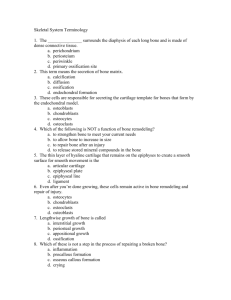
Bone Formation
advertisement

Chapter 8 Part 2: Bone Formation 1. Bone can be formed in two ways, one of which involves the temporary existence of a cartilage precursor. What are the names given to the two processes, and which one involves cartilage as an intermediary stage? 2. Which bones form by endochondral ossification? 3. Which bones form by intramembranous ossification? 4. What happens to bone tissue initially formed by these two processes? 5. By which process(s) is/are long bones originally formed? 6. What types of cells are the precursor to osteoblasts involved in intramembranous bone formation? 7. What is the appearance of newly formed bone matrix that is forming by intramembranous ossification? 8. What is a spicule? (not in the text.) 9. What are trabeculae? (not in the text) 10. How do spicules enlarge? 11. Is intramembranous bone considered “lamellar bone?” If not, what term does apply to the organization of the extracellular matrix? 12. During the early stages of endochondral ossification, what do mesenchymal cells become? 13. Which type of cartilage is produced by the chondroblasts during endochondral bone formation? 14. By what mode(s) of growth is the cartilage model enlarged? 15. Which type of growth accounts for the growth in length of the cartilage model of a long bone? 16. In a very early developing long bone, where does the first bone tissue appear? Is this bone formed by intramembranous or endochondral ossification? 17. What two names are given to the thin cuff of bone that surrounds the prospective diaphysis? 18. How does the presence of the bony collar affect the chondrocytes and the extracellular matrix in the underlying hyaline cartilage? 19. How does calcification of the cartilage matrix affect the adjacent chondrocytes? 20. Blood vessels grow into regions where hyaline cartilage has become calcified, bringing along what type of cell that becomes an osteoprogenitor cell? 21. What other types of cell are brought into the developing marrow cavity where they will engage in a process associated with red marrow? 22. What is a mixed spicule? 23. How is a mixed spicule identified with routine H&E staining? . 24. How does a mixed spicule stain with the Mallory stain? 25. What is the fate of the calcified cartilage of a mixed spicule? 26. Figure 8.17 describes the sequence of events on the formation of a long bone. According to the figure, where does the first marrow cavity form: in the region that is to become the diaphysis or the region that is to become the epiphysis? 27. How is a secondary ossification center formed? Does it form first in the proximal or distal end of a long bone? 28. Where does next secondary ossification center form in a long bong? 29. Where is the epiphyseal cartilage located? 30. If a developing bone has two secondary ossification centers, how many epihyseal growth plates will it have? 31. What zones can be distinguished in the epiphyseal plate (aka epiphyseal disk or epiphyseal cartilage?) 32. What are the distinctive features of each of those zones? 33. As cartilage is resorbed and replaced at the epiphyseal plate, what type of bone is formed? 34. Explain how the thickness of the epiphyseal plate remains essentially constant as a long bong elongates. 35. Must new cartilage be formed, calcified, and subsequently resorbed in order for a long bone to grow in length? 36. What is epiphyseal closure? Why is a long bone incapable of growing longer after epiphyseal closure? P. 37. What is meant by “internal remodeling?” 38. What is the role of osteoclasts in internal remodeling? 39. How large is the resorption cavity relative to the diameter of an osteon? 40. What are the components of a bone remodeling unit? 41. What is a cutting cone? 42. What is a closing cone? 43. What is the approximate diameter of a typical osteon? 44. What are cutting cones rather rarely encountered in sections of bone? 45. Explain how osteons come to have concentric lamellae. 46. In adults, what term is to the abnormal situation when bone resorption greatly exceeds bone deposition? 47. What are the target cells of parathyroid hormone and what is the action of this hormone on those cells? 48. A question not directly addressed in the text: How does internal bone remodeling contribute to the formation of interstitial lamellae? (Hint: think about the location of interstitial lamellae relative to Haversian systems and what would happen to an existing osteon if internal bone remodeling occurs nearby.)