Region 18: Pelvis Bony Pelvis --pelvis major/false pelvis: large, bowl
advertisement

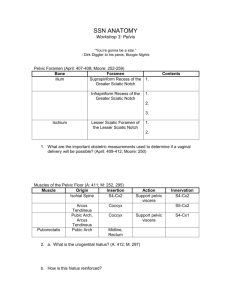
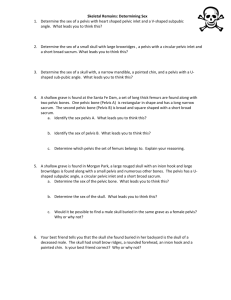
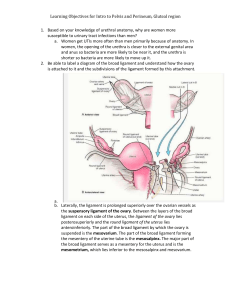
Region 18: Pelvis Bony Pelvis --pelvis major/false pelvis: large, bowl shaped superior portion --pelvis minor/true pelvis: smaller, cone shaped inferior portion --Hip/innominate bones *2 hip bones each the result of the fusion of the ilium, pubis, and ischium --Articulations of the Pelvis a. sacroiliac joint *ventral sacroiliac ligament *interosseous sacroiliac ligament (strongest ligament in the body) *dorsal sacroiliac ligament b. pubic symphysis *cartilaginous jt. b/w 2 pubic bones *fibrocartilaginous interpubic disc c. pelvic joints vertebral column *iliolumbar ligament *sacrotuberous and sacrospinous ligaments --Pelvic Basin a. pelvic brim: made up of superior aspect of symphysis pubis, crest of the pubic bone, pectin pubis, arcuate line of the ilium, ala of the sacrum, and sacral promontory b. pelvis major/false pelvis: lies above the pelvic brim c. pelvis minor/true pelvis: lies below the pelvic brim d. pelvic outlet: inferior aperture of the true pelvis --Pelvic Apertures a. obturator foramen *nearly closed by a thin aponeurosis (obturator membrane) *the membrane is incomplete at the obturator canal (an opening for the exit/entrance of the obturator nerves and vessels) b. greater sciatic notch *converted into a foramen (greater sciatic foramen) by the sacrospinous ligament *filled with piriformis muscle tendon, some nerves of the sacral plexus, some branches of the internal iliac vessels c. lesser sciatic notch *converted into a foramen (lesser sciatic foramen) by the sacrospnous and sacrotuberous ligaments *structures that pass through it: obturator internus muscle (exits the pelvis into the gluteal region), internal pudendal vessels and pudendal nerve use it for communication with the ischiorectal fossa Muscles of the Pelvis --Piriformis muscle *O: anterior aspects of sacrum, leaves through greater sciatic foramen *I: superior border of greater trochanter of femur *Act: forms a muscular bed for the sacral plexus, lateral rotator of the thigh --Obturator Internus Muscle *O: internal surface of margins of the obturator foramen and the obturator membrane (tendon passes through lesser sciatic foramen) *I: medial surface of the greater trochanter *Inn: nerve to obturator internus *Act: laterally rotates the thigh --Levator Ani Muscles *O: from tendinous arch (arcus tendinous) formed by a thickening of the pelvic fascia of the obturator internus muscle *I: in central perineal tendon (perineal body), anococcygeal raphe, and coccyx (after muscle converges in midline) *Subdivisions: puborectalis, pubococcygeus, and iliococcygeus mm. --Coccygeus Muscle (aka ischiococcygeus muscle) *O: ischial spine *Act: support the pelvic contents and are important for micturition, and defecation Contents of the Pelvis --Vesticular compartment/anterior compartment a. Urinary bladder *apex: hass attachent to median umbilical ligament (urachus remnant) *superior surface: flattened when the bladder is empty and lies w/I the pelvis, when bladder is full, surface is dome shaped *base: its superior portion receives the two ureters posterolaterally *neck: lowest portion and opens into urethra, in male the neck of the bladder rests on the prostate gland b. Ureters *in female they cross immediately inferior to the uterine a. --Genital compartment/middle compartment a. Male *seminal vesicles: their ducts are joined by the vas deferens to form the ejaculatory duct *2 ductus deferens: leave the deep inguinal rings and cross the external iliac vessels to enter the pelvis b. Female *vagina: situated b/w the bladder and urethra anteriorly and the rectum and anal conal posteriorly, the anterior wall of the vagina receives the cervix of the uterus, its posterior fornix reaches the peritoneum in the depths of the rectouterine pouch *Uterus: normally flexed forward/anteflexion so the uterus may rest on top of an empty bladder, from above to downwards the uterus consists of a fundus, body, cervix *ovary: small ovoid body with the broad ligament and capped laterally by the fimbria of the uterine tubes, its attachment to the uterus is via the fibrous ovarian ligament *uterine/Fallopian tubes: continuous with the uterus at the junction of its fundus and body, they end with the finger like projections called fimbria, each tube is narrowed medially (isthmus) and expanded laterally into the ampulla and lateral to that the infundibulum with the fimbria (oocyte is usually fertilized with sperm in the ampullary region) --Rectal Compartment/posterior compartment a. rectum: segment after sigmoid colon *begins in front of S3, ends at the pelvic diaphragm as the anal canal Pelvic Peritoneum --peritoneum of the pelvic cavity is continuous with that of the abdomen, some pelvic organs are suspended by a double layer’s of peritoneum called mesenteries and ligaments --Peritoneum over the genital/middle compartment *Male: organs are relatively small and d/n project into the pelvic cavity *Female: organs (uterus, uterine tubes, and ovaries0 project markedly into the pelvis and associated with mesenteries and ligaments that span the pelvic cavity in the coronal plane posteriorly hold a ball/ovary in each hand as your arms are extend, drape a sheet/peritoneum over whole body arms and hands, these two laters create the broad ligament *parts of the broad ligament which suspend individual organs a. mesometrium: mesentery at the sides of the uterus b. mesosalpinx: mesentery of uterine tubes c. mesovarium: mesentery of the ovary d. suspensory ligament of the ovary: peritoneal fold created laterally to ovarian vessels *Included within the braod ligament and attaching to the uterus a. fibrous ovarian ligament posteriorly b. round ligament of the uterus anteriorly *cardinal ligament (of Mackenrodt or transverse cervical ligament) this and pelvic diaphragm are primary support of the uterus and cervix --Peritoneum over rectal/posterior compartment *posteriorly it envelops and suspends the sigmoid color from the posterior pelvic wall (sigmoid colon) *the rectum d/n have mesentery, although it is covered on its anterior *Female: has posterior recess b/w rectum and bladder called rectouterine recess (pouch of Douglas) Nerve Supply of the Pelvis --Sympathetic contributions a. lumbar sympathetic trunk: continues into the pelvis and the trunks of each side join together in front of the coccyx to form the ganglion impar b. sacral splanchnic nerves (enter plexus) --Parasympathetic *S2, S3, S4 contribute parasympathetic preganglion fibers (pelvic splanchnic nerves Internal Features of Visceral Organs --Urinary bladder a. the wall consists of smooth muscle, the thickness decreases as the organ fills to capacity (about 500mL) b. the mucosa becomes rugose when the organ empties, except for the region of the trigone *a triangular area on the posterior wall b/w the ureteric orifices and the internal urethral orifice --Female urethra a. fibromuscular tube 3-4 cm long b. external urethral (orifice) positioned b/w the clitoris and the vaginal opening --Male urethra a. it is a fibromuscular tube about 20 cm long b. sections of the male urethra have different names *prostatic urethra: descends through the prostate gland --urethral crest = a narrow longitudinal ridge on the posterior wall which indents the lumen --prostatic sulci/sinuses: groove on each side of the crest where ducts from the prostate gland open --seminal colliculus: rounded eminence at midpoint o the urethral crest --prostatic utricle: small slit in the seminal colliculus that leads into a blind ouch that is the male homologue of the uterus and vagina *membranous urethra: travels through the urogenital diaphragm *penile/spongy urethra: enters the bulb of the penis, traverses the corpus spongiosum and terminates at the glans as the external urethral meatus c. urethra receives secretions from prostatic ducts, ejaculatory ducts, and ducts of the bulbourethral glands/Cowper’s glands --Prostate gland a. an accessory reproductive gland b. surrounds the urethra c. numerous prostatic ducts empt into prostatic urethra that also is pierced by the ejaculatory ducts --Seminal Vesicles a. it joins the ampulla of the ductus deferens to form the ejaculatory duct, that passes through the substance of the prostate to empty into the prostatic urethra --Vagina a. fibromuscular tube b. between the wall of the bagina and cervix are anterior fornix, lateral fornix, and posterior fornix (the largest) --Uterus a. thick walled muscular organ b. receives the uterine tubes superiorly c. constricted apex is called the isthmus (inferiorly) d. in cervix, cavity continues as the canal of the cervix and has at either end an internal os and external os --Rectum a. internally, it is marked by three folds called transverse rectal folds --Anal Canal a. anal columns: longitudinal folds of the mucosa and submucosa caused by the veins in the area, at the lower end of the anal columns are transverse folds connecting the columns called anal valves and behind these are anal sinuses *below the valves is the pectin/pectinate line or intermediate zone of the anal canal, this area marks the division of the blood supply, venous drainage, and nerve supply Blood Supply of the Pelvis --the pelvis is supplied by branches of the internal iliac a. --internal iliac has posterior parietal, anterior parietal, and visceral branches a. Posterior Parietal branches *iliolumbar artery *lateral sacral artery *superior gluteal artery: usually passes b/w lumbosacral trunk and S1 (above piriformis m.), enters gluteal region via greater sciatic foramen *inferior gluteal artery: usually passes b/w S2 and S3 (below piriformis m.), enters gluteal region via greater sciatic foramen b. Anterior Parietal branches *obturator artery: may arise from inferior epigastric a. (accessory obturator a.) *internal pudendal artery: leaves pelvis through greater sciatic foramen, reenters pelvis via lesser sciatic foramen to supply the perineum c. Visceral branches *middle rectal aa. *uterine and vaginal aa. Sacral Plexus --formed on anterior surface of piriformis m. by VPR L4,5 and S1,2,3,4 --VPR are split into anterior and posterior divisions --sciatic nerve has 2 parts a. common peroneal: made up of entirely fibers from posterior division b. tibial part: consisting of fibers from anterior divisions