Microbiology Lab Training: Antimicrobial Stewardship Stage 3
advertisement
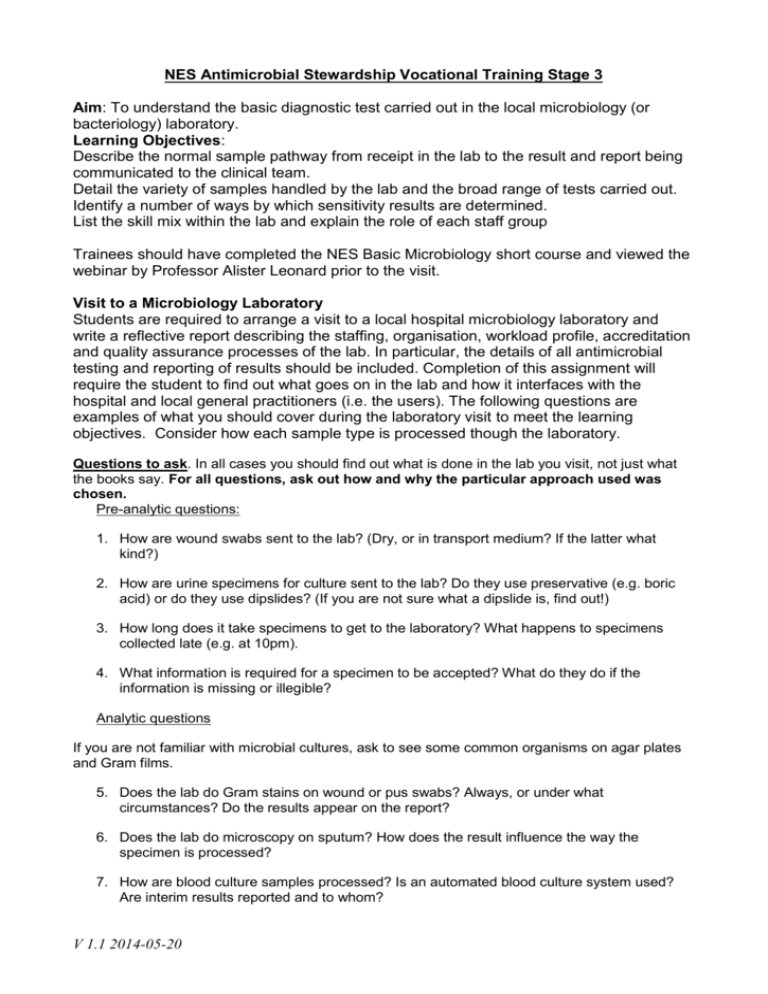
NES Antimicrobial Stewardship Vocational Training Stage 3 Aim: To understand the basic diagnostic test carried out in the local microbiology (or bacteriology) laboratory. Learning Objectives: Describe the normal sample pathway from receipt in the lab to the result and report being communicated to the clinical team. Detail the variety of samples handled by the lab and the broad range of tests carried out. Identify a number of ways by which sensitivity results are determined. List the skill mix within the lab and explain the role of each staff group Trainees should have completed the NES Basic Microbiology short course and viewed the webinar by Professor Alister Leonard prior to the visit. Visit to a Microbiology Laboratory Students are required to arrange a visit to a local hospital microbiology laboratory and write a reflective report describing the staffing, organisation, workload profile, accreditation and quality assurance processes of the lab. In particular, the details of all antimicrobial testing and reporting of results should be included. Completion of this assignment will require the student to find out what goes on in the lab and how it interfaces with the hospital and local general practitioners (i.e. the users). The following questions are examples of what you should cover during the laboratory visit to meet the learning objectives. Consider how each sample type is processed though the laboratory. Questions to ask. In all cases you should find out what is done in the lab you visit, not just what the books say. For all questions, ask out how and why the particular approach used was chosen. Pre-analytic questions: 1. How are wound swabs sent to the lab? (Dry, or in transport medium? If the latter what kind?) 2. How are urine specimens for culture sent to the lab? Do they use preservative (e.g. boric acid) or do they use dipslides? (If you are not sure what a dipslide is, find out!) 3. How long does it take specimens to get to the laboratory? What happens to specimens collected late (e.g. at 10pm). 4. What information is required for a specimen to be accepted? What do they do if the information is missing or illegible? Analytic questions If you are not familiar with microbial cultures, ask to see some common organisms on agar plates and Gram films. 5. Does the lab do Gram stains on wound or pus swabs? Always, or under what circumstances? Do the results appear on the report? 6. Does the lab do microscopy on sputum? How does the result influence the way the specimen is processed? 7. How are blood culture samples processed? Is an automated blood culture system used? Are interim results reported and to whom? V 1.1 2014-05-20 8. Are vaginal swabs cultured? What organisms are reported out? 9. Which tests are used to identify Staphylococcus aureus? 10. Are Enterobacteriaceae in urine identified to species level, or just reported as "coliforms?" What is the reason for the approach taken? 11. What method would be used to identify Enterobacteriaceae from blood cultures? 12. What method is used to screen for and identify Salmonella in stool specimens? 13. How are sensitivity tests done on Enterobacteriaceae from urine or blood? 14. How is MRSA identified? How is it reported, and to whom? 15. What methods are used on specimens other than microscopy and culture? Are molecular methods, or antigen detection methods, used and why? 16. What happens to virology requests - e.g. urgent tests from a needle-stick injury? 17. What methods are used to test the antibiotic sensitivity of each organism? Explain each method and results interpretation. Can you describe the process for antibiotic sensitivity testing of Streptococcus pneumoniae, Staphylococcus aureus and Pseudomonas aeruginosa? What governs which antibiotics are tested on each specimen and why? 18. Does the laboratory have a different approach for specific organisms such as anaerobes? Why? 19. What is the role of non-therapeutic agents used in sensitivity testing? Post-analytic questions: 20. Who reviews or checks results before they go out? Does this depend on whether the specimen is positive or negative? What about nights and weekends? 21. How are results transmitted to clinicians? Phone? Fax? Computer? Paper reports? How long does it take? 22. Does the lab report out all sensitivity test results, or hold some back? If so why? 23. How would the lab recognise a cluster of organisms that could indicate cross-infection? 24. What quality assurance testing is carried out by the lab and why is it important? V 1.1 2014-05-20