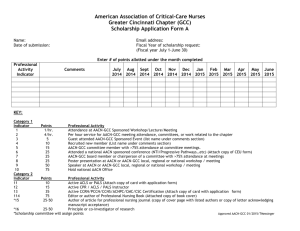
Membership Committee Report
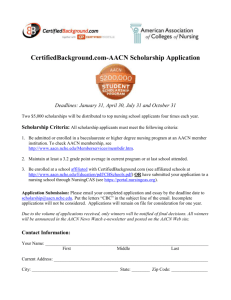
advertisement

COMMITTEE TASK FORCE PROJECT REPORTS March 16-19, 2013 Spring Annual Meeting Finance Committee March 2013 The AACN Finance Committee meets on a quarterly basis to review the financial statements and oversee the Association’s financial commitments. The January 2013 financial statements are attached and have been reviewed by both the Finance Committee and the Board of Directors. It should be noted that as of January 31st, AACN had received 84% of budgeted revenue for the current fiscal year. In addition, expenses to date were on target at 51% of the total budget. Special initiatives arise throughout the year due to the work of the association and implementation of the strategic plan. Budgets specific to each initiative are considered for approval by both the Finance Committee and the Board of Directors. Current initiatives include the CNL Steering Committee, the CNL Review Course, the Academic Practice Partnership Steering Committee, and the Faculty Policy Intensive. Board-approved expenditures total approximately $229,000 for this fiscal year. However, as in years past, we anticipate that grant offsets (salary, fringe benefits, rent, and overhead) will cover these additional expenses. As set forth in the Financial Management Guidelines, the Finance Committee is also charged with monitoring the Association’s investment portfolio with the assistance of our investment manager at RBC Wealth Management. The committee is pleased to report investment earnings of approximately $144,000. One of the committee’s primary responsibilities is to present a balanced operating budget to the Board each year. The budget is tied to the strategic goals and objectives of the Association and is built upon projected revenues and expenses, exclusive of any grant funding. Highlights of the FY 2014 budget will be presented at the business meeting. Committee members are: Margaret Callahan, Chair, Marquette University Rita Frantz, University of Iowa Barbara Landrum, Henderson State University Anne McNamara, Grand Canyon University Elias Provencio-Vasquez, University of Texas – El Paso Heather Shelford, Staff Liaison Membership Committee Report Spring 2013 The American Association of Colleges of Nursing experienced a growth of 36 new member schools this fiscal year, the largest annual growth in AACN history. This is attributed to the prospect pool enlarging (growth of new RN-BSN programs), creative acquisition strategies and the conversion of prospective members attending our annual meetings. AACN has 726 institutional members and currently represents 83% of the institutions offering baccalaureate and graduate nursing programs known to be eligible for membership in the Association. The Association also has 82 individual members. Of these, 40 are emeritus members, 36 are honorary members, and 6 are honorary associate members. The following 36 schools have been granted membership with AACN in Fiscal Year 2013: Anderson University (South Carolina) Anna Maria College (Massachusetts) Austin Peay State University (Tennessee) Bluefield College (Virginia) Chamberlain College of Nursing-Addison, IL Chamberlain College of Nursing-Atlanta, GA Chamberlain College of Nursing-Cleveland, OH Chamberlain College of Nursing-Houston, TX Chamberlain College of Nursing-Indianapolis, IN Chamberlain College of Nursing-Jacksonville, FL Chamberlain College of Nursing-Phoenix, AZ Concordia University- Portland (Oregon) Dakota Wesleyan University (South Dakota) Everest College (Utah) Freed-Hardeman University (Tennessee) Granite State College (New Hampshire) Hood College (Maryland) Lindenwood University (Missouri) Lipscomb University (Tennessee) Medgar Evers College of CUNY (New York) Methodist University (North Carolina) Miami Dade College (Florida) Mount Olive College (North Carolina) National University College (Puerto Rico) Rocky Mountain University of Health Professions (Utah) Roseman University of Health Sciences (Utah) Saint Martin's University (Washington) Santa Fe College (Florida) Sojourner-Douglas College (Maryland) Southern New Hampshire University Sullivan University (Kentucky) Texas Tech University HSC-El Paso Universidad Central de Bayamon (Puerto Rico) University of Hawaii at Hilo Vanguard University of Southern California Wesleyan College (Georgia) The following five deans are observing as prospective members: Faith Garrett, Gordon State University (Georgia) Natalie Burkhalter, Texas A&M International University Jujuan English, University of Arkansas at Pine Bluff Ellen Ceppetelli, Castleton State College (Vermont) Christy Torkidson, Unitek College (California) The following two Nursing Schools closed this year: Montreat College (North Carolina) Mountain State University (West Virginia) NEW DEAN MENTORING PROGRAM UPDATE AACN's New Dean Mentoring Program (NDMP) matches an experienced AACN-member dean with a member who is new to the dean's role for a period of mutual development. AACN members volunteer to serve as mentors in the program. New deans are matched to mentors based on their responses to the New Dean Questionnaire. Since the 2012 Spring Annual Meeting, 51 new deans/directors have been paired with experienced deans. AACN continues to solicit mentor volunteers as needed throughout the year. The annual NDMP survey was distributed in October to the participants in the fall 2012 program. The survey was completed by 84 program participants. Based on feedback from the survey, AACN staff is developing a Webinar to encourage positive mentoring experiences. The next annual survey will be emailed to our new participants in April 2013. The Board of Directors and Membership Committee will welcome new members, new deans and prospective members on Saturday, March 16, 2013 at 5:10 p.m. Membership Committee Members: Eleanor Howell, Chair, Creighton University Debra Jenks, Milwaukee School of Engineering School of Nursing Judith Lewis, D’Youville College Ann Schiele, Mount Carmel College of Nursing Jan Strom, Northern Illinois University Rosemary Smith, New Dean Mentoring Program Chair, University of Wisconsin-Oshkosh LEADERSHIP NETWORKS UPDATE Continuing on with a four year trend, the Leadership Network Membership grew 9% this fiscal year for a total of 1361 network members. For FY2014, we will focus on strengthening the current membership base. AACN is exploring new acquisition markets and working on a new special appeal to boost membership numbers. Additional revenue was produced during the year by the Leadership Network conferences. The conferences represented more than $130,000 in gross income, of which $10,000 came from sponsorships. Organizational Leadership Network (OLN) The Organizational Leadership Network currently has 316 members, representing an 8% growth over FY2012. The meeting, Academic Leaders as Change Agents: Igniting Positive Change and Innovation through Leveraging Strengths in Academia took place October 27, 2012 at The JW Marriott, Washington DC. The OLN program sessions are designed to enhance the development of academic leaders, especially those who serve as associate/assistant deans and deans who are new to the deanship. This year’s theme emphasized the important subject of Appreciative Inquiry, an organizational 4 development method which focuses on increasing what an organization does well rather than on eliminating what it does badly. Attendee group work focused on studying an individual’s leadership strengths and figuring out ways to deploy those strengths. The OLN program was evaluated at 4.76 overall and the small group discussions were evaluated at 4.47 on a 5-point scale. Small group discussions focusing on Leadership Qualities were held in the evening on October 26, 2012, at The JW Marriott, Washington DC. The small group discussions provide an additional venue to create/maintain networking opportunities for academic leader and the guided discussions help to set the stage for the OLN conference on the following morning. An informal dinner allowed participants to continue with their dialogue and seek collegial advice. Organizational Leadership Network Steering Committee Members: Chair: Judy Didion, Lourdes University College of Nursing; Chair-elect: Mary Kunes-Connell, Creighton University; Secretary: Teresa Wehrwein, Michigan State University; Communications Chair: Ann White, University of Southern Indiana; Program Committee Co-Chair: Angela PhillipsLowe, Mount Carmel College of Nursing; Program Committee Co-Chair: Rita D’Aoust, University of South Florida; and Past Chair: Patricia Underwood, Case Western Reserve University Instructional Leadership Network (ILN) The Instructional Leadership Network currently has 299 members, representing an 8% growth over FY2012. The conference, Strengthening Leadership Capacity to Foster Civility in Nursing Education took place, November 15, 2012 at the San Antonio Marriott Rivercenter, San Antonio, TX The annual ILN conference is designed for nursing faculty responsible for educational programs including curriculum development experts. This year’s conference addressed the challenges faculty experience in regards to incivility and bullying behavior. Our guest speaker described the ‘State of the Science’ regarding civility and incivility in nursing education and applied a variety of evidence-based strategies to promote civility in nursing education. The conference included table top discussions that reflected upon the opening presentation and discussion on proactive strategies and policies to reduce incivility; interdisciplinary education; standardized testing; integrating QSEN into the curriculum; faculty recruitment; and Social Media. The ILN program was evaluated at 4.85 overall on a 5-point scale. Instructional Leadership Network Steering Committee Members: Chair: Nancy Haugen, Samuel Merritt University; Chair-elect: Kerry Kosmoski-Goepfert, Marquette University; Secretary: Kelly J. Betts, University of Arkansas for Medical Sciences; Program Committee CoChair: Martha Scheckel, Michigan State University; Program Committee Co-Chair: Indira D. Tyler, Patty Hanks Shelton School of Nursing; Communication Co-Chair: Stephanie S. Pierce, Louisiana State University HSC; and Past Chair: Linda Daley, The Ohio State University Research Leadership Network (RLN) The Research Leadership Network currently has 191 members, representing a 25% growth over FY2012. The conference, Use of Open Access Journals for Research Dissemination, took place, January 24, 2013 at The Hotel Del Coronado, San Diego, CA. 5 The RLN program is aimed at those who have leadership roles facilitating research within their nursing programs. The goal of the program was to increase one’s knowledge regarding open access publication as it pertains to nursing scholarship/science and to maximizing the benefits of open access and minimizing limitations at the individual and institutional level. The RLN program was evaluated at 4.48 overall on a 5-point scale. Research Leadership Network Steering Committee Members: Chair: Nalini Jairath, The Catholic University of America; Chair-elect: Margaret Barton-Burke, University of Missouri-St. Louis; Secretary: Barbara St. Pierre Schneider, University of Nevada, Las Vegas; Communications Co-Chair: Alyce S. Ashcraft, Texas Tech University HSC; Communications Co-Chair: Barbara Fowler, Wright State University; Program Committee Co-Chair : Julie Zadinsky, Georgia Health Sciences University; Program Committee Co-Chair: Cindy Corbett, Washington State University; and Past Chair: Brenda Recchia Jeffers, St. John’s College Practice Leadership Network (PLN): The Practice Leadership Network currently has 119 members, representing a 15% growth over FY2012. The Faculty Practice Preconference, Policy, Business, and Faculty Practice: Links and Influences, took place, January 25, 2013 at The Hotel Del Coronado, San Diego, CA (one full day) and February 28-29, 2013, Buena Vista Palace, Orlando, FL (one afternoon and one morning). The PLN conference is designed for nursing faculty who administer faculty practice programs and those actively engaged in faculty practice. The conference topic include: National Health Care Policy: Impact and Influence on Nursing Practice; Institutional Policies: Making Faculty Practice Work; From Negatives to Positives: Business Aspects of Faculty Practice; and Links between Policy and Practice. Practice Leadership Network Steering Committee Members: Chair: Marilyn Wideman, Rush University; Chair-elect: Sandra Bellini, University of Connecticut; Secretary: Kathleen Miller, University of Massachusetts Worcester; Program Committee Chair: Susann Farberman, University of Missouri – St. Louis; Communications Chair: Paula McCauley, University of Connecticut; Past Chair: Leissa Roberts, University of Utah UPCOMING CONFERENCES: Graduate Nursing Admissions Professionals (GNAP) The Graduate Nursing Admissions Professionals Network currently has 138 members, representing a 5% growth over FY2012. The conference, Race Into the Future of Nursing, will take place on April 2-3, 2013 at The Westin Charlotte, Charlotte, NC. Graduate Nursing Advancement Professionals Steering Committee Members: Chair: Paddy Peerman, Vanderbilt University; Chair-elect: Carol Aspinwall, University of Wisconsin-Madison Secretary: Cathleen Mumper, University of San Diego; Program Committee Chair: Angela Kerner, University of Michigan; Communications Chair: Rhonda Flenoy-Younger, University of California-Los Angeles; Sponsorship Chair: Rita Croom, Union University; Past Chair: Elaine Andolina, University of Rochester 6 Nursing Advancement Professionals (NAP) The Nursing Advancement Professionals Network currently has 131 member,s representing a 9% growth over FY2012. The conference, Innovations and Impact in Nursing, will take place on April 5-6, 2013 at the Omni San Diego Hotel, San Diego, CA. Nursing Advancement Professionals Steering Committee Members: Chair: Coleen Southwell, University of Wisconsin-Madison; Chair-elect: Angie Peters, Southern Illinois University Edwardsville; Secretary: Sallie Ellinwood, Duke University; Membership Co-Chair: Dinny Trabert, University of Utah; Membership Co-Chair: Shelly Grider, Auburn University; Program Committee Co-Chair: Jenny Ward, Illinois State University; Program Committee CoChair: MaryK McGinley, University of North Carolina Greensboro; Past Chair: Kelly Gotschalk, Virginia Commonwealth University Business Officers of Nursing Schools (BONUS) The Business Officers of Nursing Schools Network currently has 168 members, representing a 9% growth over FY2012. The conference, A Sure Bet, will take place on April 17-19, 2013, at the Omni Austin Hotel Downtown, Austin, TX. The BONUS steering committee is currently testing the discussion groups on the Member Online Collaboration Community and they recently launched a BONUS Facebook page. Business Officers of Nursing Schools Steering Committee Members: Chair: Carla Ho-a, University of Colorado Denver; Chair-elect: Katharine Bonneson, University of Minnesota; Secretary: Sylvia Mason, Indiana University- Kokomo; Membership Committee Chair: Sybil Strano-Perry, University of Nevada-Las Vegas; Nominating Committee Chair: Delores Armstrong, Virginia Commonwealth University; Communications Committee Chair: Deidre Wesley, Rush University Medical Center; Planning Committee Chair: Diane Fine, Barry University; Special Projects Committee Chair: Cheryl McPherson, Oakland University; Past Chair: Lisa Vaughan, University of Mississippi Medical Center Social Media: AACN staff along with the network steering committees members created Facebook pages for BONUS and GNAP where members can find information about our upcoming meetings, list serves and membership information. Both the PLN and BONUS steering committee are evaluating the member’s capacity and interest for the use of an online collaboration community. All seven network listservs continue to offer the potential for participants to engage in a ‘virtual discussions" with experts and colleagues from around the world. 7 Program Committee Report March 2013 The Program Committee, chaired by Jean Leuner last met in person during the 2012 Fall Semiannual Meeting to plan the 2013 Spring Annual Meeting (March 16-19, 2013) around the theme Guiding Change: Technology in Nursing Higher Education. The committee will meet again on March 16 to begin planning the 2013 Fall Semiannual Meeting. AACN CONFERENCE UPDATES: EXECUTIVE DEVELOPMENT SERIES Chair: Greer Glazer, University of Cincinnati Nuts and Bolts of Leading a Nursing Academic Unit November 14-15, 2012, San Antonio Marriott Rivercenter, San Antonio, TX March 15-16, 2013, The Fairmont Washington, Washington, DC The popular Executive Development Series (EDS) is designed for new and aspiring academic leaders as well as for experienced faculty members who want to improve their leadership skills for a variety of positions within the nursing academic unit. The fall event attracted 110 attendees, an all-time record, and was evaluated extremely highly overall at 4.6 on a 5-point scale. Topics included creating a healthy work environment; advancing interprofessional education; critically examining the correct direction for the nursing academic unit; taking better care of oneself in order to be optimally productive as an academic leader; and using a valuable peer coaching technique to solve a real-world problem. The same program is offered March 15-16 prior to the Spring Annual Meeting. Subcommittee members: Catherine Alicia Georges, Lehmann College; Jean Giddens, University of New Mexico; Anne Hirsch, Seattle University; Sandie Soldwisch, Resurrection University; Karen Stefaniak, University of Kentucky; Jill Winters, Columbia College of Nursing; and Linda Zoeller, Western Michigan University BACCALAUREATE EDUCATION CONFERENCE Chair: Sharon Wilkerson, Texas A&M Health Science Center, Bryan, TX Changes and Challenges in Baccalaureate Nursing Education November 15-17, 2012, San Antonio Marriott Rivercenter, San Antonio, TX This conference offers undergraduate and pre-licensure faculty a forum to explore issues of particular interest and share ideas and successful strategies with colleagues. This year’s conference encouraged attendees to identify strategies to expect and enforce a climate of civility; determine what constitutes a professional identity in nursing, and how to instill desirable qualities in undergraduate nursing students; gain a national perspective on RN-to-BSN education; and consider the most common and pressing legal concerns for nursing faculty and strategies to prevent and respond to challenges. Almost 500 educators attended the conference, 8 near the record, and gave it an overall score of 4.51 on a 5-point scale. The Instructional Leadership Network also met during this event. Subcommittee members: Cindy Greenberg, California State University-Fullerton; Mary Hill, Howard University; Anita Hufft, Valdosta State University; Kathleen O'Connor, Missouri Western State University; Elizabeth Palmer, Indiana University of Pennsylvania; Peggy Rice, Lewis University; and Indira Tyler, Patty Hanks Shelton School of Nursing FACULTY PRACTICE PRE-CONFERENCES January 23, 2013, Hotel del Coronado, San Diego, CA February 20-21, 2013, Buena Vista Palace, Orlando, FL This pre-conference, designed for those who promote, administer, and engage in faculty practice, offered the same program prior to both the Doctoral and Master’s Education Conferences. The January (Doctoral) event attracted over 90 participants and was evaluated highly at 4.5 on a 5point scale. The February (Master’s) event was smaller with 51 attendees, and those evaluations are in progress. Working Group Members: Marilyn Wideman, Rush University, and Holly DiLeo, University of Texas Health Science Center San Antonio DOCTORAL EDUCATION CONFERENCE Chair: Bobbie Berkowitz, Columbia University January 24-26, 2012, Hotel del Coronado, San Diego, CA This annual conference is designed for deans, associate deans for research, directors of doctoral programs, and other faculty interested in the issues concerning this unique level of nursing education. As in recent years, the 2013 conference offered equal attention to research- and practice-focused content, with 18 sessions and 34 speakers. Over 700 participated, establishing a new attendance record. Attendees evaluated the conference highly, with an overall score of 4.325 on a 5-point scale. The Research Leadership Network also met during the conference. Subcommittee members: Lynda Davidson, Robert Morris University; Susan Dean-Baar, University of Missouri-St. Louis; Phyllis Hansell, Seton Hall University; William Holzemer, Rutgers, The State University of New Jersey; Patricia Howard, University of Kentucky; Barbara St. Pierre Schneider, University of Nevada - Las Vegas; and David Vlahov, University of California San Francisco FACULTY DEVELOPMENT CONFERENCE Chair: Susan Fetsch, Avila University Success Strategies for New Faculty February 7-9, 2013, Omni Jacksonville Hotel, Jacksonville, FL This annual conference is aimed at those new to the faculty role and those who want to gain more self-confidence in teaching in baccalaureate and higher degree programs. In addition to four plenary topics, attendees selected four concurrent topics from a slate of 12, all offering pragmatic guidance on specifics of classroom and clinical teaching. This event attracted 171 participants, and evaluations are in progress. Subcommittee members: Francesca Armmer, Bradley University; Peggy Ellis, Saint Louis University; Robin Remsburg, George Mason University; Heidi Taylor, West Texas A&M University; Sarah Thompson, University of Colorado; Christine Wynd, Ursuline College; and Lin Zhan, University of Memphis 9 MASTER’S EDUCATION CONFERENCE Chair: Debera Thomas, Northern Arizona University Looking Forward: Preparing Master’s Nursing Graduates for the Future February 21-23, 2013, Buena Vista Palace, Orlando, FL This conference is designed for master’s educators, representing many programs in transition. Plenary topics included policy implications in graduate education; challenges in online education; informatics priorities; CCNE accreditation standards; and future health care roles for master’s graduates. Concurrent and abstract sessions encouraged attendees to pursue topics of personal interest and applicability. Over 385 attended and evaluations are in progress. Subcommittee members: Betty Adams, Prairie View A&M University; Julie Anderson, University of North Dakota; Elizabeth Buck, Maryville University-Saint Louis; Lillia Loriz, University of North Florida; Helen Melland, Montana State University; Tommie Norris, University of Tennessee Health Science Center; Julia Stocker-Schneider, University of Detroit Mercy HOT ISSUES CONFERENCE Chair: Barbara Ihrke, Indiana Wesleyan University Online Teaching-Learning: Policies and Practices for the Future of Nursing Education April 11-13, 2013, Sheraton Westport Lakeside Chalet, St. Louis, MO This year’s biennial conference focuses on online nursing education. Plenary topics include online educational delivery models; regulatory issues of distance education; fun and effective applications in online teaching and learning; strategies for clinical experiences and interprofessional approaches in online learning; and global strategies using virtual communication. Concurrent and abstract sessions will allow attendees to explore topics of personal interest. Registration is in progress. Subcommittee members: Lorraine Frazier, University of Arkansas for Medical Sciences; Diane Haleem, Marywood University; James A. Hauschildt, Saint Luke's College of Health Sciences; Cynthia McCurren, Grand Valley State University; and Jan Jones-Schenk, Western Governors University SUMMER SEMINAR July 21-24, 2013, The Lodge at Vail, Vail, CO Popular executive coach and author Cy Wakeman returns for a workshop on executive leadership. The theme and program details are in progress and the brochure will be available soon. 10 Government Affairs Report March 2013 Executive Summary: An Overview of AACN’s Advocacy Progress As of March 3, 2013 I. Amplify nursing’s leadership role in the redesign and improvement of the healthcare delivery system. On November 1, 2012, the Center for Medicare and Medicaid Services (CMS) announced a final rule that will allow Certified Registered Nurse Anesthetists (CRNAs) to continue to provide and be reimbursed for chronic pain management services and all services within the full scope of CRNA practice. This ruling was a tremendous success following the dedicated campaign, Protect My Pain Care, spearheaded by the American Association of Nurse Anesthetists (AANA). AACN lent our name as well as our voice to this initiative, and we are hopeful that rulings of a similar nature will be adopted for all Advanced Practice Registered Nurses (APRNs) nationally and by state. AACN remains committed to addressing scope of practice barriers at the federal level and offers our resources to AACN state delegations. Most recently, AACN wrote to a technical review committee in Nebraska that was tasked with reviewing documentation for proposed legislation that would remove the requirement for Nurse Practitioners (NPs) to have an Integrated Practice Agreement (IPA) with physicians. To view a copy of this letter, see: http://www.aacn.nche.edu/governmentaffairs/SOP-in-Nebraska.pdf II. Advance new and existing nursing education legislation that will meet the call for a more highly educated nursing workforce. In the beginning of February, AACN met with staff from Senators Richard Durbin (D-IL) and Al Franken’s (D-MN) offices as well as Senate Health, Education, Labor and Pensions (HELP) Committee staff to discuss the role of Registered Nurses (RNs) and APRNs as these legislators look to increase the pipeline of healthcare professionals. Representative David Joyce (R-OH) will co-chair the House Nursing Caucus with Representative Lois Capps, RN (D-CA). AACN has met with the Congressman as well as his staff and are delighted by his dedication to supporing the nursing workforce at the federal level. III. IV. Expand federal appropriations to increase funding for professional nursing education. & Improve the federal investment in nursing research and elevate the role of nursing science in healthcare innovation. 11 On January 1, 2013, the House (by a vote of 257-167) and Senate (by a vote of 89-8) passed a deal that would prevent the American economy from going over the "fiscal cliff." The American Taxpayer Relief Act of 2012 (H.R. 8) addressed a series of tax provisions and delayed the sequestration (automatic cuts to discretionary spending) by two months to a new deadline of March 1, 2013. Congress failed to meet this deadline and on March 1, 2013, the Office of Management and Budget (OMB) released its Report to Congress on the Joint Committee Sequestration for FY 2013 with guidelines on how the agencies will impose the sequestration. Congressional Overview: President Barack Obama was re-elected for a second term on November 6, 2012. The elections did not change the majority of the House, which remains in Republican control, and the Senate, which is controlled by the Democrats. The results of the election were quickly overshadowed by the need for Congress and the Administration to address the “fiscal cliff,” which included negotiating a series of tax provisions and the sequestration (a set of automatic spending cuts enacted by the Budget Control Act of 2011[BCA]). At the final hour, the House (by a vote of 257-167) and Senate (by a vote of 89-8) passed the American Taxpayer Relief Act of 2012 (H.R. 8). Of interest to AACN’s advocacy, the legislation delayed the sequestration by two months to a new deadline of March 1, 2013. On January 3, 2013, the 113th Congress began its first session. Members were immediately tasked with addressing the national deficit under this new timeline. However, on March 1, 2013, Congress did not pass a solution to sequestration, and the spending cuts are now in effect. As federal dollars become increasingly scarce and the demand for RNs and APRNs continues to grow, it is essential that AACN advocacy efforts remain firm and heightened in this political climate. AACN envisions our individual and collective advocacy with the nursing community will intensify in the new Congress. The support of our membership is vital to AACN’s success in these endeavors. The following Government Affairs Report is based on the six goals outlined in AACN’s 2012 and 2013 Federal Policy Agenda and AACN’s 2012 and 2013 Strategic Government Affairs Goals set by the Government Affairs Committee (GAC) and approved by the Board of Directors in January 2012 and 2013. The six priorities are listed below and present Congressional action as well as describe the political climate, major legislative initiatives supporting nursing education, research, and practice and AACN’s advocacy efforts, in consultation with Wheat Government Relations, to address these goals. This report reflects the most up-to-date information as of March 3, 2013. 12 AACN’s FEDERAL POLICY AGENDA I. Amplify nursing’s leadership role in the redesign and improvement of the healthcare delivery system. a. Federal Barriers to APRN Scope of Practice In AACN’s October GAC report, it was noted that AACN urged CMS to issue a final rule that restores direct reimbursement to CRNAs for chronic pain management services, while not additionally burdening states to define what is “related to anesthesia.” While states set scope of practice, they do not typically define what is “related to anesthesia.” If states are required to define this, patient access to care could continue to be impaired. AACN supported our colleagues at AANA through their Protect My Pain Care campaign. On November 1, 2012, CMS announced its final ruling on Medicare coverage for chronic pain management services. CRNAs will continue to be directly reimbursed. AANA provided the following highlights of this final rule that went into effect on January 1, 2013. Expanding Medicare coverage of services within CRNA scope of practice by stating that “Anesthesia and related care means those services that a certified registered nurse anesthetist is legally authorized to perform in that state in which the services are furnished”; Agreeing with the AANA and those who submitted comments through the Protect My Pain Care campaign, whose overarching message was that the primary responsibility for establishing the scope of services CRNAs are trained for and authorized to furnish resides with the states; and Defining the Medicare benefit category for CRNAs as including any services CRNAs are permitted to furnish under their state scope of practice. During the 113th Congress, AACN will work with our colleagues representing APRNs to advance legislation and address regulation that removes scope of practice barriers. AACN belongs to the APRN Workgroup, which is comprised of national APRN organizations and the American Nurses Association, to develop a unified strategy when possible. Currently, a task force within the workgroup is finalizing the legislative and regulatory priorities for the year. Additionally, AACN was asked to lead a task force within the workgroup to address many of the workforce questions being posed by the Congressional offices. To keep members apprised of our work, AACN has created an APRN advocacy page to post our efforts, which can be found at http://www.aacn.nche.edu/government-affairs/aprn-advocacy. On this site, members will be able to see AACN recent advocacy work, such as the efforts to remove scope of practice barriers at the state level. For example, on February 26, 2013, AACN wrote to the Nebraska technical review committee that was tasked with reviewing documentation for proposed legislation that would remove the requirement for NPs to have an IPA with physicians. In AACN’s letter, the association highlighted the national support for state legislatures to remove these unnecessary barriers such as the comments from the Federal Trade Commission, National Governors Association, and the Institute of Medicine. Additionally, in AACN’s work to advance the voice of national nursing leadership in health care, the association sent a letter, signed by President Jane Kirschling, to the Senate Finance Committee on February 6, 2013, applauding their consideration of Marilyn Tavenner, RN, MHA as Administrator of CMS. AACN also supported the letters sent by the Nursing Community on February 26, 2013 and by the Tri-Council on March 1, 2013 with the same message. 13 II. Advance new and existing nursing education legislation that will meet the call for a more highly educated nursing workforce. As noted, when the 113th Congress began in early January, Congress set to work on the fiscal debates necessary to avoid sequestration, and these talks consumed the national dialogue for two months. Many issues concerning the federal budget still need to be addressed in the coming months. However, AACN anticipates that during this Congress, there will be considerable discussion concerning growing the healthcare workforce. In the beginning of February, AACN met with staff from the Senate HELP Committee as well as Senators Richard Durbin and Al Franken offices to discuss the role of RNs and APRNs as these legislators look to increase the pipeline of healthcare professionals. In addition, AACN was recently asked by the Senate Special Committee on Aging to speak with their staff on the role nurses can and should play in long-term care. This meeting will take place later this month. Representative David Joyce will co-chair the House Nursing Caucus with Representative Lois Capps, RN. AACN has met with the Congressman as well as his staff and are delighted by his dedication to supporting and developing the nursing workforce. Representative Joyce’s wife is a nurse. Through AACN’s work with the Nursing Community, a forum of 57 national nursing organizations that AACN convenes, two receptions were hosted over the past two months that allowed staff to discuss with legislators the importance of academic progression for nurses. The first was a welcome reception hosted on January 22, 2013. Members of the Nursing Community had the opportunity to engage with fourteen members of Congress in attendance and numerous staff. House Nursing Caucus co-chairs Rep. Lois Capps and Rep. David Joyce offered remarks, as did Rep. Suzanne Bonamici (DOR), Rep. Carolyn McCarthy (D-NY), Rep. Charlie Rangel (D-NY), and Rep. Jan Schakowsky (DIL). Rep. Gerry Connolly (D-VA), Rep. Julia Brownley (D-CA), Rep. Walter Jones (R-NC), Rep. Howard Coble (R-NC), Rep. Nick Rahall (D-WV), Rep. Leonard Lance (R-NJ), Rep. Glenn Thompson (R-PA), and Rep. Brett Guthrie (R-KY) were also in attendance. The second reception was hosted on February 27, 2013 by the Robert Wood Johnson Foundation (RWJF), AARP, and the Nursing Community in collaboration with the House and Senate Nursing Caucuses. This reception brought together representatives from the RWJF and AARP Campaign for Action’s State Action Coalitions. House Nursing Caucus co-chairs Rep. Lois Capps and Rep. David Joyce attended and spoke with the participants. Finally, AACN anticipates that the Higher Education Act (HEA) will be reauthorized in 2014. AACN will be working independently and with our colleagues in the higher education community to see changes set in place that will promote our nation’s nursing students. AACN also will work with the Federation of Associations of Schools of Health Professions to focus on HEA reauthorization as well as promoting interprofessional education in the 113th Congress. III. IV. Expand federal appropriations to increase funding for professional nursing education. & Improve the federal investment in nursing research and elevate the role of nursing science in healthcare innovation. 14 Since the October GAC report, the federal budget and appropriations process has been stalled due to the continued “fiscal cliff” crises and the sequester that went into effect on March 1. As noted, on September 28, 2012, the President signed into law the Continuing Appropriations Resolution [P.L. 112-175] or “CR”. The CR will continue to fund government operations at a level of $1.047 trillion, which is consistent with the level outlined in the BCA, and is above the Fiscal Year 2012 level ($1.043 trillion). The agreement also included a 0.612% across-the-board increase to most federal programs. Yet, according to a bulletin released by OMB, the 0.612% increase will not be automatically allocated, and agencies may submit a written request for that funding. Impact of Sequestration on Nursing Education and Research Programs On January 1, 2013, the House and Senate passed a deal that would prevent the American economy from going over the "fiscal cliff." The American Taxpayer Relief Act of 2012 (H.R. 8) addressed a series of tax provisions and delayed the sequestration by two months to a new deadline of March 1, 2013. The bill called for a reduction in the amount that would be cut through sequestration by $24 billion over nine years. In order to delay the sequester, the legislation lowered the spending caps outlined in the BCA in FY 2013 and FY 2014. Cuts will be made to both defense discretionary spending and non-defense discretionary spending. AACN did not take an official position on the entirety of this legislation. However, the association advocated with the broader health and education communities to request that Congress find a balanced approach to sequestration. During the Fall meeting, AACN held a Virtual Advocacy Day for member deans, faculty, and students. AACN’s message to legislators focused on the impact sequestration would have on healthcare programs, specifically highlighting the potentially devastating cuts to nursing education and research. During the Virtual Advocacy Day, 93 AACN member deans, faculty, and students sent over 300 messages to 157 Members of Congress. On March 1, 2013, Congress was unsuccessful in meeting the deadline to reach a budget deal in order to prevent sequestration from going into effect. Shortly thereafter, OMB released its Report to Congress on the Joint Committee Sequestration for FY 2013. It required that the federal agencies report the “calculations of the amounts and percentages by which various budgetary resources are required to be reduced, and a listing of the reductions required for each non-exempt budget account.” Additionally, it is on the onus of the agencies to report how they will function under the sequestration. It is important for AACN members to understand that the cuts must occur within the seven months remaining in FY 2013 as opposed to the full 12-month fiscal year. Therefore, OMB reported its earlier calculations that projected the percentage of cuts to non–exempt defense discretionary and non-defense discretionary will be inflated from 13% for defense and 9% for non-defense (earlier projections were 8.9% and 5%, respectively). On page 24 of the report, OMB outlines the impact for the Health Resources and Services Administration. While it is not broken down by program level (i.e. Title VIII Nursing Workforce Development programs), it notes varying percentages (from 2-5%). Similarly, the impact on the National Institutes of Health is not broken down by institutes and centers and reflects a 5% cut. However, as noted above, the actual funding impact depends on when the program or grants are funded and would more likely be a 9% reduction. Agencies are expected to issue guidance the week of March 4, 2013, at which time more will be known on the impact to AACN programs of interest. To read the full report, see, 15 http://www.whitehouse.gov/sites/default/files/omb/assets/legislative_reports/fy13ombjcsequestration report.pdf AACN will continue to keep our members apprised as the impact of sequestration unfolds. Finally, the President is expected to release his FY 2014 budget in mid-March. The release of his budget request will trigger the start of the FY 2014 appropriations season. At that time, AACN will work with our colleagues in the nursing and healthcare community as well as our Congressional Champions to determine a funding request for programs of interest. AACN’s STRATEGIC GOVERNMENT AFFAIRS GOALS I. Enhance AACN member education and identify federal funding opportunities for nursing and healthcare research in addition to programmatic grants. AACN provides outreach in number of ways to educate the membership on policy issues: In our efforts to better coordinate with member school’s advocacy agenda, AACN announced the launch of our University Government Relations Collaborative (UGRC) in October. Approved by AACN’s Board of Directors in July 2012, the purpose of the UGRC is to provide university government relations (GR) staff a direct link to AACN’s Government Affairs department concerning nursing education advocacy initiatives and other federal policy work. This collaborative, with close to 100 members, strives to ensure that GR representatives are armed with the most current advocacy efforts to help promote a clear, consistent, and unified message to federal and state legislators on national nursing issues. To date, the UGRC has had three conference calls to discuss collective advocacy goals. In August 2009, the government affairs staff introduced AACN’s Policy Beat. This monthly newsletter is incorporated into AACN’s News Watch and sent to AACN nursing education constituents via Capwiz. Monthly issues are posted on AACN’s government affairs website under Nursing Policy Beat. As of this report, AACN’s Policy Beat reaches 5,173 nursing deans, directors, chairs, faculty, students, and other nursing advocates, up 30% from Fall 2012. The purpose of this newsletter is to provide members and constituents with a more in-depth discussion of current government affairs issues that impact nursing education and research. AACN’s Grassroots Network has grown tremendously in 2012, with 2,383 new advocates having joined. To date, nearly 200 new advocates have signed up in the past two months. AACN encourages its members to have faculty and students sign up to be a part of AACN’s Grassroots Network. To register for the network, see http://capwiz.com/aacn/mlm/signup. This Spring AACN will present the Advocate of the Year Award to Nancy DeBasio, PhD, RN FAAN, Dean and professor at the Research College of Nursing. II. Develop Nursing Policy Leaders a. Faculty Policy Intensive 16 In October, AACN announced its inaugural Faculty Policy Intensive (FPI), which will be held March 18-21, 2013, in Washington, DC. This new initiative, approved by AACN’s Board of Directors in July 2012, will provide an in-depth immersion into healthcare policy and political process. The following eight faculty members were selected from a pool of highly competitive applicants to join the inaugural class. Patricia Brennan, PhD, RN, MS, DPNAP Assistant Professor Samuel Merritt University Lilia A. Fuentes, DNP, APRN, FNP-BC Assistant Professor The University of Texas – Pan American Camille Burnett, PhD, MPA, RN, PHCNS-BC, BScN, DSW Assistant Professor University of Virginia Mary Garnica, DNP, APNFNP-BC Assistant Professor University of Central Arkansas Joanne Noone, PhD, RN, CNE Associate Professor, Associate Dean, Oregon Health & Science UniversityAshland Campus Oregon Health & Science University Melondie Carter, DSN, RN Associate Professor University of Alabama Sharon Guthrie, PhD, ARNP, CPNP, NCSN, RN-BC Assistant Professor Mount Mercy University Andrea Sonenberg, DNSc, WHNP, CNM Assistant Professor Pace University 17 b. 2013 Student Policy Summit The fourth annual Student Policy Summit will be held March 17-19, 2013, in Washington, DC. The Summit is open to baccalaureate and graduate students of AACN member schools who desire to gain an insider’s look at the legislative process and nursing’s role in healthcare policy. Summit attendees are provided a rich experience that includes discussion sessions with leaders from federal departments and agencies, as well as the opportunity to meet with members of Congress and their staff to discuss issues relating to nursing education, research, and policy. AACN is thrilled with the interest in this year’s Student Policy Summit. Over 130 students will attend, and a robust waitlist needed to be generated. Each year, AACN sponsors two exceptional nursing students to participate. These students are chosen from an impressive array of applicants from AACN member schools across the country. Ilona van der Ven is a BSN student at Hartwick College in New York, and Erin Johnson Cole is a second year DNP student at the University of Utah studying nurse midwifery and women’s health. Regarding her desire to attend the Summit, Illona says “As an undergraduate nursing student, my education is based on the AACN Essentials in Baccalaureate Education, which focuses on leadership and decision-making abilities in the next generation of nurses. I envision that future nurses will be leaders in advocating for policies that will reduce the social inequities that are the real root of the problem. I envision that nurses will be the key component in designing solutions to create a better way to deliver health care that is equitable, effective, and affordable.” Erin wishes to attend the Summit to further develop her policy knowledge base and advocacy skills. “I want to be a part of this dynamic political process, either as an elected official or policymaker, to be a part of the change I hope to see. However, while I have the interest, the confidence, and the educational background to pursue policy work or even an entry into politics itself, I certainly don’t know the inner workings of the system. I have the communication skills and the comfort with public speaking to pursue these career avenues, but I need to develop my political savvy. I hope to begin to build these skills at the 2013 AACN Student Policy Summit.” 18 AACN-AONE Academic-Practice Partnerships Steering Committee March 2013 The AACN-AONE Academic Practice Partnership Steering Committee continues its work on the Academic Practice Partnership initiative. The Academic-Practice Partnership Online Collaboration Community currently has 709 academic members and over 100 practice members. Discussions have been extensive, and the steering committee members monitor the site and serve as moderators. Two Webinars were presented in October and November 2012 with exceptional interest and high attendance. Three additional Webinars are planned for Summer and Fall 2013. The Steering Committee continues to meet monthly via conference call. A third article highlighting the outcomes of the April conference will be published in Nurse Leader in late Summer 2013. The Steering Committee is currently working on finalizing the evaluation matrix, which will be integrated into the Online Toolkit. Plans are well underway for the April 18-19, 2013 conference, Implementing Successful Academic Practice Partnerships, to be held at the Westin Michigan Avenue in Chicago. Program sessions will be presented by Dr. Teri Pipe, Arizona State University; Dr. Bechara Choucair, Commissioner of the Chicago Department of Public Health; and Dr. Melanie Dreher, Rush University. Exceptional partnership panel presentations will be presented by the University of Michigan School of Nursing and the University of Michigan Health System; the University of Alabama at Birmingham School of Nursing and the Birmingham Veterans Affairs Medical Center; and the University of WisconsinMadison School of Nursing and the Shawano-Menominee Counties Health Department. Additional conference details can be found at this link: http://www.aacn.nche.edu/leading-initiatives/academic-practice-partnerships The Steering Committee members are: Judy Beal, Co-Chair, Simmons College Sharon Gale, Co-Chair, AONE Representative, Organization of Nurse Leaders Anna Alt-White, Office of Nursing Services, VA Judith Erickson, Jacksonville University Irene Fleshner, Genesis Healthcare Judith Karshmer, University of San Francisco Susan Swider, Rush University Jennifer Ahearn, AACN Staff Liaison 19 Bylaws Task Force March 2013 The recommendations for bylaws revisions will be voted on during the Business Meeting on Monday, March 18, 2013. The documents for consideration are included in the Business Meeting Materials in the meeting packet. The first document reflects the current bylaws, recommended bylaws changes, and justification for the change. The second document is a draft of the new Bylaws should all the changes be approved. These documents have been reviewed by the AACN attorney, and suggested language and feedback was received throughout the process from the attorney, AACN board consultant, and parliamentarian. The majority of the proposed modifications are editorial with the goal of streamlining the bylaws or providing clarification. The Bylaws Task Force was appointed in Fall 2011 with the charge to review and make recommendations for changes in the Bylaws. The task force met nine times including two in-person meetings and seven conference calls. Reports were provided to the AACN membership during the Task Force Updates and Business Meeting at the 2012 Spring Annual Meeting. The Board of Directors approved the changes on July 22, 2012 during the summer Board of Directors Meeting. Members were provided information about the Bylaws changes with the premeeting mailing materials for both the 2012 Fall Semiannual Meeting and 2013 Spring Annual Meeting. The vote was originally scheduled to take place during the fall meeting in October 2012; however, the vote needed to be rescheduled since a quorum was not present during the Business Meeting due to Hurricane Sandy. Task Force Members Fay Raines, University of Alabama-Huntsville, Chair Nancy DeBasio, Research College of Nursing Daisy Cruz-Richman, SUNY Downstate Jennifer Ahearn, Staff Liaison 20 Faculty Development Initiative March 2013 Webinars Since September 2012, AACN has offered 18 webinars with a total of 7,353 individual registrations; of the 7,353 individual registrations, 4796 actually joined the webinar, reflecting an average attendance rate of 65.2%. Faculty from 600 AACN member schools, representing 82.7% of the membership, attended at least one live webinar event during this period. Graduate student registrations at webinars accounted for 955 of the individual registrations. In addition, recordings of the webinars are available for AACN faculty, deans, and graduate students to access through AACN’s website and Online Collaboration Communities. There were over 855 member faculty views and more than 360 student views of archived webinar recordings. The following webinars, listed in order of their presentation dates, have been offered since September 2012. Please note that continuing nursing education credits from the American Nurses Credentialing Center (ANCC) were provided for all: 1. Controversies in Pain Management (registration=241) 2. Implementing the Consensus Model by 2015: Preparing APRNs to Care for Older Adults (registration= 314) 3. Incorporating Environmental Sustainability into Nursing Programs: Environmental Health and Sustainability in Simulation Labs and Nursing Education (registration= 142) 4. Integration of Genomics into Nursing Curricula (registration=415) 5. Debriefing Techniques in Simulation (registration=443) 6. The Importance of Academic-Practice Partnership (registration=311) 7. Another Way to Measure Learning: Technology Enhanced Competency Based Learning (registration= 312) 8. Navigating Academic Progression: National Insights and Action (registration= 467) 9. Academic-Practice Partnerships: If Not Now….When? (registration=282) 10. Building the Future and Continuing the Excellence: The UHC/AACN Nurse Residency Program Curriculum Update (registration=207) 11. Meeting the Expectations of the Consensus Model: Enhancing Gerontology Content in NP and CNS Programs (registration=199) 12. Simulation Evaluation (registration=411) 13. The New Congress and Nurses’ Future (registration=476) 21 14. Preparing Collaborative Ready Practitioners: Interprofessional Education (registration=387) 15. Collaborative Academic Progression Models: Showcasing Successful Partnerships (registration=342) 16. Nursing and Healthcare Delivery Under the 113th Congress (registration=1502) 17. Evaluating Class Size and Online Education (registration=450) 18. Implementing the Consensus Model by 2015: Education and Certification Requirements for CNS Programs (registration=160) 19. Five Tips for Applying ANA’s Scope and Standards in Practice and Education (registration=221) 20. Preparing for the Student Policy Summit: The Importance of Advocacy (registration=71) 21. February 26, 2013: Teaching Nursing Students to Care for Veterans, Part I (registration=72) Additional scheduled spring 2013 webinars include the following topics. Please note that ANCC continuing nursing education credits will be offered for all unless otherwise noted: 1. March 4, 2013: Online Education: Choosing between Synchronous, Asynchronous, or Hybrid Modalities 2. March 5, 2013: Integrating Oral-Systemic Health in Graduate Nursing Programs: A Faculty Tool Kit 3. March 6, 2013: Making Academic Progression Successful: Trends Among Nurses 4. March 11, 2013: Government Affairs (topic to be announced) 5. March 13, 2013: Strategies to Support the Teaching and Learning of Clinical Reasoning 6. March 14, 2013: Using the AACN/EBI DNP Assessments for Program Improvement (no ANCC contact hours will be awarded so that a perceived conflict of interest is avoided; however, an attendance certificate will be provided to all participants) 7. March 21, 2013: Designing the Unbundling of Courses 8. April 3, 2013: When Warriors Come Home: What Their College Professors Need to Know 9. April 4, 2013: Clinical Teaching: The Critical Connection to Students’ Success: Part I: Setting Realistic Expectations for a Positive Clinical Experience: Where to Begin? 10. April 5, 2013: Achieve Much More in Less Time with Power Strategies for Academic Work 11. April 9, 2013: Improvement of NCLEX Scores 12. April 11, 2013: Clinical Teaching: The Critical Connection to Students’ Success: Part II: Teaching and Connecting in Clinical: Tools for Clinical Faculty 13. April 16, 2013: Calculating Faculty Workloads 14. April 18, 2013: Clinical Teaching: The Critical Connection to Students’ Success: Part III: Evaluating Student Performance in Clinical: Meeting the Challenge with Proven Solutions 22 15. April 24, 2013: Teaching Nursing Students to Care for Veterans, Part II 16. April 30, 2013: Managing Clinical and Adjunct Faculty 17. May 1, 2013: Teaching Nursing Students to Care for Veterans, Part III Online Collaboration Community In October 2011, a grand opening of the AACN Collaboration Community took place at the Fall Semiannual Meeting. This new service is exclusively for deans and faculty of member schools; it provides an interactive, social media platform that enables members to share knowledge and best practices, establish collaborative relationships, and form strategic alliances with peers. To date, there are 3,000 dean and faculty members selfenrolled in AACN’s Collaboration Community. This platform has also been utilized to establish other online collaboration communities: AACN Student Collaboration Community (for master’s and doctoral students); Academic-Practice Partnership Collaboration Community; CNL Collaboration Community (for practicing CNLs and CNL students); Global Alliance for Leadership in Nursing Education and Science (GANES) Collaboration Community; Public Health Nursing Education Community; Gerontology APRN Education Community; Practice Leadership Network; and the Jonas Scholars Collaboration Community. The total number of members across all communities is now 6,811. Faculty Link Newsletter AACN Faculty Link newsletter is distributed monthly to 21,565 faculty at AACN member schools. It features announcements about free webinars on faculty development topics, funding opportunity alerts, enrichment opportunities, awards and scholarship programs, government advocacy resources, and bulletins on nursing education news. Here is a link to the current issue: http://www.aacn.nche.edu/faculty/facultylink/2013/february Awards: Faculty Awards Program On October 1, 2012 a call for applications was announced for the AACN’s four Faculty Teaching Awards: The Novice Faculty Excellence in Didactic Teaching Award The Novice Faculty Excellence in Clinical Teaching Award Excellence and Innovation in Teaching Award Advancement of Teaching and Learning Scholarship Award The first two novice awards focus on faculty with five years or less teaching experience. The Excellence and Innovation in Teaching Award focuses on excellence and innovation in teaching practices, while the Advancement of Teaching and Learning Scholarship Award recognizes sustained and systematic inquiry into the practice of teaching and the environment and depth of student learning. 23 The fall 2011-2012 award winners were announced in September 2012 and are as follows: Excellence and Innovation in Teaching Award: Tami Wyatt, University of Tennessee – Knoxville Novice Faculty Excellence in Didactic Teaching Award: Lori McElroy, University of Oklahoma Novice Faculty Excellence in Clinical Teaching Award: Renee McLeod-Sordjan, Pace University Teaching and Learning Excellence Award: Pamela Ironside, Indiana University The selection committee members for these awards are volunteers from the AACN’s Instructional Leadership Network (ILN). Each reviewed four applications and the winners were chosen based on the highest rubric score. This year’s selection committee members were: 1. Patricia Allen, TTUHSC School of Nursing 2. Josie Bowman, East Carolina University 3. Joanne Clements, University of Rochester School of Nursing 4. Ellen Cram, University of Iowa, Iowa City, IA, 5. Linda Finch, University of Memphis 6. Diane McNally Forsyth, Winona State University – Rochester Center 7. Janet Fraser Hale, University of Massachusetts Medical School 8. Nancy Haugen, Samuel Merritt University 9. Katherine Leigh, Troy University 10. Karen E. Miles, Barry University 11. Cathy L. Rozmus, University of Texas School of Nursing at Houston 12. Susan M. Sullivan, Winona State University – Rochester Center 13. Jane Tang, Immaculata University 14. Patricia Wagner, Cox College The call for applications for all four awards is advertised in each Faculty Link newsletter and each issue of News Watch, beginning in October 2012 through March 2013. They are also advertised during all conferences and a headline and link to the awards is also located on the Faculty homepage: http://www.aacn.nche.edu/membership/awards This year’s due date for applications for all four faculty awards is June 1, 2013. Awards: Outstanding Dissertation and Capstone Project In July 2012 AACN’s Board of Directors voted to offer two new awards year: one for an outstanding dissertation (PhD) and the other for an outstanding capstone project (DNP). The call for nominations was released in late October and applications were due December 7, 2012. AACN received over 60 nomination packets, with 32 PhD nominations and 25 DNP nominations being deemed eligible for further review. For example, AACN rejected nominations whereby the defense dates were not within the 24 established timeframe. Additionally, two schools forwarded more than one nomination packet for the same category, so they were both directed to pick one for review, which they did. This year, the first level of review was an administrative review. The second level of review was conducted by AACN doctorally-prepared staff members, who evaluated the nominations based on the criteria established by AACN’s Board of Directors (BOD). Finally, the AACN doctorally-prepared staff members forwarded their top five to six nomination packets from each category to the next level of review, completed by six members of AACN’s BOD. For the third level of review, the dissertation nomination packets were reviewed and scored by Drs. Callahan, Howell, and Luener; the capstone nomination packets were reviewed and scored by Drs. Beal, Murray, and Sebastian. No Board member reviewed a nomination packet from her own school. Last, the reviewers ranked their choices and the winners were picked based on the final rankings. The results were as follows: PhD Award 1st place: Oleg Zaslavsky (MHA-PhD student); University of Washington (Chair – Dr. Barbara B. Cochrane); Longitudinal Dynamics in Indicators of Frailty. 2nd place: Tiffany Moore (BSN – PhD student); University of Nebraska Medical Center (Chair – Dr. Ann Berger); Model of Allostatic Load and Complications of Prematurity. DNP Award 1st place: Erin Harnett (MSN – DNP student); New York University (Associate Dean – Dr. Barbara Krainovich-Miller); Integrating Preventive Dental Care in a Pediatric Oncology Center. Tied for 2nd place: Vicky Grossman (MPH – DNP student); Duke University (Director of DNP Program – Dr. Barbara S. Turner); The Role of Health Promoters in Zinc Compliance in Guatemala. Carrie Kairys (MSN – DNP student); Johns Hopkins University (Director of DNP Program – Dr. Mary Terhaar); Improving Contraceptive Counseling by Instituting a Provider Reminder with Clinical Decision Support in the Electronic Health Record. The award winners were announced via AACN’s website: http://www.aacn.nche.edu/membership/awards/winners-dissertation-and-capstoneproject-awards and via February 2013’s issue of Faculty Link: http://www.aacn.nche.edu/faculty/faculty-link/2013/february This will now be an annual award and further information may be found here: http://www.aacn.nche.edu/membership/awards/excellence-in-advancing-nursing 25 Future award winners will be selected by a review committee comprised of PhD and DNP scholars, who will score the nomination packets and then forward their recommendations to AACN’s BODs for approval. ANCC Contact Hours As of mid-August 2012, AACN became an accredited provider of continuing nursing education by the American Nurses Credentialing Center’s Commission on Accreditation (ANCC). While most previous recipients of AACN contact hours had no difficulty using them, AACN is pleased to have a universally recognized standard for continuing education for member school deans and faculty. 26 Report on the Centralized Application Service (NursingCAS) March 2013 Since October 2012 the following activities have been initiated by AACN staff and the NursingCAS Advisory Group to support the centralized application service. Current Operations: Currently, there are over 65,000 applicants in the NursingCAS system, and 138 schools are actively using the service with several others in the pipeline to go live. Many currently participating schools are expanding the numbers of programs posted on the application to include both graduate and undergraduate level program types. Innovative Approach Planned to Launch NursingCAS Cycle 4: In order to implement major system enhancements, NursingCAS plans to launch Cycle 4 (2013 – 2014) on April 15, 2013. At the same time, the current cycle of NursingCAS (Cycle 3) will remain open until July 1 in order to avoid having a closure period and allow schools with later deadline dates to finish out the current cycle without having to change their planned deadlines. Liaison International, AACN’s partner in NursingCAS, presented this solution to AACN last fall after several advisory group discussions on what to do about implementing the next round of enhancements and launching the next cycle, while minimizing service disruption. Changes at Liaison International: In January, George Haddad, the former CEO of Liaison, stepped into a new role on the Board of Directors, and Michael Behringer was appointed as the new CEO. Michael is very enthusiastic about the growth potential of NursingCAS and has indicated that new staff resources would be allocated to help expand the service. At the beginning of February, AACN’s primary operational contact at Liaison, Tania Zavarelli, was promoted from Application Services Manager to Director of Application Services. Tania has been a great support and resource for AACN. Liaison has also appointed a new Vice President of Sales, Joe Belenardo, who has extensive experience in higher education software solutions. Joe will work directly with AACN to help initiate new promotional opportunities for NursingCAS, including regional events. Marketing to Schools: Since October 2012, AACN staff, advisory group members, and Liaison staff have engaged in a variety of marketing activities to recruit new schools to the service, including: Presentations and Webinars: At AACN’s Fall Meeting, despite Hurricane Sandy, 27 35 of the 47 registrants attended the NursingCAS session. At the Baccalaureate Conference, 48 people registered for the NursingCAS live case study, 70 people attended the NursingCAS session at the Doctoral Conference, and 72 registered for the session at the Master’s Conference. NursingCAS will exhibit at the Spring Meeting, and three NursingCAS users will be presenting on “Enrollment Management in the Digital World” during the concurrent sessions. NursingCAS program sessions are also planned for the upcoming GNAP meeting, Hot Issues Conference, and the BONUS meeting. In addition, AACN is hosting several targeted Webinars about the NursingCAS service, including a recent session specifically for graduate level programs (53 individuals registered). Three additional Webinars are planned for March, and two are planned for April. Live Case Study: On November 15, five individuals from the University of Texas Health Science Center San Antonio (UTHSCSA) presented a “live case study” to share their individual experiences using NursingCAS. The presentation featured the Associate Dean for Admissions and Student Services, the Assistant Director of Admissions and Student Services, a professor, an IT programmer, and a current student who applied to the school via NursingCAS. The presentation was recorded, and AACN plans to release a case study and video clips of UTHSCSA’s experience to help market the service. Target Marketing to Hot Prospects: AACN has mobilized the NursingCAS advisory group members to reach out via phone and email to a list of schools that we have identified as highly interested in NursingCAS. There are 75 schools on the list currently, and new schools are added as interest is shown. The advisory group’s enthusiasm and support has been vital in helping to grow the service. Site Visits and Individual Teleconferences: To assist schools with the implementation process for NursingCAS, AACN staff hold individual teleconferences and schedule live visits with university stakeholders on how to successfully transition to NursingCAS. Since October, 15 individual teleconferences and four site visits were completed. Three additional visits are planned for April to coincide with presentations at AACN conferences. Open House Planning: On June 14 from 8:30 AM – 4:30 PM, AACN and Liaison are hosting an Enrollment Management Workshop and NursingCAS Open House in Watertown, MA (outside of Boston) for prospective, new, and currently participating schools. AACN will be using a different venue this year, which is adjacent to Liaison’s offices, to accommodate up to 75 attendees. This free workshop and open house is for deans, admissions professionals, faculty, IT staff, nursing school recruiters, advisors, and other decisions makers involved in the nursing admissions process. The event is being promoted via email blasts, presentations, Webinars, and at AACN’s conferences. The Open House will be preceded by the annual meeting of the NursingCAS advisory group. 28 Joint AACN/DVA Joining Forces Task Force Membership Report March 2013 The AACN/DVA Task Force on the Joining Forces Veterans Care Tool Kit began its work in May 2012. The Task Force was co-chaired by Gail Stuart, Dean at the Medical University of South Carolina, and Suzanne Thorne-Odem, Clinical Practice Program Manager at the Department of Veterans Affairs (VA), Office of Nursing Services. The Task Force charge was to develop a document that delineates resources and exemplars to assist faculty with the implementation of curriculum elements that will appropriately address the unique needs of the veterans and their families. The Task Force consisted of a Leadership Group and a larger Working Group. Both groups included representatives from schools of nursing and the VA. All branches of the armed forces were represented by various task force members from the VA. To facilitate the work of the Task Force, the Working Group was divided into three subgroups according to the types of existing resources and exemplars that are appropriate to the care of veterans and their families. The subgroups formed were: 1) Academic Resources, 2) Veterans Affairs Resources, and 3) Private/Public/Professional Organizations/Media Resources. Each resource group was led by members of the Leadership Group. A resource evaluation form was created so that each group could identify resources and evaluate them according to a common rubric. Resources were to be identified as applicable to undergraduate or graduate education, and whether they are applicable to practicing clinicians. The Task Force held a series of conference calls between July and January to complete its charge. A description and copy of the tool kit outline is attached. In addition, a link to the online tool kit itself is provided. One unique feature of the tool kit is a form that can be submitted by faculty or others who have developed curricular or other materials and would like to have them considered for inclusion in the tool kit. A process similar to the one delineated in the AACN Plan for Updating Tool Kits (March, 2012) will be employed. A presentation, “Teaching Students to Care for Veterans,” was moderated by Dr. Stuart at the AACN 2013 Master’s Education Conference. The EVC Tool Kit went live Friday, January 18, 2013 and can be accessed at http://www.aacn.nche.edu/downloads/joining-forces-tool-kit 29 AACN/DVA Joining Forces Enhancing Veterans’ Care Tool Kit OVERVIEW In summer 2012, AACN joined with the Department of Veteran Affairs (DVA) in an effort to enhance the resources of nurses working with veterans as part of the Joining Forces initiative, with a particular focus on nursing education. To that end, this Enhancing Veterans’ Care (EVC) Tool Kit was developed to highlight resources and exemplars that can assist faculty with the implementation of curriculum elements to appropriately address the unique needs of the veterans and their families. The tool kit was developed with input from representatives of the Veterans Administration, all branches of the military, and professional nursing education. The goals of the Enhancing Veterans’ Care Tool Kit are to: Provide key educational resources that will assist schools as they engage in curricular development to incorporate quality care of veterans and their families. Suggest focused, innovative learning strategies for teaching students how to care for veterans and their families. Detail a repository of resources and relevant for all nurses who care for veterans and their families. This EVC Tool Kit will be updated on a regular basis to keep it current, and welcomes the addition of new materials related to the above goals. Tool Kit Outline Introduction General Resources (listed by topic) Educational Resources: Curricular examples: School Audience (baccalaureate or graduate) Approach (separate course or integrated) Methodology (face to face or online) Contact Person VA Nursing Academy Innovative Exemplars Webinars Power Point Presentations Simulation Scenarios Case studies/Assessment tools/Class discussions Nursing students who are veterans Other Nursing Organizations with Veteran Care Resources Submit a New Resource to this Site 30 AACN/DVA Task Force on the Joining Forces Veterans Care Tool Kit LEADERSHIP GROUP Gail W. Stuart, PhD, RN, FAAN, Co-Chair Dean Medical University of South Carolina Charleston, SC Bonnie Harmer, PhD, RN Associate Professor and Nursing Project Director, VA Nursing Academy Saginaw Valley State UniversityUniversity Center, MI Suzanne Thorne-Odem MS, RN, Co-Chair Clinical Practice Program Manager Department of Veterans Affairs, Office of Nursing Services Washington, DC Cynthia S. Selleck, DSN, ARNP Associate Dean, Clinical Affairs & Partnerships University of Alabama at Birmingham Birmingham, AL Joseph Burkard, DNSc, MSNA Associate Professor University of San Diego San Diego, CA Patricia L Ten Haaf, PhD, RN Associate Director, Patient Care Services Department of Veterans Affairs Kansas City, MO Amy W. Smith, DNP, FAANP VISN 16 Nurse Executive & Deputy Chief Medical Officer South Central VA Health Care Network Karen Spada, MSN, MPH, MHA, FNP Department of Veterans Affairs Temple, TX Joan Stanley, PhD, CRNP, FAAN, FAANP, staff liaison Senior Director of Education Policy Catherine Cox, PhD, RN, staff liaison Director of Faculty Programs Horacio Oliveira, staff liaison Education Policy and Special Projects Program Coordinator 31 WORKING GROUP MEMBERS Kent Blad, DNP, FNP-c, ACNP-BC, FCCM, FAANP Professor Brigham Young University Provo, UT Patricia L. Conard, MSN, RN Clinical Assistant Professor Texas A&M University, Corpus Christi Corpus Christi, TX Mary B Dougherty, DNSc, MBA, MA, RN National Director, Veterans Affairs Nursing Academy Department of Veterans Affairs Washington, DC Christine Engstrom PhD, CRNP, AOCN Director, Nursing Practice Department of Veterans Affairs, Office of Nursing Services Washington, DC Penny Kaye Jensen, DNP, APRN, FNPC, FAANP AANP Representative Department of Veterans Affairs Salt Lake City, UT Mary Alice Johnson, MS, RN Associate Director Patient Care Services Department of Veterans Affairs Wilmington, DE Marthe Moseley PhD, RN Associate Director, Nursing Practice Department of Veterans Affairs, Office of Nursing Services Washington, DC Beverly Priefer, PhD, RN Associate Director, Research and Education Department of Veterans Affairs, Office of Nursing Services Washington, DC Richard Reusch, MA, BSN Nurse Manager, Poly Trauma Rehabilitation Center Department of Veterans Affairs San Antonio, TX Jean Rush, MSN, APN, NP-C, RN Nurse Practitioner TBI Clinic Department of Veterans Affairs Chicago, IL Ron Ulberg, MSN, RN, CCRN Associate Professor Brigham Young University Provo, UT Pamela Wall, MSN, APN, RN Psychiatric Nurse Practitioner Uniformed Services University of the Health Sciences Camp Lejeune, NC 32 Report of the End-of-Life Nursing Education Consortium Project (ELNEC) March 2013 The ELNEC project continues to grow with 13 national and international courses offered this year alone. Since the first national train-the-trainer course was offered in 2001, over 15,200 people have attended an ELNEC session. Though ELNEC was written for nurses and by nurses, other members of the interdisciplinary team have benefitted from this unique training opportunity, including physicians, social workers, pharmacists, and chaplains. In 2013, the following ELNEC courses will be offered: ELNEC Summit: ELNEC-Core, ELNEC-Pediatric Palliative Care, and ELNECCritical Care courses were held simultaneously on February 21 & 22 in Anaheim, CA, with 200 in attendance. ELNEC-Core: Three courses will be held in collaboration with the Hospice and Palliative Nurses Association (HPNA) this year. Locations include Lake Buena Vista, FL, St. Louis, MO, and Boston, MA ELNEC-Pediatric Palliative Care: HPNA will also collaborate with the National ELNEC Project Office to offer a second pediatric course in Boston in July. ELNEC-Critical Care: A second critical care course will be held in Washington, DC in November. ELNEC-APRN: This new curriculum will debut on April 4 & 5 in Anaheim, CA. The response to this course has been tremendous. Many APRNs are leading palliative care consultation teams throughout the US and will find this education to be invaluable to their current practice. Separate tracks for APRNs working with neonatal/pediatric patients and adults will be available. A second course will be held in Washington, DC in November. ELNEC-International: ELNEC courses will be held in Albania, Kyrgyzstan, and Germany. Note: ELNEC is currently translated in 7 languages—Spanish, Russian, Japanese, Korean, German, Romanian, and Armenian. To date, ELNEC has been presented in 74 countries world-wide. Next Steps The ELNEC Team has been notified that the project will be receiving an R-25 grant in 2013 from the National Cancer Institute (NCI), which will provide funding for faculty in 33 schools of nursing with a Doctor of Nursing Practice (DNP) program. This grant will provide funds to support DNP-prepared faculty and clinical partners in providing excellent palliative care to patients with cancer. More details will be available in the coming weeks. In collaboration with the California (CA) HealthCare Foundation, the national ELNEC Project Team continues to monitor and support the work of 16 public (safety net) hospitals throughout the state of CA to enhance end-of-life care. Monthly conference calls with nursing leaders in each of these institutions provides mentoring opportunities to those delivering palliative care services to the poorest and most vulnerable citizens in the state. For more information about the ELNEC Project, go to: www.aacn.nche.edu/ELNEC Betty Ferrell, Principal Investigator of ELNEC, City of Hope, Duarte, CA Pam Malloy, Co-Investigator of ELNEC, AACN 34 Report on the QSEN National Initiatives March 2013 This report addresses the activities and progress of the QSEN national initiatives led by AACN from October 2012-March 2013. Major highlights for this time frame include: 1) Dissemination of QSEN Phase III work; 2) Progress of the QSEN Phase IV graduate faculty development grant; 3) Site visits completed for Gordon and Betty Moore Foundation (GBMF) funded QSEN institute; and 4) Annual meetings for the GBMF funded QSEN Institute/ Hospital Leader Grant. Dissemination of QSEN Phase III Work Plans are underway for a special March/April 2013 issue of the Journal of Professional Nursing describing the QSEN results. This edition will be guest edited by Jane Barnsteiner, Joanne Disch, Jean Johnson, and Kathy McGuinn. The following manuscripts will be included: 1. Diffusing QSEN Competencies Across Schools of Nursing: The AACN/RWJF Faculty Development Institutes 2. Taking a “Deep Dive” on Integrating QSEN Content in San Francisco Bay Area Schools of Nursing 3. Fundamentally Updating Fundamentals 4. From the School of Nursing Quality and Safety Officer: Nursing Student’s Use of Safety Reporting Tools and Their Perception of Safety Issues in Clinical Settings 5. Academic/Clinical Partnership and Collaboration in QSEN Education 6. Nursing Student Medication Errors: A Case Study Using Root Cause Analysis 7. Human Cognition and the Dynamics of Failure to Rescue: The Lewis Blackman Case 8. A Task Force Model for Statewide Change in Nursing Education: The Michigan Experience To further the dissemination of the QSEN Phase III work, six web-based learning modules that focus on undergraduate teaching strategies for the QSEN competencies were developed and implemented. These web-based learning modules help faculty in pre-licensure programs tobetter prepare nurses with the knowledge, skills, and attitudes (KSAs) necessary to continuously improve the quality and safety of patient care in the healthcare systems where they work. The QSEN learning modules will give faculty the tools to: 35 Review with faculty the fundamental quality and safety concepts necessary to achieve the six QSEN competencies. Lead other faculty at their institution to incorporate or improve a quality and safety curriculum. Teach and mentor students regarding the concepts and skill necessary for high quality and safe patient care. Module development included the following processes: subject matter development and review; course setup and production support; instructional design of the modules; marketing and registration; hosting and maintenance of the modules; and applicant registration and awarding of CEU’s. The three QSEN expert consultants, Jane Barnsteiner, Joanne Disch, and Jean Johnson, who taught in the eight pre-licensure QSEN faculty development institutes, developed and recorded the modules. In order to assess the learner’s acquisition of the knowledge, the modules included assessment questions so that participants are able to receive ANCC contact hours. The expert consultants are committed to updating the modules on an annual basis for the next five years. The modules were launched on January 11, 2013. In order that a broad array of faculty, students, and practice partners can use these excellent resources, the modules are hosted on the AACN online Collaboration Community as well as the QSEN.org website, which is hosted by Case Western Reserve University. AACN’s Collaboration Community was created exclusively for faculty and deans and serves as a social media platform that enables participants to share knowledge and best practices. Marketing strategies for the QSEN modules include a brochure and promotional materials that will be widely disseminated at AACN conferences. Thus far, according to the iCohere statistics, self-assessment tests for all six modules have been taken 678 times: Evidence-Based Practice Test: taken 88 times Health Informatics Test: taken 83 times Patient-centered Care Test: taken 95 times Quality Improvement Test: taken 81 times Safety Test: taken 214 times Teamwork and Collaboration Test: taken 117 times Statements made on the evaluations for the QSEN modules include: “Joanne was easy to listen to and interesting. She pulled me into the content. I loved her use of repeating so that the most important concepts were emphasized.” “Very good presentation. Excellent examples of dream team in Olympics. Presenter made clear distinction between "expert team " and "team of experts."” “Speaker did an excellent presentation-really clarified the steps of evidence-based research” “Very good speaker, knowledgeable and interesting!” The work for QSEN Phase III is now complete. 36 Phase IV RWJF QSEN Grant for Graduate Faculty Development The Robert Wood Johnson Foundation has awarded $964,388 in new funding to AACN to extend the reach of the national QSEN initiative. Phase IV runs from March 2012February 2014. The grant focuses on developing the capacity of graduate nursing program faculty to teach other faculty how to incorporate quality and safety competencies and content into their programs of study. Although Advanced Practice Registered Nursing (APRN) programs are a focus of this initiative, the training institutes target all faculty in graduatelevel programs to assure that the full diversity of graduate education, such as public health or systems management, is represented. This train-the-trainer initiative encourages the participation of clinical partners through a series of five one-day institutes offered in conjunction with major organization meetings, including the CNL Summit, AACN Master’s Education Conference, NONPF Conference, American Nursing Informatics Association, and AACN Doctoral Education Conference. Thus far, two QSEN Graduate Faculty Development Workshops have taken place: New Orleans, January 16-17: 83 Attendees 65 Schools 30 States Orlando, February 20-21: 110 Attendees 95 Schools 33 States The faculty response to the first two pre-conferences has been extremely positive. Jean Johnson and Kathy McGuinn will present about the QSEN Phase IV work at the May 2013 National QSEN Forum, Embracing New Heights, in Atlanta. GBMF QSEN Institute Grant The work of the GBMF QSEN Institute Grant is now complete. The GBMF expected outcomes were attained for this grant. A final survey of the 22 participating schools was conducted to ascertain progress in 1) training faculty, 2) diffusing content across the curriculum, 3) determining the number of students exposed to the QSEN competencies: • Percent/Number of Faculty Trained in QSEN Competencies. There are a total of 777 faculty across the 22 schools. Reported school faculty sizes range from 6 – 145. Respondents reported that across all schools a mean of 72% of faculty have been trained in the QSEN competencies. Eight schools reported that 100% of the faculty have been trained in the QSEN competencies, nine schools reported 50% or more of faculty have received training while 4 schools reported that fewer than 49% of faculty have received training. 37 • • Number of nursing courses that have received an enhancement of quality and safety content. On average, respondents indicated that 90% of courses have QSEN content. Fifteen of the 22 (68%) schools reported that 100% of their courses have been enhanced with QSEN content. Number of students who were enrolled in those modified nursing courses. 3506 (88%) of the 3978 enrolled students have completed a course with QSEN content over the past year. GBMF Hospital Leader Grant Follow-up Site Visits AACN and GBMF are conducting “deeper dive evaluations” of the June 2010 San Francisco Bay Area (SFBA) QSEN Institute through a series of site visits in April 2012, April 2013, and September 2013. In addition, the 2013 site visits also will include a “deeper dive evaluation” of the October 2012 Informatics Conference sponsored by the University of Minnesota. These evaluation processes assess the integration of the QSEN competencies into the curricula and included visits to nursing schools in the five county SFBA. Examples of site visit activities included the following: review of QSEN enhanced curriculum programs; examination of course syllabi and other curricular materials; interviews with faculty, students, and clinical sites; review of policies and procedures that schools have in place for QSEN integration; assessment of schools’ organizational systems as they relate to the implementation of QSEN principles. Prior to the visits, AACN requests supporting documentation from the school that assists with the assessment process. The April 2012 site visits went exceedingly well, and the QSEN evaluation team thought it was very gratifying to observe the progress that each school had made since the 2010 QSEN Institute. A wonderful highlight of the visit was the ability to speak with the students and observe their ability to articulate the QSEN competencies. A template with 48 items was used to evaluate the school’s QSEN integration during the site visits. Each item was rated on a scale of 0-2: 0= Not Evident; 1=Evident; 2= Exceeds Expectation. There was a high degree of agreement between the reviewer’s and the non-partial observer’s results. Upon analysis of the evaluation templates, two of the six schools were early adopters and exemplars for the integration of the QSEN competencies. One of the schools will implement a new curriculum based on the QSEN competencies by 2013. One of the schools has not been able to make the anticipated progress with QSEN integration. The stability and support of leadership and access to resources are two major factors that influence the degree of QSEN implementation. Annual Meetings AACN and GBMF are preparing to host the final follow-up meeting on June 13, 2013 in Palo Alto. The purpose of the meeting will be to report progress towards implementation of the QSEN competencies and have participants share challenges and best practices. 38 AACN will share aggregate data from the evaluations (i.e., on additional faculty trained, number of nursing courses enhanced with the quality and safety content, and number of students enrolled in these courses). Each school will be provided with their individual pre- and post-data to illustrate their progress and to compare their progress with the aggregate during this meeting. In addition to setting the stage for a facilitated discussion of the implementation progress, this meeting will provide a competitive incentive for schools to accelerate their integration of the QSEN competencies. Additionally the program will assess: Ways to facilitate inter-school communication and collaboration Ways to make the listserv work better and identify other ideas for communication and collaboration links A facilitated breakout session will be held to assess future plans, anticipated challenges, and resources needed to continue progress toward implementation of the QSEN competencies. Finally, there will be a celebration to commend the schools on their hard work and attainment of integration of the QSEN competencies into the curriculum. 39 Report of the UHC/AACN Post-Baccalaureate Nurse Residency Program March 2013 This report addresses the activities and progress of the UHC/AACN Post-Baccalaureate Nurse Residency Program from October 2012 – March 2013. During this time frame, highlights include: 1) Expansion of nurse residency program; 2) Conferences, Webinar, Article; 3) NRP strategic planning; and 4) accreditation of nurse residency programs; and 5) plans for next annual outcomes meeting. Expansion of Nurse Residency Program The UHC/AACN Nurse Residency ProgramTM has expanded to 85 sites in 31 states (See Attachment 1). Conferences, Webinar, and Article AACN conference programming has highlighted the nurse residency program in sessions at the 2012 Baccalaureate Conference and the upcoming 2013 Spring Annual Meeting: Baccalaureate Conference, San Antonio, November 16, 2012 How Faculty Can Support the UHC-AACN Nurse Residency Program As patient complexity increases, so does the necessity for programs that transition graduates to increased competence in the practice setting. Learn more about the UHC-AACN nurse residency program, its achievements across the country, and specifically how undergraduate and pre-licensure educators can contribute to the success of these collaborations between academic and practice institutions. Speakers: Debra McElroy, MPH, RN, Director, Nursing Leadership, University HealthSystem Consortium, Chicago, IL; and Claudia Diebold, MSN, RN, CNE, Senior Lecturer, College of Nursing, University of Kentucky, Lexington, KY Annual Spring Meeting, Washington, DC, March 16, 2013 The UHC/AACN Residency Program Learn more about this program that prepares nursing graduates for the realities of practice, and how educators can contribute to the success of these collaborations between academic and practice institutions. Speakers: Debra McElroy, MPH, RN, Director, Nursing Leadership, University HealthSystem Consortium, Chicago, IL; Kathryn May, PhD, RN,FAAN, University of Wisconsin, Karen Miller, PhD, RN, FAAN, University of Kansas AACN Webinar: 12/6/2012 from 2:00-3:00 pm ET Building the Future and Continuing the Excellence: The UHC/AACN Nurse Residency Program Curriculum Update 40 Speakers: Speakers: Debra McElroy, Director, Nursing Leadership, University HealthSystem Consortium, Chicago, IL, Amy Drescher-Crumpley, Administrator, UHC Nursing Leadership Registered: 207; Total Attended:139 Completed Evaluation: 109; Percentage: 78%; Content Score: 4.64 Article: Goode, C., Lynn, M., McElroy, D, Bednash, G., Murray, B. (2013). Lessons learned from 10 years of research on a post-baccalaureate nurse residency program. Journal of Nursing Administration. 43(2), 73-79. Nurse Residency Program (NRP) Strategic Planning NRP strategic planning initiatives include: Revised the NRP curriculum (revision is done every three years). NRP coordinators utilized the 2008 Baccalaureate Essentials, the QSEN competencies, and Core Competencies for Interprofessional Collaborative Practice to perform a gap analysis and determine what revisions need to be made. The NRP curriculum is now online. Moving the NRP out of the research and IRB process and moving towards a benchmarking emphasis on quality outcomes approach. This change should result in an increased response rate for resident survey participation at the beginning, middle, and end of the residency program. Expanding the evaluation process of the NRP to include nurse managers’ and chief nursing officers’ feedback on the NRP. Dr. Mary Lynn is wrapping up the nurse manager project – a survey tool has been developed and managers are currently being surveyed on their response to the program. Dr. Lynn will be sharing information at the annual outcomes meeting, but preliminary results show a very positive response UHC is currently implementing two new survey tools “The Nurse Resident Progression Survey” and the “The Post-Nurse Residency Survey” – both will be proprietary to the program Exploring the development of a transition-to-practice program for Nurse Practitioners in the acute care setting. Accreditation of Nurse Residency Programs CCNE currently accredits 10 residency programs and has five new applicant programs. Of the new applicant programs, one hosted an on-site evaluation in Fall 2012 and will be considered by the CCNE Board of Commissioners in April. Three of the new applicant programs are scheduled to host on-site evaluations in Fall 2013, and the other is scheduled to host an on-site evaluation in Spring 2014. 41 2013 Annual Outcomes Meeting The next NRP annual outcomes meeting will be held March 4-7, 2013, at the Rancho Bernardo Inn in San Diego, CA. Dr. Geraldine Bednash will give the keynote address at this meeting. Attachment I Alabama DCH Regional Medical Center, Tuscaloosa University of Alabama Hospital, Birmingham (UAB) California Stanford Hospital & Clinics, Stanford UC Davis Health System, Sacramento UC Irvine Medical Center, Fullerton UCLA Health System, Los Angeles Colorado St. Mary's Hospital, Grand Junction University of Colorado Hospital, Aurora Connecticut Middlesex Hospital, Middletown Yale-New Haven Hospital, New Haven District of Columbia MedStar Georgetown University Hospital MedStar Washington Medical Center Florida Holy Cross Hospital, Fort Lauderdale Tallahassee Memorial Hospital Georgia Emory Healthcare, Atlanta Grady Health System, Atlanta Parkland Hospital, Dallas Saint Joseph’s Hospital, Atlanta St. Francis Hospital, Columbus WellStar Health System, Atlanta WellStar Cobb, Austell WellStar Douglas, Douglasville WellStar Kennestone, Marietta WellStar Paulding, Dallas WellStar Windy Hill, Marietta Hawaii Hawaii State Center for Nursing—Nurse Residency Collaborative, Honolulu Castle Medical, Kailua Hawaii Health System Corporation, Honolulu Hawaii Pacific Health—Pali Momi Medical Center, Aiea 42 Hawaii Pacific Health—Straub Clinic & Hospital, Honolulu Kaiser Permanente, Honolulu The Queens Medical Center, Honolulu Illinois Illinois Masonic, Chicago OSF Saint Francis Medical Center, Peoria University of Chicago Medicine, Chicago University of Illinois Hospital & Health Sciences System, Chicago Iowa University of Iowa Hospitals and Clinics, Iowa City Kansas The University of Kansas Hospital Authority, Kansas City Kentucky University of Kentucky Hospital, Lexington Maryland Franklin Square Hospital Center, Baltimore University of Maryland Medical Center, Baltimore Massachusetts Baystate Health Baystate Franklin Medical Center, Greenfield Baystate Mary Lane Hospital, Ware Baystate Medical Center, Springfield Minnesota The University of Minnesota Hospital Fairview, Minneapolis Mississippi Baptist Hospital Desoto, Southaven University of Mississippi Health Care, Jackson Missouri Barnes-Jewish Hospital, St. Louis Truman Medical Center, Kansas City Nebraska Methodist Hospital The Nebraska Medical Center, Omaha Nevada Nevada State College/Sunrise Hospital, Henderson New Jersey The University Hospital at UMDNJ, Newark New Mexico UNM Hospitals, Albuquerque New York Memorial Sloan-Kettering Cancer Center, New York New York-Presbyterian Hospitals, New York NYU Bone and Joint Disease, New York 43 NYU Langone Medical Center, New York Stony Brook University Hospital, Deer Park SUNY Downstate Medical Center/University Hospital, Brooklyn Westchester Medical Center, Valhalla North Carolina Duke University Hospital, Durham University of North Carolina Hospitals, Chapel Hill Ohio Cincinnati Children’s Hospital Medical Center, Cincinnati The Ohio State University Medical Center, Columbus University Hospitals Case Medical Center, Cleveland Pennsylvania The Children's Hospital of Philadelphia, Philadelphia Hospital of the University of Pennsylvania, Philadelphia Pennsylvania Hospital of UPHS, Philadelphia Presbyterian Medical Center, Philadelphia Main Line Health System, Philadelphia Bryn Mawr Hospital, Bryn Mawr Bryn Mawr Rehabilitation Hospital, Malvern Lankenau Hospital, Wynnewood Paoli Hospital, Paoli Riddle Memorial Hospital, Media Penn State M.S. Hershey Medical Center, Hershey Thomas Jefferson University Hospital, Philadelphia South Carolina Medical University of South Carolina, Charleston South Dakota Rapid City Regional Hospital, Rapid City Texas Children’s Medical Center of Dallas Memorial Hermann Hospital, Houston Parkland Health and Hospital System The Methodist Hospital System Trinity Mother Frances Hospital & Clinics, Tyler Virginia Fauquier Health, Warrenton University of Virginia, Charlottesville Virginia Commonwealth University Medical Center Hospital, Richmond Wisconsin University of Wisconsin Hospital and Clinics, Madison Wyoming Cheyenne Regional, Cheyenne 44 CNL Steering Committee Membership Report March 2013 Currently, there are 122 schools in the CNL database. An additional eleven schools have communicated they are exploring or in the planning phase and have asked to be included in the CNL online community database. The growth of CNL enrollments and graduations from 2004 through 2012 are shown in Figure 1. The percentages by model or type of program are shown in Figure 2. Many schools have more than one model, e.g. post-BSN (Model A) and RN-MSN (Model D) programs. In addition, demographic information regarding the geographic distribution and the primary CNL work setting can be accessed at http://www.aacn.nche.edu/membership/membersonly/presentations/2012/12cnlsummit/TornabeniRev.pdf. In February 2013, the Commission on Nurse Certification (CNC) reported having certified 2,490 CNLs. Figure 1: Enrollment and Graduations of CNL Students 2004-2012 45 Figure 2: Percentages of CNL Education Models 2013 CNL Summit & Research Symposium: The fifth, national CNL Summit was held in New Orleans, LA, January 17-29, 2013. Over 375 attendees representing faculty, nursing administrators/managers, CNLs, and students attended this year’s Summit. Evaluations are being processed; however, all feedback received has been extremely positive. The third CNL Visionary Award, which recognizes the long-standing and substantial accomplishments of an individual to the development, promotion and sustainment of the CNL role in U.S. healthcare, was presented to Joan Shinkus Clark, DNP, RN, MBA, FAAN, Vice President and System Chief Nurse Executive, Texas Health Resources, and Marjorie Wiggins, DNP, RN, MBA, NEA-BC, FAAN, Vice President of Nursing and Chief Nursing Officer, Maine Medical Center. This year’s recipients were selected because of their unremitting commitment to the education and advancement of the CNL role and to efforts that have helped to maximize and sustain the impact of the role. Drs. Clark and Wiggins also opened and closed the Summit with their presentations, “Growing and Sustaining the Vision: Implementing the CNL Across a Major Health System” and “The CNL: Scanning the Horizon.” Other highlights of the Summit included the presentation of the second CNL Vanguard Award to Barbara Edwards, MSN, CNL, from the St. Lucie Medical Center in Port St. Lucie, FL for her exemplary work to implement improved, patient-centered care outcomes. Other plenary presentations included a CNO panel focused on integrating and sustaining the CNL across a healthcare system, and back by popular demand Dr. James Smith presented a session on analyzing and presenting data to make your case. These and all plenary and concurrent PowerPoint presentations can be accessed at: http://www.aacn.nche.edu/cnl/professional-development/conferences/13-cnl-summit 46 In addition, 40 podium and 50 poster presentations were selected from the over 180 abstracts submitted for this year’s Summit. CNL Webinar Series A series of webinars, co-sponsored by AACN and CNC, have focused on cost benefits, patient outcomes, and implementation of the role. A list of the archived webinars offered is shown below. All archived webinars are available to the public and accessible at http://www.aacn.nche.edu/webinars/topics#cnl A Service and Academic Partnership to Design and Sustain a CNL Program Making the Business Case for the CNL CNL Outcomes Across Healthcare Systems Early Development and Evolution of the CNL Expanding the CNL Role in Quality and Safety Nursing Schools and Practice Partners: Working Collaboratively and Creatively to Foster the CNL Role Role of the Clinical Nurse Leader in Improving Patient Perception of Care The CNL Job Analysis and Certification Exam Transitioning Second Degree CNL Graduates into Practice: Innovative Models and Successes The CNL and Patient Safety and Quality: The Link to Magnet Status Revision of CNL Competencies The 2011 AACN Master’s Essentials delineates the core outcomes expected of all master’s graduates. A national consensus-building process has been initiated, similar to that used to develop nurse practitioner and clinical nurse specialist role competencies, to identify the additional competencies and curricular components expected of master’s graduates prepared for direct care or CNL certification. Expert panel members have been identified and represent education and practice from diverse geographic, academic, and healthcare settings. The Clinical Nurse Leader Association (CNLA) and CNC, as national stakeholders, are also participating in this national process. In addition to reviewing and revising the CNL competencies and curricular recommendations, the clinical requirements delineated in the white paper will be reviewed and clarified. The second phase of the process will include an electronic review of the draft competencies by a validation panel comprised of a larger representation of CNL education and practice, and potential employers; and final determination of the competencies by the expert panel. The target date for completion of the project is Summer 2013. CNL Resource Coach CNL Resource Coach, Linda Rusch, past CNO at Hunterdon Medical Center (NJ) and early adopter of the CNL role, continues to provide valuable consultative services to administrators, nursing managers, practicing CNLs, students and faculty. The focus of her services is to advance the CNL role at the local and national levels, and to increase communications and contact with healthcare institutional administrators and other leaders. For additional information regarding services provided, access 47 http://www.aacn.nche.edu/cnl/research-coach or contact Linda Rusch at lrusch@aacn.nche.edu. CMS CIIH Collaborative Grant AACN continues to collaborate with Brookdale Senior Living, LLC; North Texas Health Science University; and Florida Atlantic University to implement a CMS Innovations Grant. AACN’s area of focus and responsibility is the integration of the CNL into the interprofessional clinical leadership team in long-term care settings and the evaluation of the impact the CNL has on quality improvement outcomes with particular emphasis on care coordination and readmissions. AACN’s Senior Director of Education Policy, in conjunction with the Brookdale nursing leadership and CNLs, are developing a journaling tool and process to capture the CNL’s input and impact on patient care activities and outcomes. CNL Certification Review Course AACN has committed to developing an online CNL certification review course. To date, a CNL Review Course Advisory Group has been appointed; topics identified; and content experts/module authors identified. Members of the advisory group include: Kim Hall, MSN, RN, CNL, Sierra Pacific Network VISN 21 Frank D. Hicks, PhD, RN, Rush University Diane Park, MSN, RN, CNL, CRRN, University of Wisconsin-Oshkosh Kathryn B. Reid, PhD, RN, CNL, University of Virginia Melissa Vandeveer, PhD, RN, PNP, CNL, Sonoma State University Mary Lou Wesley, MSN, RN, Wellstar Health Care Marjorie Wiggins, DNP, MBA, RN, NEA-BC, Maine Medical Center Course development will begin in March 2013 in collaboration with iCohere, the contracted vendor. The expected launch date for the course is late Fall 2013. CNL Steering Committee Members: Susan Bakewell-Sachs, PhD, RN, The College of New Jersey, Committee Chair Joan Shinkus Clark, MSN, RN, Texas Health Resources, AONE representative Ola Fox, DNS, RN, Spring Hill College James Harris, DSN, MBA, RN, CNL, APRN, Office of Nursing Services, Department of Veterans Affairs Judith Fitzgerald Miller, PhD, RN, CNL, FAAN, University of Missouri-Columbia Karen Ott, MSN, RN, Department of Veterans Affairs, DVA liaison Kathryn Reid, PhD, RN, University of Virginia Linda Rusch, MS, RN, AACN CNL Resource Coach Jolene Tornabeni, MA, RN, FACHE, FAAN, past chair of CNL ITF Joanne Warner, PhD, RN, AACN Board liaison Marge Wiggins, DNP, MBA, RN, Maine Medical Center, Joan Stanley, PhD, CRNP, CNL, FAAN, FAANP, AACN staff liaison Kathy McGuinn, MSN, RN, CPHQ, AACN staff liaison Tracy Lofty, MSA, CAE, AACN staff liaison to Commission on Nurse Certification Horacio Oliveira, AACN staff liaison 48 Report on the Graduate Nursing Student Academy (GNSA) March 2013 Since the GNSA was launched in October 2012, the following activities have been undertaken by AACN staff in support of this new initiative. Member Registration: As of February 28, 2013, there were 4,123 graduate nursing students registered for the GNSA. This represents 2,737 students in MSN programs, 725 students in DNP programs, 414 students in PhD programs, and 247 students in other programs, which include post-master’s certificates or dual degree programs. New registration forms for the GNSA are submitted on a daily basis. Leadership Council: In October 2012 AACN released a national call for nominations for the Leadership Council, which will set priorities for future services and programming for the GNSA. Interested students were asked to complete an online application form and had to meet specific criteria in order to serve on the Leadership Council. AACN received 63 applications in total. After a thorough review of each application for eligibility and quality, ten students were selected. In February, AACN announced the Leadership Council members who began their two-year term on March 1, 2013. The Council members, which include four PhD, three DNP, and three master’s program students, are: Kristen A. Altdoerffer, University of Maryland Kim Crosby, University of St. Francis Evangeline Dowling, Arizona State University Emily Emma, The George Washington University Shantel M. Gallegos, Colorado State University-Pueblo Teresa L. Hagan, University of Pittsburgh Sarah J. Hoffman, University of Minnesota J. Michael Leger, University of Texas Medical Branch Michaela Lewis, Medical University of South Carolina Tonya L. Smith, Indiana Wesleyan University Plans are underway to convene the first meeting of the GNSA Leadership Council via conference call in late March. Inaugural Webcast: On February 25, the GNSA hosted its first webcast in collaboration with the Health Resources and Services Administration. The program was titled Pathways to Leadership for the Graduate-Prepared Nurse and featured Dr. 49 Mary Wakefield, who was invited to present by Polly Bednash. Over 1,900 people registered for the webcast with many more listening in during their class sessions. Initial feedback from students was very positive with many requesting similar webcasts featuring national nurse leaders in the future. Developing Programs and Services: In response to input from more than 10,000 graduate nursing students received via an AACN survey, the following programs and services are currently under development for members of the GNSA: Webinars: Additional webinars are being planned for the upcoming months. Topics will include applying for jobs and advice on getting noticed by employers, tips for developing a capstone project and dissertation, and mastering a faculty role. A panel of nurse editors is also being convened to give students advice on how to get published. Career Services: The GNSA has partnered with AfterCollege to develop the Graduate Nursing Career Network, an online job board focusing specifically on jobs for master’s and doctorally prepared nurses. This new resource is currently live and linked to the GNSA web site. Monthly Newsletter: The GNSA will distribute a monthly newsletter to its members – the GNSA Bulletin – with the first issue released at the beginning of March. All subsequent issues will be released on the first Wednesday of every month and provide updated membership information, details on upcoming webinars, scholarship and leadership development opportunities, and a different student highlighted every month. Student Collaboration Community: GNSA members have access to a members’ only online collaboration community where they can contribute to discussions, view archived webinars, and access resources. Currently there are 1,082 students participating in the collaboration community. Leadership Opportunities: Students will have the opportunity to further develop their leadership capacity by serving as a GNSA liaison. The goal is to have a GNSA liaison at each AACN member institution. Students who are designated as GNSA liaisons will disseminate information about resources and services to their fellow students and will also have an opportunity to bring feedback and suggestion directly to the Leadership Council. Social Media: Staff have created a Facebook page and Twitter feed where GNSA members can receive news and information about upcoming events, scholarship opportunities, webinars, and other resources. These platforms provide important outlets for engagement and allow students to interact with fellow students across the country. 50 Web Resources: AACN continues to expand the content and resources available through GNSA’s homepage: http://www.aacn.nche.edu/students/gnsa. The site currently contains links to scholarships, fellowships, and financial aid resources; direct access to the collaboration community and career network; a listing of public policy engagement opportunities; and other related resources. Marketing: A mailing to all schools with graduate programs was completed in January and included copies of the GNSA brochure and flyers. Extra copies of these materials are being made available to members on request, and electronic copies may be downloaded from the AACN Web site. Staff will work with the Leadership Council to launch the GNSA School Liaisons program this spring, which will help to expand our outreach efforts. 51 Report on The Study of Identifying Barriers and Facilitators to Nurse Faculty Careers, RWJF Grant #9468 March 2013 Purpose of the Study: The 2010 Institute of Medicine (IOM) report, The Future of Nursing: Leading Change, Advancing Health, identified significant research priorities for ensuring the transformation of nursing education. High on this agenda is the need to identify the impact that salary, benefits, and job attributes have on the recruitment and retention of graduate students into nurse faculty careers. This study is aimed to understand how these variables, along with doctoral education experiences, affect decisions for academic or non-academic careers made by those seeking a doctoral degree in nursing. The study also seeks to determine the ideal set of inducements and incentives that can be used by schools nationwide to recruit new faculty, negotiate for needed resources, and retain seasoned nurse educators in teaching roles. Although there were studies that identified barriers and facilitator to faculty careers, most of them were not aimed at doctoral students in nursing, and the scopes of the studies were often limited. Our study is the first one that is aimed to identify barriers and facilitators to faculty careers to doctoral students at the national level. Research Methods: 1,500 PhD students and 1,500 DNP students will be randomly selected from total PhD and DNP students. Since graduates from PhD programs are much more likely to seek faculty careers than graduates from DNP programs, this stratified random sampling approach is justified. To assure the representativeness of the data collected from the survey, the response rate is targeted as 70%. What we expect to generate: Doctoral Education: Time to doctoral education from initial licensure as a Registered Nurse (RN) Mean age of doctoral students Expected time to graduation with a doctoral degree Percent of doctoral students on fast track (entering doctoral programs at postbaccalaureate level) Factors that prevented students from pursuing doctoral education earlier 52 Factors that motivated students to pursue a doctoral degree Factors that influenced students to choose their specific doctoral programs Teaching, research, and leadership development activities and their impact on students’ confidence in teaching, research, and interests in academic careers Interaction with mentor and its impact on students’ confidence in teaching, research, and interests in academic careers Levels of confidence in conducting various academic activities, which are also measures of students’ preparation for academic careers Faculty Experiences Students’ faculty status (full-time/part-time, level of teaching) Percentage of students with faculty status Level of satisfaction with various aspects of faculty role Likelihood of continuing faculty careers after graduation Post-Graduation Plan for Academic Careers Students’ plan for academic or non-academic careers For students who plan to pursue academic careers, their preferred teaching setting, preferred faculty role, and preferred level of teaching Changes in students’ plan for academic careers during doctoral education Changes in students’ perception of faculty role during doctoral education Perceived factors by students that could influence them to or dissuade them from pursuing faculty careers Association between post-graduation plan for academic careers and students’ demographic and academic characteristics, employment activities, financial support, research, teaching development activities, and interactions with mentors. Association between post-graduation plan for academic careers and perceived factors by students that could influence them to or dissuade them from faculty careers Geraldine (Polly) Bednash, Principal Investigator Di Fang, Co-Principal Investigator 53 Report of the Interprofessional Education Collaborative (IPEC) March 2013 This report addresses the activities and progress of IPEC from October 2012-March 2013. During this time frame, highlights include: 1) October 2012 IPEC Institute; and 3) Plans for 2013 IPEC Institutes. October 2012 IPEC Institute IPEC hosted a repeat faculty development institute, reflecting the theme Designing an Interprofessional Curriculum: Planning, Strategies and Successes, on October 14-17, 2012 at the Crowne Plaza Atlanta Perimeter at Ravinia in Atlanta. Programming was anchored in the Core Competencies for Interprofessional Collaborative Practice released by IPEC last year. The institute provided faculty from across the health professions with the opportunity to meet with peers in plenary and interactive learning sessions focused on building strong programs for team-based learning. Attendees were divided into teams with three to five members representing faculty from a minimum of three health professions. At least one team member was from a nursing, dental, medical, pharmacy or public health school. A total of 58 teams with approximately 300 participants attended. Based on evaluations of the Spring Institute, the agenda was updated to reflect some suggestions from the Spring participants. Presentations and resources were shared with participants prior to the meeting. The institute website has a wealth of IPEC resources: http://www.aacp.org/meetingsandevents/2012FallIPEC/Pages/Resources.aspx 2013 IPEC Institutes David Davis from AAMC developed a proposal that was approved by the IPEC CEOs for the next phase of IPEC Summits. The Spring 2013 summit will focus on quality and patient safety on May 20-22, 2013 at the Dulles Hyatt in Herndon, VA. The overall goal of the institute is to create faculty champions who can enhance interprofessional curricula, learning experiences, and assessment of learners in quality improvement and patient safety at the point of care. Faculty across the health disciplines will come together to explore how to embed quality improvement and patient safety (QI/PS) content into their curriculum, while learning how to create and assess clinical QI/PS projects. Upon returning to their home institutions, 54 workshop participants will help to develop faculty teams with the knowledge and skills necessary to implement an interprofessional education plan focused on quality improvement and patient safety. The interprofessional teams will draw faculty from Dentistry, Medicine, Nursing, Pharmacy, Public Health, and other professions as appropriate. Ideally, teams of 3-5 members will attend, and the teams will include: one member who represents one of the IPEC professions; one member who has knowledge of quality improvement and patient safety; and one member who is in a position to affect curricular changes in his/her home institution. The Institute will begin at 8:00 a.m. on Monday, May 20, 2013. Therefore, participants should arrive the afternoon or evening of Sunday, May 19, 2013. The institute will conclude at 12:00 p.m. on Wednesday, May 22, 2013. The workshop objectives for this summit will be: Describe basic QI/PS processes and techniques Create competency-based, practice-based curricula in QI/PS Create and assess clinical QI/PS projects for learners Design and implement assessment strategies, e.g., Objective Structured Clinical Examinations Implement faculty development in QI/PS at the home site Advocate for curricular and educational reform in QI/PS at a local level Format: Participants will engage in highly interactive case-based and discussion-based activities, with time for team planning and reflection, information sharing, and networking. Precourse readings will be assigned prior to the face-to-face workshop. The post-course period will afford opportunities for online networking and a community of practice, linked to other similar national activities aligned with AAMC’s Teaching for Quality initiative and AACN’s Quality and Safety Education for Nurses (QSEN) initiative. Postcourse resources will include Internet-based materials, the IPE PORTAL collection, and the online iCollaborative for sharing. AACN is taking the logistical lead for this institute. Registration for the institute began on January 28 2013; capacity was reached in 2 days: 36 teams and 155 people are registered. 45 teams and 172 people are on the waiting list. 55 2013 Fall IPEC Institute The institute is being planned for late September to early October A possible venue for the Fall Institute is Chicago at the Intercontinental Hotel The American Association of Colleges of Osteopathic Medicine (AACOM) will take the logistical lead for this institute. The same planning group will continue for the Fall meeting 56 Robert Wood Johnson Foundation New Careers in Nursing Scholarship Program January 2013 Goal 1: Expand support for students previously underrepresented in nursing and assist with the development of a demographically representative professional nursing workforce. In the fifth year, of the New Careers in Nursing (NCIN) scholarship program, 55 schools of nursing will award 400 scholarships to underrepresented and economically disadvantaged second degree nursing students; 320 to accelerated degree baccalaureate students and 80 to masters’ students. To date, 119 unique schools of nursing from 41 states and the District of Columbia have participated in the NCIN scholarship program. With this fifth funding round, the Robert Wood Johnson Foundation will have authorized 2,717 scholarships, equivalent to $27,170,000 for accelerated degree nursing students. The sixth NCIN call for proposals was released in late October 2012 and closed January 9, 2013. Applications from 102 schools of nursing in 37 states and the District of Columbia request 1,578 scholarships totaling $15,780,000 funds for the 2013-2014 grant period. This sixth call authorizes up to 400 scholarships. The National Advisory Committee for NCIN will convene in April 2013 to review proposals and make funding recommendations to the Foundation. Program Outcomes: 1. Since its inception, diversity in nursing school grantees has increased. In 20082009 grantees reported 58% diversity and 36% male enrollment. In 2011-2012, diversity in nursing school grantees increased to 65% and 41% male enrollment. In addition to increased enrollment of underrepresented students by grantees, the applicant pool of these grantees continues to demonstrate greater diversity. 2. Cultural shifts have been reported by grantees as more diverse students have enrolled. Grantees report hiring Diversity Officers, forming Diversity Committees and an overall increased awareness of the need for greater diversity. 3. The Pre-entry Immersion Program (PIP), designed to prepare NCIN scholarship recipients for the academic rigors of an accelerated program, has 57 demonstrated overwhelming success among grantees. As expected, a majority of grantees now make this offering available to all enrolled students and do not limit it to NCIN scholars. In many instances this program is also been offered to traditional students. To build on that success, NCIN launched the PIP Online Supplement in August 2012.This online supplement will assist students, including those who must relocate for school, become familiar with nursing terminology before they start their coursework in an accelerated program. This practice matches the students’ predilection for online interaction, ensures consistency across the NCIN grantee institutions, and helps students develop a connection with classmates, even before they start the program, which helps increase success rates and improves retention. Doctoral Advancement in Nursing (DAN) Survey results from NCIN scholars indicated that more than 90% of these students intend to pursue advanced education. In response to this finding, AACN was awarded a planning grant by RWJF to explore opportunities and options to more rapidly advance the career trajectory of these and other early career nurses. A planning committee composed of nurse educators and leaders in the education industry was formed in October 2012 to address the shortage of scholars pursuing doctoral degrees. The DAN committee is in the process of developing strategies to identify, support and assist newly licensed nurses in applying for and enrolling in doctoral programs. A white-paper describing the committee’s recommendations will be available in June 2013. Goal 2: Assist nursing schools in their efforts to leverage support for expanding capacity in accelerated nursing programs. Outcomes: 1. Grantees reported a number of ways in which they successfully leveraged scholarship funding to increase capacity, including: - Several grantees were awarded funding from HRSA and the Helene Fuld Trust using models similar to the NCIN program requirements. - Some increased and expanded use of simulation labs to reduce clinical demands. - Several grantees expanded university-community partnerships for clinical placements. - Grantees report additional sources of institutional support to expand enrollment of diverse students. Goal 3: Support schools in the design and implementation of recruitment, leadership development and mentoring programs. In 2012, the National Program Office (NPO) produced and distributed a Recruitment Toolkit to all program sites. The toolkit was created to assist schools with developing 58 student recruitment plans that will enhance their efforts to recruit more underrepresented students. The tool kit was posted to the NCIN website along with all other toolkits that the program has developed (www.newcareersinnursing.org/resources). A hard copy was presented to all program liaisons. The Mentoring and Leadership Development Toolkits were revised and made available to grantees and posted on the website. The toolkits include a student section to help scholars learn how get the most out of their mentoring relationships. To date, NCIN toolkits have been downloaded approximately 1,616 times by both grantees and non-grantees. The Mentoring Toolkit is the most downloaded resource, with a total of 613 downloads. (www.newcareersinnursing.org/resources) Project Impact Evidence of NCIN program impact includes the following: 1. Adding the PIP Program and use of the PIP Online Supplement. 2. The evaluation focus of NCIN for the second period is Teaching and Learning in Accelerated Degree Nursing Program. 3. The formation of the NCIN Scholars Network was initiated by scholars. Students are developing a structure and organization for the Network with assistance from the National Program Office and two faculty advisors. 4. Increasing the proportion of nursing students from groups underrepresented in nursing. -Nurses from underrepresented backgrounds represent 16.8% of nurse workforce; - 60% NCIN scholars are from groups underrepresented in nursing, this percentage is increased to 79% when males are included; 5. Men comprise 6.6% of nation's nursing workforce -Men comprise 39% of NCIN scholars 6. Assessing cultural shifts—current program measures will focus on sustaining a commitment to the education and training of students from underrepresented and disadvantaged backgrounds. The challenge is identifying when the support and impetus provided by the NCIN program has established practices that will perpetuate its goals. A web conference on this topic is scheduled for March 14, 2013. Retention of Diverse Students: “Creating Inclusive Learning Environments” Paul Gorski, PhD New Century College, George Mason University 59 March 14, 2013 2 P.M. EST Commission on Nurse Certification (CNC) Board of Commissioners Report March 2013 The Commission on Nurse Certification Board of Commissioners (CNCBOC), chaired by Dr. Enna Trevathan, conducted its Annual Business Meeting via conference call on November 1, 2012. The following is a summary of CNC’s recent activities for the Clinical Nurse Leader (CNL®) Certification Program following CNC’s Annual Business Meeting. Administration CNC in collaboration with Schroeder Measurement Technologies, Inc. (SMT), the contracted testing vendor, and volunteer item writers are in the process of finalizing new exam items for the Spring 2013 testing period. Although a revised exam was offered in April 2012, CNC continues to develop items to offer various exam forms throughout the year. Since September 2012, approximately 130 new multiple choice items have been developed by CNL item writers. To ensure that the updated exam form meets national certification standards, a cut-score study must be conducted. Subject matter experts in collaboration with the testing agency will participate in the study to determine a passing score that reflects the minimal competency of a CNL. Consequently, there will be a delay in all exam score results and pass/fail notices from the April 1-May 24, 2013 CNL Certification Exam period. Those taking the exam from April 1-May 24 will receive their pass/fail results via email by June 24, 2013. It is extremely important that all examinees include an accurate primary email address on their CNL Certification Application. Successful candidates will receive an email notification of passing only – a score and diagnostic score report will not be provided to the candidate. Unsuccessful candidates will receive an email notification of failing the exam along with the score and diagnostic score report. CNC regrets the delay in the exam results. Originally, the study would have been completed with those registered the first week of April. Unfortunately, the majority of those testing registered for a later date, and a minimum number of examinees is required for the study. If you have questions regarding the Spring 2013 testing period or cut-score study, contact Tracy Lofty, CNC’s Director, at tlofty@aacn.nche.edu or call (202) 463-6930, ext. 242. 60 To date, there are 2,489 CNLs total. Since the launch of the new multiple choice exam in April 2012, there has been an increase in the number of applications received as summarized below: Testing Periods Spring Summer Fall/Winter TOTAL 2011 Year 289 208 296 793 2012 Year 360 256 271 887 CNL students in their last term of a CNL education program should register for the exam prior to graduation. Students and graduates may sit for the exam at a school of nursing or at a testing center provided by the SMT. To register as an exam site, submit the Site Registration Form posted on http://www.aacn.nche.edu/cnl/exam-site-registration. Since April 2012, the CNL Certification Exam pass rate is averaging 73%. Aggregate pass rates of students/graduates are forwarded as applicable to the CNL faculty contact and Dean approximately 45 days after a testing period. Future examination dates are: April 1-6, 2013 (registration deadline: March 1, 2013) April 29-May 24, 2013 (registration deadline: March 22, 2013) July 15-August 9, 2013 (registration deadline: June 7, 2013) December 2-13, 2013 (registration deadline: November 1, 2013) January 20-31, 2014 (registration deadline: (December 16, 2013) Last year, CNC contracted with Seacrest Consulting, a company that focuses on assisting certification organizations with program accreditation. CNCBOC is currently working with Seacrest to develop a comprehensive policy and procedure manual to meet accreditation criteria; Commissioners and staff are serving as the content experts in the development of the new and revised policies. All other documents will be updated as necessary to reflect policy changes. The most significant policy change will occur July 1, 2013 – the exam may not be proctored by faculty of a CNL education program. This policy change is an effort to avoid a perceived conflict of interest in accordance with certification program accreditation standards. In December 2012, CNC posted a Call for Volunteers to fill CNCBOC positions – two from academia and two from practice; the deadline to apply was February 15th. In addition, CNC recently posted an announcement to recruit a new public member (http://www.aacn.nche.edu/cnl/cnc/get-involved). Applications for the public member position are due by March 29, 2013. CNC’s Nominating Committee will review all applications in March and new Board members will be approved by May 2013. Terms for all positions begin July 1, 2013. 61 CNCBOC conducted a conference call on February 14, 2013 to finalize and approve CNC’s FY2014-2017 strategic plan and FY2014 budget and to discuss how CNC is addressing the key messages/recommendations of the IOM Future of Nursing report. The budget was developed in consultation with CNC’s Finance Committee chaired by Dr. Patricia Thomas. Marketing CNC’s Marketing Committee, chaired by Dr. Mary Seed, conducted a conference call along with CNL Ambassadors on November 19, 2012 to finalize CNC’s marketing plan. The overall marketing objective is to promote value in CNL certification. The marketing plan will be monitored and reviewed regularly by the Marketing Committee and staff. On November 9, 2012, CNC representatives (Tracy Lofty, Dr. Enna Trevathan, and Dr. Patricia Thomas) along with AACN representatives (Dr. Joan Stanley and Lauren Inouye) met with Ellen-Marie Whelan, Senior Advisor, CMS Innovation Center at the Department of Health and Human Services in Washington, DC. The meeting was a result of CNC’s Marketing Committee recommending that CNC educate key leaders on the CNL role. The CNL Bulletin. CNC in collaboration with AACN developed the Fall 2012/Winter 2013 issue of The CNL Bulletin (http://www.aacn.nche.edu/cnl/FallWinter2012.pdf). CNL Vanguard Award. CNC and AACN presented the second annual CNL Vanguard Award during the CNL Summit to Barbara Edwards, MSN, CMSRN, CNL, of St. Lucie Medical Center. This national award recognizes a certified CNL for innovative and outstanding professional performance and advocacy of the CNL role. In addition, the award promotes the contributions of the CNL in transforming healthcare. Clinical Nurse Leader Association. CNC continues to provide administrative services to the Clinical Nurse Leader Association (CNLA) and to market certification to its members. CNC is contracted through December 31, 2013. To date, there are 195 active CNLA members. To join CNLA, go to http://www.cnlassociation.org/. CNL Research Symposium. CNC partnered with CNLA to present the second CNL Research Symposium, Research, Quality Improvement and Evidence-based Practice: Catalysts to Innovation, on January 17, 2013 prior to the CNL Summit in New Orleans. More than 130 individuals registered for this workshop. Slide presentations are posted on http://www.aacn.nche.edu/cnl/professional-development/conferences. Individuals interested in presenting during the 2014 CNL Research Symposium should submit the Speaker Proposal Form (http://www.aacn.nche.edu/leading-initiatives/cnl/cnlcertification/pdf/Speaker-Proposal-Form.pdf) to CNC. CNL Summit. During the CNL Summit, Ms. Lofty, in collaboration with Dr. Pamela DiNapoli of the University of New Hampshire, presented two concurrent sessions of Preparing for the New CNL Certification Exam. Handouts are posted on http://www.aacn.nche.edu/membership/membersonly/presentations/2013/13cnlsummit/Lofty-DiNapoli.pdf. 62 Online Discussion Boards. To date, The CNL Online Community, an online discussion board managed by CNC and AACN, includes 1,313 active members; 1,075 individuals have logged on at least once. CNL students and graduates may register on http://www.aacn.nche.edu/cnl/professional-development/online-community. On March 25, 2013 from 2:00 to 3:30 p.m., CNC will host an online CNL Certification Exam chat room for prospective CNLs. This platform provides an opportunity for participants to connect with other CNL students, CNLs, and CNC staff. They will have an opportunity to discuss CNL Certification Exam preparation, ask CNC staff about the exam format, and learn how CNLs prepared for the exam. Discussion will be facilitated by CNC staff and volunteer CNL Ambassadors. A transcript of the discussion will be available and posted on The CNL Community after the session. CNL faculty are encouraged to register with CNC’s discussion board on www.nurseslounge.com. To date, 134 individuals have registered with this online discussion board. The discussion board continues to be monitored and maintained by CNC staff. Commission on Nurse Certification Board of Commissioners: Enna E. Trevathan, DNP, MSN, MBA, RN, CNL - Chair University of San Francisco Mary S. Seed, PhD, RN, CNL – Vice Chair University of San Francisco Patricia L. Thomas, PhD, MSN, RN, CNL - Treasurer Trinity Health System Meredith Wallace Kazer, PhD, APRN, CNL, A/GNP-BC - Secretary Fairfield University School of Nursing Sue Hartranft, PhD, ARNP, CNL Morton Plant Mease Health Care Rosemary L. Hoffmann, PhD, RN, CNL University of Pittsburgh Susan Ottenfeld, MS, RN, CNL Jesse Brown VA Medical Center Mary Stachowiak, MSN, RN, CNL Saint Barnabus Hospital 63 Tracy Lofty, MSA, CAE, ACA - AACN Staff Liaison Commission on Nurse Certification Dana Reid, ACA - AACN Staff Liaison Commission on Nurse Certification H:\CNL Reports\AACN Board\March 2013 – AACN Membership 64