Immobility, Skin Integrity, and Wound care

Immobility, Skin Integrity, and Wound Care
Dr. Belal Hijji, RN, PhD
March 31, April 1 & 7, 2012
Learning Outcomes
At the end of this lecture, students will be able to:
• Define relevant terms
• Discuss the effects of immobility on body systems
• List classifications of pressure ulcers
• Discuss factors contributing to pressure ulcer formation
• Describe the three major classifications of dressings and rules of wound care
• Discuss the medical and nursing management of wound care
2
Immobility- Definition of Terms
• Mobility: Is the person’s ability to move around freely in his/ her environment.
• Immobility: Inability to move around freely. Whether immobility causes any problems often depends on the duration of inactivity, the client’s health status, and his/ her sensory awareness
• Bed rest: Is an intervention in which the client is restricted to bed for therapeutic reasons.
3
Effects of Immobility
• Musculoskeletal system
– Disuse osteoporosis: Without the stress of weight-bearing activity, the bones deminerlise. Calcium decreases, the bones become spongy, may gradually deform and fracture easily.
– Disuse atrophy: Unused muscles atrophy (decrease in size) losing most of their strength and normal function.
– Contractures: When the muscle fibers are not able to shorten or lengthen, a contracture (permanent shortening of the muscle) forms, limiting joint mobility (See figure1).
– Stiffness and arthralgia: Without movement, the connective tissue at a joint becomes ankylosed
(permanently immobile). As bones dimineralise, excess calcium may move to joints, contributing to stiffness and pain,
Figure 1: Contractures
4
• Cardiovascular system
– Diminished cardiac reserve: Decreased mobility can lead to increase in heart rate. Rapid heart rate reduces diastolic pressure, coronary blood flow, and the capacity of the heart to respond to any metabolic demands above the basal level. Because of this diminished cardiac reserve, the immobilised person may experience tachycardia with minimal exertion.
– Increased use of Valsalva maneuver: This maneuver refers to holding the breath and straining against a closed glottis. For example, a client tends to hold breath when trying to move up in bed. This builds up sufficient pressure on the large veins in the thorax to interfere with blood flow to the heart and coronary arteries. During exhalation, the glottis again opens, pressure is suddenly released, and a surge of blood flows to the heart.
Tachycardia and cardiac arrhythmias can result in clients with cardiac disease.
5
– Orthostatic hypotension: Under normal condition, vasoconstriction prevents pooling of the blood in legs and maintains central blood pressure. During prolonged immobility, this reflex becomes dormant. When an immobile person tries to sit or stand, this reconstricting mechanism fails to function properly. The blood pools in the lower extremities, and central blood pressure drops. Cerebral perfusion is seriously compromised, and the person feels dizzy and may faint [ ىمغي
هيلع]
– Thrombus formation: Three factors collectively predispose a client to the formation of thrombophlebitis (a clot that is loosely attached to an inflamed vein wall): impaired venous return to heart, hypercoagulability of blood, and injury to a vessel wall. A thrombus (Figure
2 ) is dangerous if it breaks loose from the vein
wall to enter the general circulation an embouls (an object that has moved from its place of origin, causing obstruction to circulation elsewhere).
6
Figure 2: Blood clot
7
• Respiratory system
– Decreased respiratory movement: In a recumbent, immobile client, the body presses against the rigid bed and curtails chest movement. The abdominal organs push against the diaphragm, restricting lung movement and making it difficult to expand the lungs fully. As a result, shallow respirations are produced and vital capacity (the maximum amount of air that can be exhaled after maximal inhalation) is reduced.
– Pooling of respiratory secretions: Immobility allows secretions to pool by gravity, interfering with normal diffusion of oxygen and carbon dioxide in the alveoli. The ability to cough up secretions may be hindered by loss of respiratory muscle tone, dehydration, or sedatives that depress cough reflex. Poor oxygenation and retention of carbon dioxide in the blood can lead a potentially fatal respiratory acidosis.
– Hypostatic pneumonia: pooled secretions are an excellent media for bacterial growth leading to pneumonia. This condition can severely impair oxygen-carbon dioxide exchange and may be lethal.
8
• Urinary system
– Urinary stasis: In immobile person, gravity impedes the emptying of urine from the kidneys and the bladder. To urinate, a person in supine position must push upward against gravity. The renal pelvis may fill with urine before it is pushed into the ureters. Empting is not complete and urinary stasis (urine flow is stopped or slowed down) occurs a few days of bed rest.
Therefore, bladder emptying is further compromised.
– Renal stones: With immobility, there is excessive amounts of calcium in the urine. Calcium salts precipitate out as crystals to form renal calculi.
• Integumentary system
– Skin breakdown: Immobility impedes circulation and diminishes the supply of nutrients to specific area. This results in skin breakdown and formation of pressure ulcer.
• GIT system
– Constipation: Occurs due to decreased peristalsis and colon motility. The overall skeletal muscle weakness affects the abdominal and perineal muscles used in defecation.
9
Skin
• Has three layers (Fig.
) :
– Epidermis: the outer visible layer, contains keratin, an extremely tough, protective protein substance that can cause tissue to become hard or horny.
– Dermis: The deeper dermis is made up of proteins and mucopolysaccharides, thick, gelatinous material that provides a supporting matrix for nerve tissue, blood vessels, sweat and sebum glands, and hair follicles.
– Subcutaneous tissue: This layer is made up of fatty connective tissue. Together, the layers of the skin protect underlying structures from physical trauma and ultraviolet (UV) radiation.
The skin is essential to maintaining body temperature, fluid balance, and sensation. It is involved in absorption and excretion, immunity, and the synthesis of vitamin D from the sun.
10
Figure 3: Structures of the skin
11
Skin Integrity and Wound Care – Pressure Ulcer
Classification of pressure ulcers
Stage I is the most superficial, indicated by non blanchable redness that does not subside after pressure is relieved. This stage is visually similar to reactive hyperemia seen in skin after prolonged application of pressure.
Stage II is damage to the epidermis extending into, but no deeper than, the dermis. In this stage, the ulcer may be referred to as a blister or abrasion.
Stage III involves the full thickness of the skin and may extend into the subcutaneous tissue layer. This layer has a relatively poor blood supply and can be difficult to heal.
Stage IV (Figure
) pressure ulcer: Stage IV is the deepest, extending into the muscle, tendon or even bone.
Unstageable pressure ulcers are covered with dead cells, or eschar and wound exudate, so the depth cannot be determined.
12
Figure 4: Stage IV pressure ulcer
13
If untreated, a pressure sore can progress from a small irritated but unbroken skin patch to a potentially life-threatening wound involving extensive tissue death and infection. Treatment of the serious decubitus ulcer may include debriding
(excising) the dead tissue and administering systemic antibiotics.
14
Contributing Factors to Pressure Ulcer Formation
In addition to pressure, other factors can increase the risk for developing pressure ulcers. These are:
– Shear: Is the force exerted against the skin while skin remains stationary and the bony structures move. For example, when elevating the HoB, gravity causes the bony skeleton to pull toward the foot of bed, while the skin remains against the sheets. This process impedes circulation to deep tissues.
– Friction: Is an injury to the skin that has the appearance of an
abrasion (Figure 5 a & b). Elbows and heels are at risk for
friction because abrasion of these surfaces can occur when they are rubbed against sheets during repositioning.
– Moisture: Moisture on the skin increase the risk of ulcer formation. Moisture reduces the skin’s resistance to pressure or shear.
15
– Nutrition: Poor nutrition can cause soft tissue to become susceptible to breakdown. Low protein levels cause edema, which contributes to problems with oxygen and nutrients transport. Edema increases the affected tissue risk for pressure ulcer formation. Blood supply to edematous areas is decreased, and waste products remain.
– Infection: Fever results in sweating and increased moisture, which predispose to skin breakdown.
– Age: Older adults are at higher risk for development of pressure ulcer because of loss of dermal thickness and an increase in the risk of skin tear.
16
on elbow and lower arm. The elbow wound will produce a permanent scar.
Figure 5b:Abrasion on the palm of a right hand, shortly after falling.
17
What is a Scar?
• A scar (Figure 6) is an area of fibrous [يفيل] tissue (fibrosis) that replaces normal skin after injury. A scar results from the biological process of wound repair in the skin and other tissues of the body. Thus, scarring is a natural part of the healing process. With the exception of very minor lesions, every wound (e.g. after accident, disease, or surgery) results in some degree of scarring.
Figure 6: A minor scar from a cut to the forearm, approx. one year since the wound.
18
Wound Care
• There are three major classifications of dressings for skin conditions:
– Wet
– Moisture-retentive
– Occlusive
• These classifications will be discussed after presenting dressings and rules of wound care
19
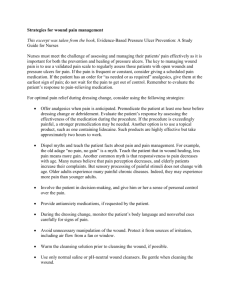
Dressings and Rules of Wound Care
•
Rule 1: Categorization . The nurse should learn about dressings by generic category because hundreds of choices are now available. The nurse should also develop a systematic approach to product selection, and should be familiar with indications, contraindications, and side effects.
• Rule 2: Selection. The nurse should select the safest and most effective, user-friendly, and cost-effective dressing possible.
Nurses should be prepared to give the physician feedback about the dressing’s effect on the wound and ease of use for the patient.
•
Rule 3: Change . The nurse changes dressings based on patient, wound, and dressing assessments, not on standardized routines, such as three or four times each day.
20
Dressings and Rules of Wound Care
•
Rule 4: Evolution . As the wound healing process progresses, the dressing protocol is altered to optimize healing. The nurse and patient have access to a wide variety of products and knowledge about their use. The nurse teaches the patient about wound care and ensures that the family has access to appropriate dressing choices.
•
Rule 5: Practice . Practice with dressing material is required for the nurse to learn the proper way of performing a particular dressing. Refining the skills of applying appropriate dressings correctly and learning about new dressing products are essential nursing responsibilities. Dressing changes should not be delegated to assistive personnel.
21
Classifications of Dressings
Wet Dressings
• Wet dressings (ie, wet compresses applied to the skin) are sterile or nonsterile, depending on the skin disorder. They are used to reduce inflammation by producing constriction of the blood vessels; to clean the skin of exudates [cellular waste product]and pus; to maintain drainage of infected areas; and to promote healing by facilitating the free movement of epidermal cells across the involved skin so that new granulation tissue forms.
• Before dressings, the nurse washes hands and puts on sterile or clean gloves. The open dressing requires frequent changes because evaporation is rapid. The closed dressing is changed less frequently, but there is always a danger that the closed dressing may cause actual maceration [soften by soaking] of the underlying skin. The dressing remains in place until it dries. It is then removed without soaking so that exudate, or pus from the wound adhere to the dressing and are removed with it.
22
Classifications of Dressings
Moisture-Retentive Dressings
• Moisture-retentive dressings have similar functions as those of wet dressing but are more efficient at removing exudate; some have reservoirs that can hold excessive exudate.
• The main advantages of moisture-retentive dressings over wet compresses are reduced pain, fewer infections, less scar tissue, gentle autolytic débridement [A process that uses the body’s own digestive enzymes to break down necrotic tissue], and decreased frequency of dressing changes. Several available products contain enzymatic débriding agents; examples include Accu Zyme, collagenase, (Santyl), Granulex, and
Zymase. Application of these products speeds the rate at which necrotic tissue is removed.
• Depending on the product used and the type of skin problem, most moisture-retentive dressings may remain in place from
12 to 24 hours; some can remain in place as long as a week.
23
Classifications of Dressings
Occlusive Dressings
• Occlusive dressings may be commercially produced inexpensively from sterile or nonsterile gauze squares.
• Occlusive dressings cover topical medication that is applied to a abnormal skin lesion. The area is kept airtight by using plastic film (eg, plastic wrap), which is thin and readily adapts to all sizes, body shapes, and skin surfaces. Generally, plastic wrap should be used no more than 12 hours each day.
24
Medical Management
Therapeutic Baths (Balneotherapy) and Medications
• Baths, known as balneotherapy, are useful when large areas of skin are affected. The baths remove crusts, scales, and old medications and relieve the inflammation and itching that accompany acute dermatoses [skin diseases]. The water temperature should be comfortable, and the bath should not exceed 20 to 30 minutes because of the tendency of baths and soaks to produce skin maceration.
• Because skin is easily accessible, topical medications are often used. High concentrations of some medications can be applied directly to the affected site with little systemic absorption and therefore with few systemic side effects. Because topical preparations may induce allergic contact dermatitis in sensitive patients, any untoward response should be reported immediately and the medication discontinued.
Continued…..
25
• Lotions, creams, ointments, and powders are frequently used to treat skin lesions. In general, moisture-retentive dressings, with or without medication, are used in the acute stage; lotions and creams are reserved for the subacute stage; and ointments are used when inflammation has become chronic and the skin is dry with scaling.
• With all types of topical medication, the patient is taught to apply the medication gently but thoroughly and, when necessary, to cover the medication with a dressing to protect clothing.
• Intralesional Therapy. Intralesional therapy consists of injecting a sterile medication (usually a corticosteroid) into or just below a lesion. Skin lesions treated with intralesional therapy include psoriasis, keloids, and acne vulgaris.
• Systemic Medications. These include corticosteroids for shortterm therapy for contact dermatitis or for long-term treatment of a chronic dermatosis, such as pemphigus vulgaris. Other frequently used systemic medications include antibiotics, antifungals, antihistamines, and analgesics.
26
Acne vulgaris
Psoriasis
Pemphigus vulgaris is an autoimmine disorder, where the body's immune system attacks some of the proteins in the skin. This picture shows a close-up of the blistering on the back. Most of the blisters have broken, which is common since these blisters are fragile .
Keloid
27
Nursing Management
• Management begins with a health history, direct observation, and a complete physical examination.
• Because of its visibility, a skin condition is usually difficult to conceal from others and may cause the patient some emotional distress.
• The major goals for the patient may include maintenance of skin integrity, relief of discomfort, promotion of restful sleep, self-acceptance, knowledge about skin care, and avoidance of complications.
• Nursing management for patients who must perform self-care focuses mainly on teaching them how to wash the affected area and pat it dry, apply medication to the lesion while the skin is moist, cover the area with plastic if recommended, and cover it with an elastic bandage, dressing, or paper tape to seal the edges.
• Dressings that contain or cover a topical corticosteroid should be removed for 12 of every 24 hours to prevent skin thinning
(ie, atrophy), striae, and telangiectasia (ie, small, red lesions caused by dilation of blood vessels).
28