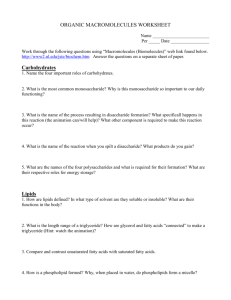
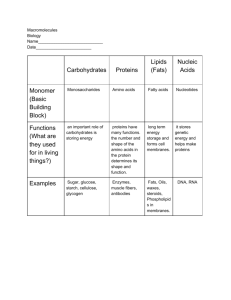
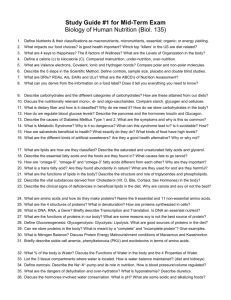
Topic: Exchange and functions of carbohydrates
advertisement

LESSON 1 Theme: Digestion. Questions for self-control: 1. Digestion as the initial stage in metabolism. I.P. Pavlov’s contribution to the research of this issue. 2. Digestion of food in the mouth cavity, stomach and intestinal. 3. Chemical composition, saliva enzymes, gastric and intestinal juices. 4. Absorption of products of digestion. Definition of membrane digestion. 5. Diagnostic importance of biochemical analysis of gastric juice. Currency of theme. A doctor must know the peculiarities of the process of digestion in normal and pathological conditions; must be able to estimate biochemical composition of gastric juice because violation of digestion and mechanisms of regular absorption may cause the following: - hypotrophy with violation of self-reproduction of parts of the body; - hypovitaminosis with the development of pathological conditions without distinct clinical manifestation; - beriberi – the illnesses with distinct clinical presentation as the result of complete absence of vitamins in the organism; - allergic conditions connected with the preservation of protein specifics and the increase of permeability of biological membranes in the cells of gastrointestinal tract. The ability to detect pathological components of gastric juice may be used while diagnosing lesions of gastrointestinal tract during the initial stages of disease. Educational and pedagogical aims. 1. The main object of the lesson: to work out skills of using the knowledge of biological role of gastric juices and mechanisms of food splitting in the mouth cavity and the ventricle (in the process of practical work of a physician). 2. The by-objects of the lesson: to form the skills of qualitative and quantitative detecting of hydrochloric acid in gastric juice, the skills of evaluation and interpretation of the results of biochemical analysis of gastric juice. 1 Annotation of the theme: Digestion. Digestion is the complex of the processes which support the mechanical decomposition and chemical (fermentative, first of all) disintegration of nutritive matter into the components which are suitable for absorption and taking part in metabolism. What is the biological significance of digestion and what are the aims of digestion? 1) The transformation of polymeric compounds into monomeric compounds: proteins – amino acids carbohydrates – monosaccharide fats – higher fatty acids and glycerine 2) While being digested, the food looses its specifics. The main types of digestion. 1) Extracellular (cavernous, distant) 2) Intracellular 3) Membrane or parietal Saliva. Saliva is educed by excretory ducts (1,5 litre a day). pH is 6,5-6,9, it is subacid, its ductitility is 1,2-2,4 units. The following buffer systems are in saliva: protein, haemoglobin, phosphate. Saliva’s composition: 99,42 percent of water; 0,58 percent of organic and inorganic substances. Inorganic substances: salt Ca, phosphates, compounds of Na and K, chlorides, bicarbonates, fluorides, rhodonites and etc. Organic substances: proteins, carbohydrates, free amino acids, vitamins and others. Organic substances (by its origin) are divided into those which generate into saliva from blood serum (amino acids, urea) and those which are synthesized by salivary glands (amylase, glycoprotein, mucin, globin and others). The basis of organic substances is protein – 17 fractions. Enzymes. There are 5 groups of enzymes. Carbonic anhydrase, esterase, proteolytic enzymes, enzymes of mixed group – more than 50. Phosphatase, lipase, lysozyme, hyaluronidase, DNase, ribonuclease. Functions. Protective: moisturizes, prevents from drying up (mucin), from cracks and mechanical irritants, assists in wetting of food debris, micro organisms and prolongs their vital activity; bactericidal effect of lysozyme, lipase, DNase, ribonuclease. 2 Digestive: the formation of bolus and digestion of carbohydrates. Composition of gastric juice. Water, HCl, mucous substances, inner factor of Kastle, histamine, gastrin, pepsin, lipase, renin, 35 million of glands which generate about 2,5 litre of gastric juice a day. HCl – produces parietal cells of ventricle under the influence of gastrin. Its role: - to activate pepsinogen - acts as antiseptic - provides pH medium 1,5-2,5 - assists in swelling and denaturation of proteins - stimulates the generation of secretin in duodenum Types of HCl: - free HCl - combined HCl (to proteins and the products of their digestion) - total HCl (free HCl and combined HCl) - total acidity (all acid reacting components of ventricle – free HCl, combined HCl, organic components, calcium phosphate salts). Mucous substances. The basis of mucous substances are glycoproteins (mucoproteins, mucopolysaccharides). They prevent the walls of the stomach from denaturated effect of HCl and from digestive effect of pepsin; also they have antiseptic action. Inner factor of Kastle. Glycoprotein, formed in the mucous substances of the stomach, is necessary for the normal absorption of B12 in the bowels (intestinal), which comes into it with the food. The absence of the factor leads to malignant anemia. Histamine. Histamine is formed in the mucous substances of the stomach; it provides the secretion of HCl and pepsin affecting the parietal and the cellula principalis of the stomach. Gastrin. It is a polypeptide formed in the walls of the stomach. It affects the parietal and the cellula principalis of the stomach stimulating the excretion of HCl and pepsinogen. Pepsin. Polypeptide disintegrates native denaturized proteins, generates the cellula principalis of the stomach under the influence of gastrin, and splits the peptide bonds which were formed by aromatic amino acids. Gastricsin. Polypeptide, the optimum is pH=3,5. It provides the adaptation of the organism to the specifics of nutrition (vegetal food). 3 Lipase. It is inactivated in the organisms of grown-ups by acid medium. It is able to hydrolyze triglycerides of milk in the organisms of infants in case of the following factors: pH=5,0 or emulsified fat. Rennin. It clots the milk in organisms of infants. Different forms of HCl have definite constants which may change in different pathological conditions or they may increase and decrease. The N (norm) of free HCl – 20-40 milimole per litre; more than 40 – hyperchlorhydria, less than 20 – hypochlorhydria, 0 – achlorhydria. N of total acidity is 40-60 milimole per litre; more than 60 – hyperacidity, less than 40 – hypoacidity, 0 – non-acid condition (the absence of HCl and pepsin leads to achylia). Composition of intestinal juice. Pancreas juice is generated under the influence of secretin in duodenum and pancreozymin. pH=7,1-8,2 1,5 litre per day 1. Enzymes affecting proteins – trypsin, chemotrypsin, enterokinase, carboxypeptidase, collagenase, elastase - turn into peptides and dipeptides. 2. Enzymes affecting carbohydrates – amylase, sucrose, lactase, maltase, amino 1,6 glycosidase, oligo 1,6 glycosidase. 3. Enzymes affecting lipids – lipase, emulsified lipids CO2 which are generated in the process of neutralization of HCl by bicarbonates. After that bile acids split them into diglycerides and take them to the stomach. 4. Enzymes affecting nucleic acids – ribonucleic acid, desoxyribonucleic acid. Bowels (intestinal). pH=7,0-8,5 1,5 litre per day 1. aminopeptidase, dipeptidase, cathepsins – dipeptides 2. aminopeptidase, dipeptidase, cathepsins + invertase – disaccharides, monosacchrides 3. lipase, esterase, cholesterolesterase – mono glycerin, glycerin – into the stomach 1. phosphatase, nuclease, nucleotidases. Defensive mechanisms in mucous substances of stomach. 1. Enzymes are generated in non-active form. 2. Mucin – mucous substances. 4 3. Defensive barrier (molecules of fat (lipids) with fumes). It is filled with water; it is situated on the external part of epithelial cell. If in normal condition, spirit and water may pass this barrier. This barrier may be destroyed only by detergents. The natural detergents in the organism are bile acids, which may pass into the stomach while reflux. Bile acids outwash fat. 4. The regeneration of epithelial cells of the walls of the stomach occurs in 3-5 days. 5 LESSON 2. (Control lesson) Theme: Digestion. Questions for self-control: 1. Digestion as the initial stage in metabolism. I.P. Pavlov’s contribution to the research of this issue. 2. Digestion of food in the mouth cavity, stomach and intestinal. 3. Chemical composition, saliva enzymes, gastric and intestinal juices. 4. Absorption of products of digestion. Definition of membrane digestion. 5. Diagnostic importance of biochemical analysis of gastric juice. 6 LESSON 3. Topic: Exchange and functions of carbohydrates. Questions for self-control: 1. Carbohydrates, their spread, their biological role. 2. Classification of carbohydrates. Their composition: a) monosaccharides and their derivatives (trioses, pentoses, amino sugar, uronic acids, glycosides, phosphoric ethers, monosaccharides); b) disaccharides (lactose, maltose, saccharose); c) polysaccharides: glycoproteins, proteoglycans, glycolipids, inulin, gum, pectic substances, agar. 3. Proteoglycans. Their biological role. 4. Glycoproteins. Sialic acids. Their biological role. 5. Glycated protein. Glycated hemoglobin. 6. Digestion and absorption of carbohydrates in the gastrointestinal tract. The role of cellulose. Intolerance of carbohydrates. Carbohydrates are hydroxyl aldehyte or ketonospirits. Functions of carbohydrates. 1. Energy. 2. Carbohydrates (ribose, deoxyribose) are in the composition of nucleic acids (deoxyribonucleic acid, ribonucleic acid), free mononucleotides (adenosine triphosphate, guanosine triphosphate, cyclic adenosine monophosphate, etc.), co-enzymes (nicotine amide adenine dinucleotide, nicotine amide adenine dinucleotide phosphate, flavin adenine dinucleotide, KoQ). 3. Structural: glucoproteins – collagen; proteins – receptors; glycocalix, proteins defining blood group; factors of blood coagulation; enzymes; hormones; glycosaminglycans, etc. 4. Defensive: immunoglobulin, interferon, mucins, fibrinogen, glycosaminoglycan, etc. 5. Disintoxicating: they are in the composition of phospho-adenosin-phospho-sulfate and uridine diphosphate. Daily maintenance is 500 gram. 7 Classification. The first class is monosaccharides. They are derivatives of polyatomic spirits containing aldehyde and ketonic groups. Depending on the quantity of carbonic atoms, monosaccharides are divided into: trioses, tetroses, petoses (ribose, deoxyribose), hexoses (glucose, galactose, fructose, etc.). CH2OH O OH CH2OH O OH OH OH OH OH OH OH α-D-glucose CH2OH O OH OH OH OH β-D-glucose α-D-galactose CH2OH CH2OH O H OH OH H OH fructose Derivatives of monosaccharides: - uronic acids: glucoronic acid, galactouronic acid). They are in the composition of glycosaminoglycans. COOH O OH OH OH COOH O OH OH OH OH OH glucoronic acid galactouronic acid - amino sugar: glycosamin, galactosamin). They are in the composition of glycosaminoglycans. CH2OH O OH OH OH NH2 glycosamin - pentose (ribose or deoxyribose which are binding to nitrous basis in nucleotide by N-glycosoid bond). They are in the composition of RNA, DNA, ATP, NAD, FAD and others. CH2OH O OH H H H H OH OH ribose CH2OH O OH H H H H OH H deoxyribose 8 - phosphoric ethers of monosaccharides – substitution of hydrogen atoms into remains of phosphoric acid: glucose-6-phosphate; fructose-1,6-diphosphate; ribose-5-phosphate and others. OH H2C O P O O OH OH OH OH OH glucose-6-phosphate The second class is oligosaccharides. They are composed of 2 or more monosaccharides (from 2 to 10 remains of monosaccharides). Disaccharides: - maltose consists of 2 molecules of L-D-glucose which are linked by L-1,4-glycoside bond. It has free semi-acetal hydroxyl. It has renewing effect. - lactose (lactic sugar) consists of B-D-galactose and L-D-glucose which are linked by B-1,2glicoside bond. It has free semi-acetal hydroxyl. It has renewing effect. - saccharose consists of L-D-glucose and B-D-fructose which are linked by L-1,2-glycoside bond. It hasn’t hydroxyl and that’s why it has no renewing effect. saccharose The third class is polysaccharides. They contain more than 10 remnants of monosaccharides. They are divided into homopolysaccharides and heteropolysaccharides. Homopolysaccharides consist of one and the same monosaccharide. Starch and glycogen consist of L-D-glucose remnants. Starch 9 Cellular tissue (cellulose) consists of B-D-glucose remnants which are linked by B-1,4glycoside bond. The role of cellular tissue. 1. Irritating the nerve ending of mucous tunic (coat) of intestinal, it intensifies the peristalsis of intestinal. 2. It increases the secretion of intestinal juice. 3. It assists in forming of fecal mass. 4. It adsorbs cholesterol, preventing its suction. 5. It adsorbs heavy metals and radionuclides. 6. Being affected in the intestinal by spirit fermentation, it suppresses the breeding of putrefactive bacteria. Heteropolysaccharides consist of different remnants of monosaccharides and their derivatives. There are the following types of heteropolysaccharides: 1. glycoproteins; 2. glycolipids; 3. proteoglycans. Proteoglycans are complex proteins which consist of proteins and carbohydrates. Carbohydrates which are in the composition of proteoglycans are called glycosaminoglycans. Classification of glycosaminoglycans. 1) hyaluronic acid, 2) chondroitin-4-sulfate, 3) chondroitin-6-sulfate, 4) dermatansulfate, 5) keratansulfate, 6) heparinsulfate and heparin. They are widely spread in the organism of a man. Skin, tendon, cartilages, bones, synovial fluid, vitreous body, eyes, cornea, umbilical cord, mucous membrane of the mouth, nose, bronchus, blood vessels and so on. Functions. 1. Defensive-mechanical. 2. They are biological cement. Filling the intercellular substance, they strengthen the connective tissue, prevent the penetration of harmful substances and morbific micro-organisms into the organism. 3. They possess high hydrophylia, that is, they restrain water and cations, assisting in regulation of water-salt metabolism. 4. They posses high viscosity, alleviate the process of swallowing, take part in the formation of a bolus. 5. Heparin is a natural anticoagulant (prevents the process of blood coagulation). 10 Composition. Hyaluronic acid consists of monomers, possessing glucuronic acid, linked with N-acetyl-D-glucosamine. Heparin consists of monomers, which possess glucuronic acid, linked with N-acetyl-D-glucosamine and 2 remnants of sulfuric acid. For example, structure of heparin: CH2OSO3H COOH OH H O OH H H OSO3H H O O H OH H O H NHCOCH3 p Digestion and absorption of carbohydrates in gastrointestinal tract. The source of carbohydrates in the human body is food carbohydrates, the main of which is starch. Also, there is glucose, sucrose, lactose and fructose in food. Starch is the form of glucose depositing in the cells of plants. Lactose is in the composition of milk and it is the principal carbohydrate in infant’s nutrition. There is glucose and fructose in honey and milk. Maltose comes in with the products in which starch is partially hydrolyzed, for example, with malt or beer. The norm of carbohydrates in nutrition is 400-500 gram per day. Food carbohydrates undergo enzymatic digestion in the gastrointestinal tract. In the process of digestion, enzymatic hydrolysis of glycosidic linkage takes place, monomers (able to be absorptive) are generated, they are able also to get into blood and after that into tissues. Starch is partially absorbed in the mouth cavity under the influence of a-amylase saliva, after that, by pancreatic amylase, in the upper part of small intestine. The products of reaction are maltose and isomaltose, which are (with other disaccharides) hydrolyzed on the surface of small intestine cells to appropriate monomers. Monosaccharide transport from lumen of intestinal into the mucous membrane cells may be realized by means of reduced diffusion and active transport. Glucose coming from intestinal by means of portal vena system gets to liver, where one portion of it is detained and another portion by means of general circulation gets into the cells of other organs and tissues. Glucose consumption by circulation cells occurs with the help of reduced diffusion with the assistance of carbohydrates-transporters. Thus, the speed of transmembrane flow of glucose depends only on gradient of its concentration. The exceptions are the cells of muscles and adipose tissue, where reduced diffusion is regulated by insulin. 11 Pathology of carbohydrates digestion and absorption. There are 2 reasons for the pathology of carbohydrates digestion and absorption: - defect of enzymes taking part in carbohydrate hydrolysis in the intestinal, - derangement of food absorption into the cells of intestinal mucous membrane. Inherited and acquired forms of deficiency of enzyme activity are known. The symptoms of inherited forms are revealed even after the first breast-feeding (when there is deficit of lactase enzyme), after transition to artificial feeding or when adding sugar and starch into the ration (deficit of a-amylase or specific disaccharidase). Acquired forms of pathology may be revealed when a person has intestinal diseases: gastritis, colitis, enteritis. Lactase activity of a grown-up person is lower than of a child. That’s why the decrease of lactase activity may be revealed with the help of the symptoms of milk intolerance. The average rate of this pathology in the African countries is up to 97 percent, in Europe – 7-12 percent. Derangement of absorption may be the result of carbohydrate-transporter deficiency in the system of monosaccharide transport through membrane. When having all these conditions, diarrhea may occur. Intestinal microorganisms make carbohydrates split and organic acids and gases generate. The inflow of water in the intestinal increases, intestinal contents increases, and peristalsis is intensified. All these conditions lead to spasms, pains, flatulence and profuse diarrhea. 12 LESSON 4. Topic: Exchange and functions of carbohydrates. Aim of the lesson: To work out skills of using the knowledge of carbohydrates exchange in the organism (in the practical work of a doctor). Questions for self-preparation: 1. The general scheme of the sources and ways of consumption of glucose in the organism. 2. Glycogen as the main reserved polysaccharide. Its properties, spread, biosynthesis, and mobilisation of glycogen. 3. Glucose content in blood. Hypo-, hyperglycemia, glycosuria, reasons. 4. Regulation of glucose level in blood. The role of CNS, the mechanism of the action of insulin, adrenalin, glucagons, glucocorticoid. The general scheme of the sources and ways of consumption of glucose in the organism Food 60% Liver glycogen 4% Gluconeogenesis 30% liver (synthesis of glycogen,) amino acids, lipids) muscular tissue (synthesis of glycogen) Aerobic glycolisis CO2+H2O+38 ATP Glucose Energy function Pentose-phosphate way of glucose oxidation Pentose ) (ribose, deoxyribose) adipose tissue (synthesis of lipids) brain (energy) Anaerobic glycolisis lactic acid (lactate + 2 ATP) NADFH2 13 Considerable part of glucose, which enters the blood, turns into glycogen – reserve polysaccharide, which is used in the intervals between food intakes as the source of glucose. Exchange and functions of carbohydrates. Glycogen is animal starch. It is the main reserve homopolysaccharide. It consists of L-Dglucose connected with L-1,4 and L-1,6 by glycosidic linkage – (C6H10O5)p. Glycogen may be found in all organs and tissues. Its content in the liver is from 2 to 6 percent; in the muscular tissue – 0,5-2 %. Coloured reaction with iodine – brown colouring. 14 H Glycogen synthesis. Glycogen synthesis in the organism takes place when after the usage of glucose, part of it is remained and it is stored in the organism in the form of glycogen. insulin CH2OH H2C O PO3H2 H H O OH H OH OH OH glucose H H 3 2 “glycogen UTP- uridyl transferase remnant” UDP-glucose + (C6H10O5)p - 2 H3PO4 glycogensynthetase, branching enzyme OH OH H glucose-1-phosphate Mutase H glucose-6-phosphate OH H OH OH glucose-6-phosphate H OH ATP-ADP CH2OH H H O + UTP OH H OPO H OH H Hexokinase, Mg UDP + ATP UTP + ADP (C6H10O5)p+1 + UDP glycogen Enzyme glycosynthetase takes part in the generation of L-1,4 glycosidic linkage. Branching enzyme takes part in the generation of L-1,6 glycosidic linkage. Glycogen decomposition. Glycogen decomposition (with the generation of glucose) takes place in the period between food intakes, physical activity and emotions. Phosphorolytic way is the basic way. phosphorylase “a” (C6H10O5)p +H3PO4 H2C H CH2OH mutase H H O OH H OPO H 3 2 OH OH glucose-1-phosphate H H O PO3H2 H H O glucose-6-phosphatase H OH H OH -H3PO4 OH H OH glucose-6-phosphate CH2OH H H O OH H OH OH OH H blood glucose 15 There is no enzyme gluco-6-phosphatase in the muscular tissue, that’s why glycogen gives no glucose to the muscular tissue, but is oxidized to lactic acid and 2 ATP (glycogenalisis). Aglycogenosis is an inherited disease connected with the absence of enzymes which take part in glycogen synthesis. Glycogen is absent. Glycogenosis is an inherited disease connected with the deficit or complete absence of enzymes which take part in glycogen decomposition. Glycogen in this case is stored in the organs and tissues. The 1st type – hepatic: Girke’s disease – the absence of enzyme glucose-6 phosphatase. Gers’s disease – the absence of enzyme phosphorylase “a”. Glycogen decomposition in the liver is violated and it is stored there. The liver enlarges, it is tight and painful while palpating. There is hypoglycaemia in blood in the periods between food intakes. Anderson’s disease – the absence of branching enzyme. Glycogen is synthesized but with the changed structure (in the shape of long threads). It causes the destruction of hepatocytes, liver cirrhosis, hepatic failure and leads to fatal outcome (children live up to 2 years). The 2nd type – hepatic: Mac Ardle’s disease – the absence of enzyme phosphorylase. Glycogen is stored both in skeletal muscle and cardiac muscle (megalocardia). The 3rd type – generalized: Pompe’s disease – the absence of enzyme 1,4-glycosidase. Glycogen decomposition in all organs and tissues is destroyed (life longevity is about 2 years). The norm of glucose in blood is 3,3-5,5 millimole per litre. The increase of glucose content in blood is called hyperglycemia. 1. Physiological hyperglycemia is temporary. It may be nutritional or emotional (stress). 2. Pathological : - pancreatic diabetes (insulin deficiency) - pituitary tumour – hyper production of STH - tumour of medullary substance of adrenal glands (pheochromocytoma) - hyper production of adrenalin - tumour of adrenal cortex – Itsenko-Kushing’s disease or steroid diabetes – hyper production of adrenal cortex hormones - Basedow’s disease – hyper production of thyroid gland hormones. 16 The decrease of glucose content in blood is called hypoglycemia. 1. Physiological hypoglycemia – after physical exercise stress. 2. Pathological : - glycogenosis (hepatic and generalized) - insulinoma – tumour of B-cell in pancreas – hyper production of insulin - hypo production of adrenal cortex hormones – Addison’s disease or bronzed disease - hypo production of thyroid gland hormones – Mixedem’s disease - insulin overdose in the organism with diabetes Glycosuria – glucose in urine. This is the case when nephritic threshold for glucose is exceeded. Its norm is 8-9 millimole per litre. Regulation of carbohydrates exchange. Adrenalin – increases glucose content by means of activating phosphorylase enzyme (adenylate cyclase system) which causes decomposition of glycogen and glucose generates; blocks glycosynthetase enzyme (glycogen synthesis). Glucagon – the same as adrenalin + activates gluconeogenesis enzymes (stimulates gluconeogenesis). Glucocortocoids – increase glucose content in blood. According to the mechanism of chronic regulation, they are inductors of gluconeogenesis enzymes synthesis (stimulate gluconeogenesis). Insulin – decreases glucose content in blood. 1. Increases permeability of cell membranes for glucose. 2. Activates hexokinase, fructokinase, pyruvate kinase (stimulates glycolisis). 3. Activates glycogensynthetase (stimulates glycogen synthesis). 4. Activates dehydrogenase of pentoso-phosphate way. 5. According to the mechanism of chronic regulation, they are inductors of hexokinase synthesis and repressors of gluconeogenesis enzymes synthesis (blocks gluconeogenesis). 6. It transforms 30 percent of carbohydrates into lipids. 7. Stimulates TAC by means of activating enzyme synthetase which catalyzes the reaction of interaction of acetyl CoA with oxaloacetic acid (OAA). 17 LESSON 5. Topic: Exchange and functions of carbohydrates. Aim of the lesson: To work out skills of using the knowledge of anaerobic oxidation of carbohydrates, techniques of glucose detecting in practical medicine. Questions for self-preparation: 1. Aerobic decomposition of glucose (succession of chemical reactions, energy effect, biological role). 2. Anaerobic decomposition of glucose. Similarities and differences of aerobic and anaerobic glycolisis. Paster’s effect. 3. Gluconeogenesis, chemism, its biological role. 4. Kori cycle (glucose-lactic cycle), biological role. 18 Aerobic glycolisis is the basic way of glucose catabolism. It occurs in the presence of oxygen. H2C O PO3H2 Insulin H C H 2O H H H O OH H OH OH H OH ADP glucose OH Isomerase H OH H OH OH H OH glucose-6-phosphate H Hexokinase ATP CH2OPO3 H2 CH2OPO3 H2 CH2OH O H OH H OH H OH H H ADP H OH H Aldolase CH2OPO3 H2 O Fructokinase ATP H fructose-1,6-diphosphate fructose-6-phosphate O CH2OH C + O H 3-phosphoglycerinaldehyde-5% O C C O PO3H2 PO3H2 C O H2 phosphodioxiaceton-95% H 2 Central reaction of oxidoreduction O C H 2 O H C OH C O PO3H2 H2 H C OH respiratory chain 2*3=6 ATP 3-phosphoglycerinaldehyde-5% 2 O C OH H C O PO3H2 Mutase 2 C OH H2 Pyruvatekinase 2ADP Enolase -HO 2 C OH H2 2-phosphoglycerate 3-phosphoglycerate 2 H C O ~PO3H2 2ATP 1,3-diphosphoglycerin acid C O PO3H2 H2 C COOH 2ADP C O PO3H2 H2 O C OH H C OH Kinase 2 C O ~ PO3H2 Dehydrogenase 2NAD 2NADH2 C 2 COOH C O 2ATP CH3 pyruvic acid phosphoenol pyruvic acid pyruvatedehydrogenase complex NAD (PP), FAD (B2), TDP (B1), SH-CoA (B3), lipoic acid O 2 H 3C + 2 NADH2 sCoA acetyl CoA respiratory chain Crebsis cycle 2∙3=6 ATP 2∙12=24 ATP respiratory chain 19 Anaerobic glycolisis is the basic way of glucose catabolism. It occurs in the absence of oxygen. OH H OH Hexokinase ATP ADP glucose H Isomerase H OH H OH OH H OH glucose-6-phosphate CH2OPO3 H2 CH2OPO3 H2 CH2OH O H OH H H H OH H O CH2OH C + O C O PO3H2 2 2 H C OH 2NAD 2NADH2 3-phosphoglycerinaldehyde-5% O C OH H C OH 2 Kinase C O ~ PO3H2 H C OH 2ADP C O PO3H2 H2 2ATP O Mutase 2 C OH H C O PO3H2 Pyruvatekinase 2 C O ~ PO3H2 2ADP phosphoenol pyruvic acid 2ATP Enolase -HO 2 C OH H2 2-phosphoglycerate 3-phosphoglycerate CH2 PO3H2 1,3-diphosphoglycerin acid C O PO3H2 H2 COOH H 3-phosphoglycerinaldehyde-5% O O Dehydrogenase C O PO3H2 H2 C C O H2 phosphodioxiaceton-95% H O C H H fructose-1,6-diphosphate fructose-6-phosphate 2 OH H ADP Aldolase CH2OPO3 H2 O Fructokinase ATP H OH O PO3H2 OH H2C Insulin C H 2O H H H H O OH H OH 2 LDH4,5 C COOH C O 2 NADH2 CH3 2 NAD 2 CH3 H OH + 2ATP COOH lactic acid pyruvic acid 20 Anaerobic glycolisis progresses in anaerobic conditions: liver, skeletal muscles, eye retina, red (blood) cells. It gives the opportunity to receive the energy in the conditions of insufficient supply of oxygen in tissues. Aerobic and anaerobic glycolisis progress in the same way (till generating of PA). This is their similarity. The differences are: NADH2 in anaerobic conditions (in central reaction of oxidoreduction) doesn’t go into respiratory chain; 6 ATP is not generated there. NADH2 is used for the restoration of PA into lactic acid. C COOH LDH C O 2 NADH2 CH3 2 NAD pyruvic acid CH3 H OH + 2ATP COOH lactic acid (lactate) Paster’s effect is suppression of anaerobic glycolisis by breath (O2). If there is O2, the generated NADH2 goes into respiratory chain and leads to generation of ATP, but is not used for transformation of PA into lactic acid. Glyconeogenesis. Glyconeogenesis is glucose generation from the products of non-carbohydrate character. The main precursors are: PA and lactic acid. Intermediate products are glycerol and amino acids. Glyconeogenesis progresses reversibly to anaerobic glycolisis. The exceptions are 3 irreversible reactions (hexokinase, fructokinase and pyruvate kinase). In these cases the reactions progress by alternative route in the presence of other enzymes. 21 Irreversible reactions. C COOH 1. COOH pyruvatecarboxylase ATP C O ADP CH2 O phosphoenolpyruvatecarboxykinase COOH CH3 GTP GDP oxaloacetate pyruvic acid COOH C -CO2 O ~ PO3H2 CH2 phosphoenolpyruvic acid 2. CH2OPO3 H2 CH2OPO3 H2 O H OH H CH2OPO3 H2 fructose-1,6diphosphotase H OH H fructose-1,6-diphosphate 3. H2C O PO3H2 glucose-6H OH phosphatase H OH H OH OH H OH glucose-6-phosphate CH2OH O H OH H H OH H fructose-6-phosphate CH2OH O OH OH OH OH glucose 22 Kori cycle (glucose-lactic, glucose-alanine cycle). Anaerobic glycolisis and glyconeogenesis progress simultaneously in different tissues. The combination of glyconeogenesis activity and glycolisis activity, which provide the circulation of carbohydrate skeletons of glucose and lactic acid between the liver and the muscle, is called Kori cycle. Glucose Glucose-6-phosphate Alanine Glucose-6-phosphate PA PA Lactate NH3 Muscle blood liver Biological role: 1. Provides economical consumption of carbohydrates in the organism. 2. Supports optimal glucose content in blood. 3. In the process of muscle activity anaerobic glycolisis takes place and large quantity of lactic acid is generated. With the assistance of Kori cycle lactic acid is not stored in muscles but is used for the generation of glucose, which means that it is utilized by the organism. 23 LESSON 6. Topic: Exchange and functions of carbohydrates. Aim of the lesson: To work out skills of using the knowledge of aerobic oxidation of glucose, glyconeogenesis in practical medicine. Questions for self-preparation: 1. The influence of ethyl alcohol on carbohydrates exchange. 2. Pentose-phosphate way of glucose oxidation, chemism of oxidizing stage, its biological role. 3. Pathology of carbohydrates exchange: pancreatic diabetes, galactosemia, fructosuria The influence of ethyl alcohol on carbohydrates exchange. The basic way of alcohol utilization in the liver (70-90 %): O C2H5OH dehydrogenase NAD NADH2 ethanol dehydrogenase NAD NADH2 C H3C H acetaldehyde O H 3C O C OH acetic acid H 3C TAC sCoA acetyl CoA When taking large quantities of spirit, the quantity of NAD decreases, the quantity of NADH2 increases. It causes the diminution of PA, the increase of lactic acid; PA is the main precursor of glucose formation. C COOH C O CH3 pyruvic acid LDH 4,5 NAD NADH2 CH3 H OH COOH lactic acid Hypoglycemia – there isn’t enough glycogen in liver and muscles taking alcohol on an empty stomach, after physical activity; chronic alcoholism). Hypoglycemia may cause the loss of consciousness when a person has alcoholic intoxication. 24 Pentose-phosphate way of glucose oxidation. It is spread in: red bone marrow, lymph nodes, adipose tissue, mammary gland, red (blood) cells, adrenal cortex. It has 2 stages: 1).oxidizing stage progresses in aerobic conditions H CH2OH H H O OH H OH hexokinase, Mg ATP ADP OH OH H glucose H2C O PO3H2 H OH H OH H OH OH H OH dehydrogenase NADF NADFH2 glucose-6-phosphate COOH H2C O PO3H2 H +H2O O H O OH H OH H OH 6-phosphogluconolacton H HO O OH H dehydrogenase H NADF NADFH2 C H OH H OH H OH H OH H OH CH2O-PO3H2 6-phosphogluconate CH2O-PO3H2 ribose-5-phosphate 2. non-oxidizing stage progresses in anaerobic conditions ribose-5phosphate fructose-6phosphate glucose-6phosphate glucose Biological role. 1). formation of ribose-5-phosphate (pentose) • synthesis of RNA, DNA • synthesis of co-enzymes NAD, NADF, FAD, KoA • synthesis of ATP, GTP, UTP, CTP, 3’5 c AMP • synthesis of glucose 2). formation of NADFH2 • synthesis of higher fatty acids • synthesis of ketone bodies • synthesis of cholesterol and its derivatives (bile acids, steroid hormones – sex hormones and adrenal cortex hormones, provitamin – D3) • neutralization of medications and venom in liver 25 Pathology of exchange of carbohydrates. Pancreatic diabetes. Pancreatic diabetes is exchange-endocrine disease which is characterized by an inherited predisposed absolute or relative deficiency of insulin. Pancreatic diabetes of the 1st type (insulin-dependent).It is caused by the mutation of the gene which is responsible for the synthesis of insulin. Insulin is either not generated or generated with the changed structure (absolute deficiency of insulin). The content of glucose is increased – hyperglycemia. The content of glycated hemoglobin in blood increases (more than 8 %). Glucose appears in urine – glycosuria. Complaints: polyuria – frequent urination (glucose increases osmotic pressure); polydipsia – dryness in the mouth, thirst; polyphagia – the sense of hunger, a person eats frequently but remains thin (since glucose is in blood, it doesn’t go into the cell and doesn’t give energy). Pancreatic diabetes of the 2nd type (insulin-independent). The reason is not known completely. The quantity of receptors to insulin is decreased, also, the structure of receptors may change. Elderly obese people are susceptible to this type of diabetes. Rapid complications of the disease are: lesions of eye vessels – retinopathy; lesions of vessels of feet legs – gangrene; essential hypertension, atherosclerosis. Late complications are connected with the decrease of artery elastin by means of glycosilation of collagen and elastin (diabetic macroangiopathy). Microangiopathy is the result of capillary injury and small vessels injury. It leads to nephropathy and retinopathy (cataract, dysfunction of kidney). Galactosemia is an inherited disease connected with the absence of enzyme galactose-1phosphate-uridyltransferase, which catalyzes the transformation of galactose-1-phosphate into glucose-1-phosphate. This leads to the storage of galactose and galactose-1-phosphate in blood, urine, cells (it has toxic effect). After taking milk (galactose is in the composition of lactose) an infant has: vomiting, nausea, diarrhea, stomachache. If milk is not excluded from the ration, it leads to cataract, liver cirrhosis, spleen cirrhosis, mental retardation. Fructosuria is the absence of enzyme fructokinase which catalyzes transformation of fructose into fructose-1-phosphate in liver. This leads to fructosemia and fructose appears in urine (fructosuria). The nephritic threshold for fructose is 0,73 millimole per litre. Since fructose is in the composition of sucrose disaccharide, after taking food containing sucrose there are the following: vomiting, nausea, diarrhea, stomachache and convulsions. Medical treatment for galactosemia and fructosuria: to exclude galactose and fructose from the ration of a child. 26 LESSON 7 (Control lesson). Topic: Exchange and functions of carbohydrates. Questions for self-control: 1. Carbohydrates. Their content in products and tissues, their biological role. 2. Classification of carbohydrates. Structure. a) monosaccharides (pentoses, hexoses, amino sugar, uronic acids, glycosides, phosphoric ethers of monosaccharides). b) disaccharides (lactose, maltose, sucrose). c) polysaccharides: homopolysaccharides (glycogen, starch, cellular tissue), heteropolysaccharides (glycoproteins, proteoglycans, glycolipids). 3. Proteoglycans. Biological role. Classification. Structure of hyaluronic acid, heparin. 4. Glycoproteins. Sialic acids. Biological role. 5. Glycated proteins. Glycated hemoglobin. 6. Digestion and absorbtion of carbohydrates in gastrointestinal tract. The role of cellulose in the organism. 7. The fate of absorbed monosaccharides, glucose content in blood (in norm). Hyper-, hypoglycaemia, the cause of their origination. Glycosuria. 8. Glycogen. The mechanism of synthesis and disintegration of glycogen to glucose. Glycogenosis. 9. Regulation of carbohydrates exchange. The importance of nervous and endocrine systems. The mechanism of hormones activity: adrenalin, glucagon, insulin, glucocorticoids. 10. Aerobic oxidation of carbohydrates (aerobic glycolisis), the succession of reactions, energy effect, biological role. 11. Anaerobic oxidation of carbohydrates (anaerobic glycolisis), the succession of reactions, energy effect, biological role. 12. Similarities and differences of aerobic and anaerobic oxidation of glucose. Paster’s effect. 13. Glyconeogenesis, chemical reactions. Glucose-lactate cycle . 14. Glucose in the cycle of tricarboxylic acids (TAC – Krebs cycle), the succession of TAC reactions, localisation in the cell, enzymes of the cycle, biological role. 15. Respiratory chain as the final stage of generating energy (catabolism of glucose). 16. Pentose-phosphate way of carbohydrates disintegration, its importance for the organism. 17. The influence of ethyl spirit on carbohydrates exchange. 18. Pathology of carbohydrates exchange in organism: pancreatic diabetes, glycogenosis, galactosemia, fructosemia, lactose intolerance. 27 LESSON 8. Topic: Exchange and functions of lipids. Aim of the lesson: To work out skills of using the knowledge of the peculiarities of chemical structure of lipids, their biological role, their digestion and absorption, transport of lipids, intracellular disintegration of lipids in practical medicine. Questions for self-preparation: 1. Spread of lipids in the organism of a person, reserve and protoplasmatic fats, the speed of their renewing in the organism. 2. Classification of lipids. Their biological role. 3. Digestion and absorption of fats. The role of bile in lipids assimilation. 4. Intracellular disintegration of lipids: B-oxidation of higher fatty acids, energy balance of palmitic acid oxidation. Glycerine oxidation. Peroxide oxidation of lipids. Initial test-control: 1. Answers to the questions of test- and programmed control (in written form). 2. Frontal oral test. Lipids are compounds, different in structure, but united by one common property – lipids are not soluble in water, but they are dissolved in organic solvents. Lipids are usually extracted by ether, chloroform, methanol. An adult person has 10-12 kg of fat, 2-3 kg of which are structural fats. Fats can be: reserve – those which are stored in adipose tissue and have energy function, structural – they take part in the building of membranes, brown fat – it is important in the process of thermoregulation (in a body of a child). Fat is quickly regenerated. Half of all lipids is renewed during 5-9 days, lipids in liver are renewed in 3 days. The functions of lipids. 1. Structural. 2. Energy. 3. Defensive (protects internals from injuries and concussions). 4. They take part in thermoregulation. 5. Formation of water (camels in a desert may do without water owing to fat in their humps). 6. Solvent for vitamins. 28 7. Phospholipids realize transport through the membrane. 8. Glycolipids take part in immunologic reactions, in the reactions of hormones detection. 9. Gangliosides are connected with long-term memory. 10. Sphingolipids take part in the transmission of nervous impulse. According to their structure lipids are classified into: 1. Fatty acids. 2. Lipids containing glycerine. a) neutral fats CH2OCOR1 CH2OCOR2 CH2OCOR3 b) phospho-glycerides CH2OCOR1 CH2OCOR2 OH CH2O P O OH 3. Lipids not containing glycerine. HC a) sphingolipids CH(CH2)12CH3 CHOH CHOH CH2O P choline b) steroids (cholesterol) H3C CH3 CH3 CH3 CH3 HO 4. Lipids connected with the substances of other classes - lipoproteins - proteolipids - lipoaminoacids - lipopolysaccharides 29 The flux of fats into the organism. The daily need of vegetable and animal fats is 50-70 g. Nutritative value of lipids is determined by the availability of unsaturated, not generated in the organism fatty acids in them (linoleic acid and linolenic acid). The daily inflow of these acids is 4-8 g. Caloric value of fat is 38,9 kilojoule/g, carbohydrates – 17 kilojoule/g, proteins – 18 kilojoule/g. When passing gastrointestinal tract, fats are disintegrated into their end products. Digestion and absorption of lipids in gastrointestinal tract. Under the influence of enzyme lipase, neutral fats (TAG) are disintegrated into glycerine and fatty acids. Cholesterol ethers (ECS) - under the influence of cholesterolesperase - are disintegrated into cholesterol and fatty acids. Phospholipids (PL) - under the influence of phospolipase - are disintegrated into glycerine, fatty acids and choline. Also in the walls of intestinal the re-synthesis of fats takes place: TAG, PL, esterase, PL, ECS. Then, the newly generated lipids (in the composition of chylomicrons) go into lymphatic fluid, and after that into blood. There is enzyme lipoproteidlipase on the surface of vessels endothelium. It hydrolyzes triacylglycerols (TAG) to glycerol and 3 moles of fatty acids. Fatty acids go into adipose tissue where they can be stored in the form of TAG or go into muscles where they are oxidized with the generation of energy. The role of bile acids. 1. They emulsify fats (crush into small drops). 2. They activate enzyme lipase. 3. They assist in the absorption of fatty acids, cholesterol, generating micelles. Bile acids are: 1. Cholic acid, 2. Deoxycholic acid, 3. Chenodeoxycholic acid. Binate bile acids are bile acids conjugated (connected) with glycine or taurine. 30 Lipids Into limphatic chylomicrons fluid Itestinal Into blood chylomicrons TAG Liver Muscles Glycerine Fatty acids Adipose tissue Oxidation of fatty acids (Knoop studied this process – 1904). First of all, fatty acid should be activated. This process takes place in the cytoplasm. There are 4 reactions of fatty acid in the matrix of mitochondrion: 1. Dehydrogenation, 2. Hydration, 3. The second dehydrogenation, 4. SH. β-oxidation of fatty acids R R R ATP, Mg dehydrogenase CH2 CH2 CH2 Acyl-СoAsynthetase CH2 CH2 CH2 COOH С COSKoA FAD FADH2 respiratory chain acyl-СoA fatty acid R dehydrogenase NAD NADH2 respiratory chain 3 ATP CH2 CH CH2 + H2 O hydrogenase HC OH CH2 CH COSKoA С С COSKoA β-hydroacyl enoil-СoA R CH2 C 2 ATP R + HSСoA O thyolase CH2 COSKoA С β-ketoacyl-СoA CH2 + CH3 COSKoA С С COSKoA acyl-СoA acetyl- СoA Krebs cycle respiratory chain 12 ATP 31 Energy balance of β-oxidation of fatty acids palmitic acid C15 H31 COOH 7 NADH2 7 FADH2 8 CH3COOSСOA 7x3=21 ATP 7x2=14 ATP acetyl-СOA 8x12=96 ATP Total 130 ATP Peroxide oxidation of lipids. POL is also called free-radical oxidation of lipids. This oxidation progresses on the low minute level (with low speed) in the membranes of mitochondrion, lysosomes, erythrocyte tunic, and where there are unsaturated lipids (phospholipids). The processes of POL are important. They take part in: - regulation of membrane permeability; - renewing of cell membranes; - regulation of the speed of organism growth; - proliferation of the cells. The products of peroxide oxidation of unsaturated lipids are: - free radicals – R; - peroxide radicals – ROO; - hydroperoxides; - aldehydes. The products of POL are molecules capable of the reactions which may accelerate chain reactions of peroxide oxidation of unsaturated lipids and react with bio-molecules (proteins, nucleic acids), causing their dysfunction. Antioxidant protective system provides the stable level of POL. Antioxidants lessen the concentration of free radicals. 32 Antioxidants. 1. Genuine antioxidants of tocopherol type (vitamin E, thyroxin, selenium). 2. SH – containing low-molecular compounds (glutathione, cysteine). 3. Antioxidants – complexes: mono-di- tricarboxylic acids (citric, nicotinic, ascorbic, benzoic). 4. Enzymatic defensive mechanisms: glutathione – reductase: glutathione – dehydrogenase, catalase, superoxidedismutase. The failure of this defensive system and, as a result of it, the intensification of peroxide oxidation occurs in the following circumstances: 1. Spring deficit of antioxidants, tocopherol, ascorbic acid. 2. Excess of caloric nutrition. 3. Stress. 4. Hypodynamia. 5. Radiation. 6. Long-term antibiotics therapy reduces C, PP. The increase of peroxide oxidation of lipids leads to the syndrome of lipid over-oxidation. The characteristic features are: 1. Membrane lesions, 2. Enzymes lesions, 3. Mitosis, 4. Accumulation of polymers. These features may prevail in different ways (in different diseases). 33 LESSON 9. Topic: Exchange and functions of lipids. Aim of the lesson: To study the mechanism of lipids synthesis, the exchange of cholesterol, regulation and pathology of lipids exchange. Questions for self-preparation: 1. Mechanism of higher fatty acids synthesis. 2. Cholesterol exchange. Inflow, synthesis and excretion of cholesterol. 3. Ways of cholesterol transformation in a cell: oxidation into bile acids, esterification, dehydrogenation. 4. The pathology connected with the derangement of cholesterol exchange: hypercholesterolemia, atherosclerosis, lipidic nephrosis. 5. Influence of poly-unsaturated fatty acids on the level of cholesterol in blood. 6. The exchange of ketonic bodies. Synthesis, biological role. Ketonemia, ketonuria. Initial test-control: 1. Answers to the questions of test- and programmed control (in written form). 2. Frontal oral test. Final test-control: 1. Solving of situational problems. 2. Reports on the topic. 3. Sizing up, signing of protocols. Fatty acids. Fatty acids are compounds with long chain of carbonaceous atoms. On one end of the chain they have COOH. There are more than 70 fatty acids in the organism. The most frequently met are fatty acids with 16, 18, 20 carbonaceous atoms. Unsaturated fatty acids are divided into: 1. mono-unsaturated (oleic acid), 2. poly-unsaturated, 3. eicosanoids (eicosa – 20 carbonaceous atoms). Saturated fatty acids: - Palmitic C15H31COOH - Stearic C17H35COOH Unsaturated fatty acids: 34 - Oleic C17H33COOH (18:1) - Linoleic C17H31COOH (18:2) - Linolenic C17H29COOH (18:3) - Arachidonic C19H31COOH (20:5) - Timnodonic C19H29COOH (20:5) from tissues of fish - Docosahexaenoic C21H31COOH (22:6) from tissues of fish “Eikonol” is a preparation for medical treatment of atherosclerosis, extracted from tissues of fish. It contains timnodonic and docosahexaenoic acids. Biosynthesis of fatty acids. Lipogenesis. Biosynthesis of fatty acids is called lipogenesis and it progresses in fatty tissue and in liver (in cytoplasm). The initial substrate in the process of lipogenesis is acetyl-CoA, the main sources of which are carbohydrates. Apart from carbohydrates, the source of acetyl-CoA may be: disintegration of fatty acids, disintegration of ketogenic aminoacids (leucine, isoleucine, lysine, tryptophan). The peculiarities of fatty acids biosynthesis. 1. The synthesis of fatty acids progresses in cytoplasm. 2. Although co-enzyme A is very important in the process of lipogenesis, the intermediate products of this process join the sulfhydric group of protein. This protein is known as acetylshifting protein (ACP); the reaction of fatty acids synthesis takes place on the basis of this (ACP) poly-enzymatic complex. 3. The assistance of the reaction of carboxylation with activated form of carbon monoxide, ATP, co-enzyme biotin in the process of lipogenesis is necessary. 4. The presence of regenerated NADF H2 is necessary. ASP is a poly-enzymatic complex. It has a specific structure formed with the help of 7 enzymes and acyl-shifting protein, which is in the centre of this complex. ASP is connected with the absorption of energy (in large quantities) which is generated with the help of oxidation processes. The transporters are acetyl-CoA+oxalacytatom – citrate into the cytoplasm. 35 The synthesis of fatty acids has the following stages: 1. Carboxylation acetyl-CoA. 2. Shift to ACP. 3. Condensation of acetyl and malonyl. 4. Regeneration of ketone into spirit. 5. Detachment of water. 6. Saturation of double linkage (bond). Deacylase detaches ACP during the last stage with the generation of palmitic acid. acetyl- СoA O H3C SCoA + CO2 carboxylase, biotin (H) malonil- СoA O ATP, Mn 2+ HOOC C H2 - HSСoA + HSACP - HSСoA transferrase transferrase HOOC C H2 S-ACP -HSAPB - CO2 synthetase O aceto-acetyl-ACP reduktase O H3C C C C H2 + NADP.H2 SAPB -ACP + NADP.H2 reduktase O H H3C C O dehydrotase C C H3C C C C H2 S-ACP - H2O H H S-ACP OH β-hydroxybutiril-ACP reduktase S-ACP malonil-ACP acetyl-ACP + NADP.H2 + HSACP O O H3C SCoA krotonyl-ACP O H3C C C C H2 H2 S-ACP butiril-ACP palmitat-ACP palmitic acid C15H31COOH 36 Generation of other fatty acids – unsaturated, poly-unsaturated. The generation of fatty acids with longer chain occurs either in microsomes or in mitochondria. It occurs with the help of successive adding of acetyl-CoA. Palmitate and generated in the process of its lengthening stearic acid (18:0) may undergo desaturation in endoplasmatic reticulum with the generation of mono-unsaturated acids: palmito-oleic (16:1) and oleic (18:1). Poly-unsaturated fatty acids – linoleic and linolenic are not synthesized in the organism of an animal (person). Metabolism of cholesterol. Cholesterol is a very important component in the organism of a person. An adult has 140150 g of cholesterol, 10 g of which are in blood. Cholesterol is in most tissues (liver, nervous tissue, red (blood) cells). Ethers of cholesterol are in blood and adrenal glands (N 3,9-5,2 millimole – in blood). Biological role. 1. It is a structural part of cell membranes. 2. It is used for the synthesis of bile acids. 3. Synthesis of steroid hormones. 4. Vitamin D is generated. 5. Turgor of skin. It has antitoxic function. Cholesterol inflows with food. Daily, 0,5 g of cholesterol is absorbed. The excess of it is removed with feces. Cholesterol may be synthesized in the organism (1 g). Active synthesis of cholesterol is in liver – 80%, intestine – 10%, skin – 5%. Synthesis of cholesterol. O O transferase 2 H3C SCoA acetoacetyl-CoA acetyl-CoA O Oxymethylglutaril -synthetase SCoA +acetyl-CoA C CH3 OH HOOC C C H2 H 3C - HSCoA O CH3 OH oxymethylglutarilreductase C C C C 2NADP ·H2 H2 H2 SCoA OH HOOC C C C CH2OH H2 H2 OH mevalonic acid β-oxy-β-methylglutaril-CoA cyclization cholesterol lanosterol squalen 37 Chemical structure of cholesterol H3C CH3 CH3 CH3 CH3 HO Ways of cholesterol transformation. 1. The main way of cholesterol transformation in the organism is its oxidation. 80% of cholesterol are oxidized in liver into bile acids. 3% are oxidized into steroid hormones. Thus, the solubility of cholesterol in water increases and this process helps to excrete from the organism. 2. The second way of cholesterol transformation in the organism is generation of ethers (esterification). Cholesterol ethers are 10% from total amount of cholesterol in the organism. Solubility reduces and this leads to accumulation of cholesterol in the organism. 3. Dehydration. UV Cholesterol (in position 7,8) 7 dehydrocholesterol (precursor of vitamin D3) Excretion of cholesterol. In order to excrete the constant level of cholesterol in the organism, 1,5 g of it should be excreted. 1. The main way of cholesterol excretion is oxidation into bile acids (up to 1 g a day). 2. With feces in the form of coprostanol – 200-300 mg. 3. With cast-off epithelium – 100 mg. 4. Synthesis of steroid hormones – 40 mg. 5. With urine – 1-2 mg. LDL transfer cholesterol into different cells. Receptors, binding protein-lipid complexes of LDL, not only support the cells with cholesterol, but also decrease the level of LDL in blood. The more receptors of LDL are on the surface of a cell, the more effectively they interact with LDL and the quicker cholesterol is excreted from blood. 38 Pathology connected with cholesterol. 1. Hypercholesterolemia – the increased amount of cholesterol in blood. 2. Atherosclerosis. 3. Lipidic nephrosis. 4. Stones in gallbladder. Ursodeoxycholic acid is used. Atherosclerosis – the changes in the inner layer of arteries. The changes are: accumulation of cholesterol lipids and its ethers in LDL, growth of fibrous tissue and changes in the medium layer of vessel wall. Atheroma is formed. It lessens the lumen of the vessel – violation of brain nutrition – memory impairment. Poly-unsaturated fatty acids cause the decrease of cholesterol in blood. This may be explained by the following: 1. Stimulation of excretion of cholesterol into bowels; 2. Activation of cholesterol oxidation into bile acids; 3. They assist in keeping blood vessels in norm. 4. They increase X-ray irradiation stability. Metabolism of ketonic bodies. Ketonic bodies are: Acetoacetic acid B-oxybutyric (B oxy-butyrate) Acetone In norm: 0,9-1,7 millimole/litre (1-3 mg/dl) Functions of ketonic bodies: 1. The source of energy (acetoacetate 33 ATP, B oxy-butyrate 21 ATP). 2. Regulatory (regulate the speed of lipolysis in adipose cells). 39 Synthesis of ketonic bodies . O O transferase 2 H3C SCoA C C H2 H 3C - HSCoA Oxymethylglutaril -synthetase O acetoacetyl-CoA SCoA +acetyl-CoA acetyl-CoA HOOC OH CH3 O C C C C H2 H2 SCoA OH O oxymethylglutarilliase H3C -acetyl-CoA Dehydrogenase β-oxy-β-methylglutaril-CoA C COOH H2 acetoacetic acid decarbo- -CO2 xylase NADH2 OH H3C C C COOH H2 H O H3C C CH3 acetone B-oxybutyric Ketonic bodies transfer from liver into peripheral tissues: skeletal muscles of heart. Brain absorbs ketonic bodies if there is a lack of glucose. In peripheral tissues, ketonic bodies are oxidized and energy is generated. Pathology connected with ketonic bodies. 1. Ketonemia – accumulation of ketonic bodies in blood. 2. Ketonuria – acetonic bodies are in urine, no ketonic bodies. 40 LESSON 10 Topic: Exchange and functions of lipids. Aim of the lesson: To study the catabolism of fats, phospholipids, regulation and pathology of lipids exchange. Questions for self-preparation: 1. Synthesis and biological role of neutral fats. 2. Chemical structure, biological role of phospholipids (phosphatidylcholine). 3. The role of thromboxane, prostacyclins, leukotrienes in pathogenesis of a disease. 4. Sphingolipids, biological role. 5. Transport forms of lipids. The structure of chylomicrons and lipoproteins, their chemical composition, their biological role. 6. The regulation of lipids exchange. 7. The pathology of lipids exchange: lipidoses – Neeman-Pick’s disease, Ghoshe’s disease, Tei-Saks’s disease, fatty infiltration of liver (lipotropic substances). Biosynthesis of triacylglycerol (neutral fats). Biosynthesis of triacylglycerol progresses in liver, mucous tunic of intestine, fatty tissue, Biosynthesis lungs and other organs. of triacylglycerol (neutral fats). Biosynthesis of triacylglycerol progresses in liver, mucous tunic of intestine, fatty tissue, lungs and other Glycerol-3-phosphate playsorgans. the leading role in the biosynthesis. Glycerol-3-phosphate plays the leading role in the biosynthesis. Glycerineph Glycerine osphokinas H2C OH e (in intestine, kidneys) ATP HC OH + Dioxyacetonephosphate (in muscles, fatty tissue) dehydrogena NADH2 se 2 C17H33COSCoA C OPO3H2 H2 Acyl-CoA Glycerol-3-phosphate O H2C O C C17H33 O HC O C C H 17 33 phosphatidsynthetase C O PO3H2 -2 HS-CoA H2 Phosphatase +H2O -H3PO4 phosphatidic acid H2C O COC17H33 HC O COC17H33 C OH H2 transferase O + C15H31 SCoA Acyl-CoA 1,2 – diacylglycerol H2C O COC17H33 HC O COC17H33 C O COC15H31 H2 triacylglycerol Activated fatty acids are formed under the influence of acyl-CoA-synthetase, which is localized in microsomes. After that, phosphatidic acid is dephospholized under the influence of 41 phosphatase and 1,2-diacylglycerine is generated. The 3rd molecule of activated fatty acid is added. This way of biosynthesis of triglycerides progresses in liver and fatty tissue. Also, the way of biosynthesis in bowels is known (secondary way). Molecules of monoglycerides are used as precursors. Metabolism of phosphoglycerides. These substances are in liver, heart, lipid layer of membranes. The formulas are: phosphatidyl – serine, p- ethanolamine, p- choline. Functions: 1. They are in the composition of membranes and they take part in selective permeability (in ions transport and organic substances transport). 2. P- choline is the component of surfactant (lines lung alveoli) and prevents alveoli from lung collapse after the 1st inspiration. 3. It takes part in blood coagulation (neutral PL increase blood coagulation; acid PL decelerate blood coagulation [p- serine decelerates the formation of thrombokinase and decelerates blood coagulation, decelerates fibrin generation]). 4. Prevents from fat deposit in liver, that is has lipotropic effect (methionine, serine, glycine, B12, folic acid, lipocain B15). 5. Take part in pathogenesis of atherosclerosis. The risk of atherosclerosis when having enough PL is very low phosphatidylcholine 1-1,5 in norm cholesterol. 6. In pathogenesis of bronchial asthma. Chemical structure of phosphatidylcholine O CH2 - O - C - R1 O R2 - C - O - CH CH3 CH3 O OH CH2 - O - P - O - CH2 - CH2 - N - CH3 42 Detachment of arachidonic acid. It is used (in norm) as energy substrate, and to form prostaglandin. It has another function in disease. Phospholipids phospholipase A2 (activate immune influence toxins, hypoxia) Arachidonic acid Prostaglandins Thromboxane Leukotrienes Prostacyclin Prostaglandins: 1. Affect the contraction of eye muscles. 2. Assist in secretory function of stomach. 3. Take part in inflammatory response. 4. Modulate the hormones activity. 5. Affect the hemodynamics of liver. 6. Regulate (independently) hab-dab. Prostacyclins – are generated in the walls of blood vessels of heart, uterus, mucous membrane of stomach. 1. Relax smooth muscular system. 2. Assist in fibrinolysis and prevent blood coagulation. Thromboxanes are antagonists of prostacyclins; they are generated in thrombocytes, in brain; they assist in blood coagulation. 1. They cause aggregation of thrombocytes. 2. They have vasoconstrictive action. Accumulation of thromboxanes may cause thrombosis, atherosclerosis. Leukotrienes are in white (blood) cells, macrophages. 1. They cause contraction of smooth muscles of respiratory tract. 2. They stimulate secretion of glycoproteins; increase the quantity of mucus in respiratory tract. 3. They take part in allergic and immunological reactions. 43 4. They improve the permeability of vessels. Heavy breathing (when a person has bronchial asthma) is connected with the action of leukotrienes. Atrophic arthritis is also caused by leukotrienes. Pathology of phosphoglycerides. Fatty infiltration of liver (fatty degeneration of liver).It is the overflow of liver cells with neutral fat, which was not disintegrated and not removed. First of all, fat drops are accumulated, then the cells overflowed with fat are destroyed, cysts are generated, connective tissue spreads around cysts, and fatty degeneration develops. This pathology occurs as the result of synthesis derangement of very low-density lipoproteins (VLDL). These lipoproteins transport endogenous neutral fats from liver into blood and after that into different tissues. Phospholipids (PL) are in the composition of VLDL. Therefore, in the case of PL synthesis derangement, VLDL are not generated and neutral fats are stored in liver. Lipotropic substances take part in PL synthesis: methionine (in curds), unsaturated fatty acids, choline, B12, B15, folic acid. Sphingolipids are: 1. Sphingomyelin; 2. Cerebrosides (in white substance), 3. Gangliosides (in gray substance of brain). Their biological role: 1. Structural function. They are in the outer layer of plasmatic membrane, they take part in intercellular contacts. 2. They are receptors of neuromediators. 3. Some of the glycosphingolipids are antigens defining blood group. Pathology (lipidoses). These are genetic inherited diseases, when incomplete disintegration takes place (because of the absence of enzyme). 1) Neeman-Pick’s disease is very seldom, there are 6 types. Accumulation of sphingomyelin in internals and nervous tissues. There is no enzyme sphingomyelinase. 2) Ghoshe’s disease is often met – cerebrosidosis (the absence of enzyme cerebrosidase). 3) Tei-Saks’s disease – gangliosidosis (the absence of enzyme gangliosidase). 44 Lipoproteins (LP) – they transport different lipids. Chylomicrons are synthesized in intestine. Their function is transport of exogenous TAG from intestine into blood, after that to different organs. VLDL (very low-density lipoproteins) are synthesized in liver. Their function is transport of endogenous TAG from liver to different organs. LDL – low-density lipoproteins. Their function is transport of cholesterol from liver to different tissues. HDL (a-LP) are synthesized in liver. Their function is transport of cholesterol from tissues into liver. Albumin + VHDL (very high-density lipoproteins). Their function is transport of free fatty acids to tissues. VLDL and LDL are atherogenic. They are not stable in vascular system, they may sediment at the walls of blood vessels, they are slowly destroyed – the basis for atherosclerosis plague. HDL – antiatherogenic fraction. Regulation of lipids exchange. Hormones which may stimulate lipolysis. Adrenaline stimulate TAG lipolysis, accelerate Noradrenaline the release of free fatty acids Glucagon from fatty tissue and increase their ACTH concentration in plasm. Thyrotropic hormones Insulin. Antagonist intensifies: 1. lipogenesis; 2. TAG biosynthesis. In fatty tissue, insulin inhibits the activity of hormone of sensitive lipase. The result is the lessening of release of free fatty acids, glycerine. 45 LESSON 11 Theme: Exchange and functions of lipids. Aim of the lesson: To work out skills of using the knowledge of exchange and functions of lipids in the practical work of a doctor. Questions for self-preparation for the test “Exchange and functions of lipids”. 1. Characteristics and classification of lipids. The role of lipids in the organism. 2. Fatty acids. The role of unsaturated fatty acids. 3. The structure of mono-, di-, triacylglycerol. Biological role. 4. Phosphatidylcholine, its chemical structure and its role in the organism. 5. Cholesterol, biological role, chemical structure. 6. Digestion and absorption of lipids. 7. The role of bile in the digestion of lipids. 8. Transport forms of lipids: the structure and role of chylomicrons and lipoproteins. 9. Modern conception of intercellular disintegration of fatty acids (B-oxidation of higher fatty acids). Chemism of the process. 10. Ketonic bodies. Chemical structure. Synthesis of ketonic bodies. Biological role. Ketonemia, ketonuria. 11. Synthesis of neutral fats. 12. Conception of synthesis of fatty acids in the organism. The peculiarities of the synthesis (the role of biotin and acetyl-shifting protein in this process). 13. Biological role of phospholipids. The role of leukotriens, prostocyclines, thromboxane in pathogenesis of bronchial asthma, atherosclerosis. 14. Fatty infiltration of liver. Lipotropic substances. 15. Cholesterols exchange. Composition of cholesterol in tissues, organs, blood. 16. Biosynthesis of cholesterol, chemism of forming of B-oxy, B-methyl, glutaril-CoA, mevalonic acid. 17. Ways of transformation of cholesterol into bile acids, esterification, dehydration. Cholesterol excretion. 18. Regulation of lipids exchange. 19. Derangements of cholesterol exchange: atherosclerosis, hypercholesterolemia (lipidic nephrosis). Influence of poly-unsaturated fatty acids on the level of cholesterol in blood. 20. Pathology exchange of sphingolipids (Neeman-Pick’s disease, Ghoshe’s disease, Tei-Saks’s disease). 21. Peroxidation of lipids. 46 LESSON 12 Theme: Exchange and functions of amino acids. Aim of the lesson: To work out the skill of knowledge of amino acids exchange (in the practical work of a doctor). Questions for self-preparation: 1. Biological role of proteins. Essential amino acids. 2. Nitrous balance, its types, “Wear” coefficient. Physiological minimum. The norms of protein in nutrition. 3. Digestion and absorption of proteins in gastrointestinal tract. Bacterial decay of protein in bowels. 4. The ways of amino acids usage in the organism after absorption. 5. Transamination, its biological importance. Diagnostic importance of detecting transaminase activity. 6. Deamination of amino acids. 7. Decarboxylation of amino acids. Proteins are high molecular compounds which contain nitrogen. They consist of amino acids linked by peptide bonds, they are life media. Functions of proteins. 1. Structural. 2. Catalic (fermentation) function. All the ferments are proteins (pepsin, trepsin, amylase, and so on). 3. Regulatory. 4. Transport function. Hemoglobin carries oxygen from the lungs to the tissues and carbon doxide rom the tissues to the lungs. 5. Defense function. -Anti-bodies of blood serum are formed in response to entry of foreign substances into the organism. 6. Contraction function. Actin and myosin are proteins of the muscular tissue. 7. Receptor function. 8. Energy. The condition of protein exchange in the organism depends not only on the quantity of consumed protein, but also on its qualitative composition. Those proteins which are closer (according to their amino acid composition) to the amino acid composition of the organism, are better hydrolyzed in the 47 gastrointestinal tract. That means that they are better absorbed. These proteins are more biologically valuable. They contain all essential amino acids. Such proteins are animal proteins: meat, fish, milk, etc. Not all amino acids may be synthesized in the organism. Those which can’t be synthesized are called essential (indispensable). A grown-up person has 8 essential amino acids: leucine, isoleucine, lysine, threonine, tryptophan, phenylalanine, cystine and valine (arginine and histidine are de bene esse essential). The bulk of nitrogen in food is in proteins. In the process of protein exchange, nitrogen is excreted from the organism in the form of nitrous substances. In order to understand the process of protein exchange, one should know the definition of nitrous balance. Nitrous balance is the difference between the quantity of absorbed nitrogen and the quantity of excreted nitrogen in the form of final nitrous products. Types of nitrous balance: 1. “positive” – if the quantity of excreted nitrogen is less than the quantity of absorbed nitrogen. That means that nitrogen is stored in the organism (it happens in norm in the organism of a pregnant woman or in the growing organism). The accumulation of nitrogen in different tissues and organs takes place. 2. “zero” – nitrous balance. 3. “negative” – if the quantity of excreted nitrogen is more than the quantity of absorbed nitrogen. The process of disintegration of protein in tissues and organs takes place. It often happens when a person has diseases (pancreatic diabetes, diseases of kidneys, burns) connected with intensive disintegration of proteins in tissues (old age). Wear coefficient – is the result of daily disintegration of tissue protein (23,2 g). It was detected with the help of volunteers. The constant quantity of nitrogen began to excrete after 8-10 days of protein-free diet (53 mg a day per 1 kg of body weight). Having detected the daily physiological minimum of protein (nitrous balance is set in the organism) – 30-45 g – the scientists substantiated and recommended the daily need of protein, which is 100-120 g. But this need depends on many factors: age, activity, physiological and pathological conditions, etc. 48 Digestion of proteins in gastro-intestinal tract. Endopeptidases: pepsin, rennin (in a child’s organism), gastricsin, trypsin, chemotrypsin, elastase – are synthesized in non-active form. The mechanism of activation is connected with the detachment of terminal peptide. This leads to the formation of three-dimensional structure and generation of the active centre of enzymes. Trypsin breaks peptide bonds formed with the help of basic amino acids: lysine and arginine; pepsin breaks the bonds between cyclic amino acids; rennin coagulates milk. Exopeptidases: Carboxypeptidases are synthesized as precursors in pancreas. They contain Zn; they break peptide bonds formed with the help of terminal aromatic amino acids. Under the influence of proteolytic enzymes amino acids are generated. They are absorbed in bowels, either diffusely, or by means of active transport. Bacterial decay of protein in bowels: Under the influence of micro flora of the lower part of bowels, some amino acids may transform into amines, fatty acids, spirits, phenols, hydrogen sulphide and so on. Putrescine is formed in the process of ornithine decarboxylation, cadaverine is formed from lysine. They are in the group of cadaveric alkaloids. They are excreted from the organism through kidneys with urine (almost in unchanged condition). The excretion of putrescine and cadaverine with urine is observed when a person has cholera, dysentery, etc. Phenol and cresol are formed from tyrosine. After absorption, they are rendered harmless in liver. It is because of the bond with H2SO4 or glucuronic acid. As a result, binate sulphuric-, phenol- or cresol-glucuronic acids are formed. They are also called ether-sulfuric acids and they are constant components of urine. Sulfuric acid joins as an active form and forms phosphoadenosine-phosphosulfate (PAPS), glucuronic acid – uridinediphosphate of glucuronic acid (UDPGA). Indole and skatole are formed in the process of decarboxylation from tryptophan. They condition the specific smell of feces, they are poisonous substances and they are rendered harmless in liver. Ways of using amino acids after absorption: 1. Synthesis of specific tissue proteins, blood plasma, enzymes, hormones. 2. Synthesis of carbohydrates (gluconeogenesis). 3. Synthesis of lipids. 49 4. Synthesis of histamine, serotonin, kreatine, porphyrins, choline, adrenalin, purine and pyrimidine nucleotides. 5. Synthesis of urea. 6. Unused amino acids are disintegrated with the energy liberation (10-15%). General ways of amino acids disintegration: 1. Transamination.. 2. Deamination 3. Decarboxylation. Transamination is the process of aminogroup transference from aaminoacid to ketoacid with the help of transaminases enzymes, the co-enzyme of which is phospho-pyridoxal (B6). The reaction has 2 stages: 1) CH3 HC NH2 + COOH ALT FP - C=O C H PA + FP - CH2-NH2 phospho-pyridoxamine COOH 2) FP - CH2-NH2 O COOH phospho-pyridoxal Alanine CH3 (CH2)2 + phospho-pyridoxamine C O COOH a-ketoglutarate COOH FP - C=O + H phospho-pyridoxal (CH2)2 CH NH2 COOH glutamate The reaction of transamination is catalysed by highly active aminotransferases: alanineaminotransferase and aspartateaminotransferase. They have substrate specificity. In the diseases accompanied by necrosis the marker (organospecific) enzymes from damaged cells enter blood flow in a great amount; their activity level increases, hyperfermentaemia appears. Determination of marker enzymes activity level in blood serum is of clinical importance in diagnostics and prognosis of some diseases. So, by myocardial infarction AsT activity level increases; by prostate gland cancer - that of acid phosphatase; virus hepatitis - that of AIT. Deamination is the process of loosing of amino acid amino group. Only glutamic acid undergoes in oxidizing deamination in the organism, because there exists active enzyme glutamate dehydrogenase (GDG), which may split it. 50 deamination in the organism, because there exists active enzyme glutamate dehydrogenase (GDG), which may split it. Other amino acids undergo indirect deamination. Other amino acids undergo indirect deamination. Oxidizing deamination. COOH COOH (CH2)2 GDG (CH2)2 CH NH2 NAD NADH2 COOH COOH (CH2)2 + H2O C NH C COOH COOH + O NH3 ammonia imine-glutaric acid α-ketoglutaric acid 3 ATP glutaminic acid Indirect deamination is the process of deamination by Respiratory chain means of transamination. In the process of the first stage, Indirect deaminationwith is the process of deamination acid by means of transamination. In the transamination a-ketoglutaric with the help of process of the first stage, transamination a-ketoglutaric of acidglutamic with the help of transaminases transaminases (with thewith formation acid) takes (with the formation of glutamicacid acid) takes (with the help of active GDG) place. Glutamic (withplace. theGlutamic help acid of active GDG) deaminate deaminates and ammonia isisgenerated. and ammonia generated. 1). Transamination COOH CH3 + HC NH2 COOH C O CH3 C (CH2)2 COOH Alanine Transaminase FP - C=O H phospho-pyridoxal COOH O COOH PA + (CH2)2 CH NH2 COOH C= O H Ф glutamateП a-ketoglutarate 2). Oxidizing deamination GDG COOH (CH2)2 CH NH2 NAD NADH2 COOH glutamate COOH + H2O (CH2)2 C NH COOH 3 ATP COOH (CH2)2 C + O NH3 ammonia COOH a-ketoglutarate imine-glutaric acid 51 Decarboxylation is the process of detachment of CO2 group. Decarboxylases take part in this process. Phospho-pyridoxal (B6) is non-protein component of decarboxylases; it is also phosphoric derivative of vitamin B6. As a result, biogenic amines are formed (serotonin, histamine, GABA). They have strong pharmacological activity. HO N H H C C COOH H2 NH2 decarboxylase HO (phospho-pyridoxal) serotonin 5-oxy-tryptophan N H H2 C + CH2 NH2 CO2 Serotonin has vasoconstrictive action. It takes part in the regulation of arterial pressure, the body temperature, breath, allergy development, toxicosis of pregnancy. N N H H C C COOH decarboxylase H2 NH2 (phospho-pyridoxal) histidine N C C NH2 H2 H2 + CO2 N H histamine Histamine has vasorelaxant action. It causes vasorelaxation in the inflammation focus, it increases the inflow of white (blood) cells (activation of body defences), it also increases the secretion of hydrochloric acid in stomach and take part in allergic and immunological reactions. Histamine is considered to be pain mediator. H HOOC (CH2)2 C COOH NH2 HOOC (CH2)2 C NH2 H2 + CO2 GABA GABA has inhibitory action on the CHS activity. In clinic it is used in the treatment of several diseases of CNS. Biogenic amines can’t be accumulated, because it may cause serious dysfunctions in the organism. That’s why biogenic amines are rendered harmless in liver with the development of appropriate aldehydes and with the development of ammonia with the help of enzymes of monoamino- and diamino-oxydases. These inhibitors are used in the treatment of schizophrenia, essential hypertension. 52 LESSON 13 Theme: Exchange and functions of amino acids. Aim of the lesson: To work out the skill of knowledge of amino acids exchange (in the practical work of a physician). Questions for self-preparation: 1. The formation of ammonia in the organism. 2. Ways of ammonia neutralization. Glutamine and asparagine. 3. Biosynthesis of urea as the main mechanism of prevention of ammonia accumulation. 4. Hyperammoniemia. 5. Synthesis of creatine, creatine-phosphate, the importance of the synthesis for the organism. 6. Reasons of creatinuria. The ways of ammonia formed in the organism: ways of ammonia formed in the organism: 1. The Deamination of biogenic amines. 1. Amino acids deamination (oxidizing and indirect). 2. Oxidizing Disintegration of pyrimidine deamination of biogenicbases amines.(uracil, thymine, cytosine). 3. Disintegration pyrimidine bases (uracil, thymine, cytosine). 3. Amino acidsofdeamination. 4. Deamination of purine bases (guanine and adenine). 4. ItDeamination of purine (guanine adenine). but enters into a reaction is a toxic compound, that bases is why ammonia is and not accumulated with glutamic or asparaginic acids and indifferent transport form (glutamine or asparagine) is It is a toxic compound, that is why ammonia is not accumulated but enters generated. The norm of ammonia in blood is 25-40 mcmol/l Hyperammoniemia is increase ammonia in blood.acids It leads to indifferent womiting, nausea, cramps, into a reaction with glutamicofor asparaginic and edema of brain. transport form (glutamine or asparagine) is generated. H HOOC (CH2)2 C NH2 glutamic acid HOOC C H2 COOH H C NH2 COOH H H2NOC (CH2)2 C + NH3 ATP - H2O + NH3 ATP - H2O glutamine H2NOC C H2 H C NH2 COOH NH2 COOH asparagine asparaginic acid The ways ammonia usage in the organism: 1. Synthesis of urea – the basic way of ammonia neutralization. 2. Synthesis of amino acids from the corresponding ketoacids. 53 CH3 C CH3 ATP O HC NH2 + NH3 COOH COOH PA alanine 3. Synthesis of ammonium salts in kidneys. 4. Synthesis of purine and pyrimidine nucleotides. Synthesis of urea Crebs and Genzeleit proved that urea synthesis is a cyclic process in which ornithine plays catalytic role. The initial reaction of this cycle is synthesis of carbamoyl-phosphate. NH2 2ATP СО2 + NH3 carbon- ammonia dioxide + 2АDP + H3PO4 C ~ PO3H2 O carbamoyl-phosphate H + H2N (CH2)3 C COOH NH2 O C O~ H2O3P citrullin + asparaginic acid NH2 carbamoyl-phosphate ornithine arganine-succinic acid arganine fumaric acid O H2N C NH2 ornithine Crebsis cycle urea Urea is an indifferent (for the organism) compound. The main place of its generation in the organism is liver where there are enzymes of urea-formation. There are all enzymes of urea synthesis in brain except carbamoyl-phosphatase, because urea is not formed there. Dysfunction of liver leads to the decrease of urea-formation and the contents of urea in blood and its excretion with urine goes down. The norm of urea in blood is 3,3-8,3 mmole/l. Synthesis of creatine. The final product of amino acids decomposition in the organism (along with urea) is creatinine. It is formed in the muscular tissue from creatine-phosphate. Creatine and creatine-phosphate are very important nitrous substances in muscles. They take part in chemical processes connected with ATP-resynthesis which is the participant of muscle contraction. Creatine synthesis also progresses in kidneys and liver with the participation of 3 amino acids: 54 the participation of 3 amino acids: arginine glycine methionine creatine CH3 rest H2N C N C COOH H H2 +ATP NH creatine PO3H2 CH3 It goes into muscular tissue activity N C N C COOH +ADP H H H2 NH creatine-phosphate CH3 + ATP N C N C C O H H H2 NH creatinine This reaction is one of the ways of ATP -resynthesis; it progresses in the muscle during activity. Creatinine is removed in the composition of urine. The contents of creatinine in urine depends on the development of muscle bulk. It should be underlined, that urea, creatinine and ammonium salts are the final products of amino acids exchange. Their detection in urine is a diagnostic index. In norm, the quantity of excreted urea in the organism of an adult is about 30 g, creatinine – 1,52,4 g, ammonium salts – 0,5-1,2 g. The quantity of creatinine in urine increases during proteins decomposition, extensive muscle activity, acromegalia, hypothyroidism. Creatine is not usually detected in urine in an adult (norm). Creatine in urine is connected with avitaminosis of vitamins C and E, diabetes, starvation and also with diseases which are connected with muscular tissue decomposition. 55 TASK TO LESSON 14 Theme: Exchange and functions of nucleoproteins. Aim of the lesson: To work out the skill of knowledge of nucleoproteins exchange in the practical work of a doctor. Questions for self-control: 1. Digestion and absorption of nucleoproteins in gastro-intestinal tract. 2. Biosynthesis of purine and pyrimidine nucleotides in tissues. 3. Disintegration of purine and pyrimidine nucleotides into final products in tissues. 4. Pathology of exchange amino acids (phenylketonuria, albinism, alkaptonuria,). 5. Pathology of exchange nucleotides (podagra). Nucleoproteins are complex proteins which consist of proteins and nucleic acids. There are 2 types of nucleoproteins which are different from each other in composition, size and physicochemical properties: deoxyribonucleoproteins (DNP) and ribonucleoproteins (RNP). Nucleoproteins are digested in gastro-intestinal tract and form some low-molecular products which are absorbed in the bowels. The 1st stage is the detachment of nucleic acid from the protein part of nucleoprotein. This break of the bonds between protein and prosthetic group takes place both in stomach and bowels. In stomach this process is due to the action of pepsin, in bowels – action of tripsin. After that, protein in gastro-intestinal tract undergoes common transformations. Disintegration of nucleic acids, contained in food, is due to the digestion in bowels under the influence of nucleases: RN-ase and DN-ase. Absorption of the products of nucleic acids hydrolysis takes place in the form of nucleotides and nucleosides, as well as nitrogen bases, pentose and remnants of phosphoric acid. Biosynthesis of purine mono-nucleotides. The initial combination of the synthesis is D-ribose-5-phosphate, which is the product of pentosephosphate cycle and on which pyrophosphate group ATP is transferred. 5phosphoriboside-1-pyrophosphate (PRPP) is formed and it interacts with glutamine which is the donor of NH2-group. As the result of this, β-5-phosphoriboside-amine is formed. This stage is the basic one in the synthesis of purines. Then, the molecule of glycine attaches to the free NH2group of β-5-phospho-riboside-amine and glycineamidribonucleotide is formed. In several stages, the first purine nucleotide inosinemonophosphate (IMP) is formed, from which other nucleosidephosphates are synthesized. 56 the first purine nucleotide inosinemonophosphate (IMP) is formed, from which other nucleosidephosphates are synthesized. PO3H2 H H2 O C O ribose-5phosphate ОН pyrophospho- PO H O C 2 O + O 3 2 kinase O P O PO3H2 ATPAMP PRPP OH CONH2 (CH2)2 HC NH2 COOH + H2O - 2H3PO4 glutamine H2 PO3H2 O C O NH2 + glycine + glutamine + CO2 + aspartate + THFA + ATP B-5-phospho-riboside-amine O HNto be continued N N N H2 PO3H2 O C O AMP GDP GTP te asparta AT P gl u tam ADP ine IMP GMP Biosynthesis of pyrimidine nucleotides. The initial combinations of this process are Biosynthesis of pyrimidine nucleotides. carbamoylphosphate and aspartic acid. Through the long chain The initial combinations of this process are carbamoylphosphate and aspartic acid. Through the of reactions, withwith thethehelp thesecombinations, combinations, long chain of reactions, help of of these uridinemonophosphate (UMP) and uridinemonophosphate (UMP) and other pyrimidine nucleotides other pyrimidine nucleotides are formed. NH СО2 + NH3 (from glutamine) 2ATP ADP -H3PO4 COOH CH2 O C PO3H2 carbamoylphosphate H2N-CH 2 PRPP PRDP aspartate HN -CO2 O N N COOH H2 H PO3H2 O C O orotic acid O COOH O O HN + COOH + glutamine urydilic acid +T HF CMP A TMP 57 Disintegration of pyrimidine nucleotides. The initial stages of this process are catalysed by specific enzymes. The final products are: (CO2 + NH3) urea + β-alanine. NH2 NH2 N N N O O phosphatase O N +H2O H2 -H3PO4 HO C O N H2 PO3H2 O C O -NH3 +H2O -ribose O N H2 HO C O uridine cytidine CMP O NADFH2 HN O NADF N H COOH NH2 CH2 CH2 + C N CO NH2 H2 H CH2 urea COOH β-ureidopropionic acid uracil NH3 + CO2 β-alanine Disintegration of purine nucleotides. Adenosine and guanosine, formed in the process of hydrolysis of purine nucleotides, undergo enzymatic decomposition with the formation of the final product – uric acid, excreted from the organism with urine. NH2 N N N N H2 PO3H2 O C O + H2O Phosphatase - H3PO4 N N N H2 HO C O AMP adenosine OH xanthineoxidase H2O2 HO N N xanthine N + H2O -NH3 OH N N N N H2 HO C O - ribose N N N N H hypoxanthine inosine OH N H2O + O2 OH NH2 N H H2O + O2 xanthineoxidase H2O2 HO N N N N H OH uric acid The formation of ureic acid progresses in liver. In norm its contents in blood is 0,180,24 millimole/l, and in urine – 0,7g in a day. The changes of these indices occur when a person has some diseases. 58 Pathology of exchange of nucleotides. Podagra (gout) – is the disease connected with the derangement of nucleic acids exchange. In cartilages, tendons, articular corpuscles, sometimes in kidneys, skin and muscles the crystals of ureic acid are stored. Around these deposits, the inflammation is formed and granulation bank develops which rounds the mortified tissue and arthroliths are formed (in joints of fingers and toes, auricular cartilages). These lead to deformation and pains in joints. Usually, the sick have atherosclerosis and essential hypertension. The large concentration of ureic acid is observed in their blood – hyperuricemy. During several days, before the attack of podagra, the excretion of water and sodium chloride with urine is increasing, that is, the water-salt metabolism is shifted. As a result of this, the concentration of ureic acid in blood and its deposits in tissues and kidneys are increasing. Pathology of exchange of amino acids. Phenylketonuria – is the disease connected with the absence of enzyme phenylalaninehydroxylase. In this case phenylalanine transforms not into tyrosine, but into phenylpyruvic acid. Its accumulation leads to the disease when children have backward mental development (oligophrenic person). There is much phenylpyruvic acid in the urine of these children. From amino acid of tyrosine are formed: thyroxin, noradrenaline, adrenaline, melanin and others. Albinism – is the inherited disease, which is connected with the absence of enzyme tyrosinase. Tyrosine doesn’t transform into dioxyphenylalanine (DOPA), that’s why the pigment of melanin is not formed. Alkaptonuria – is the disease connected with the absence of the enzyme- oxidase homogentisic acid. It is excreted with urine which becomes red in contact with air. One of the characteristic derangements of nitrogen exchange is protein deficiency which is the consequence of not only protein deficit, but also of other severe diseases even when a person gets enough protein with food. The reasons for protein deficiency: little protein in food or bad adoption of food proteins, esophageal obstruction, pathology of digestive system. The results of these pathologies are: negative nitrous balance, hypoproteinemia (the decrease of protein concentration in blood serum to 30-50 g/l, in norm – 65-85 g/l) and derangement of colloidosmotic exchange and water-salt metabolism (development of edema). When a person has a severe form of alimentary dystrophy, for example, kwashiorkora, the disease which is wide spread among the children of the developing countries. The following is observed: liver injuries, stasis, succulence, muscle atony, the decrease of body resistance to infections. The disease often has fatal outcome. When a person has protein deficiency, the following symptoms are observed: the decrease of the intensity of the processes of deamination, transamination, biosynthesis of amino acids and synthesis of urea in liver. These derangements are conditioned by the dysfunction of enzymatic functions of liver and other organs. The result of this is the accumulation of amino acids in blood, the excretion of free amino acids with urine (up to 10-20g per day, in norm – 1 g per day) and the decrease of formation and excretion of urea with urine. 59 LESSON 15 Theme: Exchange and functions of proteins. Test-lesson on the topic: Exchange and functions of proteins. Aim of the lesson: To work out the skill of knowledge of amino acids exchange in the practical work of a doctor. Questions for self-control: 1. Biological role of proteins. Contents of protein in essential food stuffs. 2. Nitrous balance. “Wear” coefficient. Physiological minimum. The norms of protein in nutrition. 3. Biological importance and aminoacid composition of protein. Substitutional and indispensable amino acids. 4. Digestion of proteins in gastro-intestinal tract. The reasons for tissue proteins decomposition. Cathepsins. 5. Transformations of amino acids under the influence of bowels microflora. Neutralization of poisonous products of the exchange. 6. Ways of amino acids after absorption. 7. The mechanism of oxidizing deamination of amino acids. 8. Transamination of amino acids (A. Braunstein, I. Kritsman). The importance of detecting of transaminase activity. The connection between transamination and deamination (indirect deamination). 9. Decarboxylation of amino acids. The formation of biogenic amines: histamine, serotonin, gamma-aminobutyric acid (GABA), biological role and their inactivation. 10. The formation of ammonia and its ways in the organism. Glutamine and asparagine. 11. Biosynthesis of urea. Hyperammoniemia. 12. Creatinine, creatine, creatine-phosphate, biological role. Reasons of creatineuria. 13. Nucleoproteins. Biological role. Composition and properties of RNA, DNA. 14. Digestion and absorption of nucleoproteins in gastro-intestinal tract. 15. Synthesis and decomposition of purine nucleotides. 16. The pathology of protein metabolism. Protein deficiency. The mechanism of formation of the inherited derangements of amino acids exchange (phenylpuryvic oligophreny, alkaptonuria, albinism). 17. Synthesis and disintegration of pyrimidine nucleotides. 18. The pathology of exchange of nucleoproteins. Hyperuricemy. Podagra. 19. Making the biuret test of protein presence. 20. Detecting of sulphur in sulphur-containing amino acids. 60 LESSON 16 Theme: Biochemistry of blood. Aim of the lesson: To work out the skill of using the knowledge of biochemistry of blood in the practical work of a doctor; to form the skill of counting the quantity of protein and albuminous fractions with the help of refractometric method and electrophoresis method. Questions for self-preparation: 1. What is blood and what are its functions? 2. Blood proteins and their role in the organism. 3. Hypoproteinemia, hyperproteinemia. 4. Dysproteinemia, paraproteinemia. 5. Evaluation of importance of blood examination, of detecting of total protein and proteins fractions (in clinical practice). 6. Methods of quantitative detecting of proteins and proteins fractions (refractometry). Annotation of the theme: Blood is the inner medium of the organism. It supports the integration of tissues and organs and eases the contacts of the organism with the external environment. The functions of blood are: respiratory, transport, excretory, protective, regulatory and others. The total content of protein in blood is 65-85 g/l (in the organism of an adult). In the process of electrophoresis, 5 main fractions may be observed on paper: albumin, a1, a2, β and y-globulin. The molecular weight of albumin is 68-70 thousand of Dalton. Normally, 40-50 g/l of albumin are in blood serum. The main functions are: 1. Keeping of oncotic pressure. 2. Transport of water-insoluble substances (lipids, bilirubin, medications: dicumarin, aspirin and others). 3. Keeping of blood pH. 4. Regulation of blood viscosity. The molecular weight of globulin is 160-180 thousand of Dalton. Its total content in blood is 20-30 g/l. 61 a1-globulins are: inhibitors of proteinase, retinol-binding protein. a2-globulins are: ceruloplasmin (the protein that transports copper and keeps its normal level in tissues), haptoglobin (the complex of protein a2-globulin and haemoglobin which is generated after its destruction in red (blood) cells. In this fraction are also those proteins that take part in blood coagulation, e.g., prothrombin. The fraction of B-globulin: transferrin (transports iron), C-reactive protein, the 3rd and 7th factors of blood coagulation. Antibodies are in the fraction of y-globulin. Fibrinogen. Its content in blood is 2-4 g/l, molecular weight is 330 thousand of Dalton. Fibrinogen takes part in blood coagulation. Normally, the chemical composition of blood is constant, but it may show even the minute changes of the metabolism in the organism. Taking into account the accessibility of this biological fluid and the opportunity of multiplicity of biochemical blood examination, a doctor may set a diagnosis on the basis of blood analysis or make a prognosis of a disease or control the efficiency of treatment. Hypoproteinemia is the reducing of protein content. It may be observed when there is the dysfunction of liver, kidneys, in starvation, bleedings, malignant neoplasms. Hypoproteinemia is accompanied by the formation of edemas. The reasons for hyperproteinemia are often connected with the loss of water (cholera, dysentery, intractable vomiting, urine-emaciation and others). At the same time, the increased formation of protein may be observed, for example, the formation of y-globulin in infectious diseases. Dysproteinemia is the change in the proportion of particular fractions. Normally, albuminoglobulin coefficient is: A/G=1,5-2,3. It may change when there is the dysfunction of liver, kidneys, in case of infectious diseases. Paraproteinemia – abnormal protein (different interferons, the protein of Bens-Jones, Valdenstrem, kryoglobulin and others). 62 LESSON 17 Theme: Biochemistry of blood. Aim of the lesson: To work out the skill of using the knowledge of mineral composition of blood, haemoglobin exchange in the practical work of a physician. Questions for self-preparation: 1. Nonprotein nitrogen-containing components of blood. Clinical importance of detecting urea, creatinine in blood serum. 2. Exchange of hemoglobin. Biosynthesis of hem, hemoglobin. 3. Decomposition of hemoglobin. What is “direct” (conjugated) and “indirect” (unconjugated) bilirubin? 4. Clinical importance of bilirubin detecting in diagnostics of Hemolytic jaundice (jaundice of newborn). 5. Clinical importance of bilirubin detecting in diagnostics of Hepatocellular jaundice. 6. Clinical importance of bilirubin detecting in diagnostics of Obstructive jaundice. 7. Mechanism of blood coagulation. Anticoagulative system and the system of fibrinolysis Annotation of the theme. Blood contains nitrogen-containing combinations: urea (50%), amino acids (25%), uric acid, creatine, creatinine, bilirubin, indicant, choline, nucleotides, polypeptides and so on. Nitrogen, contained in these combinations, is called rest nitrogen and in norm it must be 14,2-28,4 mmole/l. When a person has some diseases this quality may increase (azotemia). Azotemia Retentional renal Productional cardiovascular (disintegration of the tissue, burns, cachexia, malignant tumours) Presently, instead of counting the quantity of rest nitrogen of blood, the quantity of urea is counted (the norm is 3,3-8,3 mmole/l) and the quantity of creatinine (the norm is 0,044-0,11 63 mmole/l); this procedure gives the opportunity to solve the problems of diagnosing and prognosing the disease. The exchange of hemoglobin is its biosynthesis and disintegration. These processes take place in the cells of reticulo-endothelial system (RES). The synthesis of hem takes place with the help of succinyl-KoA and amino acids of glycine. Scheme of biosynthesis of hemoglobin aminolevulinsynthetase succinyl-СoA + glycine porphobilinogen protoporphyrin aminolevulin acid hem+globin hemoglobin The synthesis of hemoglobin is regulated according to the feedback mechanism. The accumulation of hemoglobin according to this mechanism decelerates its synthesis by means of inhibition of aminolevulinsynthetase (allosteric enzyme). Hemoglobin released from red (blood) cells (they are destroyed in 120 days) is connected with haptoglobin in blood – α2-globulin of the plasma, then it is transported into the cells of reticulo-endothelial system (RES), essentially, into the cells of spleen. Here, hemoglobin is oxidized into methemoglobin and after that it is disintegrated. Haptoglobin (during this process) is split and is transfered into blood. The initial stage of hemoglobin disintegration is oxidizing decomposition under the influence of hemoxigenase of hem’s α-methine bridge, which connects two neighboring pyrrole rings. Ring structure of the hem is broken and verdoglobin is formed. Iron is split from verdoglobin and then it connects with protein-transferine and is transferred with blood to (bone) marrow and globin. Globin is hydrolyzed by spleen cathepsin into amino acids. The broken tetrapyrrole chain of verdoglobin is called biliverdin – bile pigment of green color. It is reproduced with the help of biliverdin-reductase into bilirubin – bile pigment of red-yellow color. The reproduced bilirubin is toxic, unconjugated (not bound with glucuronic acid), indirect. It can be hardly soluted in water and blood and that’s why it is transported into liver together with albumin. One molecule of albumin can freely attach 10-35 molecules of bilirubin. Due to the strong bond with protein, bilirubin is not excreted with urine. 64 Bilirubin transfers into hepatocytes according to the mechanism of reduced diffusion. Conjugated bilirubin is formed in liver under the influence of UDP-glucuroniltransferase. Glucuronidation of bilirubin undergoes two stages, the mixture of monoglucuronids (20%) and diglucuronids (80%) is formed. Bilirubin-glucuronids are not toxic and they are soluble. Bilirubin-glucuronids may diffuse into blood capillaries only in small portions. That’s why two forms of bilirubin may be found in blood plasma: unconjugated – 75% and conjugated – 25%. They form total bilirubin. The concentration of the total bilirubin in blood of a healthy man is 3,9-19 mmole/l. In slim intestine, bilirubin (under the influence of bacteria) is transformed into mesobilinogen (or urobilinogen). The small portion of mesobilinogen (urobilinogen) is absorbed in bowels and after that is transported into liver (by portal vein), where it is fully disintegrated into mono- and dipyrroles. The major portion of mesobilinogen transfers from the slim intestine into thick intestine. There, under the influence of anaerobic bacteria, it is reproduced into colorless stercobilinogen (neither has urobilinogen). The bulk of stercobilinogen is excreted with feces. It is oxidized in the air into stercobilin – orange-yellow pigment, essentially specifying the color of feces. Up to 250 g of stercobilin are excreted with feces daily. Only the small portion of stercobilinogen is absorbed in rectum and through the system of hemorrhoidal veins transfers into postcava and is excreted with urine through kidneys. Stercobilinogen of urine is oxidized into stercobilin, partially specifying the normal straw-yellow color of urine. Daily, 1-4 mg of stercobilin are excreted with urine. Under the influence of different factors in the organism, the process of the formation and absorption of bilirubin and the products of its metabolism may be violated. The increase of bilirubin content in blood leads to the accumulation of bilirubin in tissues, including the mucous tunic and skin. This process causes yellow coloring of these tissues and after that - jaundice. Counting of bile pigments content in blood, urine and feces gives the opportunity to know the level where the violation of its exchange took place. 65 Scheme of disintegration of hemoglobin Red (blood) cells 120 days Hg + haptoglobin (α2- globulin) cells of RES Hg is oxidized into methemoglobin In blood - haptoglobin Hg hemooxigenase Verdoglobin In liver transferine Fe+3 cathepsins globin amino acids Biliverdin – bile pigment of green color NADPH+H+ biliverdinreductase NADP Bilirubine – bile pigment of red-yellow color (indirect,unconjugated, toxic) + Albumin In blood In liver Bilirubine + UDP-glucuronic acid UDP-glucuroniltransferase Mono-,diglucuronide bilirubin (direct, conjugated, not toxic) glucuronic acid In slim intestine In thick intestine Mesobilinogen (urobilinogen) In liver disintegrated into mono- and dipyrroles Stercobilinogen – bile colorless pigment In rectum the system of hemorrohoidal veins in postcava stercobilin- orange-yellow pigment (it excreted with dejection daily – 250mg) kidneys with urine stercobilin (1- 4 mg in a day) 66 There are several types of jaundice. 1. Hemolytic jaundice. It occurs as a result of intensive hemolysis of red (blood) cells. The reason is sickle cell anemia, Addison-Birmer’s disease, thalassemia, taking of several medications stimulating the hemolysis of blood transfusion of incompatible blood groups and others. As a result, the large quantity of unconjugated hemoglobin, toxic bilirubin is formed. And it can’t be conjugated in liver so quickly. Unconjugated bilirubin is not filtered into the cavity of Bowman’s capsule and it doesn’t occur in urine. While the function of liver is preserved, the increase of unconjugated bilirubin content takes place and the growth of conjugated bilirubin concentration may be seen (it is excreted with bile and undergoes all the stages of transformation). Hemolytic jaundice is characterized by: - hyperbilirubinemia (by means of unconjugated bilirubin); - the increase of stercobilin content in feces and urine. Feces has almost dark color and urine has orange-yellow color; - the absence of bilirubin in urine. 2. Jaundice of the newborn. Jaundice of the newborn is considered to be physiological. It occurs as a result of deficiency of bilirubin conjugation enzyme - UDPglucuroniltransferase. This leads to the increase of the level of unconjugated bilirubin in blood. Physiological jaundice of the newborn usually stops in 3-5 days. Immature infants suffer from this disease more. Long-term increase of unconjugated bilirubin in blood may be dangerous because of the toxic effect of bilirubin on developing brain (bilirubin encephalopathy). Grown-up person’s cells have low-permeability for bilirubin and, as a rule, there are no complications after hyperbilirubinemia. 3. Hepatocellular jaundice. It occurs when there are lesions of liver parenchyma (viral hepatitis type A, toxic hepatitis, liver cirrhosis and others). Lesions of liver cells decrease the capture of unconjugated bilirubin from blood and the intensity of conjugated bilirubin formation in these cells. That’s why, inspite of the normal hemolysis, the content of unconjugated and conjugated bilirubin increases (but it is not as intensive as in hemolytic jaundice). The content of stercobilin in urine and feces decreases. Urobilin and small portions of conjugated bilirubin (as it is soluble in water) appear in urine. Normally, they are absent. 67 4. Obstructive jaundice. It occurs as a result of violation of bile outflow into bowels. Extra-hepatic reasons are – obstruction or compression of bile duct by the stone or the swelling of head of pancreas. Intra-hepatic reasons are – several forms of viral hepatitis, jaundice caused by some medications. Obstructive jaundice progresses with large quantity of conjugated bilirubin in blood. This is the result of the reverse inflow of bilirubin from liver cells into blood. Due to the fact that conjugated bilirubin is soluble, it is excreted in large quantities with urine. That’s why urine has the color of beer. The content of stercobilin in feces and urine decreases. Feces is grey-white, clay-colored. The basis of the modern conception of blood coagulation is Schmidt and Moravits’s theory. The mechanism has two stages. The first stage: The active form – thrombin – is formed from prothrombin (the 2nd factor) under the influence of thromboplastin (III), thrombocytes and calcium ions (IV). On this stage, the factors of coagulation of outer mechanism take part: proconvertin (VII), proaccelerin (V), Stuart’s factor (X); also, the factors of inner mechanism of coagulation: Kristmas’ factor (IX), Rosental’s factor (XI), Hageman’s factor (XII). The second stage: Thrombin activates fibrinogen (I), transforming it into the active form fibrin-monomer. After that fibrin-polymer is formed (fibrin gel). It is not very strong. After that gelfibrin is stabilized. Under the influence of the enzyme transglutaminase, strong covalent bonds among molecules of fibrin are formed; also strong covalent bonds between fibrin and fibrinonectin (glycoprotein) are formed. In an hour, the thrombus is retracted (the retraction of the thrombus). Then the process of fibrinolysis takes place. Under the influence of the enzyme urokinase, plasminogen is activated and transforms into plasmin, which splits peptide bonds in fibrin. The thrombus resolves during several days. 68 Scheme of blood coagulation and fibrinolysis IX – Kristmas’s factor XI – Rosental’s factor XII – Hageman’s factor X – Stuart’s factor VII – proconvertin V – proaccelerin trombocytes of tromboplastin – III prothrombin – II Ca2+ - IV thrombin fibrinogen – I fibrin (monomer) plasminogen urokinase plasmin fibrin (polymer) splits peptide bonds in fibrin Apart from coagulative system, there exists anticoagulative system, which has the set of plasma proteins. They inhibit proteolytic enzymes (heparin, anti-thrombin II and others). 69 LESSON 18 Theme: Biochemistry of blood (test). Test-lesson on the topic: Exchange and functions of proteins. Aim of the lesson: To work out the skill of using the knowledge of chemical composition of blood and its changes in pathological states in practical medicine. Questions for self-control: 1. What is blood and what are its functions? 2. Proteins of blood plasma and their role in the organism. Albuminous coefficient. 3. Hypo-, hyper-, disproteinemia, paraproteinemia, the reasons for these diseases. 4. Nonprotein nitrogen-containing components of blood. Clinical importance of detecting urea, creatinine in blood serum. 5. Biosynthesis of hemoglobin. 6. Decomposition of haemoglobin. Conjugated and unconjugated bilirubin. 7. Reasons and laboratory diagnostics of Hemolytic jaundice (jaundice of newborn). 8. Reasons and laboratory diagnostics of Hepatocellular jaundice. 9. Reasons and laboratory diagnostics of Obstructive jaundice. 10. Hemostasis. Mechanism of blood coagulation. The role of fibronectin, transglutaminase in blood coagulation. 11. Anticoagulative system and the system of fibrinolysis. 70