungs ○ Early Development Beginnings Foregut – becomes pharynx, esophagus, stomach, duodenum ○ Lining contains endoderm Pharyngeal Arches – form the ventral and lateral walls of the foregut ○ Up by embryo’s ‘neck’ Pharyngeal Pouches – pockets along inner surface of foregut ○ Lined by endoderm (forms lining of tract) ○ Just dorsal to the pharyngeal arches A Little Later the beginning of the lower respiratory tract forms Development of the lower respiratory tract begins in the foregut around the 4th week of development Endoderm – forms epithelia and glands of larynx, trachea, bronchi and lungs Splanchnic mesoderm – forms smooth muscle and cartilage of that stuff Respiratory Primordium – invagination of endoderm that forms all of the epithelia and glands of the lower respiratory tract and laryngotracheal groove ○ Larygotracheal groove – a pocket of endoderm off of primordial gut (that will be esophagus) Is the respiratory primordium?? Invaginates to form primordial trachea and bronchial buds ○ Larygotracheal diverticulum – the beginning of the little bud formed by the invagination of the laryngotracheal groove ○ Respiratory bud – same little bud as laryngotracheal diverticulum, just bigger Induced by FGF10 from the splanchnic mesoderm, controlled by SHH ○ Tracheoesophageal fold – forms division between developing respiratory tract and existing primordial gut ○ Tracheoesophageal septum – same division, just a little more developed ○ Laryngotracheal tube – forms at base of respiratory buds and extends to make tube (trachea etc.) ○ Primary bronchial buds – more advanced respiratory buds at the end of laryngotracheal tube, they multiply ○ Development of the Larynx Endoderm of laryngotracheal tube forms laryngeal epithelium Mesenchyme of hypobrachial eminence (ventral ends of the 3rd and 4th pharyngeal arches) forms the epiglottis Hypobrachial eminence is cranial to laryngotracheal groove in the foregut lumen Mesenchyme of cranial part of laryngotracheal tube (4th and 6th pharyngeal arches) forms arytenoid, cricoid and thyroid cartilages Myoblasts in 4th and 6th pharyngeal arches forms laryngeal muscles ○ Development of Trachea Kinda need to look at pictures Hypobranchial eminence moves caudally toward laryngotracheal groove to help form the epiglottis The epiglottis on cranial side and arytenoid swellings on both sides caudally temporarily close the opening to future respiratory tract around 6 weeks, but it opens up again and laryngeal cartilages are developed Remember Endoderm forms the epithelium and glands Splanchnic mesoderm forms the cartilage rings and smooth muscle Clinical Correlation Atresia – when an organ abnormally dead-ends Fistula – abnormal connection between two organs Esophageal atresia – developmental obstruction of the esophagus Tracheoesophageal fistula – abnormal communication between trachea and esophagus ○ Associated with incomplete fusion of the tracheoesophageal folds ○ Usually occurs with esophageal atresia Polyhydramnios – excess amniotic fluid, occurs when amniotic fluid access to digestive tract is blocked Examples ○ Upper esophageal atresia with lower tracheoesophageal fistula – can only get food into esophagus by inhaling it. Results in pneomonitis because food gets into lungs since it backs up in esophagus? ○ H-type – just a fistula, things can go both directions ○ Upper tracheoesophageal fistula with lower esophageal atresia – makes polyhydramnios because no access to digestive tract, things swallowed go into lungs ○ Upper and lower tracheoesophageal fistula (with two atresias?) – esophagus ends and goes into trachea then can go down trachea or out to lower esophagus ○ Development of Bronchi and Lungs Bronchial Buds become Primary bronchi which become main Secondary bronchi which become lobar – can be seen by 6 weeks Tertiary bronchi which become segmental Respiratory bronchi Primitive lungs form in a cavity lined by somatic mesoderm (which becomes body wall) and then just inferior to that is the pericardioperitoneal canal (which is the primordial pleural cavity) The lungs are covered in splanchnic mesoderm which becomes the visceral pleura The lungs then push out laterally into the pericardioperitoneal canal and somatic mesoderm Maturation of the Lungs Pseudoglandular Period – 6-16 weeks ○ Conducting airways develop in the lungs ○ Capillaries form in splanchnic mesoderm Canalicular Period – 16-26 weeks ○ Lumens of bronchi and bronchioles enlarge ○ Respiratory bronchioles and alveolar ducts form by the end of this period ○ More blood vessels form Signaled by WNT gene from epithelium ○ Gas exchange is possible by the end of this period Terminal Sac Period – 26 weeks to birth ○ More terminal sacs present ○ More capillaries contact the epithelium ○ Epithelium (Type I cells) thins over capillaries ○ Blood/air barrier is established ○ Type II cells develop – secrete pulmonary surfactant Surfactant levels are sufficient by 28 weeks Alveolar Period – 32 weeks to 8 years ○ 95% of all alveoli form during this period ○ Mature alveoli appear after birth ○ Branching produces more respiratory bronchioles ○ Alveolar ducts and alveolar sacs form See pictures? Fetal Breathing Movements – occurs intermittently during development to stimulate lung development and strengthens respiratory muscles Changes in Respiratory Tract that Occur at Birth A. Replacement of fluid in airways with air ○ Fluid expelled during delivery due to compression of thorax ○ Fluid absorbed by pulmonary capillaries ○ Fluid absorbed by lymphatics B. Pulmonary circulation ↑ as lungs inflate with air C. Ductus arteriosus and foramen ovale close sending more deoxygenated blood to the lungs Clinical Correlations Congenital Lung Cysts – air or fluid filled cyst caused by blockage of airway ○ Usually on visceral surface of lung Lung Agenesis – when bronchial buds don’t grow into mesenchyme of lung ○ Unilateral agenesis is survivable Lung Hypoplasia – lungs or portion of lungs don’t grow enough ○ Often associated with diaphragmatic hernia that causes intesting to move up into left side of thorax ○ Usually fatal Respiratory Distress Syndrome (RDS)/hyaline membrane disease – insufficient surfactant present in lumen of alveoli ○ Results in atelectasis – alveoli collapse during expiration ○ Most common of all neonatal diseases ○ Will occur in premature babies born before week 32 ○ Symptoms Rapid, labored breathing begins shortly after birth ○ Doesn’t happen right away because it takes a while for all the alveoli to collapse Nostril flaring, grunting, cyanosis Rib retraction – due to intercostal muscles pulled inward Concavity to rib cage because not enough air in lungs (‘bell type rib cage’) ○ Treatments You can determine amount of surfactant by measuring phospholipids in amniotic fluid ○ If there isn’t enough, then give mother betamethason (steroids) & thyroid hormone to stimulate type II pneumocytes After birth, give exogenous surfactant After birth, give continuous positive airway pressure to keep alveoli open ○ Histologically Liquid leaks into alveoli from capillaries due to the stress or atelectasis ○ Fluid builds up in the lungs Heart and Pericardium ○ Objectives Describe the location of the heart within the thoracic cavity and its relationship with the pericardium and the pericardial cavity. Describe the structure and function of the layers of the pericardium Define the atrioventricular groove, anterior and posterior interventricular sulci, apex and base of the heart, anterior, posterior and diaphragmatic surface of the heart. Describe the layers of the heart, relating structure and function. Describe the internal structure of the right atrium including: right atrial appendage, superior and inferior venae cava, crista terminalis, musculi pectinati, coronary sinus, and fossa ovalis. Describe the internal structure of the left atrium, including: musculi pectinati, and the left atrial appendage. Describe the components and locations of the Tricuspid, Mitral and semilunar valves (Aortic and Pulmonary). Describe the surface projections and auscultation points for each of the heart valves on the chest wall. Describe the normal heart sounds. Describe heart murmurs and explain valve stenosis and regurgitation. Describe the internal structure of the right ventricle including: trabeculae carneae, papillary muscles, septomarginal trabecula, and supraventricular crest. Describe the internal structure of the left ventricle, including: trabecuale carnea, and papillary muscles. Describe infundibulum and conus arteriosus. Describe the fibrous skeleton of the heart. Describe systole and diastole and relate these events tthe normal heart beat and cardiac cycle Describe the flow of blood through the heart, comparing and contrasting the pulmonary and systemic circulations. ○ Note – heart is one of the first organs to start working ○ Pericardium Double-walled fibroserous sac which surrounds and covers the heart and roots of great vessels Serous pericardium - serous, lining layer Parietal layer - lines inside of fibrous pericardium Visceral layer - covers outside of heart = epicardium (which is 'part' of the heart) Fibrous pericardium – connective tissue layer outside of the parietal serous layer – forms bulk of the gross pericardial sac - fused to adjacent connective tissue planes Pericardial space - potential space between parietal and visceral layers - contains only a moistening layer of fluid All the layers in order Outside → fibrous pericardium → serous pericardium (parietal layer) → pericardial space → serous pericardium (visceral layer/epicardium) → myocardium → endocardium → inside Pericardial sinuses - formed during folding of heart tube development Transverse Pericardial Sinus - The passage between the venous and arterial mesocardia—i.e., between the aorta and pulmonary artery (making front part) and the inferior vena cava (making back part) ○ Between the ends of the primitive heart tube, separates arteries from veins Oblique Pericardial Sinus - The cul-de-sac behind the heart bounded by the pulmonary veins Pericardial Extent – where the pericardium attaches to other structures Superiorly - fuses with adventitia of great vessels at level of the sternal angle Inferiorly - fuses with fascia of the diaphragm Laterally - fuses with mediastinal pleura Posteriorly - fuses with adventitia of esophagus Blood Supply - Pericardiacophrenic - from internal thoracic Innervation - phrenic nerves (left and right), vagal nerves, sympathetic trunk Function It contains approximately 10 to 15 cc's of serous fluid. The function of the pericardium is to limit or prevent acute pathological distension of the heart once the pericardial reserve volume has been used up and the pericardium is stretched. The pericardial attachments maintain the heart in its normal position and are so arranged that external forces exerted on the pericardium by respiration or changes in body posture tend to cancel each other and maintain a constant heart position. Problems Cardiac Tamponade – when too much fluid gets into the pericardial sac (maybe by hole in heart) and prevents heart from beating (very deadly) ○ Pericardiocentesis – way to drain pericardium by sending a needle with an electrode (to make sure you don’t hit the myocardium) through the subxiphoid angle ○ Heart Wall Epicardium - visceral layer of the pericardium - external covering of heart subepicardium - between epicardium and myocardium - contains fat and coronary arteries/veins Myocardium - middle muscular layer – oblique fibers – torsion of chambers Endocardium - inner lining layer - composed of endothelium backed by thin connective tissue subendocardium - just outside the endocardium - contains tissues of the conducting system ○ Surfaces of the Heart Anterior, Right Pulmonary, Left Pulmonary, Diaphragmatic Surfaces Inferior (acute) margin – at bottom of anterior surface just before the diaphragmatic surface Obtuse margin – in between anterior surface and left pulmonary surface, basically parallel to LAD Base – where great vessels attach Apex – formed by LV Precordium – area between base and apex Left atrial appendage – pocket in left atrium that kinda sticks out (there is a right one too) Note – the leftmost portion of the heart shouldn’t extend out past the midclavicular line ○ Heart Chambers Right Atrium Crista terminalis – in RA only, like the body of the comb (boundary between RA and right appendage???) Musculi pectinati – like the teeth of the comb Fossa ovalis – remnant of foramen ovale Valve of the coronary sinus – where veins of the coronary sinus drain into Valve of the inferior vena cava – non-functional ○ Blood can back up in the venous system and will cause liver to enlarge due to backup, this can cause pain ○ Backup can also cause jugular distension Tricuspid Valve – sends blood into RV ○ Has anterior (main), septal, and posterior cusps Right Ventricle Conus Arteriosus – exit of right ventricle to the pulmonary trunk Septomarginal trabeculae – found only in RA and is part of the conduction system ○ Connects interventricular septum to anterior papillary muscle Papillary Muscles – the main one is the anterior, but posterior and septal also exist Pulmonary Valve – has anterior, right and left semilunar cusps ○ 'A&P' – since it is the Pulmonary valve it has an Anterior cusp Choradae tendinae – Connects papillary muscles to valves Trabeculae Carne – rounded, irregular muscular columns surrounding the interior of the ventricle Supraventricular Crest - The internal muscular ridge that separates the arterial cone from the rest of the cavity Left Atrium Pulmonary Veins – four of them enter Valve of foramen ovale – Mitral valve – sends blood into LV ○ Has anterior and posterior cusps Is smooth Left Ventricle Infundibulum – like the conus ateriosus, exit of left ventricle to the aorta Anterior and Posterior Papillary Muscles – only two here and each connects to half of the valve so that if one is broken the valve will still partially work Trabeculae Carne – rounded, irregular muscular columns surrounding the interior of the ventricle Aortic Valve – has posterior, right and left semilunar cusps ○ 'A&P' – since it is the Aortic valve it has a Posterior cusp ○ Heart Valves Atrioventricular Valves Have fibrous ring around the edge to hold everything together Have chordae tendinae Have papillary muscles that contract before ventricles contract to prevent regurgitation into atria Right Atrioventricular Valve (Tricuspid) - between the RA and RV Left Atrioventricular Valve (Mitral) - between the LA and LV Semilunar Valves Lunule – edge of semilunar valves Nodule – midpoint of edge of valve so that when they all close there is no opening Pulmonary valve - closes the orifice of the pulmonary trunk, which consists of three semilunar cusps Aortic Valve - closes the Aorta and also consists of three semilunar cusps ○ Openings for coronary arteries are behind the right and left semilunar valves ○ Skeleton of the Heart Fibrous connective tissue to which valves and muscle of heart are attached Function - support and rigidity Serves as an electrical insulator preventing conduction between atria and ventricles. ○ Extra Notes The angle between the right atrium and right ventricle is large The angle between the left atrium and left ventricle is small and so if anything messes up here then more problems Franklin Sterling Law of the Heart – normally if 100ml goes into the LV then 100 ml will go through circulation, if this isn’t the case then you’ve got problems Myocardial Architecture – when the heart contracts it twists like wringing a towel The muscular fibers (mainly ventricular fibers) are aligned like a spiral so that this occurs Atrial fibers go around pulmonary veins?? ○ Heart Sounds S1 (Lub) – first sound, closure of AV valves due to ventricle contracting Systole – ventricular contraction phase, between S1 and S2 S2 (Dub) – second sound, closure of semilunar valves If you ask patient to inspire while listening, then S2 will separate into aortic then pulmonary valve closing Diastole – relaxation phase Note – sounds are not associated with valves opening Extra Diastolic Heart Sounds S3 (Ventricular Gallup) – early diastole ○ Results from tensing of the chordae tendinae during rapid filling and expansion of the ventricle ○ Normal in children, but pathologic in adults S4 (Atrial Gallup) – late diastole ○ Results from the left (or right) atrium vigorously contracting against a stiffened ventricle ○ Usually indicates disease Murmurs Sound generated by turbulent flow Described by their timing, intensity, pitch, shape (gets louder or softer during the beat), location, radiation and response to maneuvers ○ Note – grade 6 is highest for systolic, grade 4 is highest for diastolic Systolic Murmur – can be caused by aortic & pulmonary stenosis OR mitral & tricuspid regurgitation Diastolic Murmur – can be caused by aortic & pulmonary regurgitation OR mitral & tricuspid stenosis ○ Ventricle dialated?? Sounds – aortic stenosis, mitral stenosis, pulmonary stenosis, mitral prolapse, mitral regurgitation, aortic insufficiency Conduction System and Coronary Circulation ○ Objectives Conduction System: Describe the components and function of the cardiac conduction system including the: sinu-atrial node, atrioventricular node, atrioventricular bundle (bundle of His), right and left bundle branches and the septomarginal fasciculus. Describe the location of the SA node and AV node. Describe the interatrial or internodal conducting tracts: ○ Bachmann’s bundle tthe left atrium ○ Anterior internodal tract (James’s Tract) ○ Middle internodal tract (Wenckebach’s tract) ○ Posterior internodal tract (Thorel’s tract) Describe the autonomic innervation of the heart and its influence in the regulation of the conduction system and control of the cardiovascular system. Correlate the sequence of excitation of the components of the heart conduction system with a basic electrocardiogram trace image. Compare and contrast normal sinus rhythm with sinus bradycardia, tachycardia, heart block and fibrillation. Coronary Arteries: Describe the origin and course of the right and left coronary arteries and explain the nature of their anastomoses. Describe the following branches of the right coronary artery: sinoatrial (SA) nodal artery, right marginal artery, Atrioventricular (AV) nodal artery, terminal branches, posterior interventricular artery and septal branches Describe the following branches of the left coronary artery: left circumflex artery, anterior marginal artery, obtuse marginal artery, atrial branches and posterior marginal arteries, anterior interventricular artery, anterior diagonal artery and septal branches. Describe the concept of Dominance of coronary circulation. Describe the specific tasks required of the coronary circulation and how the coronary circulation is structurally and functionally adapted. Define ischemic heart disease and describe the consequences of inadequate blood supply tthe heart muscle. Cardiac Veins: Describe the venous drainage of the heart. Describe the coronary sinus and the Thebesian valve (valve of the coronary sinus). Describe the relationship of the coronary sinus and the left atrial wall. Describe the distribution pattern of the tributaries of the coronary sinus: great cardiac vein, middle cardiac vein, oblique vein of the left atrium, and small cardiac vein. ○ The Conducting System Sinoatrial node (SA node) = pacemaker located along upper end of sulcus terminalis - near SVC initiates heart beat supplied by both sympathetic and parasympathetic nerves most superficial node and can be affected by pericarditis Interatrial or internodal conducting tracts: ○ Bachmann’s bundle - originates in the SA and is the only tract that conducts action potentials to the left atrium. ○ All run from SA node through RA to the AV node - Anterior internodal tract, Middle internodal tract, Posterior internodal tract Atrioventricular node - located in interatrial septum adjacent to the ostium (opening) of coronary sinus inside the Triangle of Koch. Electrical relay station between atria and ventricles Serves as a gate that slows the electrical current so that the atria contract fully before the ventricles Triagle of koch - a roughly triangular area on the septal wall of the right atrium, between the tricuspid valve, coronary sinus orifice, and tendon of Todaro, that marks the site of the atrioventricular node. Tendon of Todaro – formed by the junction of the inferior vena cava and near the pulmonary valve Atrioventricular bundle (of His) - extends from AV node along the IV septum Collection of heart muscle cells specialized for electrical conduction that transmits the electrical impulses from the AV node to the point of the apex of the 2 bundle branches Bundle Branches - AV bundle divides into right and 2 left bundle branches in the septum (near junction of membranous and muscular part of septum) Purkinje fibers – Purkinje fibers carry the contraction impulse from the left and right bundle branches to the myocardium of the ventricles. Ventricular conduction system – bundle branches + Purkinje fibers Septomarginal trabeculae (Trabeculum septum marginal) – fibers from the interventricular septum that run directly to anterior papillary muscle in RV to make sure that it is stimulated first Ectopic Pacemakers - Potential Pacemakers that aren’t the SA node If one pacemaker (the SA node) fails then others can take over, but they have different bpm ○ Places around SA Node – 60-80 bpm ○ AV Node (nodal rhythm) – 40-60 bpm ○ Ventricles – 20-40 bpm ○ The EKG P Wave - the sequential depolarization of the right and left atria (SA node) QRS Complex – right and left ventricular depolarization (usually this is simultaneous) (bundle branches and Purkinje) ST-T Wave – ventricular repolarization U Wave – unknown PR Interval – time interval between atrial contraction and ventricular contraction When impulse is in AV node and bundle of His QRS Duration – duration of ventricular muscle depolarization ○ Heart Rhythm Abnormalities Premature Ventricular Contraction – can be caused by hypoxia, electrolyte imbalance, stimulants, stress Arrhythmias Heart Block – failure of conduction system to transmit signals ○ Total heart block – damage to AV node → P Wave still present but nothing else is Ventricular Fibrillation – charges all over firing randomly ○ Nerve Supply to the Heart Sympathetic System Excitatory – can raise heart rate to 230 bpm ↑ BP, ↑HR, Vasodilate the coronary arteries, ↑the force and speed of contraction (contractility) From upper thoracic spinal cord, through sympathetic chain to cardiac nerves ○ From cervical sympathetic trunk ○ From direct branches of sympathetic nerves from the thoracic trunk ○ Preganglionic level T1-T5, most ascend to synapse Transmits ischemic pain and sensations to CNS ○ Nerves go to sympathetic trunk and get a little intermixed with left arm nerves - referred pain Parasympathetic System Inhibitory – can slow heart rate to 70-80 bpm ↓HR, ↓BP, Constrict the coronary arteries Gets to heart via vagal nerve, specifically the right vagal nerve to the SA Node and the left vagal nerve to the AV node ○ Vagus comes from both cervical branches and direct branches in thorax?? Sends visceral reflex activity to CNS via vagal nerve ○ aortic bodies – in wall of ascending aorta, monitors PCO2 and changes respiration rate Cardiac Plexus Has both sympathetic and parasympathetic contributions Superficial Plexus – near aortic arch, receives input from ○ Parasympathetic - left inferior cervical branch of Vagus nerve (CN X) ○ Sympathetic - superior cervical sympathetic branches Deep Plexus – near tracheal bifurcation receives input from all the rest ○ Parasympathetic – vagus nerve ○ Sympathetic – superior, middle and inferior (right) and middle and inferior (left) ○ Cardiac Blood Supply Coronary Arteries heart is fed during dyastole Right Coronary Artery ○ Arises from right aortic sinus (behind semilunar valve). Courses in atrioventricular (coronary) sulcus from the aorta toward region of the posterior IV sulcus ○ Branches Right marginal branch – feeds acute angle Posterior interventricular branch (80%) Sinoatrial branch - (55%) Atrioventricular nodal branch - (85%) ?? Left Coronary Artery ○ Arises from left aortic sinus (behind semilunar valve). Courses in the anterior IV sulcus where it divides. ○ Branches: Anterior interventricular (descending) branch - LAD Circumflex branch ○ Left marginal branch ○ Posterior interventricular branch (20%) ○ Sinoatrial nodal branch (45%) ○ Atrioventricular nodal branch (15%) ?? Supply to Nodes ○ SA node gets blood from right and left coronary arteries? ○ AV node gets blood from AV node artery (mainly right coronary artery) Supply to Papillary Muscles ○ Left Anterior - from LAD and circumflex Posterior - only from posterior IV branch ○ Right Anterior – LAD and right coronary artery Posterior – posterior IV branch, right coronary artery, septal (from LAD) Septal – from 1st, 2nd, 3rd septal arteries (from LAD) Coronary Veins Usually superficial to arteries Anterior Interventricular vein - along course of LAD, feeds into → Great Cardiac Vein – runs along left side of atrioventricular sulcus into → Coronary Sinus – in posterior atrioventricular sulcus, much thicker and feeds directly into RA Middle Cardiac Vein – feeds directly into coronary sinus from posterior IV sulcus area Small Cardiac Vein – feeds directly into coronary sinus from atrioventricular sulcus around right side Myocardial O2 Supply and Demand Supply – influenced by diastolic perfusion pressure, coronary vascular resistance, O2 carrying capacity Demand – responded to by wall tension, heart rate, contractility Myocardial Infarction Obstruction of each major coronary artery results in infarction of a specific area of myocardium Right Coronary Obstruction – inferior infarction, can involve posterior septum (30% of all cases) Circumflex Artery Occlusion – lateral infarction (20% of all cases) LAD Occlusion – anterior infarction artery of ‘sudden death’ (50% of all cases) Coronary artery bypass uses a vein but then after 10 years the vein will adopt properties of an artery Determining Coronary Dominance Crus Cordis – point where atrioventricular, interatrial and interventricular sulcus meet on anterior surface Can be right dominant, balanced or left dominant Dr. Gold says it is determined mainly by where SA node gets its blood supply from Collateral Circulation Network of tiny blood vessels, which under normal conditions are not open Some collateral vessels may enlarge and become active when other coronary arteries narrow to the point that blood flow to the heart is impeded. Takes a while to become active Cardiac Imaging ○ Objectives None ○ Random Notes Heart rotates to the left during development Branches of LAD – diagonals Branches of circumflex – marginals Where artery of AV node comes from is what really determines dominance RV papillary muscles have multiple connections to the interventricular septum LV papillary muscles do not have multiple connections to the interventricular septum LV is a little more smooth and does not have trabecular connections to the septa If it did, then the fetus would die Papillary muscles must contract before the ventricles There is direct fibrous continuity between the aortic valve and mitral valve leaflets Pulmonic valve is not part of the fibrous skeleton of the heart??? SA node is on the epicardial surface of the heart Mitral Valve Prolapse – trabeculae become thinned and can cause the two valves to be misaligned Echocardiograms Echocardiograms look at heart upsidedown from the apex Dots are 1 cm apart The MHz of the echocardiogram need to be different depending on where you stick the probe ○ Transesophageal echocardiogram uses 7.5 MHz In Doppler echocardiograms you can transform the velocity information into pressure info via P=4V2 Transesophageal Echo – has multiple potential views (trans-atrial, trans-gastric, epiaortic) Pathology Tumor on valves can break off tiny pieces and cause strokes and such Aortic stenosis – can see because aorta doesn’t move Thickening of aorta – can see because of dots on the image Contraindications – esophageal or pharyngeal problems, can’t bend neck, pediatric size issues Complications – hoarseness is actually a significant problem, etc. If used during an operation it will often help and change the operation Enhances preop diagnostic accuracy, well suited for evaluating great vessels, serves to guide volume & contractility so medicines can be altered?, improves evaluation of operation, reduces morbidity and mortality of cardiac surgery Development of the Cardiovascular System ○ Objectives Compare and contrast vasculogenesis and angiogenesis. List/describe the derivatives of the aortic arches. Diagram the sequential changes that lead tthe development of the definitive aortic arch and its branches. Describe the development errors that result in aortic arch abnormalities. Describe the developmental relationships of the recurrent laryngeal nerves. Define and describe: cardinal veins (anterior, posterior, common), subcardinal veins, supracardinal veins. Describe the formation of the left brachiocephalic vein, and the ductus arteriosus Describe the development errors that result in venous system abnormalities. ○ Development of Blood and Blood Vessels Blood Islands – develop in the mesodermal wall of yolk sac into vessels Hemangioblasts help form primordial blood island Hemocytoblasts – form blood inside blood islands Angioblasts – endothelial cells that line the blood island to make a primitive vessel Vasculogenesis – fusion of locally formed endothelial vesicles (tubelike free-floating vesicles made out of angioblasts) to form extensions of blood vessels A developmental process Angiogenesis – outgrowth or branching of preformed vessels Happens throughout life In early embryo there are no blood vessels, then the extraembryonic vascular channels develop, then the intraembryonic vascular network develops Differentiation process - Vascular networks develop into vessels and which type of vessel is made is determined by the amount of pressure it is exposed to? Development of Veins – the embryo’s venous system develops out of a very irregular network of capillaries ○ Thus the venous system is not very uniform and there are more variants in venous than arterial system Factors (don’t remember molecules) - Vasculogenesis – VEGFR-1,2, Angiogenesis – VEGF A-E, completion of vascular wall (angiopoietin), differentiation into artery (mesenchyme migrates and TGF-β helps out) ○ Development of Circulatory System Primordial Heart Aortic Sac – has aortic arches sprouting off of it, primitive arterial circulation ○ Helps give rise to the arterial system (see below) Sinus venosus – primitive atrium, has three veins sprouting off of it, primitive venous circulation ○ Cardinal Veins – form the basis for the intraembryonic venous circulatory system anterior cardinal veins (superior) – drain blood from the head via the left & right common cardinal vein posterior cardinal veins (inferior) – drain blood from the lower half of the body into the two common cardinal veins During development of this system vessels dissolve and reappear to form the final result, the details aren’t important Superior vena cava formed by cardinal system ○ Umbilical System – bring nutrient and oxygen rich blood from the placental villi via the umbilical cord to the embryo Is an unpaired umbilical vein Connected to two intraembryonic umbilical veins The umbilical veins become included in the developing liver Development ○ Note that the right umbilical vein disappears and that a connection between the sinus venosus and the left umbilical vein develops through the liver and this is called the ductus venosus The ductus venosus allows embryo to control the pressure of blood coming in from maternal area ○ Omphalomesenteric (Vitelline) System – for yolk sac Closely associated with development of duodenum and liver ○ Portal vein, superior mesenteric vein and splenic vein all form from vitelline Drains the blood of the umbilical vesicle Pulmonary Veins – not associated with any of the three systems because they develop independently ○ Don’t really know how they develop Aterial System ○ Ventral Aorta – sprouts off the aortic arches ○ Heart starts turning ○ Heart starts forming in the neck, then the neck grows (or the heart moves down??) and attachments stretch ○ Aortic Arches Within each arch there is an artery, a nerve, and cartilage Organized similar to aquatic vertebrates Right and left dorsal aorta becomes single dorsal aorta Appear and disappear in a cranial → caudal fashion Derivatives of Aortic Arches ○ Note - 1,2 and 3 are all related to the head Original 'Arch' End Structure Most regresses, the rest forms maxillary artery 1 Most regresses, the rest forms stapedial artery 2 Forms common and internal carotid arteries 3 Forms proximal right subclavian artery Right 4 Forms arch of aorta Left 4 Never develops 5 Forms part of right pulmonary artery Right 6 Forms part of left pulmonary artery and ductus arteriousus Left 6 Not real arches Right 7th segmental artery Forms part of the right subclavian artery Forms entire left subclavian artery Left 7th segmental artery Regresses forms the middle of the right subclavian artery Right Dorsal Aorta Forms descending thoracic aorta Left Dorsal Aorta Forms ascending aorta and the brachiocephalic artery Aortic Sac ○ Ductus Arteriosus – communication from pulmonary trunk to aortic arch Blood sent to aortic arch instead of lungs before birth since lungs aren’t needed then Neural Crest Cells – help form aortic arches and heart ○ DiGeorge Syndrome – genetic problem that causes neural crest cells to be messed up and results in a bunch of abnormalities in different systems Note – arterial system develops in lots of places simultaneously then hooks up to stuff resulting from aortic arches?? ○ Aortic Arch Anomalies Right Aortic Arch ○ Results from obliteration of the left 4th branchial arch artery regression of the left dorsal aorta ○ Aortic arch instead is constructed from equivalent vessels on the right side ○ To reach aortic arch, the ductus venosus must go around the esophagus and can cause constriction Double Aortic Arch ○ Two arches surrounding the esophagus and trachea forming a vascular ring ○ Can cause dysphasia and respiratory distress ○ Results from - a failure of regression of the section of right dorsal aorta between the 7th intersegmental artery and the junction of the left dorsal aorta Interrupted Aortic Arch ○ Results from - the obliteration of the left 4th brachial arch artery The proximal part of the aortic arch still forms the three branches, but after that it stops ○ The ductus arteriosus persists and becomes greatly dilated, but doesn’t help anything because it is connected to pulmonary trunk Right Subclavian Artery Anomaly ○ Results from regression of the right 4th branchial arch artery ○ Causes the right subclavian artery to arise from aortic arch distal to the left subclavian artery Right subclavian then goes behind esophagus and trachea to produce a vascular ring ○ Recurrent Laryngeal Nerve Branch of the vagus nerve that supplies motor function and sensation to the larynx Arises from the 4th and 6th aortic arches?? During development the right and left laryngeal nerves go down and wrap around the blood vessels in the 6th arch ○ Then the right 6th arch disappears and the only thing the right laryngeal wraps around is right subclavian artery, while the left still wraps around the aortic arch Circulatory System ○ Objectives Identify the twmajor components of the circulatory system and their functions. Identify the components of the cardiovascular and lymphatic systems and integrate the structure with the function of each component. Describe the three layers of blood vessels and integrate their structural components tspecific functions. (Tunica intima, media, & adventitia) Compare and contrast the structural and functional differences between the various types of vessels, arterial and venous as well as microcirculation. Integrate the structure of the three types of capillaries with their functional capacities and locations. Integrate the structural components of an arteriovenous anastomosis and the microcirculatory bed ttheir functions. Relate the microscope structure of the heart tits gross anatomy. Identify and describe the layers of the pericardial sac and heart wall. Be able trelate them tthe function of the heart. Describe the structural components and functions of the cardiac skeleton. Describe the structural components cardiac conduction system and relate them ttheir function. Locate and describe the function of the carotid sinus and aortic bodies. Integrate the lymphatic system circulation intthe cardiovascular system both structurally and functionally. Relate how the following diseases affect the cardiovascular system: varicose veins, Marfan's syndrome, Ehler-Danlos syndrome, atherosclerosis, & aneurysm. ○ Circulatory System Closed system Heart Basic Anatomy ○ Cardiac muscle lined by endothelium ○ Has endocardium, myocardium and epicardium ○ Pericardial Sac Fibrous Pericardium – outer wall, fibroelastic CT Parietal Serous Pericardium – inner portion of pericardium Pericardial cavity Epicardium/Visceral Serous Pericardium – inner portion ○ Epicardium Two Layers ○ Mesothelium – outermost, simple squamous epithelium AKA visceral serous pericardium ○ CT Layer – contains adipose cells, nerves, ganglia and named coronary blood vessels ○ Myocardium Consists of cardiac muscle cells Layered and arranged so the heart twists as it contracts ○ Endocardium Two Layers ○ Endothelium – simple squamous epithelium with basal lamina ○ Subendocardial CT – areolar CT with Purkinje fibers, nerves and adipose Wraps around all internal structures like trabeculae carnae, chorda tendinae etc. Cardiac Muscle Histology ○ LM Level Striated fibers, centrally placed nuclei Intercalcated discs – specialized cell junctions at end of cells to connect them Endomysium – CT enveloping each muscle fiber Perimysium – CT between the layers of muscle bundles ○ EM Level Can see branched myofibrils, sarcomere, sarcoplasmic reticulum, T tubules (help store calcium) Intercalcated disc ○ Transverse portion – has fascia adherens, macula adherenes ○ Longitudinal portion – has gap junctions Myocardial Infarction ○ Scarring (with fibroblasts) repairs the heart wall, cardiac myocytes are not replaced ○ Can get cardiac hypertrophy due to increase in individual cardiac myocytes ○ Progression 2-4 days – coagulative necrosis, 7 days – neutrophils infiltrate, 7 weeks – fibroblasts make scar Cardiac Skeleton ○ Made of concentrations of dense irregular CT in heart (chondroid cells?) ○ Components Annulus Fibrosus – rings of CT around the openings of each valve that holds them open Fibrous Trigones – triangular-shaped CT area between the valves (on cusps) ○ Left and right trigones are pierced by the AV bundle Septum Membranaceum – CT extending downward from trigone onto top of IV septum ○ perpendicular to annulus and trigones ○ Functions Holds valves open and maintains their shape Point of insertion for cardiac muscle cells Insulation of atria from the ventricles Conduction System ○ Nodes Sinoatrial Node – innervated by sympathetic and parasympathetic nerves that modify the rate of firing AV Node – in lower RA in septum by tricuspid Bundle of His - pierces right trigone and enters ventricular septum L & R Bundle Branches – divide right at top of IV septum Subendocardial Plexus – contain Purkinje fibers? ○ Contraction starts at apex and spreads upward towards base ○ Purkinje fibers - modified cardiac muscle cells that start in bundle branches and end in plexus Located in subendocardial CT layer of endocaridum ○ Differentiated Cardiac Muscles Pacemaker cells – initiate contraction, leaky cells with unstable resting potential ○ Smaller than other cardiac muscles Follower cells – pick up depolartization wave via gap junctions and transmit it Purkinje fibers – see above and ○ Lighter cells due to less myofibrils, large perinuclear space, no T-tubules, reduced sarcoplasmic ret. ○ Lots of gap junctions for impulse transfer Blood Vessels Types ○ Three major types and all three types have three subgroups ○ Arteries Elastic Arteries - characterized by elastic lamellae ○ Funtion – maintain blood pressure within vessels during diastole ○ Large lumen, relatively thin wall, numerous elastic laminae ○ Largest, ‘conducts blood’, Ex. Aorta, brachiocephalic, etc. Muscular Arteries - characterized by thick muscular wall ○ Function – regulate flow to different regions of the body as needed ○ Round lumen, prominent internal elastic layer, thick tunica media ○ Ex. Brachial, radial, ulnar, etc. Arterioles - characterized by smooth muscle layer 1-3 cells thick ○ Function – regulate blood flow into capillary bed ○ Looks like a small muscular artery ○ Microvascular Bed Arterioles & Venules Central Channel – a preferential channel through the capillary bed Capillaries – thin walled for rapid exchange ○ Veins Venules – small veins that accompany arterioles Medium Veins – thin walled vessels that run with muscular arteries ○ only vessels that contain valves ○ Tunica media reduced, thickness of wall reduced, lumen is large and irregular ○ Ex. Brachial, radial, ulnar Large Veins – large, low pressure, thin-walled vessels ○ Adventitia is the thickest portion of the wall ○ Ex. Inferior and superior vena cava, brachiocephalic vein General Structure ○ All are endothelia-lined tubes ○ Tunica Intima – innermost layer, lined by endothelium (simple squamous epithelium) Made of ○ Endothelial Lining – inner, has basement membrane ○ Subendothelial CT – longitudinally arranged ○ Internal Elastic Lamina – fenestrated elastic sheet Atherosclerosis – affects tunica intima, characterized by fatty streaks and plaques ○ Lesions of thickened tunica intima and proliferation of SMC and foam cells ○ Tunica Media – made of: Circularly oriented smooth muscle cells that reduce size of the lumen Elastic and collage fibers External Elastic Lamina – separates tunica media from tunica adventitia In capillaries, the tunica media is basically ‘replaced’ by pericytes ○ Tunica Adventitia – made of: Dense irregular CT, nerves and Vaso Vasorum – small vessels that supply the wall of large blood vessels Specifics of Each Blood Vessel Type ○ Diagnostic Characteristics = different color Arteries Tunica Intima - Endothelium - Subendothelial CT - Internal Elastic Lamina Elastic Artery Muscular Artery Arteriole Thin Thickened Difficult to see Difficult to see Difficult to see Scalloped, prominent Difficult to see Difficult to see Transient Tunica Media - Smooth Muscle - Elastic & Collagen Fib - Ext. Elastic Lamina Tunica Adventitia In between elastic sheets 40-70 layers of elastic sheets (maintains BP) Most ext. elast. Sheet 5-20 layers Scattered 1-3 layers Yes Relatively thin, Also has elastic fibers Yes No No Minimal - CT Dense irregular - Vaso Vasorum Yes No ○ Metarterioles – supply capillaries Have discontinuous smooth muscle cells that regulate blood flow into capillary beds Veins Venules Larger than arterioles Irregularly shaped lumen Where WBCs exit Tunica Intima - Endothelium - Subendothelial CT - Internal Elastic Lamina Tunica Media - Smooth Muscle - Elastic & Collagen Fib - Ext. Elastic Lamina Tunica Adventitia - CT - Vaso Vasorum - Smooth Muscle Absent Medium Vein Larger than musc. art. Irregularly shaped lumen Have valves Large Vein Thin walled Thin Thin Not well defined Thin Just a few No Thin Few circularly oriented No Thickest layer Thickest layer Penetrate deeper Longitudinally-oriented smooth muscle ○ Note – large veins need the vaso vasorum to penetrate deeper because the blood in the vein is deoxygenated and thus need more oxygen from other sources ○ Valves on the Medium Veins Protrusions of the tunica intima that are still covered by endothelium Valve Sinus – dilation of wall behind leaflet Usually found in extremities to help return blood to heart Skeletal muscle and arterial pulsation helps move the blood Prevents back pressure on capillaries, prevents back flow in veins Vericose Veins – large tortuous, usually superficial veins ○ Caused by excess pressure in veins resulting in distension and dilation of walls resulting in lengthening and tortuous appearance ○ Leaflets can no longer meet in center to prevent backflow ○ Microvascular Bed Made of arterioles, true capillaries, central channel, venules and arteriovenous shunts Arteriole – terminates in capillary bed ○ Single smooth muscle cell forms tunica media ○ Supplies either the metarteriole or the arteriovenous shunt Central Channel – a direct way through the capillary bed ○ Metarteriole – beginning portion of central channel which controls blood flow through the capillary Has scattered SMCs Opens into true capillaries ○ Thoroughfare Channel - distal end of the central channel Does not have SMCs Drains capillaries into venules Arteriovenous Shunt (AV Shunt) – a way to bypass capillaries, direct link from arterioles to venules ○ Has 2-3 layers of SMCs Capillaries ○ Basically just a tube of endothelial cells (simple squamous epithelium) Diamond shaped, thin and flat, nuclear bulges, marginal folds overlap upstream edge ○ Has basal lamina ○ Instead of tunica media there are occasional pericytes ○ Greatest concentration in myocardium ○ Capillaries also make and excrete stuff ○ Best way to distinguish subtypes is by which tissue they are in ○ Types Continuous Capillary – basal lamina is continuous with no pores or fenestrations Found in muscle, CT and gut Fenestrated Capillary – basal lamina is continuous but the endothelial cells have fenestrations (holes through the cytoplasm) Found in endocrine glands, intestinal villi, exocrine pancreas Discontinuous Capillary (Sinusoids) – basal lamina is discontinuous (does not cross gaps between cells) Large gaps between cells (allows easy transport), irregular shape Found in spleen, liver, bone marrow, lymph nodes ○ Methods of transport across epithelium Diffusion Transcytosis – pinocytotic vesicles form, are non-selective Receptor-mediated transport – also into vesicles, is selective Direct channels from fused vesicles ○ Secretions of Capillary Endothelial Cells Help form basal lamina (secretes stuff for that) Produces signals for extravasation and diapedesis (p-selectin, PAF, CAMs) Releases substances that affect vascular tone Vasoconstrictors – endothelin I Vasodilators – nitrous oxide, etc. Produces clotting factors Von Willebrand Factor – a glycoprotein used in coagulation of platelets Von Willebrand’s Disease – lack of the factor, genetic, prolonged coagulation ○ Lymphatic System Function – removes excess interstitial fluid from extracellular space, filters it then returns it to cardiovascular Second system of circulatory system Ducts Thoracic duct collects lower and left part of body ○ Cisterna chyli – beginning of thoracic duct, starting at diaphragm ○ Drains into left subclavian vein merging with left internal jugular vein Right lymphatic duct – drains right, upper quarter of body ○ Drains into right subclavian vein Vessels start as blind ended lymphatic capillaries → Drain into larger vessels with valves → into lymph nodes → return to blood vascular system Can differentiate from blood vessels because ○ No blood in lumen ○ Incomplete basal lamina ○ Thin wall and anchoring filaments (may be visible) Cardiac Development ○ Objectives Define and describe endocardial tube, myoepicardial mantle and derivatives, cardiac jelly, endocardial cushions. Describe formation of the mesodermal germ layer, cardiogenic plate and embryonic foldings. Describe early development of the primitive heart tube. Describe and discuss the relationship between sinus venosus, primitive atrium, primitive ventricle, bulbus cordis, and truncus arteriosus. Define aortic sac and explain its relationship tthe truncus arteriosus and aortic arches. Explain the process of looping of the heart. Describe partitioning of the atrioventricular canal, primordial atrium and ventricle. Describe partitioning of the bulbus cordis and truncus arteriosus. Describe development of the cardiac valves and conducting system of the heart. Describe the normal fetus blood circulation and the changes that occur when a newborn switches from fetal tadult-type blood circulation. ○ Basic Steps of Cardiogenesis Bilateral Heart Primordia Primitive Heart Tube Heart Looping Atrial and Ventricular Septation Outflow Tract Septation – this part requires neural crest cells, all others only require splanchnic mesoderm (which is derived from lateral plate mesoderm) ○ Bilateral Heart Primordia Lateral plate mesoderm → splanchnic mesoderm → precardiogenic mesoderm (first exists rostral to oropharyngeal membrane) Precardiogenic mesoderm exists on either side of the primitive gut Differentiates into myocardial primordium (closest to pericardial coelom), cardiac jelly (which becomes the subendocardial tissue), and the endocardial primordium (closest to primitive gut) Each endocardial primordium gets surrounded by cardiac jelly and makes a primitive heart tube Two blobs of this stuff then meet in the middle and in doing so partition off the foregut Eventually each heart tube is connected by vessels and then fuses, swells and begins to beat ○ This creates the primitive heart tube The pericardial coelom follows everything and becomes visceral pericardium and parietal pericardium ○ Primitive Heart Tube Original Structure End Structure Aortic Sac Aorta and Pulmonary Trunk Bulbis Cordis (truncus and conus) RV Primitive Ventricle LV Primitive Atria Common Atria Sinus Venosus RA ○ Heart Looping - Heart tube folds like an S with the sinus venosus coming up behind the bulbis cordis See picture ○ Atrial and Ventricular Septation AV Septation Atrioventricular Cushions – portions of the subendocardial epithelium (derived from cardiac jelly) thicken and help divide the common atrium from the common ventricle Original connection between future ventricles and atria is on the ‘left’ side of the looped heart tube, but it needs to get to the center so it moves there and as it does the future right ventricle gets larger and more symmetric with the future left ventricle As things grow and migrate the connection between the common atria and common ventricle splits (one for right side, one for left side) Inflow Tract Formation Sinus venosus flows directly into common atria at the sinoatrial orifice which is in the middle of the common atrium, but eventually migrates to the future RA Sinus venosus has two horns and each receives blood from a vitelline, umbilical and common cardinal vein ○ ○ ○ ○ Original Structure End Structure Right Common Cardinal Vein Superior Vena Cava Right Vitelline Vein Inferior Vena Cava Right Umbilical Vein nothing Left Sinus Horn Coronary Sinus Sinoatrial orifice flanked by valves making septum spurium? Atrial Septation Septum primum froms from top and divides common atrium into right and left ○ Ostium primum – small hole at bottom between septum primum and division of ventricles Septum primum eventually grows to fill this ○ Ostium primum – hole forms in top of septum primum Septum secundum forms in right atrium (right next to septum primum) ○ Foramen ovale – septum secundum doesn’t go down all the way and forms this In adult ○ edges of fossa ovale (was foramen ovale) are made by septum secundum ○ edges of valve of the fossa ovale are made by septum primum Things in the right atrium ○ Sinoatrial orifice disappears and end structures of sinus venosus connect directly to RA ○ Crista Terminalis – union of the right appendage and right atrium ○ Sinus venarum – smooth tissue in between crista terminalis and remnants of sinoatrial orifice Ventricular Septation Muscular Septum – forms from bottom and does not completely separate ventricles Membranous septum completes the septation and is continuous with outflow septation Complete by 8th week Outflow Tract Septation Aortic Sac connected directly to common ventricle A membranous septum forms in a spiral fashion and creates base of aorta and pulmonary trunk and extends to complete the septation of the ventricles Neural Crest Cells are required for this They also provide the elastic fibers which are required for the resiliency of the aorta and pulmonary trunk Development of Valves AV Valves Derived from growing atrioventricular cushions which bring myocardium with them. Eventually portions of this myocardium are reabsorbed and the remaining forms muscular cords (which eventually become chordae tendinae and papillary muscles) AV valves form from cushions being remodeled Semilunar Valves Neural crest cells induce endocardial cushion cells to form semilunar valves ○ Semilunar valves still form if no neural crest Innervation of the Heart Comes from neural crest cells Parasympathetic and sensory nerves from vagus Sympathetic postganglionic fibers come from sympathetic trunk Fetal Circulation Pressure in pulmonary trunk and lungs is very high, that is why blood is shunted to aorta via ductus arteriosus Deoxygenated blood goes to placenta and comes back via the umbilical vein From umbilical vein it goes to liver where there is a ductus venosus which can be regulated to decide how much blood the fetus will get Introduction tthe Autonomic Nervous System ○ Objectives Define: Somatic efferent Somatic afferent, Visceral efferent, Visceral afferent, Effector ○ ○ ○ ○ Compare the structural differences between the somatic and the autonomic components of the peripheral nervous system. Compare the sympathetic and parasympathetic divisions of the ANS. How are these twsimilar? How are they different? Be able tdiagram a “typical” visceral efferent path for both the sympathetic and parasympathetic division of the ANS. List four possible terminations for the preganglionic sympathetic fiber. What is a pelvic splanchnic nerve? Describe the course and termination for a pelvic splanchnic. Somatic parts of the CNS are derived from somites Somatic afferent – receives information Somatic efferent – sends information Autonomic Nervous System – controls activity of involuntary muscle (smooth muscle, cardiac muscle, glands) Also called visceral or splanchnic Visceral afferent – sensory, receives information from organs Visceral efferent – involuntary, supplies smooth muscle, cardiac muscle, exocrine glands (glands that secrete) Divisions ○ Sympathetic – ‘fight or flight’ ↑ HR, ↑RR, dilation of iris, vasoconstrictors in core, sweat glands ○ Parasympathetic – ‘rest and digest’, ↑ digestion, ↓HR, ↓RR, ↑lacrimal glands (tears), ↑mucus glands ○ Enteric – only in wall of gastrointestinal tract, self sustaining system Similarities between sympathetic and parasympathetic ○ Both are motor/visceral efferent ○ Both innervate effectors (smooth muscle, cardiac muscle, glands) ○ Both use 2 neuron chain – two motor neurons interrupted by an autonomic ganglion Preganglionic neuron – always within the CNS Postganglionic neuron – all reside within an autonomic ganglion Sympathetic Parasympathetic Origin of preganglionic Lateral horn T1-L2 Brainstem – CN 3,7,9,10 neuron Lateral Horn – S2-S4 Location of postganglionic Paravertebral Ganglia or Named ganglia for CN 3,7,9 Terminal Ganglia for CN 10 and S2-S4 (autonomic) ganglion Prevertebral Ganglia Neurotransmitter Pre – Acetylcholine Pre – Acetylcholine Post – Norepinephrine Post – Acetylcholine Terminal Distribution Organs Organs BV in core Mucus and lacrimal glands Smooth muscle of skin Sympathetic Division ○ Remember that every peripheral nerve going to the skin will have sympathetic innervation (ie radial nerve) ○ T1-L2 Lateral horn → ventral root → white ramus (myelinated) → paravertebral ganglia (where the synapse occurs) → gray ramus (unmyelinated) → dorsal and ventral rami Note – paravertebral ganglia AKA sympathetic chain ganglia or sympathetic trunk ○ Other than T1-L2 Same pathway, but travels in an interganglionic segment and does not synapse in a paravertebral ganglia until it travels to the vertebrae that it will exit from T1-T4 ascend, T11-L2 descend This means that white rami are only associated with T1-L2 (14), while grey rami are associated with every vertebral level ○ Paravertebral Ganglia There are only 22 of them Cervical Ganglia – superior, middle and inferior Thoracic, lumbar and sacral ganglia ○ In the sacral ganglia, there is the ganglion impar which is where the two sympathetic chains meet ○ Getting from Paravertebral Ganglia to the Effectors Thoracic Viscera – Comes from T1-T4 ○ Splanchnic nerve comes directly from paravertebral ganglion (where a synapse occurs) to effector Abdominal and Pelvic Viscera – comes from T5-L2 ○ Splanchnic nerve comes from paravertebral ganglion, but does not synapse there. Instead it synapses in a prevertebral ganglia located near the abdominal portion of the aorta ○ After the prevertebral ganglia the nerve travels with blood vessels to the effector Adrenal Medulla ○ Goes through both the paravertebral ganglia and the prevertebral ganglia and does not synapse there, instead it synapses in the adrenal medulla ○ This makes sense because the adrenal medulla is neurosecretory and secretes norepinephrine, just like a postganglionic sympathetic neuron and creates a systemic sympathetic response ○ Splanchnic Nerve – portion of ANS between the paravertebral ganglion and the prevertebral ganglion or the effector Parasympathetic Division ○ CN X uses terminal ganglia on organs of thorax and upper abdomen Travels directly from brain to terminal ganglia ○ Lateral Horn S2-S4 uses terminal ganglia on organs of lower abdomen and pelvis Travels through ventral ramus via pelvic splanchnic nerve to terminal ganglia ○ Terminal Ganglia – either in or on the wall of the organ If used, this is where the postganglionic nerve starts Remember that sympathetics also go through the dorsal and ventral rami to innervate the skin Lymphatic System ○ Objectives Be able tidentify the tissues and cells of the lymphoid system. Know the functions of the various cells of the lymphoid system. Be able ttrace cells of the lymphoid system within the body. Know the functions of the tissues of the lymphoid system. Be able tdistinguish cellular from humoral immunity. Be able tdescribe basic immune responses. Compare and contrast structure-function relationships between the lymphoid organs. ○ Organs Red Bone Marrow Encapsulated in CT – thymus, spleen, lymph nodes Diffuse lymphatic tissue – tonsils, adenoids, peyer’s patches, appendix Primary lymphatic organs – provide environment for stem cells to divide & mature into B and T lymphocytes Bone marrow and thymus Secondary lymphatic organs – site where most immune responses occur Lymph nodes, spleen, lymphatic nodules ○ Functions Non-Specific – response is always the same Surface protection Acute Inflammation – organized tissue response mediated by neutrophils Drain excess interstitial fluid and plasma protein from tissue spaces Transport of dietary lipids and vitamins from GI tract (then returned to blood) Facilitate Immune Response Specific and targeted to invading organisms Depends on ability to recognize self from non-self Immune system activated to neutralize or destroy antigen ○ Immune Reactions Cellular Immunity Humoral (antibody-mediated) Immunity Mediated by T lymphocytes Mediated by B lymphocytes Cells react to intracellular pathogens Antibodies destroy extracellular pathogens - kills fungi, viruses, parasites, cancer, etc - kills bacteria Cells mature in thymus Cells mature in bone marrow Delayed hypersensitivity takes 1-2 days Immediate hypersensitivity No circulating factors found Antibodies in circulation Inflammation at site Long term protection Directly interact with things they kill Lymphocytes Natural Killer Cells (10-15%) – kill things and do not need specific activation T-Cells (65-75%) – cell mediated response ○ Subtypes Helper T-Cells – identified by CD4, makes B-cells and cytotoxic T cells active ○ Destroyed by AIDS Supressor T Cells – don’t memorize Cytotoxic T Cells – identified by CD8, kills stuff B-Cells (5-10%) ○ Type for each antigen ○ Expresses IgM on surface – a receptor used to identify an antigen ○ When activated they become plasma cells (which make the antibodies) Maturation of T and B Cells Both come from stem cells in the bone marrow, but T-cells mature in the thymus (this is where they get their surface proteins (CD4 and CD8)) ○ Encapsulated Lymphatic Structures Surrounded by CT Stroma – framework of tissue made of reticular connective tissue Parenchyma – cells exist in spaces between reticular fibers (lymphocyes, macrophages, plasma cells, etc) Thymus Bi-lobed organ in thymus that becomes fatty with age (but not completely useless) Here T-Cells become immunocompetent, express surface proteins, recognize self from non-self, proliferate Gets rid of T-cells that recognize self Capsule and trabeculae divide it into lobules containing cortex and medulla ○ Cortex – tightly packed lymphocytes and macrophages, more dense than medulla, where self-recognizing T-cells are killed Is isolated from body Type I Epithelial Reticular Cells (ERC) – isolate cortex from body Type II ERC – divide cortex into lymphocyte-filled pockets; forms most of cortex Type III ERC – isolates cortex from medulla Type II and III ERC are antigen presenting cells? ○ Medulla – less tightly packed, only T-cells that don’t recognize self get through and are eventually released from here Type IV ERC – isolates cortex from medulla on medullary side Type V ERC – forms most of medulla Type VI ERC – unknown function, big cells Tolerance ○ Tolerance – ability to recognize self from non-self, established in the Thymus ○ Occurs via anergy (disabling) or via killing immunocompetent cells (which occurs in cortex of thymus) ○ Requires that immune cells recognize MHC and don’t recognize self-peptides 1. MHC Recognition (must occur) ○ Antigen presenting cells display MHC CD4 cells recognize MHC-II CD8 cells recognize MHC-I If they can’t then they are killed 2. Self-Recognition (must not occur) ○ Antigen presenting cells display self antigen → if T-Cell Receptor binds to self-peptide then it is killed Lymph Nodes Only structures that filters lymph Concentrated near mammary glands, axilla, groin, midline and neck Stroma (capsule) made of trabeculae & reticular fibers Parenchyma consists of cortex and medulla ○ Cortex Outer Cortex - B-Cell Domain ○ Has nodules containing active B-cells (plasma cells) called germinal centers Inner Cortex - T-Cell Domain/paracortex High endothelial venules – specialized capillaries for the lymph nodes ○ Lymphocytes enter lymph node through these Follow the Lymph Flow ○ Lymph enters through afferent lymph vessels → goes through subcapsular sinus → to medullary sinus → exits through efferent lymph vessel ○ During this course it leaves the sinuses and gets filtered by cells in the lymph node (esp. cortex) Spleen Filters all of the blood to: ○ Remove old blood cells ○ Mount an immune response in the blood Note – lymph does not enter spleen Between stomach and diaphragm Stroma made of capsule, trabeculae, fibers, fibroblasts Parenchyma made of white pulp and red pulp ○ White Pulp – lymphatic tissue containing lymphcytes and macrophages around branches of splenic artery Peri-arteriolar lymphatic sheath (PALS) - T-cell domain, a bunch of T-cells that surround central arteries in the spleen Marginal Zone Sinuses - B-cell domain, peripheral to the PALS, here B-cells form germinal centers ○ Red Pulp – splenic cords and meshwork of venous sinuses filled with blood Near end of central artery penicillar arterioles branch off into either closed circulation (where the arteriole ends in a sinusoid) or open circulation (where the arteriole just spits out blood) ○ Either way the blood passes through a sheath (a ring of macrophages that eats old RBCs) before Follow the Blood ○ Trabecular artery → central artery → passes through white pulp → ends in red pulp ○ Diffuse Lymphoid Tissue – Lymph Nodes Concentrations of lymphatic tissue not surrounded by a capsule scattered throughout CT and mucus membranes Mucosa Associated Lymphoid Tissue (MALT) – for antigen presentation and phagocytosis ○ In gastrointestinal tract (GALT) – trachea, tonsils, Peyer’s patch (in lumen of GI), appendix Peyer’s Patch – one of the only MALTs with a definitive structure and T & B cell domains ○ Antigen presenting cell (M Cell) on gut lumen can move into Peyer’s patch and help mount immune response ○ In bronchus (BALT) ○ Lymph Circulation Lymph flows in closed-ended tubes There are no lymph pump or lymph-associated muscles. Lymph propelled in vessels by surrounding skeletal muscle Empties into subclavian veins (only direct connection of lymph to blood) Cross-Sections Thoracic Imaging ○ Objectives Identify Structures ○ Heart Shadow – can’t see RV or LA Can see superior vena cava, aortic knob ○ Cross Sections – it is like you are looking at the patient from their feet while they are laying down, ○ ○ ○ ○ ○ ○ Thus right is on the left side of the image T3 – Right brachiocephalic, Left brachiocephalic, Brachiocephalic trunk, left common carotid, left subclavian, esophagus, trachea T4-T5 – Superior vena cava, aortic arch, arch of azygos, trachea begins to bifurcate, esophagus T5-T6 – Superior vena cava, ascending aorta, pulmonary trunk, right and left pulmonary arteries, right and left main bronchus, esophagus, azygos, descending aorta T6 – superior vena cava, right auricle/atrium, right ventricle, aorta, left atrium, esophagus, azygos, descending aorta This one is tricky T7-T8 – right atrium, right ventricle, beginning of ascending aorta, IV septum, interatrial septum, left atrium, a piece of the mitral valve, wall of left ventricle, esophagus, azygos, descending aorta T8-T9 – right dome of the diaphragm, liver, RA, tricuspid, RV, IV septum, LV, coronary sinus!, azygos, descending aorta Congential Heart Defects ○ Objectives List the most commonly encountered congenital cardiac malformations. Classify the congenital cardiac malformations according tstructural anomalies. Describe the development errors that take place in the heart resulting in left-to-right shunt. Describe the development errors that take place in the heart resulting in right-to-left shunt. Describe the development errors that take place in the heart causing anomalies of the outflow tract. Describe and compare the clinical consequences of: Patent Ductus Arteriosus Coarctation of Aorta Transposition of Great Arteries Atrial Septal Defect Ventricular Septal Defect Tetralogy of Fallot Persistent Truncus Arteriosus Congentical heart defects don’t have to result in alteration of heart function Caused by genes, environmental factors, maternal ingestion of toxins, viruses (Rubella) Ventricular septal defect is the most common one Cyanosis – when circulating blood has a lot of reduced hemoglobin Starling law? – if excess pressure in one chamber of the heart then eventually all will get higher pressure If constriction ahead then you will have hypertrophy behind If leaky valve ahead then you will have dilation behind? ○ Abbott Classification Acyanotic – does not have an abnormal communication between the 2 circulations Cyanotic – permanent R→L shunt (deoxygenated blood gets into body circulation) Cyanotic Tardive – initial L→R shunt with late reversal of flow to R→L Only Tetralogy of Fallot ○ Shunt Classification Initial L→R Shunt – VSD, ASD, PDA, PTA R→L Shunt – Tetralogy of Fallot No Shunt – TGV, CoA (sometimes) Note – pure TGV is incompatible with life, only another defect will save them ○ Ventricular Septal Defect Most common congenital heart defect Types Membranous VSD – most common, membranous septum doesn’t fully form Muscular VSD – part of muscular septum disappears Symptoms Small VSD – may remain asymptomatic Larve VSD – can develop congestive heart failure due to left heart volume overload Holosystolic mumur ○ ○ ○ ○ ○ The lungs are the main problem because too much blood goes to RV and it is sent to the lungs L→R shunt causes too much blood in lungs, but no cyanosis X-Rays Enlarged pulmonary vessels LA so large you can see it in heart shadow Pulmonary trunk visible in heart shadow ○ Atrial Septal Defect Types Ostium secundum defect - excessive resorption around the foramen segundum Ostium primum defect – ostium primum doesn’t close Sinus Venosus defect – blood goes through ostium primum and segundum at top Can also be caused by hypoplastic (too little) growth of the septum segundum? More common in females Symptoms Most infants are asymptomatic, often detected as murmur at school age Adults can develop palpitations. This is because part of conduction system is in interatrial septum and it is missing L→R shunt causes too much blood in lungs, but no cyanosis X-Rays Heart shadow shows large pulmonary trunk and small aortic notch Pulmonary arteries can get big too ○ Patent Ductus Arteriosus Can be life-threatening or life-saving More common in females Higher risk – premature infants, maternal rubella Symptoms If small – asymptomatic If large – gets symptoms of congestive heart failure ○ Cyanosis of the feet ○ no cyanosis in upper extremities Continuous murmur L→R shunt that causes cyanosis in lower extremities X-Ray – can have hypoplasia of the aorta How Ductus Arteriosus Closes Fetal Circulation – prostaglandins and low O2 keep ductus arteriosus open Neonatal Circulation – high O2 prompts bradykinin to be released and this constricts ductus arteriosus If ductus is only thing keeping baby alive then give prostaglandins to keep it open If ductus doesn’t close when it should then give indomethicin (a prostaglandin antagonist) ○ Coarctation of the Aorta Hypertension in the upper body Blood flow to lower extremities may be diminished Types Preductal Coarctation ○ If ductus arteriosus closes then congestive heart failure shortly after birth ○ If ductus arteriosus remains open Shunt is R→L Upper half of body will be perfused with oxygen ○ Will have high pressure here Lower half of body will be cyanotic (because it will get must of its blood from pulmonary trunk via ductus arteriosus ○ Will have low pressure here Postductal Coarctation ○ If small then not much problem ○ If big then newborn will develop congestive heart failure from pressure overload and die ○ If ductus arteriosus closes then no cyanosis No shunt Upper half of body will have high pressure and left internal thoracic will enlarge, intercostal arteries will cause rib notching because they get bigger and beat away at the bones ○ If ductus arteriosus remains open then: L→R shunt ?? Causes Preductal – anomaly resulting in hypoplastic development of aorta Postductal – muscular ductal tissue gets into aorta during fetal life, when ductus closes, so does that part of aorta ○ Tetralogy of Fallot Rightward displacement of the infundibular septum (pulmonary exit) resulting in unequal division of pulmonary and aortic outflow For anatomical anomalies Ventricular septal defect due to septum misalignment Subvalvular pulmonic stenosis because of obstruction of the conus arteriosus (path from RV to pulmonary artery) ○ Makes the shunt R→L Aorta is moved to the right so that it receives blood from both ventricles Acquired anomaly - Right ventricular hypertrophy due to high pressure load of pulmonic stenosis Symptoms Dyspnea or ‘spells’ (getting cyanotic) on exertion (crying, feeding, etc) Convulsions due to cerebral hypoxemia Often a little cyanotic Systolic murmur Cyanosis can be alleviated by ‘squatting’ ○ Venous system → trap blood in legs → ↓ blood return to RA → ↓ blood to RV → ↓ deoxy blood to R→ L shunt → decrease cyanosis ○ Arterial system → ↑ arterial resistance → ↑ aortic pressure → ↑ LV pressure → ↑ flow in aortic valve → ↑ oxygenated blood in aorta → decrease cyanosis X-Ray – slightly more prominent aortic arch Boot heart due to largeness ○ Transposition of the Great Arteries Great vessels (aorta and pulmonary) arise from the opposite ventricle Cause unknown, but could be due to failure of aorticopulmonary septum to spiral Deadly outside of uterus unless another congenital defect, ASD, VSD, PDA is present Not deadly as a fetus because ductus arteriosus is still present X-Ray – large egg shaped heart ○ Persistent Truncus Arteriosus Absent or incomplete partitioning of the truncus arteriosus by the spiral septum Could be because of neural crest problem Right and left ventricles give blood to aorta and pulmonary trunk Blood can go mainly to pulmonary trunk, if so then heart failure due to pressure overload Presence of cyanosis is dependent on which ventricle is stronger? Will often end up with cyanosis?