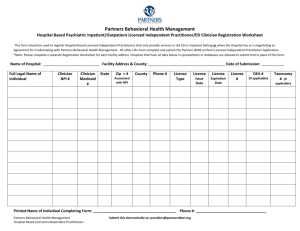
Consumer's Legal Name
advertisement

Date of Service: Cost Center/Program: Direct: Clinician’s Name & License: Total: Code: Client Identifier: Consumer’s Name: Date of Birth: Guardian’s Name: Gender: Guardian’s Phone: Address: City: Ethnicity: Preferred Language: Is interpreter needed? Travel: Yes No Zip: Phone Number: Provider speaks preferred language: Yes No Consumer accepts offer of interpretive services: Yes No Youth Link: Yes No Probation: Yes No Legal Issues/Legal Status: Education(Highest Grade Completed): Current School: IEP Suspended Expelled Veteran Employment Status: CalWorks Provider Preference (gender, location, culture, etc.): Advance Directive Information Offered (Adults Only) Medi-Cal Handbook Provided DESCRIBE HOW YOU WELCOMED THE CONSUMER INTO SERVICE: WHAT IS THE MOST IMPORTANT THING WE CAN DO TO SUPPORT YOU AND YOUR FAMILY TODAY? (in his/her own words): DESCRIBE A TIME WHEN YOU AND YOUR FAMILY WERE DOING WELL(in his/her own words): WHAT DO YOU NEED TO LIVE A HAPPY LIFE? (in his/her own words): ISSUES/AREAS OF FOCUS: (in his/her own words) ARE THERE CO-OCCURRING ISSUES: Stage of Change: 1. <select one from below> 2. <select one from below> 3. <select one from below> Clinician’s Signature / License Clinician’s Name & License Printed CLINICAL MENTAL HEALTH ASSESSMENT PAGE 1 OF 5 FRESNO COUNTY MENTAL HEALTH PLAN Yes No Date Consumer’s Name: Client Identifier: MRTF eform rev 4-12-2010 WHAT STRENGTHS AND RESOURCES DO YOU AND YOUR FAMILY HAVE IN THE CURRENT SITUATION? SPIRITUAL AND CULTURAL PRACTICES: FAMILY HISTORY: (If “yes” to any of the following, please explain in description section.) No significant information. ETOH abuse/dependence Suicide attempt Domestic violence Divorce Drug abuse/dependence Mood disorder Emotional abuse Physical/Sexual abuse Life threatening disease Death Other: Description of Family History: DESCRIPTION OF CONSUMER/FAMILY RELATIONSHIPS: Bio Mother Step Parent Foster Parent Bio Father Siblings Significant Other Accepting/Supportive: Avoidant or Infrequent Contact: Hostile/Absent: Living Arrangement: Number of dependent children (if consumer is an adult): Number of dependent adults: Description of family relationships and living situation: DEVELOPMENTAL HISTORY: (Include prenatal, perinatal, milestones, drug exposure, abuse, premature birth history, ect.) Describe: No information available. Explain: SUBSTANCE USE (consumer and/or family): Caffeine Use/abuse issues: Yes No Abuse Substance abuse in family: Yes No Describe (age of onset, drug of choice, last use, periods of sobriety): Clinician’s Signature / License Clinician’s Name & License Printed CLINICAL MENTAL HEALTH ASSESSMENT PAGE 2 OF 5 FRESNO COUNTY MENTAL HEALTH PLAN Tobacco Alcohol Illegal Drugs Dependence Recovery Denies Rx Drugs Date Consumer’s Name: Client Identifier: MRTF eform rev 4-12-2010 TREATMENT HISTORY (Please check all that apply): None Self-Help Group Support Inpatient Substance TX Psychiatric Hospitalization Outpatient Substance TX Other: Psychotropic Medication Management Outpatient Psychotherapy Describe: CURRENT PSYCHIATRIC & GENERAL HEALTH MEDICATIONS Name of Medication Current Dosage/Frequency Clinician’s Signature / License Clinician’s Name & License Printed CLINICAL MENTAL HEALTH ASSESSMENT PAGE 3 OF 5 FRESNO COUNTY MENTAL HEALTH PLAN None Prescribing MD Start Date Date Consumer’s Name: Client Identifier: MRTF eform rev 4-12-2010 Please use the following scale to rate the individual’s current problem severity for each domain & record duration (optional), in months or years. Check all adjectives that apply. For ages 0-36 months replace with IFMH ADDENDUM. Use substance use/abuse addendums as needed. 0 No Problem 1 Less than Slight AFFECT __ 2 Slight Problem 3 Slight to Moderate 4 Moderate Problem __ ANXIETY __ Appropriate Normal Range Other Labile Constricted DEPRESSION __ 5 Moderate to Severe Expansive Blunted __ 6 Severe Problem 7 Severe to Extreme 8 Extreme Problem __ Calm Phobic Obsessions Other: Anxious/Tense Worried/Fearful Compulsions THOUGHT PROCESS Guilt Panic Anti-anxiety meds. Anti-psychotic Rx Appropriate Sad/Depressed Irritable Hopeless Withdrawn Grief Sleep Problems Lacks Energy/Interest Appetite Disturbance Intact Illogical Loose Associations Oriented Delusional Ruminative Circumstantial Paranoid Disoriented Angry Other: Guilt Anti-Depressants Dissociative State Other: Tangential Hallucinations Disorganized HYPERACTIVITY__ Relaxed Sleep Deficit Pressured Speech ADHD Meds Other: _ COGNITIVE PROCESS Inattentive Manic Overactive/Hyperactive Emotional Numbness History of Abuse: Emotional Sexual Physical Witnessing/ being victim of crime, severe accident, or natural disaster Other: RELATIONSHIPS_ _ Adequate Social Skills Supportive Relationships Marital Problems Negative Peer Influence Relatedness toward Examiner: Poor Social Skills Egocentricity Problems w/Friends Overly Shy Relationship problems at work Difficulty Establish/Maintain Relationships SCHOOL Regular Attendance Absenteeism Poor Performance Expelled/Terminated Employed Permanent Disability: Insightful Irrational MEDICAL/PHYSICAL Good Health Stress-Related Illness Somatization Rx Non-Compliance _ Acute Illness Pregnant Eating Disorder Seizures Medical Tx Non-Compliance Other Medical Condition: Impaired Judgment Concrete Thinking _ Tardiness Disruptive Dropped Out Illiterate Not Employed BEHAVIOR AT HOME _ Within cultural norms Uncommunicative Dominating Tantrums SOCIO-LEGAL__ Suspended Defies Authority Learning Disabilities Employed Part-time Seeking Employment Other: DANGER TO SELF _ Doesn’t Appear Dangerous to Self Denies Suicidal Ideation Past Attempt Serious Self-Neglect Past Ideation Recent Attempt Self-Mutilation Current Plan Self-Injury Inability to Care for Self Last Hospitalization Date: Last attempt date: Other: Clinician’s Signature / License Clinician’s Name & License Printed CLINICAL MENTAL HEALTH ASSESSMENT PAGE 4 OF 5 FRESNO COUNTY MENTAL HEALTH PLAN Chronic Illness Hypochondria Poor Nutrition CNS Disorder Other: Calm Uncooperative Belligerent Runs Away Oppositional Sexualized Other: Other: WORK Poor Attention/Concentration Developmental Disability Slow Processing Poor Memory: Other: TRAUMATIC STRESS Acute Hyper vigilance Chronic Dreams/Nightmares Detached Repression/Amnesia Avoidance Agitated Mood Swings Impulsivity Intrusive Disregards Rules Threatening Inappropriate __ Disregards Rules Lying Fire setting Initiates Fights Offense/Property Offense/Person Street Gang CPS Involvement Member Detention/Incarceration Hx: Last Incarceration Date: Stealing Pending Charges Probation/Parole Restraining Order Other: DANGER TO OTHERS Doesn’t Appear Dangerous Threatens Others Violent Temper Homicidal Ideation to Others Cruelty to Animals Assaultive Homicidal Threats Accused of Child Abuse Denies Domestically Violent Use of Weapons Homicidal Attempt Accused of Sexual Assault Other: Date Consumer’s Name: Client Identifier: MRTF eform rev 4-12-2010 CLINICAL SUMMARY/ PRESENTING MENTAL HEALTH PROBLEM: MEDICAL NECESSITY -- Check all that demonstrate medical necessity for mental health services. Significant Impairment Probability of significant deterioration No Medical Necessity NOA-A issued Probable developmental arrest CONSUMER IS IMPAIRED IN THE FOLLOWING AREAS: Living Arrangement Employment Daily Activities Social Relationships Health Describe clinical impairment in above areas : Is mental health treatment needed? Yes No Prognosis: General Medical Condition Concerns: Identify: Yes No Allergies: Identify: Good No Fair Poor Yes Primary Care Physician: Phone: DSM DIAGNOSIS (Must complete all Axes using most current version of DSM codes.) Axis I list any secondary substance use Dx on Axis I Axis II Axis III Axis IV (Psychosocial stressors including co-occurring disorders in the family and homelessness) Axis V Current Clinician’s Signature / License Clinician’s Name & License Printed CLINICAL MENTAL HEALTH ASSESSMENT PAGE 5 OF 5 FRESNO COUNTY MENTAL HEALTH PLAN Past Year Date Consumer’s Name: Client Identifier: MRTF eform rev 4-12-2010