Bacteria (for Micro Exam)
advertisement

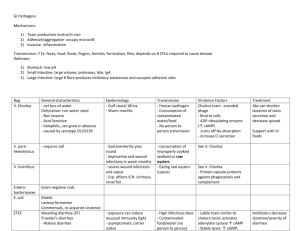
SALMONELLA Structure/ID: Gram (-) rods, encapsulated Motile (like a salmon) with flagella (-) Lactose fermentation (colorless on MacConkey) (+) H2S Ags: O (cell wall), Vi (capsule around O (= K Ag)), H (flagella) – variable to avoid Abs Virulence factors: Vi (virulence) Ag in capsule – inhibits opsonization LPS (endotoxin released on lysis) Type III secretion organelle Can survive in MΦ’s (resistant to lysosomal enzymes) S. enteritidis – cholera-like toxin Pathogenesis: Fecal-oral transmission from animals (via chicken, raw eggs, etc.) S. typhi: 1. Invades cells of distal ileum & colon by inducing ruffling/phagocytosis (type III secretion) 2. Crosses brush border → lymphatics/lymph nodes → blood (1º bacteremia) → liver, spleen 3. Survive & multiply within MΦ’s of liver & spleen (facultative intracellular parasite) → 2º bacteremia/septicemia → enteric/typhoid fever, inflammation of Peyer’s patches (GI sx) 4. In some hosts (i.e. Typhoid Mary), hide out in gall bladder – asymptomatic but infectious S. enteriditis: 1. Invades mucosal cells of small intestine 2. Cholera-like toxin → watery diarrhea 3. Ileal inflammation → mucous/bloody diarrhea S. choleraesuis: bacteremia → brain, lungs, & bone (asplenic pts prone to osteomyelitis) Clinical: Enteric (typhoid) fever (S. typhi): Sx (slow onset): fever, headache, abdominal pain, rash (rose spots) on abdomen Complications: splenic rupture, intestinal hemorrhage Dx: stool culture Rx (intracellular!): chloramphenicol (50S rRNA inhibitor), ceftriaxone (3rd gen. cephalosporins), new floroquinolones, i.e. cipro (DNA gyrase inhibitor) Gastroenteritis (S. enteriditis): 2-day incubation N/V/D (diarrhea may be watery or with mucous & blood) Dx: stool culture Rx: self-limiting (≤1 week); fluid & electrolyte replacement Hosts prone: asplenic (i.e. SCA pts.), ↓gastric acid production (Salmonella is acid-sensitive) SHIGELLA Structure/ID: Gram (-) rods, aerobic Non-motile (Shigella has no flagella) (-) Lactose fermentation (colorless on MacConkey) (-) H2S O Ag different between species: S. dysenteriae (A), S. flexneri (B), S. boydii (C), S. sonnei (D) S. dysentariae most often causes dysentery, but S. sonnei most common in industrialized world 1 Virulence factors: Type III secretion organelle ICS-A protein → actin tail formation → movement from cell to cell (Listeria do this too!) σ factor of RNA polymerase: adapts to acidic environment Shiga toxin (like EHEC toxin) – AB toxin inhibits 60S rRNA → ↓protein synthesis → cell death Pathogenesis: 1. Fecal-oral transmission (water, hand-to-hand) 2. Passes through stomach (thanks to σ factor), multiplies in small intestine 3. Invades intestinal epithelial cells by inducing ruffling/phagocytosis (type III secretion) 4. Multiplies in cytoplasm 5. Uses host proteins to form actin tails → form protrusions at membrane → engulfed by adjacent cell 6. Lysis of membrane → inflammatory cytokine response (so (+) fever) 7. Inflamed colon unable to reabsorb ions/fluid → diarrhea 8. Cell death from Shiga toxin & immune response → capillary thrombosis → bloody diarrhea Clinical: Sx: fever, dysentery (bloody diarrhea with WBCs/pus), cramping abdominal pain Dx: stool culture Rx (intracellular!): 3rd generation cephalosporins (β-lactamase resistant), TMP/SMX (THF inhibitors), floroquinolones (DNA gyrase inhibitors) VIBRIO CHOLERA Structure/ID: Gram (-) rod, aerobic/facultative Motile (single polar flagellum) (-) Lactose fermentation (colorless on MacConkey) (+) Oxidase Virulence factors: Choleragen (cholera toxin) – AB toxin → ↑Gs → ↑AC → ↑cAMP → ↓ Na+/Cl- reabsorption, ↑Cl- & HCO3- secretion (does not cause cell damage or invade) – similar to ETEC’s LT toxin Adhesins on pili/fimbriae (toxin coregulated pilus (TcpA)) Pathogenesis: 1. Fecal-oral transmission (water, food, seafood) 2. Release cholera toxin → ↑TcpA adhesions → binds to brush border of small intestine → multiplication 3. Cholera toxin → ↑cAMP → ↓ Na+/Cl- reabsorption, ↑Cl- & HCO3- secretion → watery diarrhea Clinical: Sx: high-output watery (“rice water”) diarrhea → severe dehydration may → death; NO fever Dx: stool culture, serology Rx: oral rehydration solution, doxycycline (inhibits 30S rRNA) may shorten duration ESCHRECHIA COLI Structure/ID: Gram (-) rod, aerobic Motile (flagella) (+) Lactose fermentation (85-95%) – pink on MacConkey, metallic green on EMB agar Ags: O (cell wall) – highly variable, K (capsule around O (= Vi Ag)), H (flagella) > 4 pathogenic strains (different virulence factors): ETEC, EHEC (O157:H7), EIEC, EPEC 2 Virulence factors: LPS (endotoxin released on lysis) Adhesins on pili ETEC: LT (like cholera toxin)/ST – AB toxins → ↑Gs → ↑AC(LT)/GC(ST) → ↑cAMP/cGMP → ↓Na+/Cl- reabsorption, ↑Cl- & HCO3- secretion (does not cause cell damage or invade) EHEC: Shiga-like toxins (Stx1/Stx2) – AB toxins inhibit 60S rRNA → ↓protein synthesis → cell death EIEC: type III secretion organelle, maybe a little Stx EPEC: intimin & other proteins → non-intimate attachment & effacement Pathogenesis: Fecal-oral transmission Nonpathogenic E. coli (normal flora) + virulence factors = pathogenic E. coli ETEC: 1. Pili adhesins bind intestinal epithelial cells 2. Releases LT/ST → ↑AC(LT)/GC(ST) → ↑cAMP/cGMP → ↓Na +/Cl- reabsorption, ↑Cl- & HCO3secretion → watery diarrhea (like cholera) EHEC (O157:H7): 1. Pili adhesins bind intestinal epithelial cells 2. Release Stx1/Stx2 → inhibit 60S rRNA → ↓ protein synthesis → cell death → capillary thrombosis → hemorrhagic colitis, renal endothelial damage (hemolytic-uremic syndrome) EIEC: 1. Invades intestinal epithelial cells by inducing ruffling/phagocytosis (type III secretion) 2. Stimulates inflammatory response → bloody diarrhea with WBCs (like Shigella) 3. May secrete a little Stx → cell death EPEC: Complex mechanism (alters cytoskeletal proteins) to form localized attaching & effacing lesions in small intestine → watery diarrhea (mostly in infants) Clinical: ETEC: 1-2 day incubation; 3 day – several week duration Traveler’s diarrhea – “rice water”, no fever (no invasion) Dx: stool culture Rx: oral rehydration EHEC: 3-4 day incubation; 1 week duration Hemorrhagic colitis – bloody diarrhea, abdominal cramping, NO fever Hemolytic-uremic syndrome (8-11%, usually children) – hemolytic anemia, thrombocytopenia, thrombosis of glomerular capillaries → renal endothelial damage → acute renal failure may → death Dx: stool culture Rx: fluids, dialysis if needed, supportive (antibiotics may ↑LPS release → ↑HUS) EIEC: <24 hour incubation Sx: blood and pus in stool, fever (like Shigella) Dx: stool culture Rx: ?? EPEC: 1-3 day duration Sx: watery diarrhea Rx: oral rehydration UTI (#1 cause) Sx: dysuria, frequency, fullness/urge Compications: cystitis, pyelonephritis 3 Rx: TMP/SMX (inhibit THF) Meningitis in neonates (2nd to group B strep) Rx: ampicillin (cell wall) + cefotaxime (3rd generation cephalosporin – β-lactamase resistant) Nosocomial infections: Pneumonia Septic shock (from LPS endotoxin) – Rx: aminoglycoside (30S rRNA) + 3rd gen. cephalosporin ANTHRAX (BACILLUS ANTHRACIS): Structure/ID: Gram (+) rod, encapsulated (only bacterium with amino acid capsule), forms chains Spore-forming, aerobic Virulence factors: Glutamic acid capsule (encoded on plasmid PXO2) – prevents phagocytosis of vegetative form Spore – resistant to drying, heat, UV light, disinfectants; can survive many years in soil Anthrax toxin (3 proteins encoded on plasmid PXO1): Edema factor (EF) – like AC → ↑cAMP → ↓ PMN function, ↑edema Protective antigen (PA) - ↑ entry of EF & LF into phagocytic cells (like B subunit) Lethal factor (LF) - ↑MΦ → TNF-α, IL-1, IL-6 → inflammatory response → death Pathogenesis: Cutaneous: 1. Skin contact with spore in soil (or terrorist letter) 2. Spores germinate on skin abrasions; activated at 37ºC to express PXO1 & PXO2 virulence factors 3. Rapidly multiplies and releases exotoxin → necrotic ulcer 4. May spread to bloodstream (bacteremia) GI (rare but deadly): 1. Ingestion (from contaminated meat) 2. Multiplies and releases exotoxin in mouth/esophagus or terminal ileum/cecum → necrotic ulcer Inhalational: 1. Inhaled from animal hides (or terrorist letter) 2. Spores taken up by MΦ’s in lungs → hilar & mediastinal lymph nodes (germinate there) 3. Release exotoxin → hemorrhage, pleural effusion Clinical: Cutaneous (malignant pustule): Painless necrotic (black) ulcer with edema 3-10 days s/p exposure 20% progress to bacteremia Dx: lab ID Rx: cipro (inhibit DNA gyrase) or doxycycline (inhibit 30S rRNA) GI: Sx: abdominal pain, vomiting, bloody diarrhea Rx: penicillin, doxycycline, cipro/levofloxacin Inhalational (Woolsorters disease): Fever, chills, sweats, fatigue, chest pain, cough (no purulent sputum) 1-7 days s/p exposure Progresses to: hemorrhagic meningitis, mediastinal hemorrhage (see widening on CXR), pleural effusions, respiratory failure, shock Dx: clinical findings, lab ID Rx: 60 days cipro or doxycycline IV; clindamycin (inhibits 50S rRNA) to ↓ toxin production if widened mediastinum or bacteremia/shock; add drugs for meningitis (rifampin, vancomycin, etc.); note: lots of bugs → β-lactamase production → penicillin resistance Anthrax Vaccine Adsorbed (AVA): PA protein from toxin – immunogenic 4 TUBERCULOSIS (MYCOBACTERIUM TUBERCULOSIS): Structure/ID: Acid-fast rods – show up red on blue background, due to lipids (mycolic acids) in cell wall Obligate anaerobe Grows slowly on culture media, (+) niacin test Cell wall lipids: mycolic acid, mycosides (FA + carbohydrate), cord factor, sulfatides, wax D Virulence factors: Cell wall lipids – survival inside MΦ’s (facultative intracellular), granuloma formation Cord factor → ↑TNF-α → cachexia Sulfatides – inhibit phagosome/lysosome fusion → survival in MΦ’s Wax D – adjuvant σ-factors – induce expression of genes involved in survival within granulomas Drug resistance plasmids! Pathogenesis: 1º infection: 1. Aerosol; inhaled (transmission by respiratory droplet) 2. Droplet → middle & lower lobes of lung (highest air flow) 3. Pneumonitis with PMNs & edema → alveolar MΦ response → phagocytosis 4. Bugs multiply in MΦ’s → bloodstream → lymph nodes → organs (especially liver & spleen) 5. Immune response: (+) CMI → DTH response → small caseous granuloma formation → asymptomatic (-) CMI (kids, elderly, immunocompromised) → large granulomas → progressive disease or miliary TB (disseminated disease) Latency: bugs hanging out within caseous granulomas; reactivated when ↓CMI 2º infection (5-10% lifetime risk for normal hosts; 8-10% annual risk for HIV (+) hosts): form granulomas in lungs (upper lobe – ↑O2 tension) & other organs Clinical: Dx of old 1º infection: PPD (TB → DTH response) – note: HIV+ pts may not have DTH, so test Candida or mumps too CXR: see calcified tubercle (Ghon focus) in lower lung, calcified granulmoa (Ghon/Ranke complex) in hilar lymph node, or scarring in upper lobe Dx of active infection: CXR: see cavitary lesions with air fluid levels in lung (+) Sputum culture, acid-fast stain Clinical picture of active infection: Pulmonary TB – apical areas (↑O2 tension); sx: productive cough/hemoptysis, chronic low-grade fever, night sweats, weight loss/cachexia → death in 50% if untreated Pleural/pericardial infection Lymph node TB = scrofula Kidney (“sterile pyuria”) – see RBCs/WBCs in urine, but no bacteria (slow growing) Skeletal/joints – destruction of T- and L-spine intervertebral discs (Pott’s disease); arthritis CNS – subacute meningitis, granulomas in brain Miliary TB – disseminated (may see millet-seed pattern in lung on CXR) Immunocompromised hosts more likely to develop extrapulmonary TB Rx: isoniazid (INH), rifampin, pyrazinamide in combo – all are hepatotoxic and may → hepatitis MDR TB is a huge problem, especially in HIV+ pts 5 PNEUMOCOCCUS (STREP PNEUMONIAE): Structure/ID: Gram (+) diplococcus (lancet-shaped), encapsulated α-hemolytic, (+) optochin-sensitivity (+) Quelling reaction (antiserum causes capsule to swell) Normal flora of nasopharynx; causes problems in cavities/tubes (but does not invade cells) 84 capsular serotypes (reinfection possible) Virulence factors: Polysaccharide capsule – inhibits phagocytosis & complement IgA protease – inhibits mucosal immunity C-substance – targeted by C-reactive protein → acute phase response Pathogenesis (pulmonary disease): 1. Transmitted via respiratory droplets (inhaled) 2. Proliferate in alveoli 3. Activate compliment & cytokines 4. Alveoli fill with bugs & inflammatory cells Clinical: Pneumonia (#1 cause in adults) Sx: sudden onset of high fevers, shaking chills (rigors), chest pain on respiration, dyspnea, cough productive of yellow-green sputum Dx: may see lobar infiltrate (middle R, lower L) on CXR, clinical picture, sputum culture Rx: some resistance to penicillin, erythromycin, chloramphenicol, TMP/SMX; try high-dose penicillin or cephalosporins (β-lactamase resistant); vancomycin if highly resistant Meningitis (#1 cause in adults) Otitis media/sinusitis (#1 cause in kids) Vaccine (pneumovax) – 25 most common capsular Ags for immunocompromised pts; new 7-Ag vaccine for kids (100% effective in preventing invasive infections) GONOCOCCUS (NEISSERIA GONORRHEAE): Structure/ID: Gram (-) diplococci (kidney bean shaped), encapsulated Aerobic, oxidase (+), ferments glucose Grow best on Thayer-Martin VCN medium (chocolate agar with abx) & in CO2-enriched environment Virulence factors: Polysaccharide capsule Pili & outer membrane proteins – attach to reproductive epithelium, prevent phagocytosis by staying close to host cells Antigenic variation of pili & OMPs to evade Abs LPS endotoxin IgA protease Pathogenesis: 1. Transmitted by sexual contact or during childbirth 2. Infects columnar epithelium of cervix (♀) or mucous membranes of urethra (♂) 3. Phagocytized by professional APC in submucosa, presented to CD 4+ T-cells 4. Inflammatory response initiated → symptoms 6 Clinical: Gonorrhea in ♂: Urethritis → painful urination, purulent urethral discharge Complications: epdidymitis, prostatitis Gonorrhea in ♀: Urethritis → painful/burning urination, purulent urethral discharge – or asymptomatic Cervicitis → lower abdominal discomfort, dyspareunia, purulent vaginal discharge Complications: PID – endometritis, salpingitis and/or oophoritis – (sx: fever, lower abdominal pain, bleeding, CMT) → sterility, ectopic pregnancy, abscesses, peritonitis, peri-hepatitis (FitzHugh-Curtis syndrome) Dx: culture of infected area – see Gram (-) diplococci within WBCs Rx: cipro or ceftriaxone (resistance to others); treat for chlamydia too (doxycycline/azithromycin) Complications of both: Bacteremia (sx: fever, joint pains, skin lesions on extremities) → peri/endocarditis, meningitis Septic arthritis (1 or 2 joints at first → progressive); dx: culture of synovial fluid Infants: ophthalmia neonatorum → damages cornea → blindness; give erythromycin eyedrops ENTEROCOCCUS Structure/ID: Gram (+) cocci (+) growth in 6.5% NaCl, (+) growth in 40% bile (bile esculin hydrolysis) Virulence factors: Part of normal intestinal flora – only when they get out do they cause a problem Most infections are nosocomial Clinical: UTIs Biliary tract infections Subacute bacterial endocarditis (SBE) Wound infections Bacteremia Rx: Ampicillin + aminoglycoside – but now many resistant; use vancomycin – but VRE now (cell wall dAla-dAla → dAla-lactate – eliminates vancomycin target); try older abx or new pristinomycins STREP PYOGENES Structure/ID: Gram (+) streptococci, encapsulated Group A Lancefield Ag, β-hemolytic (-) Catalase, (+) bacitricin susceptibility Normal flora of skin and mucous membranes (especially oropharynx) Virulence factors: Streptolysin O – hemolysin (→ β-hemolysis); anti-streptolysin O Abs measured by ASO titer M protein (80 types) – inhibits phagocytosis and complement activation (but B-cells make Ab to it) Hyaluronic capsule – inhibits attachment of phagocytes Erythrogenic/pyrogenic exotoxins (especially A) → scarlet fever, TSS Streptokinase – catalyzes plasminogin → plasmin → degrades fibrin → tissue degredation Protein F and lipoteichoic acid (LTA) – binds fibronectin on respiratory epithelial cells 7 Pathogenesis: 1. Transmitted by respiratory droplets or contact with skin/fomites (sometimes in food) 2. Binds fibronectin on epithelial cells via protein F & LTA 3. Spread/multiplication: Impetigo – localized in skin Pharyngeal infection – localized, may → bacteremia Necrotizing fasciitis – moves rapidly through fascia (thanks to streptokinase & M proteins) 4. Exotoxin release: Erythrogenic/pyrogenic exotoxins (superAgs) → ↑ TNF-α, IL-1 → scarlet fever, TSS 5. Complications (acute rheumatic fever, acute glomerulonephritis) may be due to autoimmune crossreactivity and/or immune complexes Clinical: Pharyngitis: Sx: beefy red tonsils with exudates, fever, NO cough, lymphadenopathy Dx: throat culture (note: rapid strep test has poor sensitivity – false (-)’s) Rx: penicillin (within 10 days to prevent rheumatic fever) Scarlet fever: Sx: fever, rash on trunk/neck → extremities (NOT on face); skin may scale during healing Rx: penicillin Skin infections: Impetigo (vesicular blister → crusty; often around mouth), cellulites, folliculitis Rx: could be caused by staph, so use dicloxacillin (penicillinase-resistant) Necrotizing fasciitis: Sx: inflammation moving away from initial site; then skin color changes from red → purple → blue; large blisters (bullae) form; later – skin necrosis, myositis Rx: rapid penicillin G (IV) + clindamycin (↓ toxin production) TSS: Sx: fever, diffuse erythematous rash, N/V/D, septic shock Rx: penicillin G (IV) + clindamycin (↓ toxin production) Acute rheumatic fever (ARF): Complication of untreated strep pharyngitis (but not skin infection) Sx: fever, myocarditis, joint swelling, chorea, subcutaneous nodules, erythema marginatum (red margin) rash Valvular disease develops later Rx: prophylactic penicillin; if (+) valvular disease – amoxicillin for dental work Acute glomerulonephritis (AGN): Complication of strep pharyngitis or skin infection (penicillin may not prevent it) Caused by only a few nephritogenic M-types Sx: smokey or tea-colored urine (hematuria), puffy face, ↑BP STAPH AUREUS Structure/ID: Gram (+) cocci in clusters β-hemolytic, (+) catalase, (+) coagulase Non-spore forming, but fairly resistant to heat & drying Normal flora on skin & in nares Virulence factors: Factors that screw up our defenses: Protein A – binds IgG Fc → ↓ complement activation Coagulase – prevents phagocytosis 8 Hemolysis & leokocidins – destroy RBCs & WBCs Penicillinase & novel PBP – penicillin resistance Factors that tunnel through tissues: Hyaluronidase – hydrolizes CT (works with exfoliative toxin) Staphylokinase – lysis fibrin → tissue degredation Lipase & protease – do just what it sounds like Toxins: α-toxin – cellular destruction/abscess formation Exfoliative toxin – splits epidermis at stratum granulosum (works with hyaluronidase) TSS toxin → ↑IL-1, IL-2 Enterotoxins – resistant to heat & gastric acid Pathogenesis: Transmission: contact with skin or fomites, ingestion of exotoxin Usually remains localized → inflammatory response at site May release exotoxin → gastroenteritis, TSS, scalded skin syndrome May → blood (bacteremia) → sepsis May invade other organs (lungs, meninges, bones, etc.) Clinical: Skin infections (contained): Impetigo, cellulitis, local abscesses, furuncles (subcutaneous), carbuncles (when furuncles join) Wound infections (especially post-surgical) → abscess/cellulitis; must reopen Rx: dicloxacillin (penicillinase-resistant) – covers Strep too Exotoxin release diseases: Gastroenteritis – ingested enterotoxin→ ↑peristalsis → N/V/D, abdominal pain, fever? (12-24 hrs) TSS – fever, diffuse erythematous rash, N/V/D, septic shock; must clean infected area Scalded skin syndrome – exfoliative toxin → cleavage of middle epidermis, skin peeling – usually in kids (especially neonates s/p severed umbilicus) Rx: abx may help with TSS, but mostly supportive therapy Bacteremia: often from catheter (IV) → sepsis, endocarditis Organ invasion diseases: Lobar pneumonia – nosocomial, usually follows viral flu → cavitations, effusions, empyema (pus) Meningitis/cerebritis/brain abscess – fever, CNS sx Osteomyelitis – usually in boys <12 y/o; inflammation over bone, fever Acute endocarditis – high fever, chills, myalgias; cause valvular destruction & embolism of vegetations → brain (L side valve) or lung (R side valve – often IV drug users) Septic arthritis (#1 cause) – inflamed joint, septic synovial fluid with ↑PMNs Rx: methicillin, nafcillin (penicillinase-resistant) MRSA: Resistance via plasmid (most encode altered PBPs) Nosocomial – transferred from pt to pt by us Use vancomycin for critical infections only (due to emergence of VRE) 9