Cardiac Assessment Study Guide
advertisement

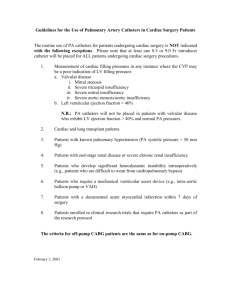
Page 1 of 8 Study Guide for Cardiac Assessment Anatomy and Physiology Base Apex Pericardium Parietal Visceral Precordium, Apex, and Base Anatomy and Physiology Chambers of the heart Right and left atria Right and left ventricles Heart Valves Semilunar valves Pulmonic Aortic Atrioventricular valves (A-V) Tricuspid Mitral Conduction Heart has unique ability: automaticity SA node has intrinsic rhythm, it is called the pacemaker Current flows in orderly sequence, SA to AV to bundle of His, right and left bundle branches, and then through ventricles Electrical impulse stimulates heart to do its work, which is to contract Small amount of electricity spreads to body surface, and can be measured and recorded on electrocardiograph (ECG) ECG ECG waves arbitrarily labeled PQRST, which stand for P wave: depolarization of atria P-R interval: from beginning of P wave to beginning of QRS complex (time necessary for atrial depolarization plus time for impulse to travel through AV node to ventricles) QRS complex: depolarization of ventricles T wave: repolarization of ventricles Electrical events slightly precede mechanical events in heart Conditions Related to Coronary Circulation Ischemia Infarction Angina Cardiac Output 1 Page 2 of 8 CO = SV x HR CO = Cardiac Output Stroke Volume (SV) Volume of blood ejected by the ventricles in one cardiac cycle Heart Rate (HR) Number of cardiac cycles in one minute Problems Associated with Decreased Cardiac Output Loss of blood volume _______________________ Hemorrhagic Burns, Emesis, etc. Heart Rate Tachycardia Bradycardia Pump Issues Coronary Circulation Angina Pectoris __________________________ Congestive Heart Failure (CHF) Trauma Direct Indirect Peripheral Vasculature Arterial system Arteries Arterioles Capillaries Venous system Veins Venules Subjective Data Chest pain Palpitations Syncope Dyspnea Orthopnea Cough Fatigue Cyanosis or pallor Edema Vascular Claudication DVT Past cardiac history Family cardiac history 2 Page 3 of 8 Personal habits (cardiac risk factors) Chest Pain…Cardiac? Something Else? Chest Pain - Cardiac Angina, MI, pericarditis Other concerns Differentiate between cardiac, respiratory, musculoskeletal, gastrointestinal or psychosomatic Past Health History Medical Cardiac specific: AAA, angina, CAD, CHF, HTN, MI, PVD, hyperlipidemia Noncardiac specific: bleeding or blood disorder, DM, gout, renal artery disease, CVA, or thyroid disease Surgical Prior cardiovascular procedures: aneurysm repair, coronary bypass graft surgery (CABG), heart transplant, valve replacement, implantable or internal cardioverter or defibrillator (ICD) Common medications Antianginals or vasodilators Antidysrhythmics Anticoagulants Antihypertensives Antilipemics Diuretics Inotropics Thrombolytics Communicable diseases Childhood illnesses Allergies Aspirin ____________________ Seafood Betadine Latex Family Health History Assess for the following diseases Aneurysm – AAA (abdominal aortic aneurysm) CAD (coronary artery disease) CVA (stroke) HTN (hypertension) CHF (congestive heart failure) MI or sudden cardiac death MVP (mitral valve prolapse) Rheumatic fever Social History Alcohol, drug, or tobacco use Sexual practices Work and home environment 3 Page 4 of 8 Stress Health Maintenance Activities Sleep Diet Exercise Health checkups Patient Education Risk factor modification Heart Smart diet Exercise Sexual activity Risk Factors _______________________ HTN, hyperlipidemia, tobacco use, physical inactivity, diet, glucose intolerance, stress, sedentary lifestyle, obesity Nonmodifiable Age, gender, race, family history Assessment Equipment Stethoscope Sphygmomanometer Watch with second hand Assessment tips Explain procedure Ensure room is quiet and well lit Expose patient’s chest only Position patient in a supine or sitting position Stand to the patient’s _______________ Assessment of the Precordium and Peripheral vasculature Inspection Palpation Auscultation Inspection Assess the following areas: aortic , pulmonic, midprecordial, tricuspid, and mitral Normal findings: no visible ______________except for the PMI in the mitral area Palpation Assess for pulsations, thrills, _________________ Assess the following areas: aortic , pulmonic, midprecordial, tricuspid, and mitral Normal findings No pulsations, thrills, or heaves palpated, except in the mitral area where the apical impulse may be palpated 4 Page 5 of 8 Landmarks – APE To Man A=Aortic 2nd ICS RSB P=Pulmonic 2nd ICS LSB E= Erb’s point 3rd ICS LSB T= Tricuspid 4th ICS LSB M= Mitral 5th ICS MCL Auscultation Warm stethoscope Listen to all ______cardiac landmarks Listen for at least a few cardiac cycles in each area Listen first for S1 and S2, then for possible S3 and S4. Finally listen for murmurs, clicks and friction rubs Normal Systolic Sound: S1 S1 – blood heaves against the closed mitral and tricuspid valves in the heart High pitched – heard with diaphragm Heard best at Apex –____________area LUB – dub Normal Diastolic Sound: S2 Represents closure of aortic and pulmonic valves Heard best at Base –____________area lub – DUB Auscultation: Normal Findings Aortic: S2 is louder than S1 Pulmonic: S2 is louder than S1 Midprecordial (______________) both aortic and pulmonic murmurs by be heard Tricuspid: S1 is louder than S2 Mitral: S1 is louder than S2 Mitral and tricuspid: S3 (gallop) may be heard in children, young adults, and pregnant women. S4 may indicate cardiac decompensation Evaluating Cardiac Sounds Rate Bradycardia Tachycardia Rhythm Murmurs, Gallops Clicks or Rubs Abnormal Finding - Murmur Blowing, whooshing, or rasping sounds The result of vibrations caused by abnormal blood flow patterns valve does not close tightly (such as with mitral regurgitation) an irregularity in the shape of a heart chamber or one of the great vessels (such as an aortic aneurysm) Blood is flowing through a narrowed opening or a stiff valve (such as with aortic stenosis). 5 Page 6 of 8 Does not necessarily indicate a disease or disorder, and all heart disorders do not cause murmurs. If difficult to hear Place in lateral recumbent position – low pitched, mitral – use bell Lean patient forward – high pitched, aortic or pulmonic – use diaphragm Murmurs – Seven Descriptive Characteristics Location (where it is loudest) Radiation (from valves to adjacent anatomic areas) Timing (systolic, diastolic) Loudness/Intensity Quality (description) ________________ (high, low) Pattern (crescendo, decrescendo) Grading Intensity of Murmurs The intensity of murmurs range from grade 1/6 to 6/6. A murmur is said to be at least Grade 4/6 if associated with a ____________ Abnormal Finding Click _________________Heart valves – mitral and aortic most common Click noted especially with mechanical valves, human tissue valves produce sounds similar to human valves – but may produce a murmur Pericardial friction rub Caused by rubbing together of the inflamed visceral and parietal layers of the pericardium Noted in ____________________ Characterize based on location, radiation, timing, quality and pitch Does not change with respiration Bruits For persons middle-aged or older, or who show symptoms or signs of cardiovascular disease, auscultate each carotid artery for presence of a bruit This is a blowing, swishing sound indicating blood flow turbulence; normally none is present Lightly apply bell of stethoscope over carotid artery Avoid compressing artery artificial bruit and could compromise circulation Ask person to hold an exhaled breath so that tracheal breath sounds do not mask Sometimes you can hear normal heart sounds transmitted to neck; do not confuse these with a bruit Assessment of Arterial Pulses Evaluate carotid, brachial, radial, femoral, popliteal, posterior tibial, dorsalis pedis Patient position Characteristics: rate, rhythm, amplitude, symmetry Other CV assessments Carotid and Popliteal pulses Dorsalis Pedis and Post-Tibial pulses Capillary Refill Peripheral Edema 6 Page 7 of 8 CMS Check C (_______________) M (Motor function) – neuro function S (Sensation)- neuro function Homan’s Sign Sharply dorsiflex foot toward tibia Should be no pain in calf muscle Tenderness could indicate DVT If DVT suspected, measure calf circumference with nonstretchable tape measure Notify _______________________ Not routine assessment; used in OB Cardiovascular assistive devices Artificial pacemakers, ICD Hemodynamic monitoring Antiembolic stockings Chest tubes EKG monitoring IV Catheters Infants Heart rate best auscultated because radial pulses are hard to count accurately; use small (pediatric size) diaphragm and bell 170 bpm or more with crying or being active to 70 to 90 bpm with sleeping Expect heart sounds to be louder in infants than in adults because of infant’s thinner chest wall. Murmurs are relatively common in first 2 to 3 days because of fetal shunt closure Children Physiologic _______________ is common in children Heart murmurs that are innocent (or functional) in origin are very common through childhood Most innocent murmurs have these characteristics Soft, relatively short systolic ejection murmur Medium pitch; vibratory Best heard at left lower sternal or midsternal border, with no radiation to apex, base, or back Pregnancy Enlarging uterus elevates diaphragm and displaces heart up and to left and rotates it on its long axis Heart sounds Exaggerated splitting of S1 and increased loudness of S1 A loud, easily heard ____________________ Heart murmurs Systolic murmur in 90% which disappears soon after delivery Aging Adults Chest often increases in anteroposterior diameter with aging More difficult to palpate apical impulse 7 Page 8 of 8 S4 often occurs in older people with no known cardiac disease Systolic murmurs common, occurring in over 50% of aging people Peripheral blood vessels grow more rigid with age, resulting in a condition called arteriosclerosis Documentation Chest symmetrical with no visible pulsations, masses, heaves, or scars. No tenderness from palpation of anterior and posterior thorax. No thrills. The abdominal aorta is not enlarged to palpation and there are no bruits. Apical pulse 2+, regular, 64 B/M. Positive S1 and S2. No murmurs, rubs, gallops, or S3 and S4 sounds. No jugular vein distension or carotid bruits. Carotid, brachial, radial, femoral pulses equal and present at a 1+ bilaterally equal. Popliteal, posterior tibial, dorsalis pedis present at a 1+ in left leg. Edema present at +1 in lower left leg. No edema in right leg. Capillary refill <2 seconds in fingers bilaterally and in toes. Negative Homan’s sign. No assistive devices present. ----------------------Carl Smith, ADNS CVTC 8