Heads meeting agenda and papers_May 17 2012
advertisement
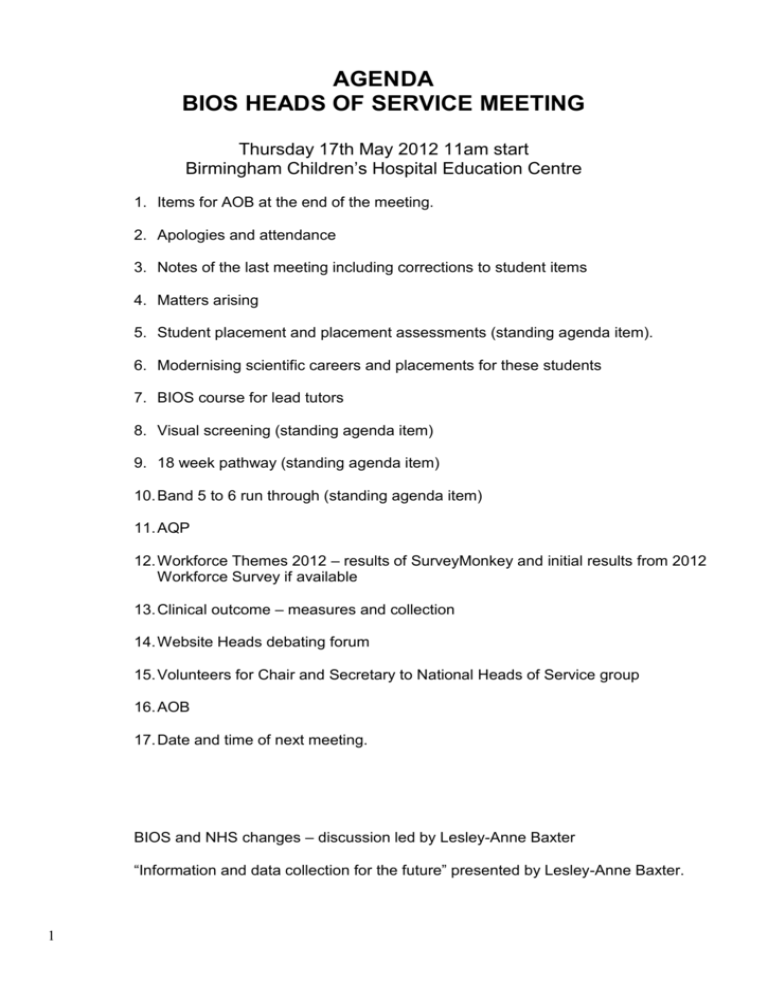
AGENDA BIOS HEADS OF SERVICE MEETING Thursday 17th May 2012 11am start Birmingham Children’s Hospital Education Centre 1. Items for AOB at the end of the meeting. 2. Apologies and attendance 3. Notes of the last meeting including corrections to student items 4. Matters arising 5. Student placement and placement assessments (standing agenda item). 6. Modernising scientific careers and placements for these students 7. BIOS course for lead tutors 8. Visual screening (standing agenda item) 9. 18 week pathway (standing agenda item) 10. Band 5 to 6 run through (standing agenda item) 11. AQP 12. Workforce Themes 2012 – results of SurveyMonkey and initial results from 2012 Workforce Survey if available 13. Clinical outcome – measures and collection 14. Website Heads debating forum 15. Volunteers for Chair and Secretary to National Heads of Service group 16. AOB 17. Date and time of next meeting. BIOS and NHS changes – discussion led by Lesley-Anne Baxter “Information and data collection for the future” presented by Lesley-Anne Baxter. 1 PAPERS Appendix 1 EXTRACT FROM NOTES FROM NATIONAL HEADS OF SERVICE MEETING Thursday 12th May 2011 at Birmingham Children’s Hospital Response from Marie Cleary, Chair of BIOS Education Committee (shown in blue) 4. Student placement and placement assessments (standing agenda item). The universities are still experiencing difficulties with a lack of placement sites. Even if sites only take one student there will still be a shortage. Small departments find it difficult to take more than one student. Many sites find it difficult during the summer months with staff annual leave. Options to consider: Could small departments work with another nearby department in a hub and spoke model, or share 2 students. If this is planned, the departments should inform the BIOS education committee for approval. I have experience of this model, and am happy to discuss with anyone interested. Could the students have shared tutorial / study time or any other learning experiences together each week, e.g. one session on same site, one with orthoptist, the other with medic, optometrist, etc., then can meet up after to reflect together at end of session. Could they share accommodation even if main placements are separate. This will facilitate time together to share experiences. - The universities feel that having 2 students together provides a better learning experience since they are presumed to share experiences. They will consider sending one student, and anyone who can only offer this arrangement for some placements should contact Gail or Helen directly. Whether band 5s could be involved in Orthoptic undergraduate teaching may be discussed in the future by the Education Committee. Band 5s currently teach health visitors, trainee GPs, school nurses. BIOS Education Committee have reviewed clinical tutor requirements, and currently feel that 2 years post-graduate experience is appropriate as a minimum requirement, as well as attendance at the BIOS clinical tutors course (only a recommendation at the moment). This is in keeping with most other AHP professions. Band 5s cannot contribute to the formative assessment of undergraduate orthoptists, but they are not precluded from involvement with the students, for instance demonstrating cases or techniques to them. This would have to be at the discretion of the Lead / Head Orthoptist, as long as they were deemed competent to do so. Following discussion by the Education committee, Lead tutor training is to be reviewed, initially via a focus group. BIOS requirements do exceed many other AHPs. The decision about this has to be measured and be in consultation with education staff, tutors and students. Further feedback from Helen Davis : Sheffield University feel that band 5 Orthoptists with the correct experience could contribute to assessment of Orthoptic students. 2 Two Community SHAs are looking at making it mandatory for Trusts to take students. This may become a nationwide decision and therefore it would be prudent for all Trusts to ensure they take students where possible or plan for it if not currently taking students. This may involve training of clinical tutors. Some SHAs have courses which are suitable for clinical tutor training. It would be useful to create a list of these courses. There was a recent call from PDC to create a list of all post-graduate training opportunities for Orthoptists. Could all Heads be asked to send information about these training opportunities to PDC to add to the database. Orthoptics set high standards for student training – band 6, two years experience for staff. This may also be reviewed. This has been given due consideration by the Education Committee, but as stated above, this is in line with other AHPs, and if felt to be appropriate. The Lead tutor training, however, is to be reviewed. 3 Appendix 2 Feedback from Helen Davis (Sheffield University) to the notes made after the National Heads of Service Meeting on Thursday 12th May 2011 at Birmingham Children’s Hospital. 4. Student placement and placement assessments (standing agenda item). Note made: The HPC decided students have to go on placement as a minimum of two and it consequently appears as such in the university handbooks. Feedback from Helen Davis: HPC have never been this prescriptive in their Standards of Education & Training. The SET nearest is item 5.6 - ‘ There must be an adequate number of appropriately qualified and experienced staff at the practice placement setting’. Iin the guidance for this SET it states ‘some professional bodies play an active role in providing advice on staffstudent ratios. Please contact the individual professional bodies if you want further guidance in this area. ‘ All mandates and recommendations of this nature will have been made by the BIOS education committee. 31-5-11 4 Appendix 3 NOTES FROM HEADS OF SERVICE MEETING 2011 Thursday 12th May 2011 at Birmingham Children’s Hospital Education Centre 1. Apologies and attendance 55 in attendance 6 apologies received The meeting welcomed Lesley-Anne Baxter, Chairman of BIOS. 2. Notes of the last meeting No amendments requested 3. Matters arising All matters were covered on the agenda for the meeting 4. Student placement and placement assessments (standing agenda item). The universities are still experiencing difficulties with a lack of placement sites. Even if sites only take one student there will still be a shortage. Small departments find it difficult to take more than one student. Many sites find it difficult during the summer months with staff annual leave. The HPC decided students have to go on placement as a minimum of two and it consequently appears as such in the university handbooks. The precedence is the elective placement with only one student. It was noted that one student could live at home and one in hospital accommodation. They would only meet at lunchtimes. This issue will be taken to the Education Committee on Friday. Whether band 5s could be involved in Orthoptic undergraduate teaching may be discussed in the future by the Education Committee. Band 5s currently teach health visitors, trainee GPs, school nurses. Two Community SHAs are looking at making it mandatory for Trusts to take students. This may become a nationwide decision and therefore it would be prudent for all Trusts to ensure they take students where possible or plan for it if not currently taking students. This may involve training of clinical tutors. Some SHAs have courses which are suitable for clinical tutor training. Orthoptics set high standards for student training – band 6, two years experience for staff. This may also be reviewed. 5. Vision screening (standing agenda item) A national chain of optometrists are bidding to provide vision screening. This service would be cheaper but will need Orthoptists to do the training. This would then make the service ‘Orthoptic lead’ as per the guidelines. There was a discussion as to whether departments should be training optometrists. Some want in-depth training to be able to call themselves Orthoptic Specialist Optometrists. Some departments only take pre-reg optometrists for one visit to ensure they are not training them ‘to do our job’. Some optometrists are asking how to obtain HPC registration to enable them to practise Orthoptics. Orthoptists need to raise the issues of clinical governance and culpability if optometrists undertake vision screening. The profile of Orthoptics needs to be raised. An advantage to optometrists screening would be the child having their refraction on the same day. Screening will be cheaper on a GOS budget rather than PCT. Maybe central government need to look at the GOS budget to make savings - a counter argument to optometrists screening rather than Orthoptists. One Trust has initiated a screening service since the last meeting. One PCT has funded an optometry leaflet for school reception class parents encouraging them to take their child for a sight test because there is no local vision screening service. 5 One commissioner is asking for details about screening. Another Trust after giving details of their screening service to their PCT, received notice of the termination of their SLA in December on the grounds of parents being able to take their child to a local optometrist. Details of the critical age, visual development and the need for extra binocular status screening persuaded the PCT to reinstate the service. All screening programmes are going to be run by Public Health once the PCTs are disbanded and under the jurisdiction of the local authority. The local authority may not want to fund screening. BIOS and SALT are taking this issue forward through the AHP Federation. A question was asked as to how people occluded when screening. Of the 55 Heads in attendance, 40 Trusts undertake primary screening. Of these, 10 use tape when testing vision to occlude the child and 28 use occluding glasses. Some Trusts use both if a child peeps. Neither cost nor a child’s fear of a patch was a factor in choice of occlusion. Of the 10, none have signed parental consent to use tape. Testing is possibly quicker using the occluding glasses but Durapore can be quickly torn off the roll. Infection control was one reason for using tape. Infection control is not such an issue in the community as the individual Trust policies should only apply when working on a Trust site but recently a nurse was dismissed in Northants when working offsite at a GP practice. One Trust has decided envelopes and patches should not be stored in the same cupboard to avoid infection control issues. Of the 55 Trusts present, only 8 test visions below the pass criteria. There was a variety of different pass levels. If using different criteria from the national guidelines, Trusts have agreed their new criteria after undertaking audit. About 5 years ago research showed there was little difference between Kays and Keeler - published (? in Eye). One Trust uses Sonksen Silver to screen 3 ½ year olds. Positive failures are assessed in the Hospital Eye Service and then tested with Keeler. Sonksen Silver is found to be easier to use on this age group. 6. 18 week pathway (standing agenda item) Waiting times are no longer a national target as quality and examples of good practice are more important. Some Trusts still have to adhere to 18 weeks as it is part of their negotiated contracted for this year. One Trust has to observe 18 weeks and monitor AHP Referral to Treatment Times. Some Trusts cover capacity issues by working 9 day fortnights or long day flexi hours seeing adults in the evenings. With less staff on duty each day, work has to be absorbed if staff are off sick. One Trust is paying staff double time for waiting list initiatives. Waiting list initiative clinics will create problems with the new to follow up ratio once Trusts are penalised for breaching the agreed ratio. Some Trusts have combined Optometry/Orthoptic clinics to reduce the number of visits. A single tariff can be applied to a combined clinic. Combined clinics are still under the name of a Consultant to avoid Clinical Governance concerns. In some Trusts, all patients have must have refraction and fundoscopy prior to discharge. Coventry works to every child over the age of 4 attending the combined clinic if they have an Orthoptic problem and every child under the age of 4 or if they have other pathology, attending a Consultant clinic. At some Trusts, adults under shared care, attending stroke clinics do not see a Consultant if registered under a Physician. The difference between multi disciplinary and multi professional clinics was discussed. In general, the former involve different professionals in the Trust (eg TEDs see Ophthalmology and Endocrinology). The latter involve different professionals within Ophthalmology (eg Paed clinic patients see Orthoptists, Optometrists and Paediatric Ophthalmologists on the same day). Both will have one tariff although special conditions may have an enhanced tariff. One Trust is using block contracts rather than Payment By Results but it essential to undertake a skill mix review is this happens. 7. Band 5 to 6 run through (standing agenda item) This is happening in some Trusts for posts that were banded as a 6 but the Trust employed a band 5 for short term. Providing the staff have had an appraisal and met the desired competencies, their run through to a band 6 should happen without problems Some Trusts have established band 5 posts. This can be an issue when looking at student training. 6 Coventry runs a successful 2 year Preceptorship Programme. The Orthoptist has to apply for the second year post when they reach the end of the first year. The second year has objectives which are reviewed six months into the year. The Orthoptist has to leave at the end of the second year but can apply for a Coventry post if available within the establishment. Coventry has a large number of applicants for the Preceptorship programme. 8. Workforce Issues Lesley-Anne thanked everyone for completing their surveys. The information is essential in helping establish the size of undergraduate placements. Thank you also to everyone who completed the survey-monkey. Issues from this include workforce, TU activities, GP commissioning and undergraduate placements. This survey will be sent out again as not everyone received it. One of the biggest issues from the surveys is communication. Lesley-Anne asked everyone to use the BIOS website which is still undergoing development. Some Heads feel there is no time to read Parallel Vision on line or visit the BIOS website but Lesley-Anne felt these are the best means of communication. The Professional Development Committee are currently producing a database. GP Commissioning will happen but the timescale may change. The changes to the Health and Social Care Bill will be published on the BIOS website. The BIOS office will close on Saturday 14th May and will go “Virtual” from Monday 16TH May. The SLA with CSP still stands and there will still be a desk at CSP offices if needed. 9. Finance Issues BIOS finances are safe for the coming year. There has been a 75% reduction in reserves and any savings or profits will go back into the reserves. Two departments have had staff down-banded whilst still in post. Skill mix reviews are very important to banding issues. It isn’t known yet whether the workforce survey represents the departmental loss in Orthoptic hours and this may need to be addressed next year. There were many examples of banding issues, vacancies and recruitment delays discussed at this point in the meeting. Some Trusts are merging Optometrist and Orthoptic Head posts. It is important to note that optometrists undertake eye tests whereas Orthoptists undertake more than one role with Orthoptics as well as Public Health (screening) and multi disciplinary roles (stroke service). 10. Atropine Occlusion. The supply of atropine was discussed. Some use a PGD and some ask the GP to supply it on a repeat prescription. The PGD must cover supply as well as administering atropine. The PGD is better if the child tends to DNA. If a GP is supplying the atropine patient compliance must be good. If the patient DNAs they can still continue to get hold of the atropine without being monitored if their GP supplies it. Some departments prescribe atropine occlusion as part of parental choice on the method of occlusion. There is less of a risk with Atropine now as it is supplied in minims rather than a whole bottle. One Trust’s Pharmacy feels that the toxic risk could be left off the risk warnings. It was suggested to use the BIOS forum to ask for evidence on the adverse reactions after using atropine. Recent evidence shows that atropine is more cost effective as well as being more clinically effective. One Trust has a protocol which states that under 3 years old atropine is not used whereas if over 3 years old it is a first line choice because of concerns about the risk of reverse amblyopia. The atropinised eye can always be monitored by assessment with a pinhole and if the acuity starts to drop atropine can be stopped. It was agreed that atropine is still more effective as a form of occlusion if the visual acuity is 0.5 or better. 7 11. Medisoft Orthoptic Module and Linking Electronic Clinical Data to Paperless Records. Some Trusts use the Orthoptic Medisoft module. The disadvantage - it only goes to two decimal points (unsuitable for some vision tests). Some areas of the module need improvement and the task has been given to a project manager by Medisoft. It is useful for Orthoptic pre and post ops. Medisoft is used for HRTs, OCTs, IOLs and A-scan biometry. HVF cannot be linked electronically to Medisoft. One Trust has linked HVF via Optical Imaging Systems. All has been networked. HVF machines may be too old to be networked. Open Eyes is the format used by Moorfields. Synergy project manager is looking at Topcom to electronically link records. 12. A.O.B. i. Modernising Scientific Careers. This course or degree has a ‘vision’ element. It has a large curriculum and will include EDTs, audiometry and biometry. It is being piloted by four or five universities and will be available at band 4 technicians, undergraduate or doctorate level. The course will need clinical placements and will cause pressure on the demand for student placements. It will also need formal lecturing. It may be a source of Ophthalmic Technicians. Leicester Royal Infirmary is linked to De Montfort University and will therefore have to take students which could be a large commitment. Some departments already undertake BPs, urine testing, Tonopens and are involved in Epiphora, Lumps and Bumps and uveitis screening clinics. Orthoptists should be looking to expand into some of the medics roles before the Optometrists and Technicians take over all our roles. ii.PCT Reduction in Payment for Surgery. Some PCTs have refused to pay for or request prior application from Trusts to pay for second eye cataract surgery and adult cosmetic lid and squint surgery. There needs to be a change in the classification. Some of the cosmetic surgery should be classified as reconstructive or non-functional to be acceptable for surgery. The DVLA Humphrey Visual field test is worth undertaking when considering surgery for blepharoplasty. Leicester has designed an HVF test to perform when considering ptosis surgery. Details have been published in ‘Eye’. iii. Lunch at Future Meetings. There was a debate as some Heads want a quicker lunch break if they have a long journey home. Some Heads wanted to use the chance to network. There is always the opportunity to network after the meeting. It was agreed in future to decide at the start of each meeting by a vote. 13. Date and time of next meeting. To be advised by Jackie Nolan. 14. Manager’s Forum. 13th October 2011 in Birmingham. Details to follow. It will take the format of working parties with external facilitators. 8