I. What is Parkinson's Disease?
advertisement
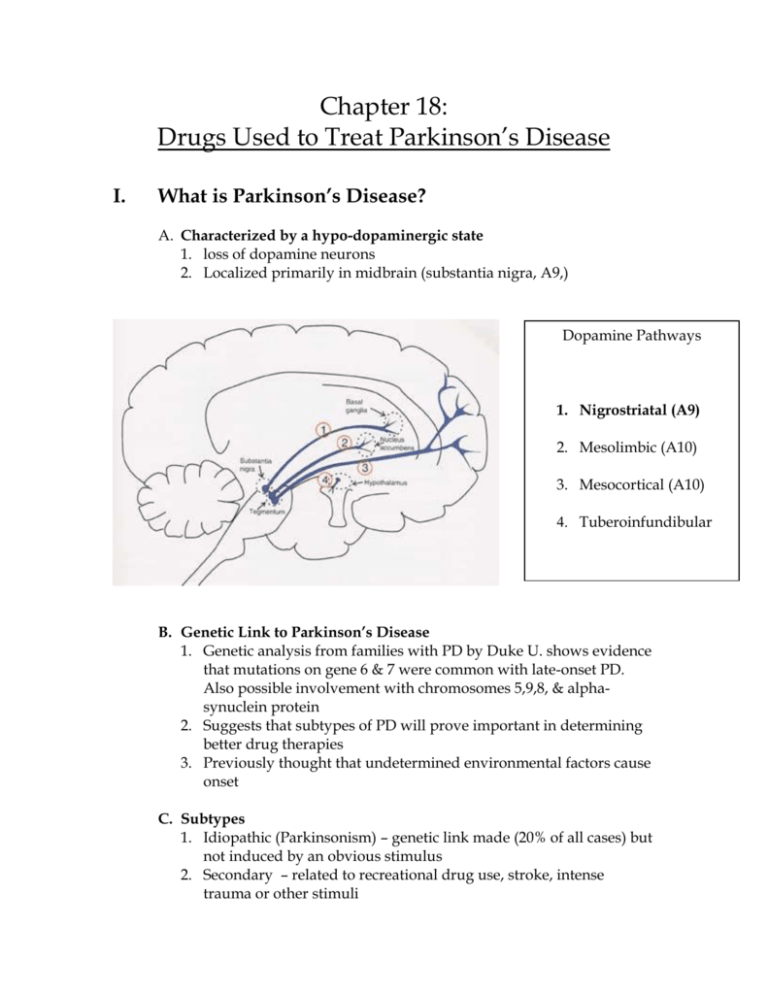
Chapter 18: Drugs Used to Treat Parkinson’s Disease I. What is Parkinson’s Disease? A. Characterized by a hypo-dopaminergic state 1. loss of dopamine neurons 2. Localized primarily in midbrain (substantia nigra, A9,) Dopamine Pathways 1. Nigrostriatal (A9) 2. Mesolimbic (A10) 3. Mesocortical (A10) 4. Tuberoinfundibular B. Genetic Link to Parkinson’s Disease 1. Genetic analysis from families with PD by Duke U. shows evidence that mutations on gene 6 & 7 were common with late-onset PD. Also possible involvement with chromosomes 5,9,8, & alphasynuclein protein 2. Suggests that subtypes of PD will prove important in determining better drug therapies 3. Previously thought that undetermined environmental factors cause onset C. Subtypes 1. Idiopathic (Parkinsonism) – genetic link made (20% of all cases) but not induced by an obvious stimulus 2. Secondary – related to recreational drug use, stroke, intense trauma or other stimuli D. Incidence 1. Apx. 500,000 Americans suffering from Parkinson’s today 2. 1% of all adults over 65 3. only clinically diagnosed when dopamine levels are at 20% of normal E. Clinical Features 1. Four primary clinical symptoms: bradykinesia – (aka on/off function) difficulty initiating or stopping movements muscle “cogwheel” rigidity – seen as motion lock motion lock, etc. (demonstrate) resting tremor gait disturbances – shuffling feet and disturbances in posture 2. Many secondary afflictions (See Table 18.1 in Book) F. Types of Treatment 1. Dopamine replacement therapy (drugs) dopamine agonists dopamine breakdown inhibitors, ex: COMT inhibitors 2. Alternative therapies stem cell theory/ implants Pallidotomy 3. Additional considerations exercise physical therapy cognitive therapy acupuncture support groups G. Goals of Treatment 1. Replace dopaminergic function 2. Reverse loss of dopamine 3. Give patient a chance to live a normal life as possible keep patient healthy with exercise and proper diet keep patient in a positive mind frame II. Drug Treatment A. L-DOPA (levodopa) Logic states that if Parkinson’s is caused by a loss of dopamine then a drug should be used to replace that lost dopamine Dopamine itself does not cross the blood-brain barrier Precursor DOPA (dihydroxyphenylalanine) does and is then converted to dopamine Only 1-5% of administered L-DOPA crosses the blood-brain barrier but that is enough to have an effect 1. L-DOPA has 2 main problems it is destroyed by intestinal enzymes in the periphery, L-DOPA is converted to dopamine with negative side effects (inc. blood pressure and nausea) solution is Carbidopa 2. Carbidopa inhibits the enzyme dopa-decarboxylase in the PNS but not the CNS this lowers the ED for L-DOPA (same positive results in lower dose) Sinemet (Carbidopa-Levodopa) is the current drug of choice in treating Parkinson’s disease 3. Limitations of Carbidopa-Levodopa short half life means symptoms will return a few hours after taking the drug within a span of 2-5 years after taking the C-L therapy its effect will diminish cause for this is unknown, but there are ways to prolong the drug’s effects: increase the dose, decrease the intervals between doses, add a COMT inhibitor B. COMT Inhibitors (Peripheral) 1. COMT converts L-DOPA to 3-ortho-methyl-dopa which has no clinical benefits 2. COMT also decreases the half-life of C-L and shortens its clinical effects 3. By inhibiting peripheral COMT half-life of C-L will increase as will its clinical effects 4. It is thought that by inhibiting peripheral degradation of levodopa, the levels of central levodopa will increase hence creating higher dopamine concentrations 5. Two COMT inhibitors on the market: Tolcapone (Tasmar) – introduced in 1998 but has been shown to cause liver damage Entacapone (Comtan) – introduced in 2000 and so far no adverse side effects known C. Dopamine Receptor Agonists 1. Goal of new therapy is to find drugs that stimulate postsynaptic dopamine receptors in basal ganglia 2. This would avoid transformation to metabolites 3. Four dopamine receptor agonists are on the market Bromocriptine (Parlodel) – introduced in 1978, derived from ergot alkaloid lysergic acid, marginally effective, many bothersome side effects (find some!) Pergolide (Permax) – introduced in 1989, also derived from ergot alkaloid lysergic acid, marginally effective, many side effects Pramipexole (Mirapex) and Ropinirole (Requip) – both introduced in 1997, greater affinity for dopamine3 receptors than dopamine2 receptors, significance of dopamine3, receptors unclear, recommended for early-onset of Parkinson’s, longer half-lives than C-L, side effects: dizziness, nausea, hallucinations, insomnia D. MAO-B inhibitors 1. MAO-B has affinity for dopamine neurons 2. (look this stuff up first about MAO-B) 3. Selegiline (1-Deprenyl, Eldepryl) – inhibits MAO-B this preserves small amounts of dopamine used in younger patients to delay need for C-L therapy one primary side effect: two metabolites produced are amphetamine and methamphetamine E. Muscarinic Receptor Agonists 1. Used to control tremors 2. Work in 50% of patients but do not reduce rigidity or bradykinesia 3. Two main muscarinic agonists used: Trihexphenidyl (Artane) Procyclidine (Kemadrin) Alternative Treatment A. Pallidotomy 1. last resort if medicine no longer controls symptoms. only performed on patients < 70 years old without dementia 2. 4. 5. 6. improves rigidity, tremors, dyskinesia, freezing, and falling NOT a cure for Parkinson’s disease Performed on the hemisphere opposite of the worst symptoms Procedure: Stereotaxic surgery, MRI and an electrode are used to produce a lesion on the globus pallidus while the patient is awake under local anesthesia 7. If lesions on both sides are needed, additional surgery is preformed at a later time 8. Some improvement can be seen in the operating room 9. Surgical Risks: typical anesthesia related, abscess or meningitis (result from excess fluid from infection and clotting), strokes and bleeding can cause paralysis or death, speech problems, partial blindness, symptoms may not improve 10. Medication must be resumed after procedure B. Fetal Cell Implants (US, UK, Sweden, & Germany) 1. Dopamine producing fetal cells implanted in the brain 2. May show dramatic improvements in function 1-3 months after implants. Possible to restore speech and walking. Reduces need for medicine, but still not a cure. 3. Negative irreversible effect is that fetal cells have been shown to produce too much dopamine after ~one year, which leads to same side effects as with too much prescribed medication. Tumors have also occurred 4. Still experimental and there is a further need for research, even though research opportunities have strict guidelines 5. Rodent studies w/ fetal cells are helping scientists to better understand and control how and where stem cells produce dopamine. Hopefully this will reduce side effects III. Relation to other disorders A. Schizophrenia? 1. Condition called secondary Parkinsonism, or neuroleptic-induced parkinsonism, can result from taking anti-schizophrenic medications including anti-psychotics such as haloperidol, metoclopramide, and phenothiazine. This is usually reversible by lowering the dosage. 2. A9 & A10 pathways affected by dopamine in both PD & schizophrenia 3. Symptoms of secondary Parkinsonism: rigidity, bradykinesias, tremor and restlessness. Also tardive dyskinesias, (motor disorders) can occur and be permanent 4. There is no finite evidence surrounding a reverse connection of Parkinson’s drugs producing schizophrenic effects B. Depression 1. Present in about 40% of patients 2. Greater risks of anxiety, sadness without guilt or self-blame, lower suicide rates despite high rates of suicidal thought compared to depressed patients without PD 4. Hard to measure and diagnose in the context of this illness 5. Loss of nerve cells in the locus coerleus and substantia nigra may be similar to non-motor symptoms of PD which may also contribute to depression 6. Medications for depression are prescribed, but there is a need to determine which types work best. Currently SSRI’s are used over TCA’s because they are less sedative IV. Interesting websites: http://www.nlm.nih.gov/medlineplus/parkinsonsdisease.html http://www.x-plain.com http://parkinsonsinfo.com http://pdf.org http://www.1uphealth.com/ http://michaeljfox.org http://www.ninds.nih.gov http://www.pfizer.com/brain http://wings.buffalo.edu/aru/Parkinsons.html



![[1] Edit the following paragraph. Add 4 prepositions, 2 periods](http://s3.studylib.net/store/data/007214461_1-73dc883661271ba5c9149766483dcfed-300x300.png)

