Drugs used to treat Parkinsons disease and Schizophrenia
advertisement

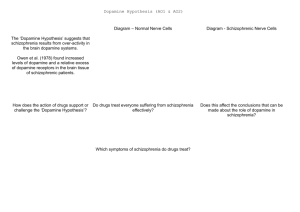
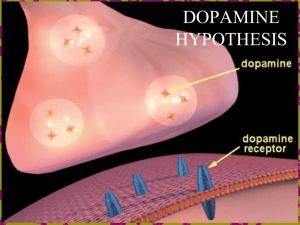
Pharmacology 18c - Drugs used to treat Parkinson’s disease and Schizophrenia Anil Chopra 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Describe the synthetic and metabolic pathways of the neurotransmitter dopamine. What are the three main dopaminergic pathways in the brain and what are their basic functions. What are the two main sub-groups of dopamine receptors. Describe the main clinical features of Parkinson’s disease. Which age group of the population is affected by Parkinson’s disease. What are the main pathological and biochemical features of Parkinson’s disease. Do the symptoms of Parkinson’s disease appear immediately. Can dopamine itself cross the blood brain barrier. In standard preparations what drug is combined with L-DOPA to prevent peripheral side effects. What are the short and long-term side effects of L-DOPA therapy and how common are such side effects experienced. In the treatment of Parkinson’s disease how does the mechanism of action of bromocriptine differ from that of L-DOPA. By what mechanism can Deprenyl be utilised to reduce the dosage of L-DOPA required. How do the COMT inhibitors and the MAO inhibitors differ in their mechanism of action. Describe the clinical symptoms of schizophrenia. Which age group are most likely to be affected. What is the principle neurotransmitter defect in schizophrenia. Are neuroleptic drugs selective for dopamine receptors. Apart from anti-schizophrenic actions, what are other effects produced by neuroleptic drugs that are due to antagonism at dopamine receptors. What are acute and tardive dyskinesias and when do they occur in the treatment of schizophrenia. What are the other unwanted side-effects of neuroleptics that are unrelated to their blockade of dopamine receptors Tyrosine Hydroxylase (rate limiting step) Tyrosine DOPA Decarboxylase DOPA Reuptake by pre-synaptic cell, repackaging into vesicles COMT = catechol-O-methyltransferase MAO = monoamine oxidase Metabolism into excretable metabolites Dopamine Storage in vesicles, and release via exocytosis COMT MAO Dopamine Pathways There are a number of different pathways that dopamine neurones travel along: Nigrostriatal pathway: Cell bodies originate in the substantia nigra zona compacta and project to the striatum – Initiation and Control of Movement. Mesolimbic pathway: Cell bodies originate in the ventral tegmental area and project to the nucleus accumbens, frontal cortex, limbic cortex and olfactory tubercule Involved in emotion and perception. Tuberoinfundibular system: Short neurones running from the arcuate nucleus of the hypothalamus to the medial eminence & pituitary gland - Regulate hormone secretion. Dopamine Receptors D1-like Family • D1 & D5 • G-protein linked • Second messenger - increase in cAMP • Postsynaptic • found mainly in nigrostriatal & limbic system D2-like Family • D2, D3 & D4 • G-protein linked • Second messenger - decrease in cAMP or increase in K+ • Pre & Postsynaptic • Limbic - D2, D3, D4 • Nigrostriatal - D2 • Pituitary - D2 Parkinson’s Disease A progressive neurodegenerative disorder of movement first describe by James Parkinson in 1817. Characterised by loss of pigmented cells in pars compacta of substantia nigra and depressed striatal dopamine. • • • • • 1 in 1000 of the general population. 1 in 100 of those aged over 60 years of age. Mean age of onset is 65years but younger people can develop the disease. Women are less likely to develop the disease than men (4:1 males: females) It is a disease of long duration and is progressive in nature. Signs & Symptoms of Parkinson’s Disease Rest tremor – Shaking of the limb when relaxed Rigidity – Stiffness, limbs feel heavy/weak Bradykinesia – slowness of movement Postural abnormality – flexion of neck and trunk, lack of arm swing. Difficulty with fine movements –micrographia. Poverty of blinking. Impassive face. Monotony of speech & loss of volume of voice. Disorders of posture – flexion of the neck and trunk Lack of arm swing Swallowing difficulties Loss of balance – lack of righting reflex, retropulsion Short steps, shuffling gait and festination. Symptoms appear on one side of the body first (unilateral onset) and then spread to both sides of the body. Generally symptoms worsen with the patient becoming severely disabled. Secondary Symptoms can include Depression Pain Taste-disturbances Dementia Autonomic dysfunction o Constipation o Postural hypotension o Urinary frequency/urgency o Impotence o Increased sweating Pathogenesis of Parkinson’s Disease Parkinson’s disease is mainly caused by cell loss in the substantia nigra. Other parts of the brain such as the coeruleus, Dorsal Vagus Nucleus and Nucleus Basalis of Mynert can also be affected by to a lesser degree. The main characteristic is a loss of dopamine in the caudate and putamen. This loss needs to be significant: it is necessary to loose 80-85% of the dopaminergic neurons and deplete 70% of the striatal dopamine before symptoms appear. Treatment of Parkinson’s Disease Name – L-DOPA Sinamet (Carbidopa + L-DOPA) Madopar (Benserazide + L-DOPA) Usage Hypokinesia, rigidity & tremor Mode of Action Because most of the L-DOPA that is administered into peripheral tissues is converted straight into dopamine, L-DOPA is normally co-administered with a peripheral LDOPA decarboxylase inhibitor. It replaces the lost dopamine. - Dopamine itself cannot cross the blood brain barrier (only at the chemotactic trigger zone vomiting) - Cannot give tyrosine because the conversion of tyrosine to L –DOPA is the rate limiting step! Side Effects ACUTE • Nausea - prevented by Doperidone (peripheral acting antagonist) • Hypotension • Psychological effects - Schizophrenia like syndrome with delusions, hallucinations, also confusion, disorientation & nightmares. CHRONIC • Dyskinesias - Abnormal movements of limbs & face. • “On-Off” effects - Rapid fluctuations in clinical state. Off periods may last from minutes to hours. Occurs more with L-DOPA Dopamine Agonists Names Bromocriptine, Lisuride, Pergolide, Ropinirole, Cabergoline, Apomorphine Usage Parkinson’s Disase Mode of Action • Act on D2 receptors • Longer duration of action than L-DOPA • Smoother & more sustained response • Actions independent of dopaminergic neurons • Incidence of dyskinesias is less Side Effects • Common - Confusion, dizziness, nausea/vomiting • Rare - Constipation, headache, dyskinesias, drowsiness & hallucinations Monoamine Oxidase Inhibitors Name - Deprenyl Usage – Parkinson’s disease Mode of Action – it is an inhibitor of Monoamine Oxidase B which is predominantly found in the dopaminergic areas of the CNS. Side Effects and Pharmacokinetics – can be given on its own or with L-DOPA (if given with L-DOPA then reduce dose by 30%). Has no peripheral side effects. Side effects: RARE (nausea vomiting) - hypotension - confusion - agitation COMT Inhibitors Names Tolocopone (peripheral) Entacapone (peripheral + CNS) Usage Parkinson’s disease Mode of Action – COMT causes the breakdown of dopamine in the CNS, therefore its inhibition will maintain dopamine levels. COMT in the periphery converts L-DOPA to 3-0-methyl-DOPA (3-0MD). 3-OMD and L-DOPA compete for same transport system into the brain. COMT inhibitors stop 3-OMD formation thus increasing the bioavailability of L-DOPA, Thus more L-DOPA converted to dopamine in the CNS. Schizophrenia Schizophrenia affects around 1% of the general population. It normally manifests itself in adolescence or young adulthood and there are 2 types: A) Relapsing and remitting B) Chronic and progressive Symptoms of Schizophrenia • Positive symptoms - Delusions, hallucinations, Thought disorders. • Negative symptoms - Withdrawal, Flattening of emotional responses. Causes and Risk Factors of Schizophrenia There has been a strong hereditary link shown: - 10% increase risk in first degree relatives - 50% increase risk in monozygotic twins There is a possible viral link with an autoimmune response. Possibly caused by a developmental abnormality in the amygdala or temporal lobes. The positive symptoms of schizophrenia are caused by dopamine hypersensitivity - Dopamine agonists induce psychotic symptoms Neurochemical Involvement: - Dopamine hyperactivity underlies at least the positive signs of schizophrenia - Dopamine agonists (e.g. bromocriptine) can induce schizophrenic behaviour - Typical anti-schizophrenic drugs are dopamine receptor antagonists - Drug naïve patients show increased dopamine receptor numbers – up to 6x increase Changes in other transmitters such as 5-HT and NA which also strongly interact with dopaminergic pathways Neuroleptics Names – Chlorpromazine, fluphenazine, haloperidol, clozapine, sulpride Usage – Schizophrenia, nausea, vomiting, motion sickness Mode of action – they are antagonists at dopamine “D2 like” receptors thus stopping the effects of increased dopamine, however it takes many weeks to occur – initially the synthesis of dopamine is increased and only lowers slowly with time. This treats only the positive symptoms not the negative ones. All the drugs have effects at some other receptors (5-HT) which gives them their side effects. Clozapine in particular antagonises D4 receptors which are shown to be over-expressed in schizophrenia. They are anti-emetic because the dopamine receptors in the chemoreceptor trigger zones are blocked and used in motion sickness for their anti-histamine properties. Side Effects Can induce “Parkinson” like side effects due to decrease d dopamine. Acute dyskinesias (intermittent muscular spasms, affecting especially face and neck) due to increased cholinergic function. These can be treated with anticholinergics. Tardive dyskinesias – involuntary movements, usually of the face. These cannot be treated with anti-cholinergics but only occur in long term use of neuroleptics. Endocrine effects – e.g. lactation and swelling of breasts. This is caused by the inhibition of dopamine receptors in the infundibular system which includes the pituitary gland. Neuroleptics cause increase serum prolactin. Antagonism of Muscarinic receptors – this can have typical anti-muscarinic side effects such as blurring of vision, increased intra-ocular pressure, dry mouth, constipation, urinary retention. Anti-emetic: o Block dopamine receptors in the chemoreceptor trigger zone. Phenothiazine effective in controlling vomiting – e.g. chemotherapy associated, or in renal failure o Also have a blocking action at histamine receptors – blocking motion sickness



![[1] Edit the following paragraph. Add 4 prepositions, 2 periods](http://s3.studylib.net/store/data/007214461_1-73dc883661271ba5c9149766483dcfed-300x300.png)