TR Oral Flash Cards for Oxygen Transport Acid Base Chemistry
advertisement

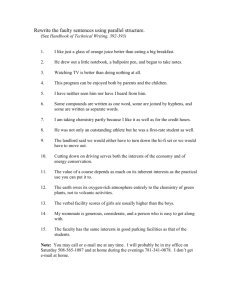
O2 Transport & Acid Base Chemistry State the two ways Oxygen is carried in the blood, explaining where each occurs. Dissolved in plasma Combined with hemoglobin Define Henry’s Law. Weight of gas dissolving in liquid is proportional to the partial pressure of a gas Define Graham’s Law. Rate of diffusion of a gas is directly proportional to its solubility coefficient and inversely proportional to the square root of its density. O2 Transport & Acid Base Chemistry CO2 is ____ times more diffusible than O2. 20 CO is ______ times more diffusible that O2. 200 What is Hemoglobin’s affinity for CO as compared to that of O2? Hgb’s affinity for CO is 200 times more than for O2. O2 Transport & Acid Base Chemistry How would you find the amount of dissolved O2 in 1 ml of plasma? 0.003 x PAO2 True or False: The oxygen in hemoglobin exerts a partial pressure. False How do you calculate the amount of oxygen combined with hemoglobin? 1.34 x Hgb x SaO2 O2 Transport & Acid Base Chemistry True of False: The oxyhemoglobin dissociation curve is sigmoidal due to Hgb affinity for O2 at each of 4 binding sites True True or False: In the steep portion of the oxyhemoglobin dissociation curve, minimal changes in PO2 will cause minimal changes in saturation and total O2 content False – in the steep portion of the curve, minimal changes in PO2 will cause drastic changes in saturation and total O2 content What P50? P50 is where Hgb is 50% saturated with O2 and is normally a PaO2 of 27 mmHg O2 Transport & Acid Base Chemistry A shift of the oxyhemoglobin dissociation curve to the right causes what? A decreased affinity for O2, resulting in decreased saturation but increased O2 to tissues What factors will cause the oxyhemoglobin dissociation curve to shift to the right? Increased PCO2 Increased H+ (decreased pH) Increased 2,3, DPG Increased temperature A shift of the oxyhemoglobin dissociation curve to the left causes what? Increased affinity for O2, resulting in increased saturation but decreased O2 to the tissues O2 Transport & Acid Base Chemistry What factors will cause the oxyhemoglobin dissociation curve to shift to the left? Decreased PCO2 Decreased H+ (increased pH) Decreased temperature Decreased 2,3, DPG Describe the Bohr effect. The effect of H+ or CO2 on Hgb affinity for O2 At lungs – PCO2 is low – increased affinity for O2 At tissues PCO2 is high decreases affinity for O2 Give the formula for total O2 content. CaO2 = (0.003 x PaO2) + (1.34 x Hgb x SaO2) O2 Transport & Acid Base Chemistry Give three causes of hypoxemia. 1. Decreased alveolar oxygen tension 2. Alveolar hypoventilation 3. Decreased hemoglobin saturation 4. V/Q abnormalities – intrapulmonary shunting Give two physiologic responses to hypoxemia. Increased ventilation Increased cardiac output Define hypoxemia. Deficiency of oxygen in the arterial blood. O2 Transport & Acid Base Chemistry What is the alveolar air equation? PAO2 = FIO2 (PBar - PH2O vapor) - PaCO2 RQ What is an intrapulmonary shunt? Blood going from the right to left heart without oxygenation. Name the four types of hypoxemia. Hypoxic/Ambient Anemic/Hemic Stagnant/Circulatory Histotoxic O2 Transport & Acid Base Chemistry Define Hypoxia. Decreased oxygen to the tissues. Describe hypoxemic hypoxia. PaO2 is decreased (high altitudes) Describe anemic hypoxia. Decreased Hgb or the inability of Hgb to accept O2 (CO poisoning) O2 Transport & Acid Base Chemistry Describe stagnant hypoxia Heart unable to deliver oxygenated blood to tissues (Low C.O.) Describe histotoxic hypoxia. Cells are unable to accept or use oxygen (cyanide poisoning) What is the result of hypoxia? Anaerobic metabolism O2 Transport & Acid Base Chemistry Define the Alveolar-Arterial Oxygen Difference P(A-a)O2? Measurement of the pressure difference between the alveoli and the arterial blood. Used to estimate the percent of intrapulmonary shunt. What is an increased P(A-a)O2 an indication of? Respiratory defects in oxygenation diffusion abilities On 100% O2, every 50 mmHg difference in P(A-a)O2 approximates what? A 2% shunt O2 Transport & Acid Base Chemistry What is the normal P(A-a)O2 value on room air? 10 – 15 mmHg How is Carbon Dioxide produced in the body? Produced from normal metabolism How is CO2 carried in the blood? 1. In plasma and red blood cells 2. dissolved, as bicarbonate, & attached to plasma proteins O2 Transport & Acid Base Chemistry How much percent of CO2 is dissolved in plasma? Approximately 8% 80% of CO2 is transported as what? As Bicarbonate 12% of CO2 is transported where? Attached to plasma proteins O2 Transport & Acid Base Chemistry Describe the Haldane Effect. Effect of O2 on CO2 transport At the lungs, PO2 is increased – CO2 is unloaded off Hgb At the tissues, PO2 is decreased – CO2 is loaded on Hgb Define eucapnea. Normal CO2 (35-45 mmHg) Define Hypocapnia. CO2 below 35 mmHg O2 Transport & Acid Base Chemistry Define Hypocarbia. CO2 below 35 mmHg Define Hypercapnia. CO2 above 45 mmHg Define Hypercarbia. CO2 above 45 mmHg O2 Transport & Acid Base Chemistry State the Henderson-Hasselbalch Equation. pH = pk + log (HCO3) (H2CO3) In the Henderson-Hasselbalch Equation, what does pk =? pk= 6.10 In the Henderson-Hasselbalch Equation, what is the value of HCO3? 24 mEq/L O2 Transport & Acid Base Chemistry In the Henderson-Hasselbalch Equation, what is the value of H2CO3? 1.2 mEq/L In the Henderson-Hasselbalch Equation, what is the ratio of HCO3 to H2CO3? 20 to 1 In relation to the HendersonHasselbalch equation, what would a ratio of HCO3 to H2CO3 of 10/1 indicate? acidemia O2 Transport & Acid Base Chemistry In relation to the HendersonHasselbalch equation, what would a ratio of HCO3 to H2CO3 of 30/1 indicate? alkalemia What is the log of 20? 1.3 What is the purpose of buffer systems? To maintain the pH O2 Transport & Acid Base Chemistry Name two buffer systems? 1. HCO3/H2CO3 ratio 2. Hgb 3. Blood phosphates proteins sulfates ammonia groups 60% of the buffer system is made up of what? The HCO3/H2CO3 ratio 30% of the buffer system is made up of what? The Hgb O2 Transport & Acid Base Chemistry What is pH? 1. Negative log of the hydrogen ion 2. Reciprocal of the hydrogen ion concentration What is the entire pH scale from (what to what)? 0-14 What is the normal pH range in blood? 7.35 – 7.45 O2 Transport & Acid Base Chemistry Give normal blood gases for venous blood. (pH, PVCO2, PVO2, HCO3). pH 7.36, PVCO2 46, PVO2 40, HCO3 24 What is the normal O2 Saturation for arterial blood? 95 – 100% What is the normal O2 Saturation for venous blood? 75% O2 Transport & Acid Base Chemistry What is the normal O2 content for arterial blood? 18 – 20 vol% What is the normal O2 content for venous blood? 15 vol% In relationship to compensation, what do the kidneys do? Excrete H+ which ↑ HCO3 to compensate for an ↑ CO2 Excrete less H+ & more HCO3 to compensate for ↓ CO2 O2 Transport & Acid Base Chemistry In relationship to compensation, how long does it take the kidneys to compensate? May take 3 days In relationship to compensation, what do the lungs do? ↓ CO2 to compensate for a ↓HCO3 ↑ CO2 to compensate for a ↑HCO3 In relationship to compensation, how long can the lungs maintain compensation? For a short term only O2 Transport & Acid Base Chemistry What would you pharmacologically administer to increase pH? Sodium bicarbonate (NaHCO3) What would you pharmacologically administer to decrease pH? Ammonium chloride (NH3Cl) How is hypoxemia assessed differently for patients of 60 years old? Subtract 1 mmHg for every year over 60. O2 Transport & Acid Base Chemistry How is hypoxemia assessed for patients with abnormal Hgb? Calculate total O2 content. (Hgb x 1.34 x SaO2) + (0.003 x PaO2) In mild hypoxemia what would the CaO2 be? CaO2 17 vol% 15-17 vol% In moderate hypoxemia what would the CaO2 be? CaO2 15 vol% 12-14 vol% O2 Transport & Acid Base Chemistry In severe hypoxemia what would the CaO2 be? CaO2 12 vol% How is ventilation controlled? 1. Under control of autonomic nervous system 2. Is controlled by central & peripheral chemoreceptors What stimulates the central chemoreceptors? 1. Increased CO2 in CSF causes increased H+ 2. Causes a stimulation of the Inspiratory center O2 Transport & Acid Base Chemistry What is the purpose of the HeringBreuer Reflex? Limits inspiration True or False: Stretch receptors are located in smooth muscle of the large airways only False – in both large and small airways Name the two Peripheral Chemoreceptors? Carotid bodies Aortic bodies O2 Transport & Acid Base Chemistry What stimulates the peripheral chemoreceptors? Respond to hypoxemia What does stimulation of the carotid bodies cause and where are they located? Increases ventilation Located in the bifurcations of the common carotid arteries What does stimulation of the aortic bodies cause and where are they located? Stimulate heart rate Located in the aortic arch