24- Antihypertensive drugs
advertisement

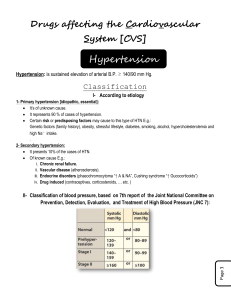
Antihypertensive drugs 1. Overview 1.1 Definition Antihypertensive drugs are used to help control blood pressure in people whose blood pressure is too high. Hypertension is defined as a sustained diastolic blood pressure greater than 90mmHg or systolic blood pressure greater than 140mmHg. 1.2 The type of hypertension Treatments for high blood pressure depend on the type of hypertension. Most cases of high blood pressure are called essential or primary hypertension, meaning that patients have no specific cause of the problem. Elevated blood pressure is usually caused by several abnormalities such as genetic inheritance, psychological stress, environmental and dietary factors (eg. Increased salt decreased potassium intake). Such hypertension usually can be controlled by some combination of antihypertensive drugs and changes in daily habits (such as diet, exercise, and weight control). Controlling primary hypertension, on the other hand, is usually a lifelong commitment. Although people may be able to reduce the amount of medicine they take as their blood pressure improves, they usually must continue taking it for the rest of their lives. Secondary hypertension has a specific cause, such as kidney disease, narrowing of certain arteries, or tumors of the adrenal glands (pheochronocytoma). Correcting these problems often cures the high blood pressure. 1.3 Major factors influencing blood pressure Arterial blood pressure is directly proportional to the cardiac output and the peripheral vascular resistance. The activation of sympathetic nervous system and renin-angiotensin-aldosterone system is responsible for hypertension. Most antihypertensive drugs lower blood pressure by reducing cardiac output and/or decreasing peripheral vascular resistance. 2. Major classes of antihypertensive drugs 2.1 Diuretics 2.1.1 Thiazide Diuretics (moderate efficacy diuretics): hydrochlorothiazide, chlorothiazide, et al. 2.1.1.1 The mechanism for reduction of BP (1) Diuretics decreased BP initially by increasing water and sodium excretion from the kidneys. This causes a decrease in extracellular volume and blood volume, resulting in a decrease in cardiac output. This in turn decreases the pressure within the blood vessels and reduces the workload on the heart. (2) With long-term treatment (6-8weeks), blood volume approaches a normal value, but peripheral resistance decreases. Sodium is believed to contribute to it by increasing Na+--Ca2+ exchange with a resultant decrease in intracellular Ca2+. decrease Na+ of vessel wall ------ Na+-Ca2+ exchange----reduce intracellular Ca2+concentration (smooth muscle cell)----- decrease peripheral resistance. (3) Some diuretics such as indapamide have direct vasodilating effects in addition to their diuretic action. (4) Amiloride inhibits smooth muscle responses to contractile stimuli (eg. NE). 2.1.1.2 Clinical uses (1)Low-dose of thiazide diuretic therapy is safe and effective for hypertension. Thiazide diuretics are appropriate for most patients with mild or moderate hypertension, particularly elderly patients. Low doses of hydrochlorothiazide (25-50mg/d) exert as much antihypertensive effect as do higher doses. (2) Thiazides are useful in combination therapy with other antihypertensive drugs including β-Blockers and ACE inhibitors. 2.1.1.3 adverse effects (1) Thiazide diuretics induce electrolyte disturbance: hypokalemia (potassium depletion), hypomagnesaemia, hyposodium et al. (2) Thiazide diuretics can increase TC, TG, LDL level and renin activity; impair glucose tolerance. Therefore diuretics should be avoided in treatment of hypertensive diabetics or patients with hyperlipidemia. 2.1.2 Loop diuretics (high efficacy diuretics): furosemide, etacrynic acid. The loop diuretics act promptly and can be used in hypertensive emergencies or hypertension combined with renal function failure. 2.1.3 Potassium-sparing diuretics (low efficacy diuretics): spironolactone, amiloride. Potassium-sparing diuretics are useful both to avoid excessive potassium depletion and to enhance the natriuretic effect of other diuretics. 2.2 β-receptor blockers (adrenergic antagonist): propranolol, atenolol, metoprolol. 2.2.1 The mechanism of antihypertensive action (1) β-Blockers reduce BP primarily by decreasing cardiac output. (2) β-Blockers also inhibit the release of rennin from the kidneys. (3) β-Blockers block peripheral β-adrenoceptor in presynaptic membrane to reduce sympathetic vasoconstrictor never activity by inhibitting noradrenaline release. (4) β-Blockers block β receptor in CNS to inhibit vasomotor center. 2.2.2 Pharmacokinetics The β-Blockers are orally active. Propranolol undergoes extensive first-pass elimination. The β-Blockers may take several weeks to develop their full effects. 2.2.3 Clinical use and evaluation The β-Blockers are more effective for treating hypertension in young patients compared to the elderly. The β-Blockers are useful in treating conditions that may coexist with hypertension, such as superventricular tachyarrhythma, previous myocardial infarction, angina pectoris, glaucoma, migraine headache. 2.2.4 Application attention: (1) Beginning with small dose (individual variation is larger) (2) Combining with diuretics 2.2.5 Adverse effects (1) Common effects: CNS side effects: fatigue, lethargy, insomnia; Sexual dysfunction can severely reduce patient compliance. (2)Alteration in serum lipid patterns: decrease HDL and increase plasma triacylglycerol(TG). (3)Drug withdrawal: Abrupt withdrawal may cause rebound hypertension, probably as a result of up-regulation of β receptor. 2.2.6 Contraindication: serious AV conduction block, bradycardia, bronchial asthma, peripheral vascular disease, et al. 2.3 Angiotensin converting enzyme inhibitors (ACEI) 2.3.1.Drugs including Catopril, Enalapril, Cilazapril, Benazapril, Ramipril 2.3.2. The mechanism of antihypertensive action (1) These drugs inhibit angiotensin converting enzyme that cleaves angiotensin I to form the potent vasoconstrictor, angiotensin II(Ang-II) both in circulating system and local tissue. (2) These inhibitors also diminish rate of bradykinin inactivation----increase bradykinin levels----release of NO, EDHF PGE2 (3) By reducing circulating Ang-II levels, ACEI also decrease the secretion of aldosterone, resulting in decreased sodium and water retention. 2.3.3. Clinical use (1) The ACE inhibitors are appropriate for most patients with mild or moderate hypertension, particularly hypertension with high rennin activity. (2) The ACE inhibitors are useful in treating conditions that may coexist with hypertension, such as CHF, myocardial infarction. 2.3.4. The merits of treatment of hypertension: The ACE inhibitors (1)have no tachycardia (2)have no lipid metabolism disturbance (3)Inhibit proliferation and hypertrophy of vascular smooth muscle cells and myocardial cells (4)improve life quality , decrease mortality 2.3.5. Adverse effects (1) Common side effects: hypotension(2%), dry cough(5-20%), rashes, fever, hyperkalemia, (2) angioedema, fetotoxic (influence on development of fetus) 2.4 Angiotensin II type 1 receptor antagonists 2.4.1. Drugs: Losartan, Valsartan, Irbesartan 2.4.2. Clinical use and evaluation Its pharmacological effects are similar to ACEI, while its adverse effects profile is improved over ACEI and dose not cause cough and angioedema although it is fetotoxic. Losartan can promote excrention of uric acid. 2.5. Calcium channel blockers 2.5.1. drugs: nifedipine, amlodipine, verapamil, diltiazem 2.5.2. The mechanism of antihypertensive action Calcium antagonists block the inward movement of calcium by binding to L-type calcium channel in the heart and in smooth muscle of the coronary and peripheral vessel. This cause vascular relaxation and lower blood pressure. Blocks the entry of calcium into the smooth muscle of the blood vessels, causing it to dilate or relax. Certain types such as verapamil and diltiazem can also slow the heart rate. 2.5.3 Therapeutic uses Calcium channel blockers are useful in the treatment of hypertensive patients who also have asthma, diabetes, angina, and/or peripheral vascular disease. 2.5.4 Characters of every drug Nifedipine belongs to short-acting calcium channel blockers which are associated with an increased risk of myocardial infarction and can increase mortality if used for long time. (1)It is more selective to vessels; therefore its action of dilating vessel is stronger than verapamil and diltiazem. (2) Complication: tachycardia, increasing renin activity and cardiac output (3) Treatment of mild and moderate hypertension. Amlodipine belongs to short-acting calcium channel blockers which are better than nifedipine. (1) It takes effect slowly (1--2w), lower BP steadily and continuously (2) It does not affect heart obviously. (3) It can reverse myocardial hypertrophy. 2.6 α-Blockers: Prazosin, Terazosin, oxazosin. 2.6.1. phyarmacological action: α-blockers inhibit the effect of norepinephrine, a hormone that causes constriction of blood vessels, by blocking α1-R selectively. In this way, dilate the arteries and decrea blood pressure, but not decrease cardiac output renal blood flow (renal dysfunction). Moreover, prazosin also decrease plasma TG, TC, LDL, VLDL level and rise HDL. 2.6.2. Clinical use α-Blockers are used to treat moderate hypertension and is prescribed in combination with β-R blockers or diuretics for additive effects. 2.6.3. Adverse effects (1) nasal congestion, dry mouth, drowsiness, headache, diarrhoea et al. (2) first dose phenomenon: postural / orthostatic hypotension, reflex tachycardia 2.6.4. α β- adrenergic receptor antagonist: Labetalol blocks both α-R and β-R. Labetalol blocks β-R more than α-R, blocks β1-R and β2-R in the equal potency, blocks α1-R more than α2-R. Mechanism of lowing BP is due to blocking α1-R and β1-R. 2.7. Centrally-acting drugs: 2.7.1 Clondine 2.7.1.1. pharmacological action (1)antihypertensive effect( iv or oral) (2)sedative effect (3)inhibit gastrointestenal secretion and motion 2.7.1.2 The mechanism of action (1) activate imidazoline I1receptor of rostral ventrolateral medulla (RVLM) (2) excite α2-R of RVLM (3) excite α2-R and imidazoline I1 receptor of peripheral sympathetic synaptic premembrane---- decrease release of NA (4) increase the release of endogenous opioid peptides, such as enkephalin 2.7.1.3. clinical use (1)moderate hypertension (2)morphine addiction 2.7.1.4. adverse effects (1)dry mouth, sedation, headache, sexual dysfunction, constipation. (2)withdrawal reaction: tachycardia, sweating, acute rising in BP, 2.7.2 Methyldopa is used to treat moderate hypertension, particularly with renal function failure complication. 2.7.3 Moxonidine is belong to secondary central hypotensor, mainly excite I1 imidazoline receptor of rostral ventrolateral medulla oblongata. Actions on central and peripheral α2-R are very weak, so the adverse reaction is rare. 2.8. Vasodilators 2.8.1 Hydralazine mainly dilate arteriols but not veins, is useful to treat moderate hypertension, often being combined with other hypotensors. Its can cause resembles erythematosus(10-20%) in large dose. 2.8.2 Sodium nitroprusside lowers BP rapidly by releasing NO. It take effects rapidly(1-2min after iv), the effects disappear quickly too(5min after stopping iv). Sodium nitroprusside is always used to treat hypertensive emergency and severe cardiac failure. 2.8.3 Minoxidil belongs to potassium channel openers. It can promote the growth of hair besides its antihypertensive effect. Treating obstinate hypertension must combine with diuretics and β-R blockers; male alopecia 2.9 Ganglionic blocking agent 2.10 Adrenergic neuron blocking agents: Reserpine and quanethidine have been rarely used because of their severe adverse reaction, reserpine is used in some traditional compounds sometimes. 3. The antihypertensive treatment strategies 3.1 To normalize blood pressure effectively. 3.2 Controlling hypertension is usually a lifelong treatment (patient compliance) 3.3 To prevent target-organ damage to the heart, brain, kidneys and blood vessels. 3.4 To decrease the blood pressure steadily. 3.5 Individualized care. 3.6 To achieve this with no or minimal side effects by combination administration.