Strategies for wound pain management
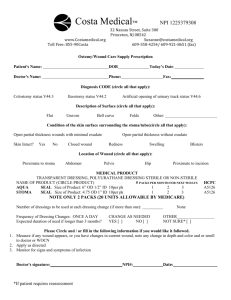
advertisement

Strategies for wound pain management This excerpt was taken from the book, Evidence-Based Pressure Ulcer Prevention: A Study Guide for Nurses Nurses must meet the challenge of assessing and managing their patients' pain effectively as it is important for both the prevention and healing of pressure ulcers. The key to managing wound pain is to use a validated pain scale to regularly assess those patients with open wounds and pressure ulcers for pain. If the pain is frequent or constant, consider giving a scheduled pain medication. If the patient has an order for “as needed or as required” analgesics, give them at the earliest sign of pain; do not wait for the pain to get out of control. Remember to evaluate the patient’s response to pain-relieving medication. For optimal pain relief during dressing change, consider using the following strategies: Offer analgesics when pain is anticipated. Premedicate the patient at least one hour before dressing change or debridement. Evaluate the patient’s response by assessing the effectiveness of the medication during the procedure. If the procedure is exceedingly painful, a stronger premedication may be needed. Another option is to use a topical product, such as one containing lidocaine. Such products are highly effective but take approximately two hours to work. Dispel myths and teach the patient facts about pain and pain management. For example, the old adage “no pain, no gain” is a myth. Teach the patient that in wound healing, less pain means more gain. Another common myth is that responsiveness to pain decreases with age. Many nurses believe that pain perception decreases, and elderly patients increase their complaints. But sensory processing of painful stimuli does not change with age. Older adults experience many painful chronic diseases. Indeed, they may experience more pain than younger adults. Involve the patient in decision-making, and give him or her a sense of personal control over the pain. Provide antianxiety medications, if requested by the patient. During the dressing change, monitor the patient’s body language and nonverbal cues carefully for signs of pain. Avoid unnecessary manipulation of the wound. Protect it from sources of irritation, including air flow from a fan or window. Warm the cleansing solution prior to cleansing the wound, if possible. Use only normal saline or pH-neutral wound cleansers. Be gentle when cleaning the wound. Allow the patient to stop and rest during a painful procedure, such as a dressing change. Agree on a signal in advance. Match the dressing and treatment product to the wound. Use dressings that are nonadherent and reduce pain. Avoid woven cotton gauze, which is highly irritating to sensitive skin. Select wound products that maintain a moist environment in the wound bed. Do not allow the wound to become desiccated. Select treatments that can remain in place for a prolonged period of time. Avoid frequent dressing changes by using advanced products, if possible. Consider contact-layer dressings that remain in place. Doing so decreases the need to manipulate the tender wound bed, which causes increased pain. Use compression bandages, if needed, to reduce edema and relieve pain. Apply barrier products to protect the wound margins, thus preventing maceration and further breakdown. This is particularly important if chemical debriding agents are being used. Allow the patient to remove his or her own dressing, if desired. Remove tape and dressings carefully and gently. If the dressing or tape sticks to the skin during dressing removal, apply normal saline, and then wait a few minutes. Minimize the use of tape if the patient’s skin is sensitive, or if he or she is at risk for skin tears. Instead, use bandages, Montgomery straps, Coban wrap, etc., to cover the dressings. Follow manufacturers’ instructions for removal of hydrocolloids and transparent films. Splint or immobilize the wound during movement and treatment, if possible. Teach patients to use relaxation and distraction techniques, such as guided imagery; slow, deep breathing; biofeedback; and listening to comforting music through a headset. Pain management tip Provide pain management by eliminating mechanical sources of pain (e.g., choosing a dressing that can be changed once daily versus multiple changes during the day, or adjusting the support surface/repositioning plan). Collaborate with the patient’s physician regarding analgesia and, if pain is severe, talk to the physician about a pain management service consultation, if available. Remember: New onset pain may be a sign of wound infection. Editor’s note: This excerpt was taken from the book, Evidence-Based Pressure Ulcer Prevention: A Study Guide for Nurses. To find out more about the book and to order a copy visit http://www.hcmarketplace.com/prod-6133.html.