Table 3. Lung Function Test in Placebo group
advertisement

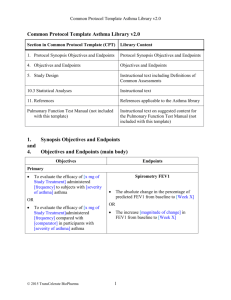
Efficacy of Inhaled Budesonide in the Treatment of Childhood Asthma Ariyanto Harsono, Mario B Nara, Anang Endaryanto Division of Allergy-Immunology of Child Health Dr. Soetomo Hospital/ Airlangga University Surabaya Abstrak Latar belakang: Budesonid hirupan merupakan glukokortikoid dengan rasio efek topical yang lebih baik dari efek sistemik. Perbaikan klinis pada penggunaan budesonide untuk asma ringan telah banyak dilaporkan, tetapi perbaikan fungsi paru masih banyak perselisihan. Penelitian ini mempelajari penggunaan budesonid hirupan pada pengobatan asma anak dengan menggunakan parameter uji fungsi paru. Tujuan: Untuk mengevaluasi efektifitas budesonid hirupan pada asma anak dengan menggunakan parameter uji fungsi paru. Metode: Penelitian Prospektif, longitudinal, buta ganda tersamar membandingkan budesonid hirupani dengan plasebo pada anak dengan asma sedang. Randomisasi dilakukan dengan cara “Systematic random sampling”. Besar sampel ditentukan 30 pasien tiap grup untuk memenuhi distribusi normal. FEV-1 dan FVC diukur mengambil 3 terbaik sebelum dan sesudah hirupan terbutalin pada waktu pemeriksaan awal dan sesudah 2 tahun perlakuan. Nilai % prediksi FEV-1 dan FVC didapatkan dari nilai yang didapat dibandingkan dengan harga normal menurut ras, umur, jenis kelamin dan tinggi badan. Perubahan FEV-1, FVC, % prediksi FEV-1, % prediksi FVC pada kedua grup pada pemeriksaan awal dan akhir dianalisa menggunakan “paired t-test”. Mann Whitney U test dipakai untuk membandingkan karakteristik grup budesonid dan plaasebo. Hasil: Tidak ada perbedaan pada nilai FEV-1 (mean 1.68+0.35: 1.65+0.48), FVC (mean 1.86+0.39: 1.92+0.57) and FEV-1 Reversibility (mean 7.42%+5.86%: 11.08+9.20) antara grup budesonide dan placebo setelah pengamatan 2 tahun, tetapi ada perbedaan bermakna pada % prediksi FEV-1 antara kedua grup (mean: 94%+9.62%) pada grup budesonid dengan p=0.004. Kesimpulan: terjadi perbaikan uji fungsi paru yang ditunjukkan dengan perbaikan % prediksi FEV-1 pada pemakaian budesonid hirupan selama 2 tahun pada penderita asma anak ABSTRACT BACKGROUND: Budesonide is an inhaled glucocorticosteroid with a favorable ratio between topical anti-inflammatory activity and systemic activity. The improvement of clinical indices is well establish in the use of budesonide in mild asthma, but the beneficial effect of this drug indicated by lung function test is inconsistent. We prospectively investigated the use of inhaled budesonide in controlling asthma in children by lung function tests evaluation. OBJECTIVE: To evaluate the efficacy of budesonide inhaler in children with asthma using Lung Function Tests. METHODs: This was a 2 years prospective longitudinal study, double blind, randomized, controlplacebo study comparing budesonide inhalation or placebo in 51 children ages 6 to 12 years old, with mild asthma. The best of three FEV-1 and FVC value were measure before and after terbutalin inhaler in baseline and after 2 years observations. The value of % predicted FEV-1 and FVC were measure by compare the FEV-1 measurement with normal value for race, age, sex and 2 height. The change of FEV-1, FVC, % predicted FEV-1, % predicted FVC from budesonide and placebo groups at baseline and after 2 years were analyzed by use paired t- test statistical test. Mann-Whitney test was used to compair between budesonide and placebo groups characteristics. RESULTS: There were no different in the value of FEV-1 (mean 1.68+0.35: 1.65+0.48), FVC (mean 1.86+0.39: 1.92+0.57) and FEV-1 Reversibility (mean 7.42%+5.86%: 11.08+9.20) between budesonide and placebo group after 2 years observation, but there was significant different in the value of %predicted FEV-1 (94%+9.62%) in favour of Budesonide group in the end of investigation (p.0.004) CONCLUSION: There is significant improvement of the Lung Function Test (% predicted FEV-1) after the use of budesonide in the treatment of asthma in children. Key words: Asthma, budesonide, lung function tests Abreviation used: FEV-1: Forced Expiratory volume in 1 second FVC: Forced volume Capacity. LFT: Lung Function Test. INTRODUCTION Asthma is chronic inflammatory disease with clinical manifestation that result from variable airflow obstruction. The incidence and prevalence of asthma in children in the world were variable between 0.06% until 11.4%. National statistics in USA show that asthma prevalence, morbidity, and deaths are increasing, and children appear to be at highest risk. Hospitalization rates for asthma from 1980 to 1993 were highest among persons 4 years of age and younger, and asthma accounts for one third of pediatric emergency department visits. (1,2,3) Childhood asthma is one of the most common illnesses, good clinical skills are essential for optimal treatment. Lung Function Test (LFTs) are an important part of good asthma management. However, clinical impressions of the degree and severity of the disease may be unreliable unless made in conjunction with results of LFTs. (4) While LFTs are not diagnostic of specific lung diseases, they provide an objective assessment of airway function, airway narrowing and changes in airway caliber. They offer a method to determine whether airway obstruction exists, its degree and its response to triggers and treatment. One of the major planks of the Asthma Management Plan is to assess severity accurately and this can only be done with LFTs. Because growth has a major effect on lung function, spirometer values need to be interpreted with the aid of a table or graph giving normal values for FEV-1, FVC in relation to the sex and height of the child. (5,6)) Spirometric measures, principally FEV-1, have long been used as marker of the degree of airway obstruction. The National Asthma Education and Prevention Program as an important means for grading quality of life endorse FEV-1. FEV-1 had been used widely in the world as an instrument of evaluation of disease progressions. (1) The disadvantages of FEV-1 to test of the lung function are FEV-1 use same categories in measured pediatric and adult population, whereas the growth has a major effect on lung function. (7) In children, pyrometer is an indispensable tool for assessing the degree of inflammatory airway obstruction and providing accurate information for medication adjustment. Pyrometer is the most reliable tool to make an accurate assessment of lung function. The problem of using FEV-1 in a test of lung function in children is the inconsistent result between clinical and functional 3 improvement. In long-term follow-up study before reported that the improvement of clinical indices is well establish in the use of budesonide in mild asthma, but the beneficial effect of this drug indicated by LFTs is in consisted. While FEV-1 and other parameter of LFTs are inconsistent between the result and the clinical impressions of the degree and severity of the disease, they provide an objective assessment of airway function, airway narrowing and changes in airway caliber. (5,6,7) Managing asthma, assessing the degree of inflammatory airway obstruction and providing accurate information for medication adjustment without measuring spirometry is impossible. Therefore, an exertion to find the precise parameter of LFTs to asses the improvement of lung function as well as the clinical indices must to be done. The long-term follow-up study needed to found it. The purpose of this study was to evaluate the LFTs, such as FEV-1, FEV-1 Reversibility, FVC and % predicted FEV-1 (a predicted normal range, based on age, sex, height and race) in the use of Budesonide inhaler in children with asthma. METHODS Patients with asthma aged between 6-14 years with onset of disease of less than 2 years were selected to take part in this study. Thorax photo, Mantoux test, peripheral blood, urine and feces examination was done before the visit to exclude the possibility of other diseases causing chronic cough. Patients should not take antihistamines, corticosteroids, symphatomimetics and xanthenes 48 hours prior to allergy testing. Patients who fulfill all of the inclusion criteria and none of the exclusion criteria were recruited in this study. Inclusion criteria: 1. Prior to conducting any study related procedures, signed informed consent from Patient or parent or legal guardian must be obtained. The investigator inform obviously about the purposes and procedures of the study. 2. Outpatients of either sex, aged between 6-14 years. 3. Ability to use Turbuhaler correctly confirmed with a Turbuhaler Usage Trainer (TUT). The patient should be able to light at least two of three indicator lamps on the TUT display. 4. Asthma diagnosis made preferably within I year but not more than 2 years prior to the visit. The diagnosis should be verified by both of the following: Symptom at least once a week, but not as often as everyday during 3 month. Preceding the visit patient must have experienced one of the following: Wheeze, cough, dyspnea, chest tightness or night wakening due to any of these symptoms. Cough, as an isolated symptom may be present everyday. Reversible airway obstruction, demonstrated as historical data or assessed at the visit as one of the following: A. Increase of FEV-1 of more than 12% compared with baseline after inhalation of a short acting bronchodilator, in this study is 0,5mg Terbutalin Turbuhaler. Reversibility in FEV-1 relative to predicted normal is formulated as: FEV-1 after bronchodilator-FEV-1 before bronchodilator ----------------------------------------------------------------------- X 100% FEV-1 Predicted normal 4 B. PEF variation of more than 15% without bronchodilator, calculated out of 14 days period after discarding the first 3 days, is formulated as: (A1+A2)-(B1+B2) ----------------------- X 100% (A1+A2) A1=highest PEF A2=second highest PEF B1=lowest PEF B2=second lowest PEF Exclusion criteria: 1. Symptom compatible with diagnosis of asthma for more than 2 years prior to the visit. 2. Patient for whom it would be inappropriate to delay chronic treatment with Glucocorticoids as judged by physician at the visit. 3. Patient with a history of more than 30 days per year of oral or inhaled Glucocorticoids, or one depot injection per year of glucocorticoid irrespective of reason within 2 years prior to the visit. 4. Regular, at least once daily antiasthma treatment for more than two years prior to the visit. 5. Pre bronchodilator FEV-1 less than 60% predicted normal value at the visit. 6. Post bronchodilator FEV-1 less than 80% of predicted normal value at the time of visit. 7. Other concomitant cardiopulmonary diseases such as Cystic Fibrosis, active untreated tuberculosis, bronchopulmonary displasia, and severe congenital heart disease. 8. Immunosuppressive therapy. 9. Cancer as past and present diagnosis. 10. Patients with known or suspected difficulty in complying with the study protocol as judged by investigator. Data collection: Demographic data consisted of age, sex are recorded along with weight and height. The medical record of each patient is reviewed to confirm the diagnosis of asthma including BCG scar, Mantoux test, thorax photo, atopy status, history of other atopic disease, history of atopic disease in the family, onset of asthma, frequency of attack, total days of each asthmatic attack, intensity of asthmatic attack, frequency of nocturnal asthma total days of nocturnal asthma, addition of drugs, total loss of school day between two visit, total loss of daily activity between two visit, adverse reaction related to Tilade,adverse event unrelated to Tilade and symptoms at the time of visit. Study design: The study is an open comparative study comprising of two groups: Group A (with Budesonide inhaler treatment) and group B (control). Variable that will be compared between these two group are: FEV-1 pre and post Brochodilator, FVC pre and post bronchodilator, % predicted FEV-1 pre and post Bronchodilator, FEV-1 reversibility pre and post Bronchodilator. The dose of Budesonide is estimated 200 mcg daily for children age 6-11 years, and 400 mcg for children age more than 11 years . Assessment of lung functions at the visit 1 and at the end of study. Assessment of the lung functions: During the LFTs, the patient sits and may use nose clip. The patient must not have inhaled short acting or long acting bronchodilator 6 hours and 24 hours respectively prior to the procedures. The largest FEV-1 value and the largest FVC are recorded out of three technically satisfactory expiration even if two values do not come from the same curve. The largest FEV-1 and FVC, and the second largest FEV-1 and FVC from acceptable curves should preferably not vary more than 5 5%. If they differ by more, further measurement should be performed until this condition is met. Pre bronchodilator FEV-1 should be compared predicted normal value. This should be not below 60% of predicted normal value at visit 1. Inhalation of terbutalin 0.5 mg turbuhaler than to be initiated. Fifteen minutes then the procedure to be repeated. The post bronchodilator FEV-1 value should not be below 80% of predicted normal value at visit 1. Reversibility in FEV-1 relative to predicted normal value should not be less than 13% at visit 1.If it is less than 13%, PEF variability examination should be performed. The result of PEF variation should not be less than 15%. Analysis of result: All of data were computerized as database. Paired samples t-test was used to compare variables of the two groups. Mann Whitney U test was used to compare the characteristics of Budesonide and Placebo group. RESULT A total of 63 subjects was randomized to study treatment: 25 to the placebo group and 26 to the budesonide inhaler groups, respectively. LFTs and demographic characteristics at enrollment are shown in Table I . Table 1. Patients Characteristic Budesonide (n=26) Placebo (n=25) 16(61.5%) 15(57.7%) 10(38.5%) 10(38.5%) Age (y) 8.4+1.7 9.0+1.3 Weight (kg) 26.4+7.1 24.7+6.9 Height (cm) 126.3+11.2 127.1+9.1 FEV-1 1.08+0.2 1.15+0.3 % Predicted FEV-1 75.1+10.1 76.2+9.5 Reversibility (%) 21.1+8.4 19.0+10.0 FVC 1.25+0.2 1.32+0.3 %Predicted FVC 76.0+10.5 75.8+10.7 Sex: Male Female Two subject (1 in each of the budesonide and placebo groups) were excluded in this study because they were not control routinely. . There were no significant differences among the groups in sex, age, height, weight and pulmonary function (FEV-1, % predicted FEV-1, FEV-1 Reversibility, FVC and % predicted FVC) at baseline of the study. The mean of % predicted FEV1 in each groups are 75.1+10.1 and 76.2+ 9.5, so the patients include to mild-moderate asthma Table 2. Lung function test in Budesonide group Baseline After 2 years Means change P 6 FEV-1 before bronchodilator 1.08+0.20 1.56+0.35 -0.49 0.00 FEV-1 after bronchodilator 1.31+0.22 1.67+0.35 -0.36 0.00 % Predicted FEV-1 before bronchodilator 75.11+10.95 88.15+11.46 -13.03 0.00 % Predicted FEV-1 after bronchodilator 90.12+9.18 94.19+9.62 -4.07 0.04 Reversibility (%) 21.11+8.4 7.42+5.85 13.69 0.00 FVC before bronchodilator 1.25+0.23 1.84+0.37 -0.59 0.00 FVC after bronchodilator 1.45+0.25 1.86+0.38 -0.40 0.00 % Predicted FVC before bronchodilator 76.03+10.54 90.42+10.80 -14.38 0.00 % Predicted FVC after bronchodilator 87.38+9.76 92.84+10.19 -5.46 0.01 There are significant improvement (p<. 05) in The value of FEV-1, % predicted FEV-1, FEV-1 reversibility, FVC and % predicted FVC in Budesonide group after 2 years observation (Table 2). But in placebo group, there is no significant improvement in %predicted FEV-1 value after 2 years observation (means before inhalation 76.16 + 9.49:: 80.2 +9.69,p=0.07, after inhalation 90.36+8.73: 84.72+18.11, p=0.13) (Table 3) Table 3. Lung Function Test in Placebo group Baseline After 2 years Means change P FEV-1 before bronchodilator 1.15+0.28 1.42+0.42 -0.33 0.00 FEV-1 after bronchodilator 1.36+0.28 1.65+0.48 -0.29 0.00 7 % Predicted FEV-1 before bronchodilator 76.16+9.49 80.20+9.69 -4.04 0.074 % Predicted FEV-1 after bronchodilator 90.36+8.73 84.72+18.11 5.64 0.132 Reversibility (%) 19.00+10.01 11.08+9.20 7.92 0.009 FVC before bronchodilator 1.32+0.35 1.81+0.52 -0.49 0.00 FVC after bronchodilator 1.49+0.34 1.92+0.56 -0.42 0.00 75.80+10.77 85.32+10.95 -9.52 0.001 86.12+9.04 90.16+11.27 -4.04 0.018 % Predicted bronchodilator % Predicted bronchodilator FVC FVC before after Next, after compare the result of pulmonary function test in budesonide and Placebo groups used Mann-Withney statistic test, we found there are significant different in the value of % predicted FEV-1 before inhalation (88.15+ 11.46:80.20+9.69, p 0.01) and after inhalation (94.19+9.62: 84.72 +18.11,p 0.01). (Table 4) Table 4. Comparison between Budesonide and placebo group after 2 years observation Budesonide Placebo P Mean rank Sum of rank Mean rank Sum of rank FEV-1 before bronchodilator 29.25 760.50 22.62 565.50 0.11 FEV-1 after bronchodilator 27.33 710.50 24.62 615.50 0.52 % PredictedFEV-1 before bronchodilator 31.29 813.50 20.50 512.50 0.01 bronchodilator 31.00 8.06 20.80 520.00 0.01 Reversibility (%) 22.46 584.00 29.68 742.00 0.08 FVC before bronchodilator 27.29 709.50 24.66 616.50 0.53 FVC after bronchodilator 26.08 678.00 25.92 648.00 0.97 bronchodilator 29.25 760.50 22.62 565.00 0.11 % Predicted FVC after bronchodilator 28.10 730.50 23.82 595.50 0.30 % Predicted FEV-1 after % Predicted FVC before Fig.1. The graph of FEV-1 (pre and post bronchodilator) comparison between budesonide and placebo groups at the end of the study 8 4.0 3.5 49 49 3.5 3.0 3.0 2.5 2.5 2.0 2.0 1.5 FEVPOS FEVPRE 1.5 1.0 .5 N= 26 25 budesonide kontr ol 1.0 .5 N= 26 25 budesonide kontr ol KELOMPOK KELOMPOK (FEV-1 pre bronchodilator) (FEV-1 post bronchodilator) 120 140 110 120 100 100 90 80 80 60 70 40 PRDFEVPS PRDFEVPR Fig.2. The graph of % Pred.FEV-1(pre and post bronchodilator) comparison between budesonide and placebo groups at the end of the study 23 60 50 N= 26 25 budesonide kontr ol KELOMPOK 20 50 0 N= 26 25 budesonide kontr ol KELOMPOK (% predicted FEV-1 pre bronchodilator) bronchodilator) (% predicted FEV-1 post DISCUSSION Objective assessments of pulmonary function are necessary for the diagnosis of asthma because medical history and physical examination are not reliable means of excluding other diagnoses or of characterizing the status of lung impairment. Although physicians generally seem able to identify a lung abnormality as obstructive they have a poor ability to assess the degree of airflow obstruction or to predict whether the obstruction is reversible [6,7,8,9]. This study was undertaken to evaluate whether the Lung Function Tests(LFTs), such as FEV-1, FEV-1 Reversibility, FVC,% predicted FEV-1 and % predicted FVC (a predicted normal range, based on age, sex, height and race) in the use of Budesonide inhaled in children with asthma are different with placebo. Jonasson et al, 1998 in a long-term follow up mild-asthma study for 2 year, found that budesonide treatment produced dose-related improvement of FEV-1 and the exercise-induced fall in FEV-1. 9 (10) Shapiro et al in 2001 reported that once daily budesonide inhalation powder maintains pulmonary function in symptoms of asthmatic children previously receiving inhaled corticosteroid. (11) Vervloet et al(2001) in a long-term follow-up moderate-asthma study for 2 year, reported budesonide treatment produced dose-related improvement of FEV-1, morning PEF, and rescue bronchodilator use and proportion night without asthma. (12) In the literature the studies about LFTs, such as FEV-1, FEV-1 Reversibility, FVC and % predicted FEV-1 (in the use of Budesonide inhaled especially compared with placebo was difficult to found. Even, many studies about budesonide only evaluated the absolute value of LFTs without compared with placebo. In this study, absolutely (without compared with placebo) all parameters of LFTs in Budesonide group were improve. The result of this study demonstrate that the administration of Budesonide inhaled resulted in significant improvement after 2 years of LFTs such as FEV-1, %predicted FEV1, Reversibility, FVC, and % predictive value of FVC compared with baseline. This is consistent with the finding of several studies about the efficacy of Budesonide inhaled in infant and young children with asthma before. (10) Selroos O et al, 1995 in their study of inhaled budesonide in 105 mild-moderate asthmatic children describe that improvement of FEV-1 was influenced by duration of asthma symptom, if the patient have duration of symptom more than 1 year; there is no improvement of FEV-1. But like as this study, they also report that in the whole patient population, there was significant improvement of FEV-1 compared with baseline after 2 years study. (11) All parameters of LFTs in Placebo group improve, except % PREDICTIVE FEV-1. The administration of Placebo inhaled resulted in significant improvement after 2 years in FEV-1, Reversibility, FVC, and % predictive value of FVC compared with baseline. Only % predictive FEV-1 was not different. Nevertheless, % predictive value of FEV-1 was precisely different between Budesonide and Placebo group. Consistent with it, Table 4 shows significant different between Budesonide and placebo group in % predictive FEV-1. In asthma control, patient cannot be achieved inhaled steroid only, and they need combination with the symptomatic therapy, elimination diet or immunotherapy. Therefore, the results of absolute of LFTs were increase significantly compared with baseline although only given placebo. All parameters of LFTs in Budesonide group in this study did not significant different compared with Placebo group, except % Predictive FEV-1 This study found that there were no different in the value of FEV-1, FVC, and FEV-1 reversibility between Budesonide and placebo group after 2 years observation, but there was significant different in the value of % predicted FEV-1 in favor of Budesonide group in the end of investigation. Theoretically, the disadvantages of FEV-1 if used for measure Lung function are (1) does not reflect disease progression well. (2) Results can be highly variable. (3) does not add any useful information on a longitudinal basis (4) as an absolute value, the result of FEV-1 assessment must be controlled with the variable of age, sex, and height. These explanation clarify that FEV-1 cannot be used precisely to assess the degree of inflammatory airway obstruction and providing accurate information for budesonide medication adjustment, cause of some disadvantages of FEV-1 above and influence of the children growth factor on lung function. (6,7,8,9) FVC in this case clarify likewise. The disadvantages of FVC are (1) may not be a sensitive early indicator; may have a 1 to 3 year lag compared with maximal expiratory pressure (MEP). (2) patients with airway obstruction may produce low and variable reading. Asthmatics can have FVC greater than normal, normal, or less than normal in attack condition. Because of that, neither FVC nor % predictive value of FVC cannot be used in assessing he degree of inflammatory airway obstruction in children. (6,7,8,9) 10 In this study, % Predictive FEV-1 in placebo group did not improve in 2 years, in budesonide group compared with placebo group improved. Maybe % Predictive FEV-1 is the most representative value to measure improvement of lung function, because FEV-1 evaluated by comparison of the patient's results with reference values based on age, height, sex, and race. (6,7,8,9) The used% Predictive FEV-1 in this study based on published equations, after matched with age, height, sex and race.(9). An advantage of % Predictive FEV-1 as marker of asthma severity is it objectivity and reproducibility.(7,8) It is frequently acquired in clinical trials, and the efficacy of new therapies is often expressed in term of impact on FEV-1. National Asthma Education and Prevention Program (NAEPP) endorsed FEV-1 as an important means for grading asthma severity,(2) However, this statement still need to evaluation especially in children, because this study confirmed that the most precise of LFTs to evaluate asthma outcome is % predictive FEV-1 and other study of risk asthma attack by Fuhlbrigge et al, 2001 in retrospective cohort of 13,832 children also found the strong association between % predictive FEV-1 and risk of asthma attack during the subsequent year. (14) Although asthma is typically associated with an obstructive impairment that is reversible, neither absolute of FEV-1 nor any other absolute parameter measure is adequate to diagnose asthma. Many factors of the children growth are associated with the LFTs. Many previous studies usually stressed to compare absolute value of two different time of observation or LFTs associate dose of drug without compare it with placebo group. The most common parameter of LFTs used previously is FEV-1. CONCLUSION Significant improvement of the LFTs (% predictive FEV-1) was seen after the use of Budesonide inhaler in asthmatic children. REFFERENCE 1. US Department of Health and Human Services Centers for Disease Control and Prevention. Morbidity and Mortality: 1996 chart book on cardiovascular, lung and blood disease. Bethesda (MD): The National institutes of Health, National Heart, Lung and Blood Institute; May 1996. 2. National Asthma Education Program. Expert panel report: guidelines for the diagnosis and management of asthma. Washington (DC): US Department of Health and Human Services, August 1991. Publication no 91-3042. 3. National Asthma Education Program. Expert panel report 2: guidelines for the diagnosis and management of asthma. Bethesda (MD): The National institutes of Health, National Heart, Lung and Blood Institute; April 1997. NIH Publication no 97-4051 4. Warner JO, Goetz M, Landau LI et al. Management of asthma: a consensus statement. Arch Dis Child 1989; 64 : 1065-79. 5. Toogoog JH,. Side effects of inhaled corticosteroids. J Allergy Clin Immunol; 102: 705-13. 6. Bye MR; Kerstein D; Barsh E. The importance of spirometry in the assessment of childhood asthma. Am J Dis Child 1992;146(8):977-8 7. Enright PL, Lebowitz MD, Cokroft DW. Physiologic measure: LFTs. Asthma outcomes. Am J Respir Crit care Med 1994;149 : S9-20 8. Enrich PL, Johnson LR, Connet JE, Voelker H, Buist AS. Spirometry in the lung health study. 1. Methods and quality control. Am Rev Respir Dis 1991; 143: 1215-21 11 9. Wang X, Dockery D, Wypij D, Fay M, Ferris B. Pulmonary function between 6 an 18 years of age. Pedtr Pulmonol 1993; 15 : 75-88. 10. Jonasson G, Carlsen KH. Mowinkel P. Asthma drug adherence in long term clinical trial. Arch Dis Child 2000; 83(4):330-3 Li JT, O'Connell EJ.Clinical evaluation of asthma.Ann Allergy Asthma Immunol 1996 ;76(1):1-13 11. Shapiro GG, Mendelson LM, Pearlman DS. Once daily budesonide inhalation powder maintains pulmonary function in symptoms of asmatic children previously receiving inhaled corticosteroid. Ann Allergy Asthma Immunol 2001; 86: 633-40 12. Vervloet D, Fontaine T, Bernabeu L, Gailiot P, Ostinelli J. Comparison 0f 800 ug once 400ug twice daily inhaled budesonide in patient with moderate ashtma. Eur Resp J 2001; 18(supp 33): 49s.Bousley HA. Effect of inhaled corticosteroids on the consequences of asthma. J Allergy Clin Immunol 1998; 102: S5-S16. 13. Selroos O, Pietinalho A, Lofroos AB et al. Effect of early vs late inttervention with inhaled corticosteroid in asthma. Chest 1995; 108: 1228-34 14. Fuhbrigge AL, Kitch BT, Paltiel AD, etal. FEV is associated with risk of asthma attacks in pediatric population. J Allergy Clint Immunol 2001;107:61-7 .