alabama's “fat tax”
advertisement

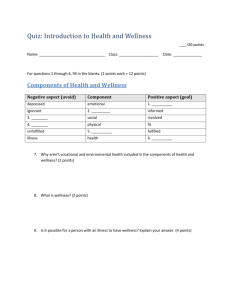
Alabama’s “Fat Tax” 1 ALABAMA’S “FAT TAX” © 2009 Asbjorn Osland, Ph.D.1 & Pamela Wells, M.S. Organization & Management College of Business San José State University San José, CA 95192-0070 Cassidy Talmadge, the Marketing Manager for the Alabama State Employees’ Insurance Board (ALSEIB), was to manage the public relations aspects of ALSEIB’s wellness program and was taken aback that some of the media reports had been so critical when her employer thought that it was trying to help employees. The media had sensationalized the program by referring to it as a “fat tax.” How can she take the offensive and draw positive attention to the program? Description of the Program Employees receive a $25 discount toward their health insurance premium if they do the following: participate in wellness screenings covering: blood pressure, cholesterol, glucose, and body mass index and if found to be obese, they agree to be monitored by a physician. They don’t even have to lose weight if they participate in the program; they just have to try to lose weight. Alternatively, they could get a doctor’s excuse if there’s a medical reason for non-participation. The normal premium is $50/month for health insurance. Employees are also eligible for a $25/month discount if they don’t use tobacco products. Coupled with the $25 discount for the wellness screenings and follow up, if required, the employees could reduce their health premium to zero. Cassidy served as the Marketing Manager for ALSEIB, the insurance entity that managed the health assessment program for the state. When asked about the program in March 2009, Cassidy believed that although there was some misunderstanding early on members proved happy with the program when it was properly explained. She stated: “It's just a matter of explaining that as long as they are addressing their health risk, they will not be charged the premium. And we are spending a lot of time explaining that obesity is not the only risk factor being screened. Someone with a perfectly healthy BMI may be deemed at risk for hypertension, making them subject to the premium. We are doing our best to convey that obesity is not the ONLY health risk focus in this program.” Cassidy said that the media had been the biggest problem in the roll out of the program. The program was sensationalized by calling it a “fat tax.” Actually, it’s a wellness program comparable to others offered throughout the nation and it doesn’t single out the obese. 1 Direct correspondence to osland_a@cob.sjsu.edu . This case was developed as the basis for classroom discussion and is not intended to illustrate effective or ineffective management. Alabama’s “Fat Tax” 2 ALSEIB’s four insurance advisors located throughout the state contact each agency that has a wellness screening scheduled to offer a meeting with their employees to address any questions or concerns they have prior to the screening date. The employees that cannot attend meetings can inform themselves through the web site, newsletter, and other publications. The State Employees’ Association, an employees union, has been supportive of the program. Cassidy explained, “If the member is found to be at risk for any of the four risk factors, they are provided a referral to visit a physician along with a co-pay waiver form. So, even if they are at risk, they are able to go to their own personal physician, free of charge, and address the issue. In addition, we offer the Weight Watchers at Work ® and YMCA memberships at discounted rates, whether the member is at risk or not.” She added, “… in my opinion, the biggest misunderstanding is that if you are at risk for any of the four risk factors, you will not receive the discount. When, in fact, if the member is at risk and they address this issue w/ their physician or through one of the SEIB approved programs (YMCA or Weight Watchers), they will receive the discount.” On November 18, 2009 she stated that 93% of 38,000 members had been screened. Many that were found to be at risk did not know so. What the program needs is “a few years of claims information to show its savings.” ALSEIB became concerned about rising insurance costs due in part to avoidable illnesses. It decided to monitor the following potential health risks: blood pressure, cholesterol, glucose, and body mass index. Effective January 2010, employees were eligible for the following discounts to their active employee monthly premium of $50: a $25 deduction for non-tobacco use and an additional $25 deduction for wellness participation. Free health insurance is uncommon in the private sector so in this regard Alabama state employees are privileged. Employees desiring to participate in the wellness program receive a referral and a co-pay waiver for a visit to their physician. They then need to certify each year that they are attempting to manage their condition by verifying that they (1) consulted with a physician, (2) participated in a Wellness Management Program, or (3) reduced risks through selfmanagement” (accessed on July 27, 2009 at http://www.alseib.org/PDF/SEHIP/SEHIPFAQEmployeesWantToKnow.pdf ). They receive the discount if they continue under a physician’s care or participate in a wellness program. However, the self-management option requires improvement by reducing the monitored risks. Delaware, Kentucky, and South Dakota also offered “free health screenings and wellness or risk management programs to their state employees” (http://www.mchcp.org/State%20Members/state_OpenEnrollment_WhatsNew.asp ). Arkansas gave employees with very low risk of chronic conditions, as shown in the screenings, additional discounts (Conis, 2008). Arkansas offered a $10 monthly premium discount to each state employee for yearly health screenings as well as discounts for positive screenings that indicated no or low health risks. Missouri offered $15 for individuals and $30 for couples monthly for wellness program participation and (Wolke & Sandoe, October 14, 2008). Alabama’s “Fat Tax” 3 ALSEIB’s program provides the following services: medical and lifestyle histories used to screen individuals at the worksite and provide follow-up testing such as blood pressure, glucose and cholesterol evaluations with professional health counseling follow up administration of flu shots and BMI calculation (plotted on a matrix showing height and weight – see http://www.nhlbisupport.com/bmi/ ) William Ashmore in the Media In an Auburn, Alabama newspaper article (Limerick, September 18, 2008) William Ashmore, the ALSEIB CEO, stated that the wellness program is voluntary. “We’re doing this as an incentive to get employees to participate in the screening,” Ashmore said. “It’s a voluntary program, and the vast majority of employees are appreciative of these programs … The objective is to get as many employees as possible to go through the screenings and for people to understand what risks they have,” Ashmore said. “The main focus of this program is on making each individual employee healthy.” He regarded the relationship between ALSEIB and its employees as mutually beneficial. “Healthy employees cost the health plan less,” Ashmore said. “We would have never gotten the employee association to endorse this program if it discriminates against employees,” Ashmore said. “I fully expect to see more and more states do similar plans,” Ashmore said. “We already have numerous states call in on a daily basis, asking questions about how do we do it (sic), looking at doing something similar to this.” Ashmore added, “Any program of this nature has to be focused on improving the health of employees.” In a CNN interview (Sloane, December 9, 2008), Ashmore added, "Over 10 percent of the people we screen are at risk for one of the factors we're screening for, and the vast majority had no earthly idea they were at risk." He continued, "A healthy employee will cost the program less money." He explained that the emphasis was on education. "What we want to do is, number one, make the employee aware of any risk factors they may have," Ashmore stated, "and then knock down the barriers so that they can go get the services they need." Wellness Wellness programs (Osland & Wells, 2008) are: 1) to reduce cost of healthcare by keeping people well, and 2) to promote a healthier work-force. The program typically includes a health risk assessment questionnaire that measures lifestyle choices and behaviors that may impede wellness. For example, in determining risk factors for disease and illnesses associated with obesity (e.g., cancers, diabetes, high blood pressure, heart disease, and many others), health risk assessment questionnaires may ask for a calculation of the body mass index (BMI). Questionnaires also cover tobacco use. Other illnesses, such as asthma, diabetes, and cardiovascular disease, are all suspected to be associated with some common origins such as decreased physical activity, diet, and obesity. The surveys also sometimes include questions Alabama’s “Fat Tax” 4 about guns and motor vehicle safety as part of the injury prevention section because these are among the leading causes of accidental death and serious injury in the United States. Why do organizations utilize wellness models? A fact report published by the Henry Kaiser Foundation cited that healthcare costs have repeatedly outpaced the growth of the economy (retrieved April 27, 2009 from http://www.kff.org/insurance/upload/7692_02.pdf ). Utilization is the key reason healthcare costs increase each year. The impact on businesses is significant. A dilemma occurs for businesses that wish to attract and retain quality employees. On one hand, the organization must make the compensation package attractive to potential candidates, who have come to expect comprehensive healthcare benefits. One American research study found that healthcare benefits are more important than salary when an employee is choosing where to work (Princeton Survey Research Associates International, 2007). On the other hand, the organization must protect its budget or profit margin. High healthcare costs have a direct negative impact on the organization’s bottom line. Hence, one can understand why an organization might seek measures such as a wellness initiative to reduce healthcare costs. In addition, workers with health problems are absent from the job more than healthy workers (absenteeism), or they come to work, but perform at lower levels, referred to as presenteeism (Samuel & Wilson, 2007). Below is a list of some of organizational concerns with regard to an unhealthy workforce. Decreased profits Decreased morale Increased workplace accidents Increased overhead and Decreased quality of life for the employees caused by chronic disease related to unhealthy behaviors Reducing the risk of a host of chronic diseases including erectile dysfunction. A variety of guides to establishing wellness programs are available on the internet such as: http://www.arkansas.gov/ha/worksite_wellness/index.html http://www.prevent.org/images/stories/Files/publications/Healthy_Workforce_2010.pdf http://www.wellnessproposals.com/about_wellness_proposals.htm http://aspe.hhs.gov/health/prevention/prevention.pdf . Commercially available questionnaires attempt to rank health risks. Such questionnaires are generally based on scientific data that show a correlation between certain lifestyle choices and habits, and resulting illness and disease. Health assessment tools can be effective in pointing out unhealthy lifestyle choices and habits. Risk mitigation could motivate the employee to utilize the health promotion support from the organization. But it’s not enough for most people to simply be aware of what needs to be done; changes such as weight loss frequently require social support and counseling. After the assessment data are reviewed, a risk ranking is often assigned (e.g., high, medium, low). Organizations then encourage the employees to use the results to mitigate risk. People are sometimes given a token incentive to take the test and then another reward should they achieve their targets (e.g., smoking cessation or weight loss). Alabama’s “Fat Tax” 5 A large scale wellness program in King County (Seattle, WA) reported the following results (personal communication, Kerry Schaefer, King County Benefits Strategic Planning, July 30, 2009): The Health Reform Initiative includes BMI in our population as one of the 14 risk factors we measure. We have seen (and maintained over the last 3 years) a drop of more than 2% in BMI. … Our medical plan covers medically supervised weight loss programs for people who have a BMI over 40 or a BMI over 35 plus weight-related medical conditions. There are two programs offered locally which have a good track record of keeping the participant engaged and achieving significant and lasting improvement in health (both programs to continue to track participants 5 or more years after the end of their supervised programs.) Both programs provide individual and group sessions several times a week related to nutrition, exercise and dealing with the psychological components of weight management. These programs are successful but expensive--around $6,000. We're not sure that we can make the business case to open them up to more people. Thus wellness programs can have a positive impact but dramatic changes for the obese can entail expensive specialized programs not included in ALSEIB’s plan. How could Cassidy promote the Wellness program? Cassidy hoped the furor regarding the “fat tax” misrepresentation of the wellness program and premium discount was over. She wondered, “How can we avoid such misunderstanding and the accompanying negative publicity in the future?” She knew that testimonials could prove encouraging to prospective participants. If the State of Alabama saved money on health costs the legislators, ALSEIB, state government and the public would be happy; but the first evaluation was more than a few years off. She wondered what she could do to immediately to draw attention to the wellness program. Perhaps something catchy and humorous would be a way to get people’s attention. References CDC (Center for Disease Control). July 18, 2008. State-specific prevalence of obesity among adults --- United States, 2007. MMWR Weekly, 57 (28): 765-768. (retrieved on August 6, 2009 from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5728a1.htm ). CDC. 2009. (Retrieved on August 3, 2009 from http://www.cdc.gov/obesity/data/trends.html). Conis, E. November 2008. Alabama's wellness premium discount program. Health Policy Monitor. (retrieved on August 3, 2009 from http://hpm.org/survey/us/a12/3). Alabama’s “Fat Tax” 6 Fernandez, D. 2008. Alabama 'Obesity Penalty' Stirs Debate: Plan Calls for State Employees to Pay More for Health Insurance if They Don't Lose Weight. WebMD Health News; Reviewed By Louise Chang, MD. Aug. 25, 2008 — Obese Alabama state workers may soon pay a health insurance penalty for their excess pounds (retrieved on April 21, 2009 from http://www.medicinenet.com/script/main/art.asp?articlekey=92151). Glover, M. A. Winter, 2008. Employment & disability law – Americans with Disabilities Act of 1990 – the weight of personal responsibility: obesity, causation, and protected physical impairments. University of Arkansas at Little Rock Law Review, 381 Goldstein, J. August 12, 2009. Should employers be allowed to deny jobs to the morbidly obese? Health Blog - WSJ's blog on health and the business of health (Retrieved on August 24, 2009 from http://blogs.wsj.com/health/2009/08/12/should-employers-be-allowed-to-denyjobs-to-the-morbidly-obese/ ). Limerick, G. September 18, 2008. Alabama initiates new health care plan. Auburn Statesmen. Osland, A. and Wells, P. 2008. Gunning down health assessment. Journal of Critical Incidents, 1: 35-41. Sloane, M. December 9, 2008. Alabama to link premium costs to workers' health. CNN. Wolke, A. and Sandoe, E. October 14, 2008. Improving the state of state employees’ health: Alabama acts. State Health Notes, 29. Issue 525. National Conference of State Legislatures (retrieved on August 5, 2009 from http://www.ncsl.org/IssuesResearch/Health/IMPROVINGTHESTATEOFSTATEEMPLOYE ESHEALTHAL/tabid/14197/Default.aspx ).